Symptoms of respiratory tract infection (RTI) are a frequent reason for visiting a doctor( Reference Gulliford, Latinovic and Charlton 1 , Reference Ginde, Mansbach and Camargo 2 ), although most people with symptoms of a common cold do not seek health care( Reference Scambler, Scambler and Craig 3 ). RTI represent a major economic burden because of the need for hospitalization in severe cases and because of disruption of work caused by RTI symptoms( Reference Fendrick, Monto and Nightengale 4 , Reference Bramley, Lerner and Sames 5 ).
Vitamin D plays an important role in bone mineralization and skeletal health( Reference Ross, Manson and Abrams 6 ). Vitamin D is formed in the skin from 7-dehydrocholesterol after activation by UV-B radiation (290–315 nm)( Reference Holick, Uskokovic and Henley 7 ). Dietary products are the most important source of vitamin D at northern latitudes during the wintertime because sunlight exposure during this time is inadequate for inducing sufficient endogenous production of vitamin D( Reference Laaksi, Ruohola and Mattila 8 , Reference Engelsen, Brustad and Aksnes 9 ). Foods that contribute the most to dietary intake of vitamin D vary between countries and habitual dietary patterns. In Norway, fish and cod-liver oil are the predominant food sources( Reference Engelsen, Brustad and Aksnes 9 , Reference Calvo, Whiting and Barton 10 ) and intake of fresh cod liver is important in northern Norway( Reference Brustad, Alsaker and Engelsen 11 ). The presence of the vitamin D receptor and enzymes needed to hydroxylate 25-hydroxyvitamin D (25(OH)D) to its active form 1,25-dihydroxyvitamin D is found in the intestines and in tissues throughout the body( Reference DeLuca 12 ); this widespread distribution suggests that vitamin D is important for more than skeletal health. Low circulating levels of 25(OH)D have been associated with a number of extraskeletal diseases such as cancer, diabetes and CVD( Reference Holick 13 – Reference Pilz, Dobnig and Fischer 16 ), and 25(OH)D plays a key role in immunity( Reference Laaksi 17 ).
Previous studies have reported associations between low serum 25(OH)D concentration and increased occurrence of RTI( Reference Ginde, Mansbach and Camargo 2 , Reference Laaksi, Ruohola and Tuohimaa 18 , Reference Berry, Hesketh and Power 19 ). However, other studies performed in selected populations have not found a significant association( Reference Porojnicu, Moroti-Constantinescu and Laslau 20 , Reference Aydin, Aslan and Yildiz 21 ). The evidence for a favourable effect of vitamin D on resistance to RTI is inconsistent and is not based on randomized controlled trials( Reference Laaksi 17 ). The main aim of the present study was to determine whether vitamin D level is associated with symptoms of RTI in the Norwegian population.
Experimental methods
The Tromsø Study is a repeated, multi-purpose, population-based study in the municipality of Tromsø, Norway( Reference Jacobsen, Eggen and Mathiesen 22 ). Tromsø is a city in the northern part of Norway, 69°N, with 69 000 inhabitants. The sixth survey (Tromsø 6) took place between October 2007 and December 2008, with a break in July 2008. The Department of Community Medicine, University of Tromsø, provides scientific leadership and administration of the Tromsø Study.
Persons invited to participate in Tromsø 6 included all residents aged 40–42 years or 60–87 years, a 10 % random sample of individuals aged 30–39 years, a 40 % random sample of individuals aged 43–59 years, and persons who had attended the second visit of Tromsø 4 if not already included in the three groups above. The Population Registry of Norway, which maintains the unique national identity number given to all citizens, was the source of the invitations.
The attendance rate was 65·7 %, giving 12 984 individuals who attended the first visit. About two-thirds of the participants who attended the first visit were invited to a second visit, which included an extended medical examination, if they fulfilled one of the following criteria: all persons aged 50–62 years or 75–84 years, a 20 % random sample of men and women aged 63–74 years, or persons, if not already included in the two groups above, who had attended the second visit of Tromsø 4.
