Child undernutrition leading to suboptimal growth in early life continues to be highly prevalent in South Asian countries(Reference Caulfield, Richard and Rivera1, Reference Black, Allen and Bhutta2). In Bangladesh, two out of every five children suffer from moderate-to-severe underweight(3), falling at least 2 sd below the median weight-for-age of the WHO Child Growth Standards(4). In addition to facing an elevated risk for infectious diseases(Reference Caulfield, Richard and Rivera1, Reference Lanata and Black5), undernourished children face impaired cognitive and social development, poor school performance, reduced physical work capacity and the development of long-term cardiovascular and metabolic conditions(Reference Pelletier, Olson and Frongillo6–Reference Victora, Adair and Fall11). Despite the importance of early child nutrition for survival and long-term development, the international nutrition community has faced many challenges in the development of a consensus on priorities, actions and strategies to combat the enduring problem of child undernutrition(Reference Pelletier, Olson and Frongillo6, Reference Bryce, Terreri and Victora12, Reference Morris, Cogill and Uauy13).
More than 30 years ago, the 1978 Alma-Ata Declaration(14) envisioned the provision of comprehensive, universal and affordable health-care services in all countries through community-based primary health care (PHC). The PHC model emphasized the delivery of care by community workers with a focus on prevention and on the underlying determinants of maternal and child health and nutrition, including the environment (community), agriculture, education and livelihoods(Reference Lawn, Rohde and Rifkin15). The process of local community involvement and improvement of the social environment was challenging and inconsistently applied(Reference Lawn, Rohde and Rifkin15, Reference Morley, Rohde and Williams16). Instead, a selective programme of PHC with a focus on the implementation of a few key interventions deemed to be most cost-effective and epidemiologically important was generally favoured in many developing countries(Reference Walsh and Warren17). Key interventions aimed at improving child undernutrition implemented over this period largely focused on maternal and child-level determinants, including low birth weight(Reference de Onis, Blossner and Villar18–Reference Christian, West and Khatry20), maternal undernutrition(Reference Kramer21, Reference Semba and Victora22), vitamin A(Reference West23, Reference Lopez, Mathers and Ezzati24), Fe and Zn deficiencies(Reference Caulfield, Richard and Rivera1, Reference Brown, Wuehler and Peerson25, Reference Kraemer and Zimmermann26), infectious diseases(Reference Rowland, Rowland and Cole27, Reference Assis, Barreto and Santos28), feeding practices, maternal education and health-seeking behaviour(Reference Frongillo, de Onis and Hanson29–Reference Terra de Souza, Peterson and Andrade32).
More recently, renewed interest in the importance of community-based PHC, use of community health workers and increased recognition of the social determinants of health have highlighted the ongoing relevance of the Alma-Ata principles for maternal and child health in developing countries(Reference Lawn, Rohde and Rifkin15, Reference Marmot33, Reference Haines, Sanders and Lehmann34). Landmark cross-country research by Smith and Haddad(Reference Smith and Haddad35, Reference Smith and Haddad36) has implicated basic contextual, environmental and societal factors (including health environments, women's education and status and food availability) as important determinants of child nutrition in developing countries. The potential strength of these underlying determinants of child nutrition was first raised at Alma-Ata in 1978 and later incorporated into the framework on child undernutrition developed by UNICEF in 1991(14, 37). Although recent studies have shown a growing recognition that mothers and children reside in communities and that shared environmental contexts may be of key importance in improving child nutrition(Reference Griffiths, Madise and Whitworth38–Reference Uthman40), we are not aware of any corresponding research that has systematically quantified and investigated the influence of multiple aspects of the community environment on child nutritional status.
The present paper extends previous research by examining the amount of variation in child nutritional status in Bangladesh that is attributable to communities, with a focus on specific aspects of the community environment that may account for such variation(Reference Subramanian, Glymour and Kawachi41). The Bangladesh Demographic and Health Survey (BDHS)(42) reported moderate evidence of between-community variation in child weight-for-age (8 % of variation attributed to communities) and height-for-age (9 % of variation attributed to communities). In the present study, we tested whether community water and sanitation infrastructure, availability of community health and education services, community employment and social participation, and education level of the community explained between-community variation in child nutritional status using a nationally representative sample of children in Bangladesh.
