e-Poster Viewing
Abstract
A complex polymorphous psychosis or a cycloid psychosis with a different onset?
-
- Published online by Cambridge University Press:
- 19 July 2023, pp. S1058-S1059
-
- Article
-
- You have access
- Open access
- Export citation
100 years of recovery and prognosis in schizophrenia
-
- Published online by Cambridge University Press:
- 19 July 2023, p. S1059
-
- Article
-
- You have access
- Open access
- Export citation
Fate of the first Brief Psychotic Disorder in hospitalised patients
-
- Published online by Cambridge University Press:
- 19 July 2023, p. S1059
-
- Article
-
- You have access
- Open access
- Export citation
Aggressive behavior in patients hospitalised for a psychotic relapse
-
- Published online by Cambridge University Press:
- 19 July 2023, pp. S1059-S1060
-
- Article
-
- You have access
- Open access
- Export citation
Testostérone and Positive Dimension in Schizophrenia
-
- Published online by Cambridge University Press:
- 19 July 2023, p. S1060
-
- Article
-
- You have access
- Open access
- Export citation
The role of immune disfunction in schizophrenia pathogenesis
-
- Published online by Cambridge University Press:
- 19 July 2023, pp. S1060-S1061
-
- Article
-
- You have access
- Open access
- Export citation
Comorbid Obsessive-Compulsive Symptoms in Schizophrenia - Diagnostic and Treatment Challenges
-
- Published online by Cambridge University Press:
- 19 July 2023, p. S1061
-
- Article
-
- You have access
- Open access
- Export citation
Clozapine in First Episode Psychosis: The best is delayed
-
- Published online by Cambridge University Press:
- 19 July 2023, p. S1061
-
- Article
-
- You have access
- Open access
- Export citation
A phenomenological approach to the affective core of Delusional Disorder.
-
- Published online by Cambridge University Press:
- 19 July 2023, p. S1062
-
- Article
-
- You have access
- Open access
- Export citation
Daytime/nighttime levels of serum IL-33 in schizophrenia at hospital admission and before discharge
-
- Published online by Cambridge University Press:
- 19 July 2023, pp. S1062-S1063
-
- Article
-
- You have access
- Open access
- Export citation
Differential diagnosis of late onset psychotic symptoms. A case report.
-
- Published online by Cambridge University Press:
- 19 July 2023, p. S1063
-
- Article
-
- You have access
- Open access
- Export citation
Ekbom Syndrome - A Case Report
-
- Published online by Cambridge University Press:
- 19 July 2023, pp. S1063-S1064
-
- Article
-
- You have access
- Open access
- Export citation
Combined Foot and Eye Dominance Scale as a useful tool for the assessment of lateralization
-
- Published online by Cambridge University Press:
- 19 July 2023, p. S1064
-
- Article
-
- You have access
- Open access
- Export citation
Evaluation of sexual dysfunction in patients with schizophrenia:A descriptive cross-sectional study
-
- Published online by Cambridge University Press:
- 19 July 2023, p. S1064
-
- Article
-
- You have access
- Open access
- Export citation
Folie a Deux in 2 Elderly Sisters - Challenges in Diagnosis and Management
-
- Published online by Cambridge University Press:
- 19 July 2023, p. S1065
-
- Article
-
- You have access
- Open access
- Export citation
Neutrocytopenia associated with a lurasidon therapy in a patient with paranoid schizophrenia
-
- Published online by Cambridge University Press:
- 19 July 2023, p. S1065
-
- Article
-
- You have access
- Open access
- Export citation
The correlation beteen lifestyle and risk of metabolic syndrome in schizophrenia
-
- Published online by Cambridge University Press:
- 19 July 2023, p. S1066
-
- Article
-
- You have access
- Open access
- Export citation
Double dystonia secondary to risperidone: acute laryngeal dystonia and oculogyric crisis.
-
- Published online by Cambridge University Press:
- 19 July 2023, p. S1066
-
- Article
-
- You have access
- Open access
- Export citation
Amantadine augmentation in electroconvulsive therapy-resistant catatonia: a case report.
-
- Published online by Cambridge University Press:
- 19 July 2023, pp. S1066-S1067
-
- Article
-
- You have access
- Open access
- Export citation
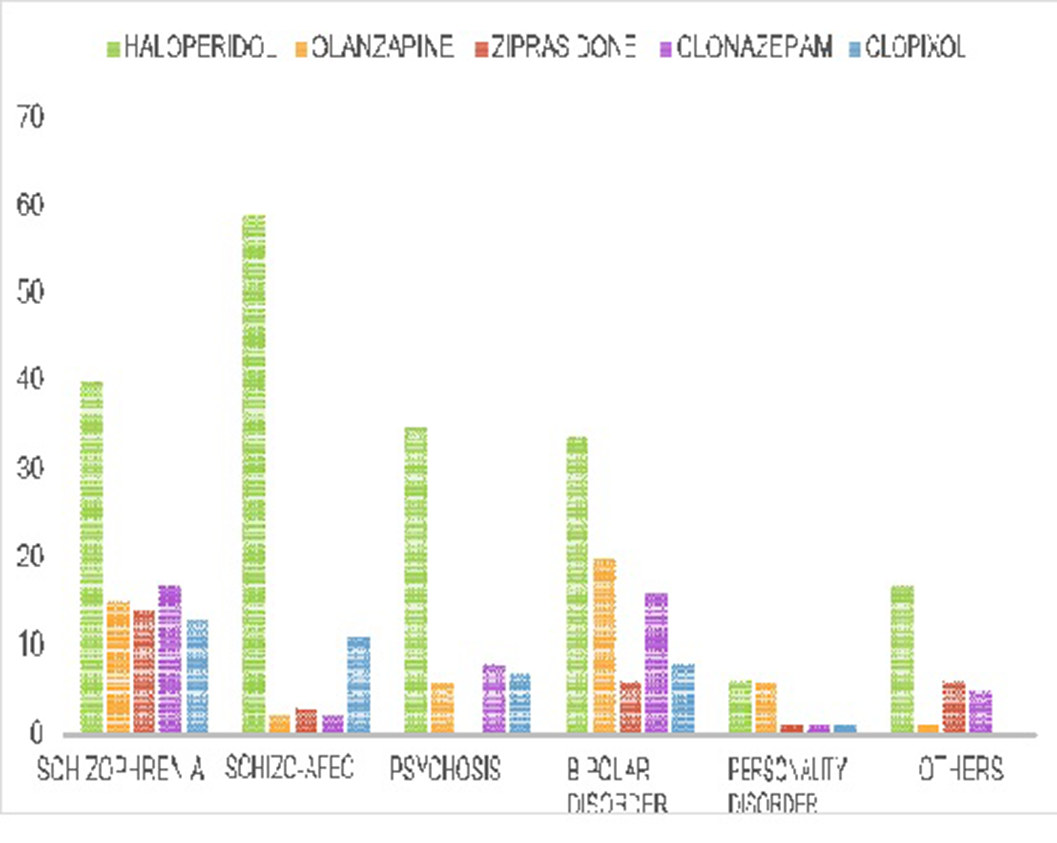
Review of a sample of episodes of forced medication in an area of southern Spain
-
- Published online by Cambridge University Press:
- 19 July 2023, p. S1067
-
- Article
-
- You have access
- Open access
- Export citation