A total of 7958 persons who attended the first visit were invited to the second visit, of which our study was a part, and 7307 attended (91·8 %).
Examinations
Information was obtained from questionnaires, clinical examinations and blood samples collected by specially trained health-care workers using standardized procedures.
The primary outcome was recent symptoms of RTI based on the response to the following question asked during the second visit: ‘Have you had symptoms of the common cold, acute bronchitis or other airway infection in the last 7 days?’ Those answering ‘yes’ were asked how many days had passed since the illness started. The participants also answered questions about smoking, self-reported health, CVD, asthma and chronic obstructive pulmonary disease (COPD), sunlight exposure, eating fish, and use of fish oil, n-3 (omega-3) and vitamin and/or mineral supplements. Height and weight were measured in all individuals.
Non-fasting blood samples were drawn from an antecubital vein at the first visit. Serum 25(OH)D concentration was measured using an electrochemiluminescence immunoassay on an automated clinical chemistry analyser (Modular E170; Roche Diagnostics GmbH, Mannheim, Germany)( Reference Jorde, Sneve and Hutchinson 23 ). The total analytical CV was 7·3 %. At the second visit, blood was also drawn for measurement of C-reactive protein (CRP) concentration( Reference Melbye, Amundsen and Brox 24 ).
Spirometry was performed using a SensorMedics Vmax Encore 20 spirometer, following American Thoracic Society/European Respiratory Society criteria( Reference Miller, Hankinson and Brusasco 25 ). Norwegian reference values were used( Reference Langhammer, Johnsen and Gulsvik 26 ).
Statistical analysis
The percentages of persons reporting symptoms of recent RTI were analysed in relation to the characteristics of the participants such as smoking habit, self-reported diseases, sun exposure, intake of fatty fish and vitamins, BMI, spirometry results and serum 25(OH)D concentration. Information about CRP concentration was also included in the analyses to increase the validity of the RTI questions.
The spirometry results were dichotomized, and the ratio between forced expiratory volume in 1 s (FEV1) and forced vital capacity (FVC) <0·7 was regarded as indicating bronchial obstruction. The FEV1:FVC ratio is used as a diagnostic criterion of COPD in the guidelines of the Global Initiative for Chronic Obstructive Lung Disease (GOLD)( 27 ).
The immunometric method used to measure serum 25(OH)D concentration yields systematically higher values in smokers than in non-smokers( Reference Grimnes, Almaas and Eggen 28 ). Serum 25(OH)D level varies by season. Because the serum 25(OH)D threshold needed for an adequate immune response is not known, we divided serum 25(OH)D concentrations into four quartiles and adjusted these data for current smoking status and month of participation by allocating smokers and non-smokers into quartiles for each month.
The main outcome measure was recent RTI symptoms. Patient characteristics, sun exposure, intake of fatty fish and vitamins, BMI, lung function and pre-questionnaire serum 25(OH)D concentration were analysed as possible predictors of RTI. The serum 25(OH)D quartile was used as a secondary outcome with the same explanatory variables.
Three sensitivity analyses were performed. Because the time difference between the first and second visit varied considerably, we narrowed the analyses to participants who attended the second visit within 28 d after the first visit. Recent RTI symptoms are associated with increased CRP values( Reference Melbye, Amundsen and Brox 24 ), and the variation in the prevalence of RTI symptoms supported by a CRP level ≥5 mg/l was analysed. In the third sensitivity analysis, smokers and non-smokers were analysed separately, using 25(OH)D quartiles adjusted only for the month of attendance.
A two-sided Pearson χ 2 test was used for dichotomous variables. Tests for linear trends of frequencies were performed using the Wald χ 2 test. The statistical software package SPSS 19·0·0 for Windows was used in the statistical analyses. A P value <0·05 was considered significant. The Tromsø Study complies with the Declaration of Helsinki, and each individual gave written informed consent prior to participation. The Regional Committee of Medical and Health Research Ethics approved the study.
