Poor sleep (disturbed sleep and/or not getting the recommended 7 to 9 h sleep(Reference Watson, Badr and Belenky1)) is a major public health problem and a regular occurrence for almost half (45 %) of all Australian adults(Reference Gupta, Duncan and Ferguson2). Poor sleep has important implications, including an increased risk of developing chronic conditions such as hypertension, obesity, diabetes and CVD(Reference Cappuccio, Cooper and D’Elia3). As a consequence, it has a significant economic and personal impact (i.e. increased health care costs, lost productivity, impaired decision making, workplace absenteeism, road traffic accidents); at an estimated cost of ∼$66 billion annually in Australia(4). In older adults, poor sleep has also been linked with adverse mental health outcomes including depression, dementia and cognitive decline, particularly in women(Reference Stone and Xiao5).
Many environmental and behavioural factors contribute to the quality of sleep, including lifestyle behaviours such as poor dietary habits, stress and physical inactivity(Reference Binks, Vincent and Gupta6–Reference Memon, Gupta and Crowther8). From a dietary perspective, consumption of foods high in saturated fat, alcohol and caffeine may lead to poor quality sleep(Reference Binks, Vincent and Gupta6). Physical inactivity and stress may also disrupt neuropsychological processes and decrease sleep quality(Reference Wang and Boros9). Despite the availability of population-based diet(10) and physical activity(11) guidelines, most Australians do not meet these recommendations(12). In older adults, reduced appetite(Reference Pilgrim, Robinson and Sayer13) or compromised ability to prepare foods(Reference Ibrahim and Davies14) may affect both the types and amount of food consumed(Reference Pilgrim, Robinson and Sayer13), leading to poorer adherence to dietary guidelines. Age-related increases in sleep disorders (e.g. insomnia, sleep-disordered breathing, periodic limb movements in sleep, restless legs syndrome and REM sleep behaviour disorder)(Reference Byles, Mishra and Harris15) psychological stress(Reference Lavretsky and Newhouse16) and decreased physical activity(Reference Milanović, Pantelić and Trajković17) may also influence sleep quality(Reference Wang and Boros9). Therefore, older adults often report a high prevalence of symptoms of sleep problems (i.e. short sleep duration, longer time taken to fall asleep, increased number of awakenings, etc.)(Reference Gordon, Yao and Brickner18). Older women are also more susceptible to the impact of ageing on sleep compared with older men(Reference Stone and Xiao5). Hormonal changes post-menopause can lead to circadian disruption and sleep architectural changes(Reference Pengo, Won and Bourjeily19). These may explain the gender differences in the relationship between diet and sleep in the older populations previously reported(Reference Lee, Chang and Liu20,Reference Gupta, Irwin and Vincent21) . Given that there is an increasing proportion of older Australians in the population(22), and that older women are more susceptible to the consequences associated with poor sleep, it is important to understand the relationship between dietary behaviours and sleep in this specific demographic; including the influence of contextual factors (i.e. physical activity, stress, alcohol intake) on this relationship.
Therefore, the aim of this study was to explore the association between adherence to dietary guidelines and symptoms of sleep problems (controlling for contextual factors), in a sample of older Australian women (68–73 years of age). Findings from this study will inform the development of interventions and recommendations aimed at improving sleep quality and dietary intake, as well as the overall wellbeing of older women in Australia.
Methods
Study participants and design
This study involved an analysis of data collected in the Australian Longitudinal Study on Women’s Health (ALSWH). This population-based longitudinal study was established in 1996 to monitor the health of Australian women in three age groups according to birth year (1973–1978 cohort, 1946–1951 cohort, 1921–1926 cohort) with a fourth age group (1989–1995 cohort) added in 2013. Details of the study and methods are available at www.alswh.org and have been published elsewhere(Reference Dobson, Hockey and Brown23). Briefly, women were randomly selected from the Medicare database to ensure a nationally representative sample was obtained. Ethical approval was obtained from the Human Research Ethics Committees of the University of Newcastle (approval number: h–076–0795) and the University of Queensland (approval number: 200400224). Participants were invited to complete a survey containing questions on physical and mental health, well-being, lifestyle behaviours, life satisfaction, medical history and demographic characteristics.
The current study used data from the 1946 to 1951 cohort (survey 9, completed in 2019). The response rate from the first survey was 58 %. Information collected on dietary intake, symptoms of sleep problems, stress, physical activity, alcohol intake, sleep medication use and demographic characteristics were included for analysis.
