Background
Health promotion for older people is an important policy objective because the number of older people across the European Union is growing and this will put considerable strain on existing medical and social care systems (Robine et al., Reference Robine, Michel and Herrmann2007), (Tonks, Reference Tonks2000). In England promotion of health and prevention of functional impairment in later life are major health and social care policy priorities with defined standards explicitly elaborated in England within the National Service Framework for Older People (Department of Health, 2001). Commissioners and providers of social care services, amongst others, have begun to consider systems of effective delivery that connect older people with information, advice and services (Commission for Social Care Inspection, 2008); enhance their potential for self-assessment and self management (Department of Health, 2007) and enable service providers and commissioners to anticipate future needs (Wanless et al., Reference Wanless, Forder, Fernàndez, Poole, Beesley, Henwood and Moscone2006).
Whilst the policies are clear, the international evidence base for health promotion with older people through primary care is relatively weak. Although many older people perceive health promotion activities as beneficial, engage in healthy behaviours more frequently than younger adults, and participate in community-based and other health promotion programmes, there is little definitive evidence that health promotion activities result in better health outcomes (Heidrich, Reference Heidrich1998). For example, the evidence that primary care based exercise promotion for older people results in sustained levels of activity that are likely to have lasting health benefits rests on trials from one centre, in New Zealand (Lawton et al., Reference Lawton, Rose, Elley, Dowell, Fenton and Moyes2009). Hopes that secondary prevention of disability through case finding, comprehensive assessment and case management were undermined by the failure of the Medical Research Council’s trial of screening in the 75 and over population to show any benefit (Fletcher et al., Reference Fletcher, Price and Ng2004). Tertiary prevention of disablement in frailer older people by primary care nurses did show improvements in quality of life, but not in other outcomes like functional ability (Markle-Reid et al., Reference Markle-Reid2006).
The effectiveness of different approaches to preventative care remains a matter of debate (Stuck et al., Reference Stuck, Egger and Beck2004a). Strategies based on intensive case-management have only a limited impact. A recent large UK trial failed to show benefits of population-based multi-domain assessment of older people (Fletcher et al., Reference Fletcher, Price and Ng2004). Conversely, a more recent systematic review of community-based multi-factorial interventions in elderly people (a mean age of at least 65 years) living at home were identified for 89 trials involving 97 984 people, and concluded that complex interventions can help elderly people to live safely and independently, and could be tailored to meet individuals’ needs and preferences (Beswick et al., Reference Beswick, Rees, Dieppe, Ayis, Gooberman-Hill, Horwood and Ebrahim2008). This positive evidence gives grounds for optimism, but only refers to the containment of disability, not its primary or secondary prevention where behaviour change is essential if healthy older people are to avoid future lengthy disablement (Syme, Reference Syme2003).
An evidence-based, theoretical framework that provides definition and direction for health promotion practice may be the key to the task of promoting behaviour change in older people. When the health risk appraisal system was first developed specialists in health promotion favoured the transtheoretical model and the theory of planned behaviour (Enguidanos, Reference Enguidanos2001).
The transtheoretical model of behaviour change proposes progress through six stages of change: precontemplation, contemplation, preparation, action, maintenance and termination (Prochaska and DiClemente, Reference Prochaska and DiClemente1984). Basic research has generated a rule of thumb for at-risk populations: 40% in precontemplation, 40% in contemplation and 20% in preparation. Applied research has demonstrated dramatic improvements in recruitment, retention, and progress using stage-matched interventions and proactive recruitment procedures. The most promising outcomes to date are found with computer-based individualised and interactive interventions, with personalised counselling a promising enhancement to computer-based programmes. Tailoring interventions to an individual’s stage in the change process is most effective in promoting behaviour change (Burbank et al., Reference Burbank, Padula and Nigg2000).
A number of factors influence whether an individual will move from contemplating change to actually changing their behaviour. The theory of planned behaviour identifies attitudes to change, social pressure or subjective norms favouring change and perceived control over the behaviour. Control has two components: self-efficacy (dealing largely with the ease or difficulty of performing a behaviour) and controllability (the extent to which performance is up to the actor) (Azjen, Reference Azjen2006). This framework for understanding behaviour change allows health promotion interventions to be designed in ways that take into account the complexities of motivation. Prochaska and Velicer, (Reference Prochaska and Velicer1997) argue that ‘If results with stage-matched interventions continue to be replicated, health promotion programs will be able to produce unprecedented impacts on entire at-risk populations.’