Results
A total of 6350 persons, 86·9 % of those who attended the second examination, provided a serum 25(OH)D measurement and answered the main question ‘Have you had symptoms of the common cold, acute bronchitis, or other airway infection in the last 7 days?’, and were thus included in the study. The mean age was 63·7 years, 56·9 % were women and the average BMI was 27·1 kg/m2. Of the 6350 individuals, 791 (12·5 %) answered ‘yes’ to the main question. Characteristics of the participants are presented in Table 1.
Table 1 Characteristics, including intake of fish and dietary supplements, of 6350 middle-aged and elderly participants in the Tromsø Study 6, Norway (October 2007 to December 2008)

Current smokers had 20–25 % higher serum 25(OH)D concentrations. A similar pattern of seasonal variation in serum 25(OH)D concentration was found among smokers and non-smokers (Fig. 1).
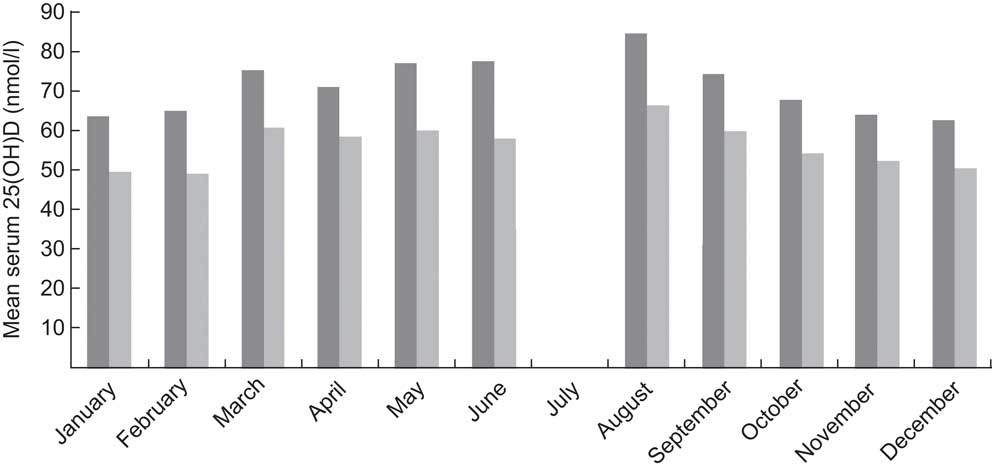
Fig. 1 Seasonal variation in serum 25-hydroxyvitamin D (25(OH)D) concentration according to smoking status (![]() , smokers;
, smokers; ![]() , non-smokers) among 6350 middle-aged and elderly participants in the Tromsø Study 6, Norway (October 2007 to December 2008, with a break in July 2008)
, non-smokers) among 6350 middle-aged and elderly participants in the Tromsø Study 6, Norway (October 2007 to December 2008, with a break in July 2008)
There was no significant association between the prevalence of RTI symptoms and reduced serum 25(OH)D concentration (Table 2). The prevalence of RTI symptoms was highest in quartile 3 (15·0 %), followed by quartile 4 (12·4 %), and lowest in quartiles 1 and 2 (11·1 % and 11·4 %, respectively). This yielded a significant linear-by-linear association (P = 0·042) between increasing serum 25(OH)D level and recent RTI symptoms. This relationship was strongest in women, participants with good or excellent self-rated health, those without COPD according to the GOLD criteria and those with a BMI of <30·0 kg/m2 (Table 2).
Table 2 Frequency of recent symptoms of RTI (n 791) analysed by quartile of serum 25(OH)D concentration and patient characteristics, adjusted for smoking and date of attendance, among 6350 middle-aged and elderly participants in the Tromsø Study 6, Norway (October 2007 to December 2008)

RTI, respiratory tract infection; 25(OH)D, 25-hydroxyvitamin D; FEV1, forced expiratory volume in 1 s; FVC, forced vital capacity.