Adherence to dietary guidelines
Dietary intake was assessed using the Commonwealth Scientific and Industrial Research Organisation (CSIRO) Healthy Diet Score tool(Reference Hendrie, Baird and Golley24). This is a validated short FFQ containing thirty-eight questions about the quantity, quality and variety of foods consumed. For food quantity, consumption frequency was converted to the daily number of serves for the following food groups: ‘fruit’, ‘vegetables and legumes/beans’, ‘grains (cereals)’, ‘meat and alternatives’, ‘dairy and alternatives’ and ‘discretionary foods’. For food quality, consumption frequency of wholegrains, reduced fat dairy and water (fluid), meat trimming and the types of fat used were assessed. This allowed the calculation of an overall diet score (out of 100)(Reference Hendrie, Baird and Golley24), based on compliance with the Australian Dietary Guidelines (ADG)(25), with higher scores representing better adherence and diet quality(Reference Hendrie, Baird and Golley24).
Symptoms of sleep problems assessment
Symptoms of sleep problems were explored using five questions asking about the presence of any of these typical sleeping problems: ‘waking up in the early hours of the morning’; ‘lying awake for most of the night’; ‘taking a long time to get to sleep’; ‘worry keeping you awake at night’ and ‘sleeping badly at night’. These questions target symptoms such as difficulty falling asleep and restless sleep; key indicators of poor sleep quality in older populations(Reference Neubauer26). A score was allocated to each of the five questions (1 = ‘Yes’, 0 = ‘No’ responses) and an overall score was determined from the sum of individual scores (max 5), with acceptable internal consistency reliability (Cronbach’s α = 0·643, n 5). Higher scores suggest more symptoms of sleep problems(Reference Neubauer26).
Assessment of demographic and contextual factors
Stress, physical activity, alcohol intake, sleep medication use and demographic characteristics of age and marital status were also explored. Perceived stress was assessed using a 10-item Perceived Stress Questionnaire scale previously developed and validated in the ALSWH(Reference Bell, Lee and Powers27). It includes questions relevant to different aspects of life (i.e. own health, living arrangement, money, health of family members, work/employment, study, relationship with parents, relationship with partner/spouse, relationship with children, relationship with other family members)(Reference Bell, Lee and Powers27). Participants rated each aspect according to the Likert categories ‘Not applicable’, ‘Not at all stressed’, ‘Somewhat stressed’, ‘Moderately stressed’, ‘Very stressed’ and ‘Extremely stressed’, which were scored as 0, 0, 1, 2, 3 and 4, respectively. An overall stress score was calculated using the sum of perceived stress scores across all aspects(Reference Bell, Lee and Powers27).
Physical activity status was assessed using a modified version of Active Australia Survey(Reference Armstrong, Bauman and Davies28), which has previously demonstrated acceptable reliability and validity(Reference Brown, Burton and Marshall29). Participants’ frequency and duration of walking, moderate and vigorous physical activities per week were scored based on MET-minutes/week and categorised as ‘Nil/Sedentary’ (representing 0 to 10 min of moderate activity per week), ‘Low ’ (representing 11 to 150 min of moderate activity per week), ‘Moderate’ (representing 151 to 300 min of moderate activity per week) and ‘High’ (representing > 300 min of moderate activity per week)(Reference Russell, Ball and Brown30). Moderate activity of at least 30 min 5 times per week (> 150 min per week, representing ‘Moderate’ and ‘High’ category of physical activity status) is considered as the threshold of meeting physical activity guidelines(11,Reference Russell, Ball and Brown30) .
Alcohol intake was measured using a questionnaire derived from the Australian National Health and Medical Research Council (NHMRC) guidelines(31) on the frequency and quantity of alcohol intake and was categorised as ‘non-drinker’, ‘Low risk (≤ 2 standard drinks/d)’, ‘Risky (3–4 standard drinks/d)’ and ‘High risk (≥ 5 standard drinks/d)’(Reference Russell and Ball32).
Sleep medication use was assessed using one question on using medication to help sleep. Demographic data of age, living arrangement and marital status were also included.
Statistical analysis
Statistical analysis was performed using SPSS (Version 26, IBM Corp, New York). Descriptive statistics were used to determine the mean ± sd or frequency (%) for diet scores, symptoms of sleep problems, stress score, physical activity status and patterns of alcohol consumption. The association between scores for diet quality and symptoms of sleep problems was investigated using multivariate linear regression, either unadjusted (model 1) or adjusted for the potential confounding influence of demographic (i.e. age and marital status) and lifestyle (i.e. physical activity, stress, alcohol intake, sleep medication use) variables (model 2). Outcomes were presented as regression (standardised) coefficients with 95 % CI. Linear regression assumptions were checked prior to analysis. The linearity of the relationship was investigated via a scatterplot and correlation analysis. A P-value of < 0·05 was accepted as statistical significance.