In the UK this approach has been adopted, and an on-line ‘Life Check’ personal health and lifestyle risk assessment tool, linked to the provision of specific health and social care advice, is planned in the current phase of English health policy. (Department of Health, 2006). Although this approach to risk assessment does not yet focus on the older population, we do have some insights into how it might work with an ageing population from the extensive evaluation of health risk appraisal (HRA). This system was originally developed through an evidence-based process at the University of California, Los Angeles (Breslow et al., Reference Breslow, Beck, Morgenstern, Fielding, Moore, Carmel and Higa1997) and evaluated in Europe (Stuck et al., Reference Stuck, Elkuch, Dapp, Anders, Iliffe and Swift2002). HRA is a systematic approach to collecting information from individuals that identifies risk factors by questionnaire and provides individualised feedback. A systematic review of HRA in older people based on controlled studies showed potential benefits on behaviour (particularly exercise), physiological variables (particularly blood pressure and weight) and general health status in those studies that included personalised reinforcement (Rand, 2000).
The health risk appraisal for older (HRA-O) people system consists of a self-administered; questionnaire that is sent to patients registered with a general practitioner (GP), to identify risk factors for disability, ill-health and social isolation. The questionnaire is constructed from existing instruments validated for use with community-dwelling older people; full details of the derivation of the instruments have been published elsewhere (Stuck et al., Reference Stuck, Kharicha, Dapp, Anders, von Renteln Kruse, Meier-Baumgartner, Harari, Ivanova, Bachmann, Egger, Gilman, Higa, Beck, Swift and Iliffe2007). The domains included in the questionnaire are shown in Figure 1.
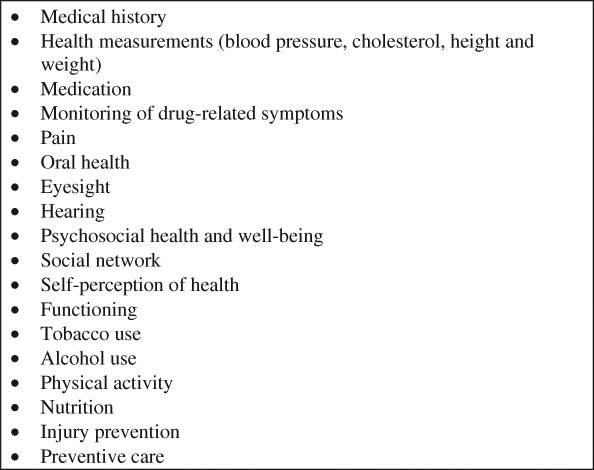
Figure 1 Domains of the health risk appraisal in older people questionnaire
Each individual’s answers to the questionnaire are entered by researchers into a computer decision support software package, which compares an individual’s responses with an evidence-based knowledge set to produce a series of recommendations for changes in behaviour.
A patient feedback report, based on the concepts of the transtheoretical model and the theory of planned behaviour, is then produced for the patient. This gives specific, personalised advice on changing any reported health risk behaviours, taking into account links between risk factors. Therefore, for example, dietary advice for a person with diabetes is different from that for a non-diabetic person. General evidence-based health promotion advice is also given on each risk factor and advice on social care and social networks where relevant. Prompts to seek advice from the primary care team are given if appropriate, along with details on how to get in touch with other sources of support and information (eg, details of national and local voluntary organisations). When an individual reports health-promoting behaviour he or she is congratulated and encouraged to maintain the behaviour.
The HRA for older people system is designed to work within primary care. The invitation to participate comes from the GP, and a summary of the feedback report is produced for the older person’s primary care team, so that reinforcement of health promotion advice can occur opportunistically. The process is designed to work as shown in Figure 2.