Methods
Sample
In 2004, a household survey was conducted in Bangladesh to obtain detailed information on maternal and child health and nutrition as part of the demographic and health survey (DHS) programme(42). The 2004 BDHS used a nationally representative multi-stage sample design, stratified according to urban and rural areas. The primary sampling unit was defined as census enumeration areas, based on the 2001 census. We have used the term community to describe these small areas, which comprised around 100 households. The 2004 BDHS systematically selected a sample of 10 811 households from 361 communities, with a target of thirty households per community. Among the selected households, 10 500 (99·8 %) were contacted successfully. All ever-married women aged 15–49 years residing in contacted households were invited to participate in the survey, and 11 440/11 601 (98·6 %) of eligible women completed an interview(42).
The BDHS identified 6424 children younger than 5 years of age in the sampled households. In order to capture continuing influences of the community environment on child nutritional status, we excluded 571 children (8·8 %) who did not permanently reside in the community in which they were sampled. An additional 2·1 % of the sample had missing information on covariates and were excluded from analyses, which yielded a final sample for the present analysis of 5731 children under the age of 5 years and their mothers.
Outcome measures
Weight and height measurements for children (aged 0–59 months) were obtained by trained data collectors, using solar-powered scales and adjustable measuring boards, according to the standard DHS fieldwork protocol(42). The measured weights and heights of children were converted to weight-for-age and height-for-age sd units (Z-scores) using the WHO Child Growth Standards(4). These measures are routinely analysed to provide assessment of child nutritional status(Reference Black, Allen and Bhutta2).
Assessment of community environment
Data collected in the 2004 BDHS occurred at the individual, household and community levels. Community-level data collection and community service availability assessments were carried out in December 2003, immediately before individual- and household-level data collection processes, which were completed between January and May 2004(42). In the present study, we used each data source to assess the community environment according to four specific characteristics, which are described below. We operationalized each community characteristic in tertiles (low, moderate and high) in order to allow for the possibility of non-linear relationships with child nutrition.
‘Community water and sanitation infrastructure’ is based on the household-level questionnaire and represents the proportion of households within each community that reported being supplied with piped drinking water and modern toilet facilities.
‘Availability of community health and education services’ was defined using data from the community-level questionnaire. Distances to educational facilities (primary and secondary schools) and health-care services (hospitals, primary care facilities, private and non-governmental organization (NGO) clinics) were reported to survey interviewers by a group of knowledgeable informants (community officials, teachers or local leaders) identified in each community(42). Informants reported the distance to services available in their communities as the approximate distance (in km) from the centre of their community to the facility. To ensure the validity of these self-reported measures, fieldworkers randomly checked a subsample of the reported distances. Previous DHS validation studies have documented good accuracy using this methodology(Reference Wilkinson, Njogu and Abderrahim43). The quality of service facilities was not assessed in the survey. Information on all community-level services was combined into a single variable using principal component analysis, with communities reporting shorter distances to services being considered to have better community service availability.
‘Community employment and social participation’ was defined using individual responses from female survey respondents and their husbands and aggregated to the community level. Community social participation came from the proportion of female respondents (husbands of survey respondents were not asked about social participation) who were members of at least one of six possible organizations, including Grameen Bank, mother's club and Bangladesh Rural Advancement Committee (a community-based NGO). Community employment was based on the proportion of respondents' husbands who were employed outside the agricultural sector, as an indicator of community economic development. Women's employment was not included as a community-level characteristic, as a majority of women (82 %) were not currently working at the time of the survey(42). Social participation for women and employment for men were combined in a simple average and aggregated to the community level to represent the level of community employment and social participation.
The ‘education level of the community’ was specified as the average number of years of education of all residents of the community over the age of 15 years. These data came from the household questionnaire, which included a listing of all members of the household, their age and number of years of education, and covered 34 910 individuals in the 361 communities (mean: 61 individuals per community). The mean number of years of education of our sample was about 4·2 years.
Communities were further classified according to the type of residential environment (urban centre, small city, town or rural area) and geographical region of Bangladesh (Barisal, Chittagong, Dhaka, Khulna, Rajshahi or Sylhet).