Results
Data available for the current study included n 7956 women aged 68–73 years (mean ± sd: 70·8 ± 1·5). Demographic characteristics of the participant cohort are presented in Table 1. Most participants were living with partners, family members or others (76·5 %). Less than half (42·3 %) of participants reported not being active or having low physical activity, and the majority (95·2 %) reported not drinking alcohol or having a low risk of drinking alcohol (≤ 2 standard drinks/d). Participants’ mean stress score was 0·4 ± 0·4 (representing not or somewhat stressed).
Table 1 Demographic characteristics of participants

* Presented as mean ± sd.
At the time of the survey, the majority of participants (70·2 %) reported having at least one symptom of sleep problems and 20·5 % had between 3 and 5 symptoms. The mean of the symptoms of sleep problem score was 1·4 ± 1·4 (range 0 to 5). The prevalence of type of symptoms varied, but more than half (54 %) of the participants reported ‘waking up in the early hours of the morning’, almost one-third (31·4 %) reported they ‘took a long time to go to sleep’ and 28·1 % reported they ‘sleep badly at night’. In 14·2 % ‘worry kept them awake’, and another 14·1 % reported they ‘lie awake for most of the night’. However, the majority (n 6287, 83 %) reported not taking any medications in the past 4 weeks to help with sleep.
The average number of serves consumed from the five core food groups and discretionary foods, including the age- and sex-associated (i.e. 70+ years) serve recommendations according to the ADG(10) are presented in Table 2. Participants had lower intakes (number of serves) for ‘dairy and alternatives’ and ‘vegetables and legumes/beans’, and higher intakes for ‘grains (cereals)’ and ‘discretionary foods’ compared with the ADG recommendations. This resulted in an average diet quality score of 56·86 ± 10·73 (n 7141; range from 0 to 100).
Table 2 Number of serves of ADG-based food groups and their comparison between dietary patterns
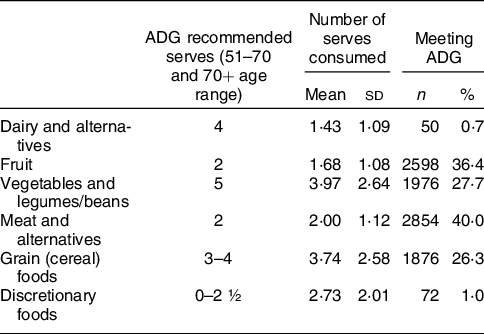
ADG: Australian Dietary Guidelines – serves based on the recommended average daily number of serves for women aged 51–70 and 70+ years(10).
The association between diet score and symptoms of sleep problems is presented in Fig. 1. A higher diet quality score (better adherence to ADG) was associated with lower symptoms of sleep problem score (β: –0·065, 95 % CI: –0·012, –0·005, P-value < 0·001). The association remained significant when the model was adjusted for the confounding influence of demographic (i.e. age and marital status) and lifestyle (i.e. stress, alcohol intake, physical activity, sleep medication use) variables (β: –0·025, 95 % CI: –0·006, –0·000 P-value 0·035). The influence of using sleep medication, not being physically active and higher stress scores (but not risky alcohol intake or demographic variables) were significant in the association between higher diet score and lower symptoms of sleep problems (P-values < 0·001). Linear regression assumptions were met with no multicollinearity observed between independent variables and sleep score (correlation r < 0·7). Probability–probability (P–P) plot showed normal distribution. Cook’s distance was also < 1. However, the dependent variable (sleep score) was not normally distributed (Kolmogorov–Smirnov = 0·246, P-value < 0·01). Given the large sample size (n > 3000), linear regression is still a valid test despite the non-normally distributed dependent variable(Reference Li, Wong and Lamoureux33).

Fig. 1 Associations between scores for diet quality and symptoms of sleep problems confounding by the influence of stress, physical activity and sleep medication use
Discussion
This study explored the association between adherence to dietary guidelines and symptoms of sleep problems in a sample of older Australian women (68–73 years of age) using data from the ALSWH. The data indicated low adherence to dietary guidelines and a high prevalence of having at least one symptom of sleep problems in this population group. The analyses suggest that better adherence to dietary guidelines is associated with fewer self-reported symptoms of sleep problems, even after controlling for the influence of stress, physical inactivity, alcohol intake and sleep medication use.