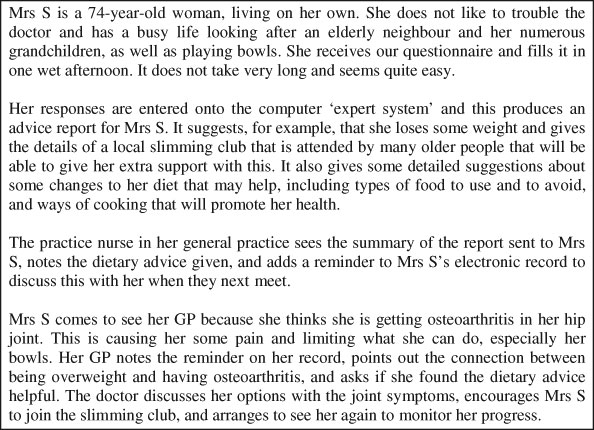
Figure 2 The health risk appraisal in older people system in clinical practice
We have previously published the feasibility and yield of an HRA system for older people (adapted for European use and titled HRA-O to distinguish it from its North American equivalent), and demonstrated high levels of acceptance amongst participants and primary care providers (Iliffe et al., Reference Iliffe, Kharicha, Harari, Swift and Stuck2005). However, the ‘unprecedented impact’ that Prochaska anticipated did not materialise in a randomised controlled trial of the HRA-O system in British general practice (Harari et al., Reference Harari, Iliffe, Kharicha, Egger, Gilmann, von Renteln Kruse, Beck, Swift and Stuck2008). The only benefits attributable to the intervention one year later were a statistically significant increase in the uptake of immunisation against pneumococcal pneumonia and a slight but equivocal effect on physical activity.
There are several possible contributory reasons for this observed lack of impact in the UK of the health risk appraisal system as a model for IT-driven health promotion in older people. These may have included 1) certain putative aspects of experimental design and analysis, 2) differential nuances in the national health service (NHS) delivery system compared with other settings (in particular less manpower-intensive professional reinforcement) and 3) limitations (in terms of elements of the transtheoretical model) of the HRA-O technology as currently presented. Given the current policy towards computerised self-assessment (Life Checks) it is important to understand these fully before significant investments in this technology are made.
We report here the findings of a subsequent study designed primarily to investigate the third of these factors. It is based on interviews and nominal groups with older people who completed the HRA-O questionnaire on at least two occasions and with the professionals in the same communities who provide services for older people.
Methods
The study took place in two primary care trusts/social services areas in north-west and south-east suburban London. Three primary care teams involved in the earlier testing of HRA-O agreed to participate in a further round of research and development. Ethics committee approval was obtained from Harrow ethics committee and Kings College ethics committee. Over 3000 primary care patients aged 65 and over from these practices had already received a personal report in response to the HRA-O questionnaire at least once since 2001. A further cycle of HRA-O mailing to them was carried out, to measure changes in health behaviour and risks. The practice team checked the appropriateness of asking this cohort to complete another questionnaire at this time point. Individuals were excluded if they had died, moved into nursing/residential care, moved away, were no longer registered at the practice or whose health status as judged by their GP had deteriorated sufficiently to justify their exclusion based on the original randomised controlled trial (RCT) criteria.
Eligible older people were posted the HRA-O with a letter from their GP, a consent form and information sheet about the study. Those that completed and returned the questionnaire were sent a personalised feedback report. No reminders were sent due to budgetary constraints. Older people were also invited either with a letter from their GP, or through a voluntary organisation with which they were involved, to take part in nominal groups to explore their perceptions of the value, usability and appropriateness of the information given to them through HRA-O. Nominal groups potentially powerful learning and development tools (Dockery, Reference Dockery1996) which have a particularly useful role in analysing health care problems (Van den Ven and Delbecq, Reference Van den Ven and Delbecq1972) and which can help to bridge the gap between researchers and practitioners (Carney et al., Reference Carney, McIntosh and Worth1996). A nominal group approach designed for ill-structured problems was chosen, to allow for disagreements over problem definition and for potential solutions that overlapped or varied widely in specificity. This required the groups to generate ideas, confirm that they were addressing the same problem, analyse the content of the ideas, categorise ideas and clarify the items in each category (Bartunek and Murningham, Reference Bartunek and Murningham1984). The nominal groups for older people were held in community centres or in a general practice, were facilitated by the same member of the research team and were observed by a non-participant researcher, who took detailed notes that could later be compared with the transcripts of tapes. No rewards were given for participation in the study and all groups (and interviewees) were asked to comment freely on all aspects of the HRA-O questionnaire, which they received in advance. No demographic information was collected from group participants and so we do not know how much the groups represented the diversity of the local population.