Individual-level covariates
We included several individual socio-economic and demographic variables as covariates in our analyses(Reference Subramanyam, Kawachi and Berkman44): child's age and gender, preceding birth interval, early breast-feeding, recent illness, mother's education, father's education, mother's age at birth, mother's BMI, household socio-economic status (SES) and household food security. Preceding birth interval was classified as 0–23, 24–47 and ≥48 months. A binary illness variable indicated whether the mother reported an incidence of fever, cough or diarrhoea in the previous 2 weeks. Mother's and father's education was defined in terms of the following categories: no formal education, primary education, secondary education and higher than secondary education. Maternal age at birth was measured in years. Mother's BMI (kg/m2) was calculated from the measured heights and weights of survey participants. Household SES was measured by an index derived from the education of the head of the household, as well as from dwelling characteristics and ownership of consumer goods and assets(Reference Rutstein and Johnson45, Reference Filmer and Pritchett46). Asset-based indices are routinely used as measures of wealth or SES, and have been validated in several countries(Reference Rutstein and Johnson45–Reference Barros and Victora47). Household food consumption during the past year, a basic measure of food security, was based on a single question in the BDHS asking whether the household had sufficient food throughout the previous year or if there was an occasional or continuous deficit (or surplus) of food.
Analysis
Descriptive statistics were calculated and mean weight-for-age and height-for-age of children were examined across individual- and community-level variables using the STATA statistical software package version 10·0 (StataCorp., College Station, TX, USA). Our analytical approach used a multilevel conceptual and methodological framework and was conducted in two steps(Reference Subramanian, Jones and Duncan48). First, we examined the overall effect of communities on child nutritional status by specifying a two-level random intercepts linear model, composed of children (level 1) nested in communities (level 2)(Reference Goldstein49, Reference Raudenbush and Bryk50). Second, we extended this model by including the specific community exposures under study, which were hypothesized to account for between-community differences in child nutrition(Reference Subramanian, Glymour and Kawachi41). A total of six models were specified for each outcome (child weight-for-age and height-for-age Z-score). All models were estimated using MLwiN statistical software version 2·20 (Bristol, UK)(Reference Rasbash, Browne and Healy51), and included random intercepts for each community and parameters for the sd of individual- and community-level errors(Reference Gelman and Hill52).
The first model estimated (model 1) was an unconditional model, which examined the average weight-for-age and height-for-age of children assessed for the amount of variation across communities. From this model, between-community variation was summarized using the ‘intra-class correlation’, or the relative value of the community-level variance to total variance, and was expressed as a percentage from 0·0 to 100·0(Reference Goldstein49, Reference Gelman and Hill52). In model 2, we added individual-level covariates to model 1, and in model 3 we added community-level covariates to model 2. Models 2 and 3 re-estimated the community-level variance, adjusted for ‘compositional’ (individual-level) characteristics of the communities (in model 2) and further adjusted for ‘contextual’ (community-level) variables (model 3). The intra-class correlation estimates of community-level variance obtained from these models indicated the extent to which community-level variation in child weight and height persisted over and above that which could be attributed to observed individual-level factors (model 2) and observed community-level environmental factors (model 3).
The next set of estimated models tested the association between characteristics of the community environment and child weight- and height-for-age. First, a separate multilevel model was fitted for each outcome specifying one of four community-level characteristics (community water and sanitation infrastructure, availability of community health and education services, community employment and social participation, and level of community education) but no individual-level predictors (model 4A–D). To each of these models, the matrix of individual-level covariates was added (model 5A–D). The primary interest of these models was the association between child nutritional status and a specific aspect of the community, i.e. community water and sanitation infrastructure, before (model 4) and after (model 5) the model was adjusted for individual-level compositional characteristics of the community. The final model (model 6) included all community-level and individual-level covariates and was equivalent to model 3, although the interest here was in examining the mutually adjusted coefficients for community-level environmental characteristics.
Results
The sample for analyses comprised 5731 children (aged 0–59 months) from 361 communities (seventeen from urban centres, twenty-three from small cities, eighty-two from towns and 239 from rural areas), with an average of sixteen children per community. The distribution of sample characteristics and the average height-for-age and weight-for-age across the characteristics are presented in Table 1. No between-community differences in child-level demographics (age and sex) were observed. Overall, the average height-for-age and weight-for-age of children were −1·9 and −1·8, indicating that the sample of children was 1·9 and 1·8 sd below the WHO reference population in height and weight, respectively.
Table 1 Sample characteristics and average weight-for-age and height-for-age of 5731 children aged 0–59 months in the 2004 Bangladesh Demographic and Health survey

SES, socio-economic status.
Figure 1 presents the average weight-for-age and height-for-age of children across tertiles of each community characteristic. Descriptively, these figures indicated a trend of increasing child nutritional status across increasing levels of community water and sanitation infrastructure, availability of community health and education services, community employment and social participation and level of community education. All trends were statistically significant (P-trend < 0·001).