*Linear-by-linear association: P = 0·042.
†Linear-by-linear association: P = 0·004.
‡Linear-by-linear association: P = 0·008.
§Linear-by-linear association: P = 0·011.
||Linear-by-linear association: P = 0·022.
The participants who answered ‘yes’ to the main question were also asked how many days had passed since the symptoms started. The average was 14·2 d, but there was no trend for increasing duration of illness according to serum 25(OH)D concentration (Fig. 2).
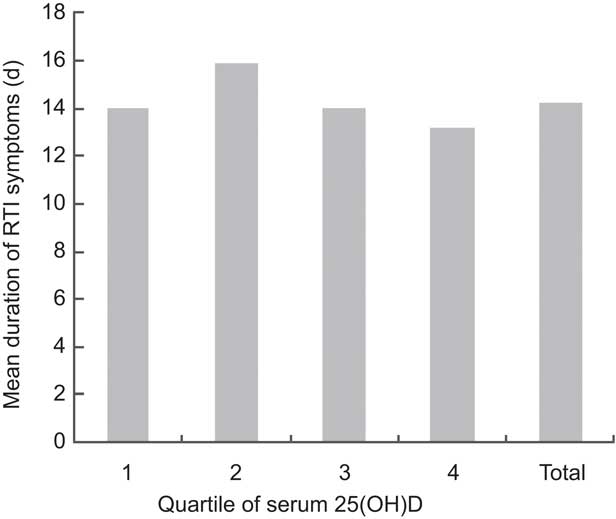
Fig. 2 Mean duration of symptoms of respiratory tract infection (RTI) according to quartile of serum 25-hydroxyvitamin D (25(OH)D) concentration and in total among 6350 middle-aged and elderly participants in the Tromsø Study 6, Norway (October 2007 to December 2008)
There were no associations between the prevalence of RTI symptoms and the frequency of eating lean fish, fatty fish or cod liver and roe, or use of n-3 capsules or vitamin and/or mineral supplements. Of those who reported taking cod-liver oil or fish oil capsules daily or sometimes, 10·9 % and 10·3 %, respectively, reported RTI symptoms in the previous 7 d compared with 12·9 % of those not taking cod-liver oil or fish oil capsules (P = 0·04; Table 3). There was no association between sun exposure and RTI symptoms (Table 3).
Table 3 Frequency of serum 25(OH)D concentration in the lowest quartile and of RTI symptoms according to dietary factors and sun exposure among 6350 middle-aged and elderly participants in the Tromsø Study 6, Norway (October 2007 to December 2008)

25(OH)D, 25-hydroxyvitamin D; RTI, respiratory tract infection.
*χ 2 test for linear trend: P < 0·001.
†χ 2 test: P = 0·007.
‡χ 2 test for linear trend: P = 0·030.
A significantly lower frequency of 25(OH)D concentration within the lowest quartile was found by higher intake of fatty fish, cod liver and roe, capsules of cod-liver oil or fish oil, and vitamin and/or mineral supplements (Table 3).
Sensitivity analyses
Non-fasting blood samples were drawn at the first visit and the participants answered the main question on RTI symptoms at the second visit. There was variability in the time difference between the first and second visit; e.g. for 37·7 % of participants the time difference was 4–8 weeks, and for 17·4 % it was ≥8 weeks. We thus narrowed the analyses to participants with a time difference <28 d. This included 2850 (44·9 %) of the participants. The main result was unchanged. That is, there was still no significant association between the prevalence of RTI symptoms and reduced serum 25(OH)D concentration, and the highest frequency of RTI symptoms was found in the third quartile (Table 4).
Table 4 Sensitivity analyses: frequency of RTI symptoms in the previous week in subgroups and of RTI symptoms in combination with elevated CRP level by quartile of serum 25(OH)D concentration among 6350 middle-aged and elderly participants in the Tromsø Study 6, Norway (October 2007 to December 2008)
RTI, respiratory tract infection; 25(OH)D, 25-hydroxyvitamin D; CRP, C-reactive protein.