A map of local services and organisations in the two study areas was drawn up via information available on the Internet and local publications to start this consultation exercise. Purposive sampling was initially used to recruit local stakeholders to the consultation exercise. Older people, primary health and social care practitioners and managers, the voluntary sector and key individuals in the primary care trust, joint commissioning boards and local authority were invited to participate.
An initial contact (via letter or email) was made with heads of organisations or key individuals requesting a meeting or referral to an appropriate colleague. A study information sheet and copy of the HRA-O questionnaire were sent in advance. Participants were given the choice of feeding back their views by interview (face to face or telephone) or in a nominal group (held locally). Participants were asked to identify local individuals they thought should be included in the consultation exercise; i.e. purposive sampling was followed by opportunistic sampling (Murphy et al., Reference Murphy, Dingwall, Greatbatch, Parker and Watson1998). All stakeholders were asked for their views on the value, usability and appropriateness of the information given through the HRA-O system.
Interviews and nominal groups were tape-recorded and transcribed verbatim. Content analysis was used to identify key themes and issues in the transcripts. Broad categories were then developed, based both on themes related directly to questions asked in the interview schedule, as well as those that emerged during the analysis. Transcripts were read and analysed by three members of the project team (KK, SI and CG) who individually identified the main categories. The three other members of the project team then read all the transcripts. A consensus approach based on informed deliberation by experts about complex problems was used to finalise themes (Ryan et al., Reference Ryan, Scott, Reeves, Bate, van Teijlingen and Russell2001) following which categories were reviewed and finalised. Transcripts were analysed by study area. Emergent findings from the first study area informed data collection in second, both in terms of validation of themes as well as ensuring gaps in information were addressed.
Findings
The numbers and roles of people who participated in this study are shown in Table 1. Eight nominal groups were held, four with older people and four with professionals, together with 17 interviews with 20 people. In Table 1 all contacts are interviews unless otherwise stated. Older people identified positive and negative features in the HRA-O questionnaire and feedback report, some of which were shared by the professionals. There was, however, considerable divergence in perspective between professional views and those of older people.
Table 1 Participants in the HRA-O evaluation
HRA-O = health risk appraisal in older people; PCT = primary care trust.
The perspectives of older people
Older people, many of whom had completed the questionnaire over three successive annual waves, identified a number of positive aspects of the HRA-O system. The questionnaire and feedback report were seen as ‘clearly set out, well-worded and easy to follow, so user-friendly’. Many older people thought that the level of detail made them stop and think in detail about themselves, their health and lifestyle. Receipt of the invitation to complete the HRA-O questionnaire was seen as evidence that the GP was ‘taking my requirements seriously’.
The features of HRA-O system that concerned older people who had completed it were around its format, its purpose, the consequences of completing it, its generalisability and its overall usefulness.
The format of the responses was seen as a problem, a ‘tick box’ approach being more limiting than free text answers. The questions and their answer options were sometimes too ‘black and white’ and not able to pick up on the ‘grey areas’ of health and wellbeing. As a consequence, the individual’s response could be the best available match rather than a nuanced reflection of health status, and this might have a detrimental effect on the feedback, which may miss the point.
A clear explanation of purpose of questionnaire was needed, they suggested, to encourage completion. There was some confusion about the use of the data; was it primarily for the benefit of the older person, for their GP (to know more about them) or for the government (to know about the population)?
Completion of the HRA-O questionnaire was seen as being dependant on the honesty of the older person’s responses, operating in two ways. For example, defensiveness and fear of authority may influence the responses given (eg, about finances, or alcohol consumption). On the other hand, some older people had felt obliged to get recent cholesterol and blood pressure data, in order to complete the questionnaire accurately. This added to the time taken to answer the questionnaire, which was often completed over several days.
HRA-O captures a snapshot of the person, and older people stressed how quickly an individual’s circumstances can change, asking how useful a snapshot is, given the potential for rapid obsolescence. Similarly, some processes of change can be slow, but in variable ways. For example, bereavement can be a complex and prolonged process for some but not others. Social and family relationships can be equally complex and changeable, sometimes making a description of a social network of limited value.