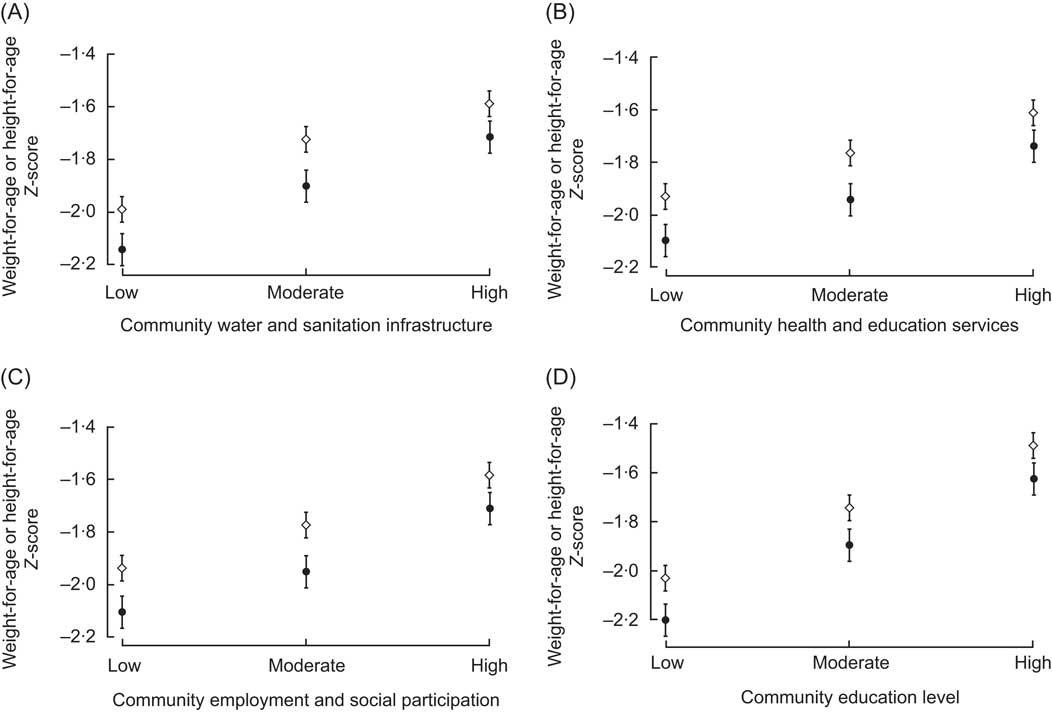
Fig. 1 Mean weight-for-age (◊) and height-for-age (•) of Bangladeshi children aged 0–59 months across low, moderate and high levels of assessed community characteristics: community water and sanitation infrastructure (A), community health and education services (B), community economic and social participation (C) and level of community education (D). All trends were statistically significant (P-trend < 0·001)
Variation attributable to communities
Figure 2 shows the amount of variation in child weight- and height-for-age that was attributed to communities in our sample, in the unconditional model (model 1) and in the models adjusted for individual- (model 2) and community-level covariates (model 3). Geographical (between-community) variation in the unconditional model accounted for 7·8 % and 8·5 % of the total variation in child weight-for-age and height-for-age, respectively. The model adjusted for individual-level covariates explained roughly half (53 %) of the between-community variation in weight-for-age and slightly less than half (41 %) of the height-for-age variation. In model 3, which added community-level characteristics, the remaining variation was further reduced by 20 % for weight-for-age and 13 % for height-for-age, indicating the importance of the community environmental context in further explaining between-community variation beyond individual variables alone. Community-level variation in child nutritional status remained statistically significant in all models.