Among the 791 participants reporting RTI symptoms, 167 (2·6 % of the total study sample) also had a CRP value of ≥5 mg/l. The frequency of RTI symptoms in combination with CRP ≥5 mg/l in the four vitamin D quartiles showed the same pattern of distribution as for RTI symptoms alone (Table 4).
Of 5113 non-smokers and 1147 smokers, 569 (11·1 %) and 212 (18·5 %) respectively reported RTI symptoms (Table 2). Analysis of the serum 25(OH)D quartiles, adjusted only for month of participation, produced no significant association between serum 25(OH)D concentration and RTI symptoms among either non-smokers or smokers. However, there was an unexpected association between increasing serum 25(OH)D and RTI symptoms only in smokers with COPD, the group with good or excellent self-reported health and those with BMI < 30·0 kg/m2 (P = 0·020, 0·017 and 0·045, respectively).
Discussion
In the present large population-based study, we could not confirm an association between vitamin D level and recent RTI reported by Ginde et al. ( Reference Ginde, Mansbach and Camargo 2 ) and Berry et al.( Reference Berry, Hesketh and Power 19 ). Serum 25(OH)D concentration was not inversely associated with recent RTI symptoms. This finding seemed to be robust after controlling for date of attendance and smoking habit.
Laaksi et al.( Reference Laaksi, Ruohola and Tuohimaa 18 ) found that people with a serum 25(OH)D concentration <40 nmol/l had significantly more days of absence from work because of respiratory infection. We found no association between serum 25(OH)D level and duration of RTI symptoms.
The findings are consistent with the results from an intervention study by Jorde et al.( Reference Jorde, Witham and Janssens 29 ), which concluded that the role of vitamin D in the prevention of influenza and upper respiratory infections remains unresolved.
A strength of our study is that it was a population-based survey with a high attendance rate that included information on recent symptoms obtained directly from the participants. Serum 25(OH)D concentrations were measured before the RTI symptoms were recorded and hence were not a consequence of infection. Another strength is that we measured CRP concentration to confirm that an RTI had occurred( Reference Melbye, Amundsen and Brox 24 ). A limitation of our study is the time difference between the blood sample obtained to measure vitamin D level and the questionnaire. 25(OH)D, the major circulating form of vitamin D, has a half-life of about 2 weeks in the blood( Reference Holick 30 ) and we assumed that the serum 25(OH)D level is stable in most of the participants because of the relatively consistent intake of vitamin D and sun exposure. We reanalysed the data by including only those data for participants with <4 weeks difference between the time of blood sample and questionnaire and found the same results.
We also adjusted for current smoking status. When smokers and non-smokers were analysed separately, we found no associations between decreasing levels of vitamin D and RTI symptoms. We found a significantly higher vitamin D level in participants with a high intake of lean fish, fatty fish, cod liver and roe, and in those who took cod-liver oil, fish oil capsules or vitamin and/or mineral supplements, as one might expect( Reference Calvo, Whiting and Barton 10 ). Only use of cod-liver oil or fish oil capsules daily or sometimes was significantly associated with fewer RTI during the previous 7 d. However, the difference between users and non-users of cod-liver oil or fish oil capsules was small and may have occurred by chance. If the difference is real, we cannot conclude that this is related to an effect on the serum 25(OH)D concentration. It is possible that regular ingestion of cod-liver oil, a strong tradition as a preventive measure against RTI in Norway, may be related to an unknown factor.
In conclusion, low serum 25(OH)D concentration was not associated with recent RTI symptoms. Our findings do not indicate that vitamin D supplementation reduces the incidence of RTI in Norway.
Acknowledgements
Sources of funding: The study was partly supported by the Norwegian Committee on Research in General Practice. Conflicts of interest: There are no conflicts of interest. Authors’ contributions: H.M. planned the study; all three authors participated in analyses and writing of the paper.