Most Australians (irrespective of age and gender) do not meet the recommended intakes outlined in the ADG for the core food groups (i.e. fruit, vegetables, grains, lean meats and alternatives, dairy and alternatives) and over-consume discretionary (‘junk’) foods(Reference Williams, Vandelanotte and Irwin34,35) . Adherence to dietary guidelines is important for healthy ageing and to maintain quality of life and good mental health(Reference Milte and McNaughton36). However, poor adherence to dietary guidelines has been previously reported in studies of older Australians(Reference Gadowski, Curtis and Heritier37,Reference Chen, Liu and Sachdev38) . The current study also confirms a similar trend in a relatively large sample of older Australian women. Individual and environmental changes that occur with ageing may explain this poor adherence to dietary guidelines(Reference Pilgrim, Robinson and Sayer13). Many older adults experience a decline in appetite due to changes in the digestive system, increased prevalence of illnesses and medication use and psychological changes(Reference Pilgrim, Robinson and Sayer13). In older women, hormonal changes post-menopause may exacerbate the psychological and mood changes(Reference Pengo, Won and Bourjeily19). Reduced mobility and financial constraints may also affect the accessibility and affordability of food in older ages(Reference Whitelock and Ensaff39). More older women, compared with men are likely to live alone or in cared accommodation(Reference De Vaus and Qu40), further influencing their food choices and dietary quality. While living arrangement was controlled in the analysis of the current study, almost one-fourth (23·5 %) of the older women who participated in this study reported living alone.
The analysis in the present study also indicates that symptoms of sleep problems are highly prevalent in older Australian women. Indeed, the majority (87 %) of the cohort surveyed in the ALSWH reported having at least one sleep problem symptom. This is consistent with data reported in a 2016 survey of Australian adults, with more than half (61·1 %) of adults aged 65 years and older self-reporting to have at least one sleep problem symptom; with a higher prevalence of symptoms in females compared to males in all age groups(Reference Adams, Appleton and Taylor41). A possible explanation may relate to age-associated physiological changes in sleep architecture and normal circadian rhythms(Reference Byles, Mishra and Harris15,Reference Pengo, Won and Bourjeily19) . In older women, this is exacerbated by the age-related decrease in melatonin secretion and increase in the onset of cardiovascular, metabolic and mood disorders(Reference Pengo, Won and Bourjeily19). Other individual and environmental factors such as feeling safe, noise and light, living arrangements, stress and lifestyle/behavioural factors can also influence sleep quality and architecture(Reference Johnson, Billings and Hale42,Reference Binks, Vincent and Irwin43) .
From a dietary perspective, a bidirectional relationship between dietary choices and sleep quality exists. High intakes of discretionary (‘junk’) foods(Reference Binks, Vincent and Irwin43) and lower adherence to healthy dietary patterns (e.g. Mediterranean(Reference Mamalaki, Anastasiou and Ntanasi44)) have been associated with poorer sleep quality(Reference Theorell-Haglöw, Lemming and Michaëlsson45). Furthermore, diets rich in carbohydrates, dairy foods and certain nutrients and phytonutrients have been linked to improved sleep outcomes(Reference Binks, Vincent and Irwin43,Reference Gupta, Irwin and Vincent46) . On the other hand, poor-quality sleep has been linked with increased intake of energy-dense (i.e. discretionary) foods(Reference Soltanieh, Solgi and Ansari47,Reference Spiegel, Tasali and Penev48) .
Several mechanisms are proposed for the relationship between diet and sleep. Dietary intake of the amino acid tryptophan (abundant in dairy, beans, chicken, nuts, etc.) has the ability to convert to serotonin and consequently the sleep-promoting hormone, melatonin, which plays a major role in reducing sleep problems and improving sleep quality(Reference Gupta, Irwin and Vincent46). Carbohydrates (especially low glycemic and complex carbohydrates) in food can also help with the availability of tryptophan to cross the blood-brain barrier and convert to melatonin(Reference Gupta, Irwin and Vincent21,Reference Zimmermann, McDougle and Schumacher49) . In addition, lower consumption of fibre and higher intakes of saturated fats and sugar (characteristics of discretionary foods) have been associated with increased sleep problems and lighter sleep(Reference St-Onge, Roberts and Shechter50). Conversely, sleep restriction has been linked with an increase in the hunger hormone, ghrelin(Reference Spiegel, Tasali and Penev48), a decrease in the appetite-suppressing hormone, leptin(Reference Soltanieh, Solgi and Ansari47,Reference Dashti, Scheer and Jacques51) and stimulation of the brain reward centre(Reference Dashti, Scheer and Jacques51). This may lead to an increase in the number and portion size of meals consumed and desire for energy-dense (i.e. discretionary) foods. As such, adherence to dietary guidelines (that promote healthier food intake behaviours) is likely to be associated with better quality sleep (and vice versa). Results presented in the current study align with this premise, with the regression analyses suggesting that a higher diet quality score is inversely associated with symptoms of sleep problem in older Australian women, even after controlling for other lifestyle and behavioural factors such as stress, alcohol intake, physical inactivity and sleep medication.