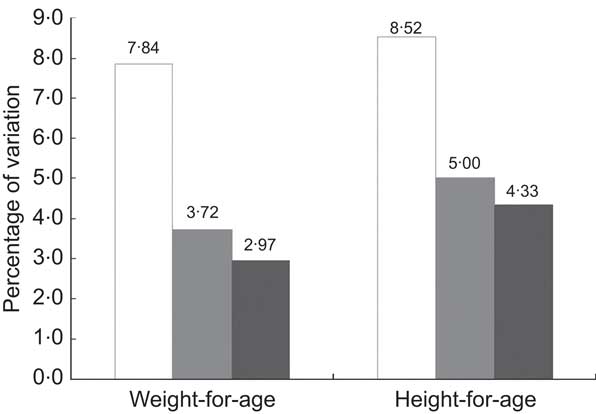
Fig. 2 Percentage of variation attributed to communities for child weight-for-age and height-for-age before (model 1, □) and after (model 2, ![]() ) adjusting for individual-level covariates and after adjusting for community-level environmental characteristics and individual-level covariates (model 3,
) adjusting for individual-level covariates and after adjusting for community-level environmental characteristics and individual-level covariates (model 3, ![]() )
)
Note: The proportion of variation attributable to communities was calculated as the ‘intra-class correlation’(48). The model adjusted for maternal and child covariates (model 2, ![]() ) included child's age, gender, preceding birth interval, early breast-feeding, recent illness, mother's age at childbirth, mother's BMI, mother's and father's level of education, household socio-economic status and household food security. The final model (model 3,
) included child's age, gender, preceding birth interval, early breast-feeding, recent illness, mother's age at childbirth, mother's BMI, mother's and father's level of education, household socio-economic status and household food security. The final model (model 3, ![]() ) included community environmental characteristics under study (community water and sanitation infrastructure, community health and education services, community economic and social participation and level of community education) and was adjusted for community-level covariates (‘type of community’: urban centre, small city, town, rural village and ‘geographic division’: Barisal, Chittagong, Dhaka, Khulna, Rajshahi or Sylhet) and all individual-level covariates
) included community environmental characteristics under study (community water and sanitation infrastructure, community health and education services, community economic and social participation and level of community education) and was adjusted for community-level covariates (‘type of community’: urban centre, small city, town, rural village and ‘geographic division’: Barisal, Chittagong, Dhaka, Khulna, Rajshahi or Sylhet) and all individual-level covariates
Community characteristics associated with child nutritional status
Table 2 presents point estimates, se and 95 % CI for each community characteristic from multilevel regressions of child weight-for-age and height-for-age (models 4A–D, 5A–D and 6). The upper third of this table presents unadjusted associations between each community characteristic and child weight-for-age and height-for-age from four multilevel models (models 4A–D). These models find that all levels of community characteristics are positively associated with child nutritional status (weight-for-age and height-for-age). In the middle third of Table 2, models for each community-level characteristic adjusted for individual-level covariates are presented (models 5A–D). The addition of individual-level covariates to these models attenuated the associations between the community environment and child nutrition, although community water and sanitation infrastructure, level of community education, and the highest levels of community health and education services and community employment and social participation remained positively associated with weight-for-age (Table 2, left side). The findings for the height-for-age outcome were largely similar. In the height-for-age models adjusted for individual-level covariates (Table 2, model 5A–D, right side), the highest level of community health and education services was found to be positive and statistically significant, although the moderate level of community sanitation infrastructure was not. In the lower third of Table 2, we present estimates and 95 % CI from multilevel models for weight-for-age and height-for-age adjusted for all community- and individual-level covariates (model 6). In these models, level of community education emerged as a strong independent predictor of child height-for-age (highest v. lowest tertile, β = 0·18 (se 0·07); moderate v. lowest tertile β = 0·14 (se 0·06)) and weight-for-age (highest v. lowest tertile β = 0·21 (se 0·06); moderate v. lowest tertile β = 0·14 (se 0·05)). In the height-for-age model, the highest tertile of community employment and social participation also emerged as significant compared with the lowest tertile (β = 0·13 (se 0·06); Table 2).
Table 2 Estimates, se and 95 % CI for community-level environmental characteristics derived from multilevel regressions of child weight-for-age and height-for-age v. community-level characteristics and covariates
*In model 4 (A–D), one community-level environmental characteristic was modelled at a time (the lowest tertile is reference (not shown)), without adjustment for individual-level covariates.
†In model 5 (A–D), one community-level environmental characteristic was modelled at a time, adjusting for the following individual-level covariates: child's age, gender, preceding birth interval, early breast-feeding, recent illness, mother's age at childbirth, mother's BMI, mother's and father's level of education, household socio-economic status and household food security. Models also adjusted for community-level covariates: (type of community: urban centre, small city, town, rural village; and geographic division: Barisal, Chittagong, Dhaka, Khulna, Rajshahi or Sylhet).
‡In model 6, the community-level environmental characteristics presented are mutually adjusted, with additional adjustment for all individual- and community-level environmental covariates (as in model 5).
Discussion
The present study investigates the shared community environment as a determinant of child nutritional status in Bangladesh. We found that between-community variation in child weight-for-age and height-for-age was not completely accounted for by the distribution of child- and maternal-level correlates and risk factors. Although studies on the determinants of child nutrition in Bangladesh have traditionally focused on individual-level factors(Reference Rahman, Chowdhury and Karim31, Reference Bairagi and Chowdhury53–Reference Hussain and Smith56), our research shows the potential independent influence of the community environment on the distribution of nutritional status among Bangladeshi children. This finding is further supported by demonstrated reductions in unexplained between-community variance in child nutritional status after adjustment for specific contextual variables measured at the community level. Examined associations between specific community characteristics and child nutritional status were found to be positive, although independent effects of community environmental variables were largely attenuated after accounting for individual-level covariates. Community education, however, remained a consistent and positive predictor of child nutritional status across all models, including fully adjusted models.