Our results also suggest that physical inactivity and higher levels of stress positively influence the association between diet and symptoms of sleep problems in older women. Physical activity can increase energy expenditure, improve neuropsychological performance and reduce mood and stress, ultimately improving sleep quality(Reference Vanderlinden, Boen and van Uffelen52). In a sample of post-menopausal women, a 12-week increase in the amount of walking improved sleep quality and reduced sleep disturbances/problems(Reference Najafabadi, Farshadbakht and Abedi53). Physical activity is also associated with improved mental and emotional health and reduced stress and anxiety in older adults(Reference Kazeminia, Salari and Vaisi-Raygani54). Stress can lead to nervous system hyperactivation, overriding the normal sleep-promoting processes(Reference Kalmbach, Anderson and Drake55). It can also lead to depression and anxiety, further reducing sleep quality(Reference Hu, Visser and Kaiser56).
Results for the current study are based on a large sample of older Australian women (n 7956), which increases the generalisability of the findings. However, the current study also has some limitations. Outcomes are based on self-reported information, which may not accurately represent an individual’s actual measures. The study was also limited to women aged between 68 and 73 years, limiting the generalisability of the findings to all older Australians (i.e. 65 years and older). Also, while the sleep questions were chosen to target common symptoms of sleep problems in older adults and had acceptable internal consistency reliability, they do not constitute a validated scale. Future studies using validated scales, such as Pittsburgh Sleep Quality Index(Reference Buysse, Reynolds and Monk57) in this population are required to support the findings of this study. Other individual factors, such as sleep hygiene and environmental factors such as light, noise and distractions, can also confound the relationship between diet quality and symptoms of sleep problem, which were not accounted for in the available data. Furthermore, since the findings are based on observational data, a cause–effect relationship cannot be determined.
Conclusion
Symptoms of sleep problems are prevalent in older Australian women and their adherence to dietary guidelines is poor. There is a link between better adherence to dietary guidelines and lower likelihood of reporting symptoms of sleep problems in this population, even after controlling for the influence of stress, physical inactivity, alcohol intake and sleep medication use. Future public health guidelines and interventions aimed at improving diet and sleep quality in older women should consider the bidirectional relationship between the two and assess and monitor their adherence to the guidelines to improve general health and well-being in this population.
Acknowledgements
Acknowledgements: This study involved an analysis of data collected as a part of the Australian Longitudinal Study on Women’s Health (ALSWH) by The University of Newcastle and the University of Queensland. We are grateful to the Australian Government Department of Health and Aged Care for funding and to the women who provided the survey data. The authors thank Dr Gilly Hendrie from CSIRO Nutrition & Health and Professor Rebecca Golley from Flinders University for permission to use the Short Food Survey (also known as the CSIRO Healthy Diet Score).” Furthermore, all parties are to notify each other before presenting any Short Food Survey data at a conference, seminar or other forum and, where appropriate, provide copies of the presentation, papers etc. to Dr Gilly Hendrie ([email protected]). Authorship: S.K., C.V., G.D.M., C.I., G.E.V. & C.G.: conceptualisation, design and methodology; S.K.: Data Analysis; S.K., C.V., C.I., G.E.V. & GC: Interpretation and Result drafting; S.K. Manuscript drafting; All Authors: Validation, Review and Contribution to the final manuscript. Ethics of human subject participation: This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving research study participants were approved by the [name of the ethics committee. Written informed consent was obtained from all subjects/patients.
Financial support:
SK is supported by a Postdoctoral Fellowship from the National Heart Foundation of Australia. GDM is supported by a Principal Research Fellowship from Australian National Health and Medical Research Council.
Conflict of interest:
Authors have no known conflict of interest that influence this work.