These findings provide public policy information on the potential benefits of targeting the community context, especially education, for the improvement of child nutrition. Our results are consistent with other recent studies in developing countries on the influence of shared residential context on child nutritional status(Reference Pongou, Ezzati and Salomon39, Reference Uthman40, Reference Fotso57). Maternal education has long been established as having a positive effect on child nutrition, and recent evidence from India recognizes additional benefits of educated fathers, grandmothers and the community at large(Reference Frost, Forste and Haas58, Reference Moestue and Huttly59). Children will likely benefit from residing in communities that are primarily literate and in which community-based approaches to the management of undernutrition (e.g. the promotion of breast-feeding and appropriate complementary foods) are emphasized(Reference Bhutta, Ahmed and Black60). We noted a positive relationship between community employment/social participation and child nutritional status. One possible mechanism through which such an effect may operate has been suggested in a report from India, in which participation in micro-credit organizations was found to increase sharing of child-care-related knowledge between mothers(Reference Moestue, Huttly and Sarella61). Income-generating activities, development of social networks and increasing maternal economic autonomy have also been shown to contribute to health improvements(Reference Griffiths, Madise and Whitworth38, Reference Rosenzweig and Wolpin63).
An important consideration of the study findings is that characteristics of the community environment such as levels of services and infrastructure may not be distributed randomly(Reference Rosenzweig and Wolpin63, Reference Sastry64). Development policies, programmes or other external factors may influence the distribution of certain facilities and services within communities with high (or low) socio-economic or health indicators, leading to an uneven distribution of resources across communities. Uneven distribution of services and infrastructure may have implications on child and maternal nutrition and on national and sub-national nutrition programmes and policies. In addition, individuals may choose to live in certain communities on the basis of reputation or perceived levels of services and amenities. Although community-level variables were treated as exogenous in our analyses, we have controlled for the possibility of migration by excluding individuals who were not permanent residents of their community. Typically, women included in the analysis had resided in their communities for 12 years.
There are certain limitations of our study. The measures used in the present study to denote access and availability to facilities were based on self-reported distances that may be prone to error, although validation studies indicate good accuracy. In addition, the quality of services was not assessed in the BDHS community service availability questionnaire. This may have introduced some measurement error into the community health and education services availability variable, since quality of services is likely to be inconsistent across communities in this sample. In all analyses, significant between-community variation in child nutritional status remained unexplained, underscoring the need for further systematic research on the mechanisms operating at the community level that may influence child nutritional status. Potential mechanisms related to child nutrition that we could not examine within the BDHS include access, availability and price of food, as well as local transportation and safety(Reference Chow, Lock and Teo65). Furthermore, the reliability of the observed coefficients on the community-level predictors studied is subject to unmeasured maternal, child or household covariates. These coefficients should be interpreted with the consideration that their effects may be proxies for uncontrolled covariates at individual and household levels. We found maternal BMI to be positively associated with child nutritional status, suggesting the importance of considering the health of the parents(Reference Subramanian, Ackerson and Smith66).
In summary, our study suggests evidence for independent contextual variation in child nutrition in Bangladesh. Although prospective studies are required to fully understand the potential influence of the community environment on child nutritional status, we emphasize the importance of incorporating a community-based approach for research on preventive and treatment strategies for child undernutrition in developing countries.
Acknowledgements
The present research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors. C.K.C. is supported by a Public Health (Sidney Sax) Overseas Fellowship co-funded by the National Health and Medical Research Council and National Heart Foundation of Australia. S.V.S. is supported by the National Institutes of Health Career Development Award (NHLBI K25 HL081275). The analysis was conducted entirely using public use secondary data sets with no access to identifiers. The authors have no conflict of interest to declare. D.J.C. planned the study and conducted statistical analyses with the collaboration of C.K.C. and S.V.S. All authors participated in interpretation of the data and writing the manuscript. D.J.C. acknowledges the instruction and guidance of Dr M Boyle, Dr K Georgiades, H Kyu and student colleagues participating in the course title Advanced Analysis of Survey Data at McMaster University.