Perhaps the most telling perspective was that, overall, the feedback from the HRA-O questionnaire (although very detailed) often did not provide new knowledge: ‘It told me nothing that I did not know already’.
Professional perspectives
Overall professionals across different disciplines considered that the HRA-O system appeared comprehensive and its domains were relevant to the health and well being of older people. It included questions not asked in other assessment forms, obtained new information useful to professionals (well-being, social network) and could help to provide evidence to challenge some of the myths about older people and their needs. Many saw that it could be useful for long-term conditions, and was person-centred, allowing them for self-assessment. Most assessments are carried out at times of crisis or need for intervention, they noted, but HRA-O fits the prevention agenda.
The negative perceptions from professionals centred on the complexity of the questionnaire and feedback report, the responses that professionals would make to the information, the need for reinforcement of the advice given and the problem of compatibility of information systems.
The length of questionnaire was seen as a problem, derived from the belief that older people dislike filling in forms. There was a need to balance information gathering against the risk of overloading people. ‘HRA-O may be too much for older people’. Older people may not understand their medical history clearly enough to report it accurately (ie) ‘mind-boggling for an older person’. It was assumed that older person would require a certain amount of confidence to complete the questionnaire, which could be anxiety provoking because of the fear of making mistakes and of the implications of such mistakes. For them it would be easier to say ‘No’ to the opening question in each domain than to complete all the subsequent questions. A group of social workers debated ‘Who would complete this?’ and answered that ‘It’s for nice little old ladies’.
Professionals asked about the uses of the information, but in a different way to the older people, because they were concerned about balancing enquiries about needs and wants with what services could deliver. ‘What would happen if a person really answered those questions in a way that would cause concern?’
Reinforcement of motivation was seen as essential to make change come about, because, in the thinking of the professionals, health risk behaviour was socially determined (ie, not determined by knowledge or information). As a result older people may have different definitions of healthiness (particularly with reference to diet and exercise).
Sharing of information with other professionals was seen as key to producing benefits for older people. ‘Unless this is shared, it is not worth the paper it is written on’. Practitioners were not always discriminating about what information would be useful to them – ‘Any information is good information’ – but were equally sure that data from the HRA-O must fit with assessment tools and IT systems already in use.
Discussion
This study has identified several important factors that may partly explain the limited observed impact of HRA-O in the British NHS setting. The positive attributes of HRA-O were that it was comprehensive and relevant, obtained new information useful to professionals, was person-centred and allowed self-assessment, fitted the prevention agenda, was clearly set out, well-worded and easy to follow, and was user-friendly for its target population. Its negative features were its length and the time taken to complete the questionnaire. The discussion about these attributes challenged some underlying assumptions about the approach taken to health promotion, highlighted some potentially important modifications, and emphasised the need for policy caution in introducing interventions (such as ‘Life Checks’) based on similar premises. The conclusions that we draw from the study refer to necessary refinements of the HRA-O technology, the necessity of greater insight into the social psychology of ageing, and the necessary and appropriate involvement of professionals in reinforcing health promotion advice.
1) Necessary refinement of technologies. Although the older people participating in this study appreciated the HRA-O questionnaire as evidence of attentiveness to their health and wellbeing, they were unsure of its purpose and sometimes uncertain how to respond to it. The snapshot of the individual generated by the HRA-O questionnaire was a fuzzy one, lacking the detail of an accurate portrait of a dynamic self. Crucially, with the exception of the most basic lifestyle factors, the HRA-O system did not start out by ascertaining what they already knew about improving their health, and what decisions they had already made about doing so, but assumed that providing knowledge of alternative ways of living would prompt changes in behaviour in those contemplating change. This is open to criticism as a scattergun approach for changing behaviour, rather than a truly personalised one, because the advice given is tailored only to the individual’s responses, not to their intentions, which were not elicited.
2) Necessary insight into the social psychology of ageing. Two attributes of older people appear to be important in promoting or inhibiting behaviour change: attitudes to ageing and motivation. Individuals with more positive self-perceptions of ageing tend to practice more preventive health behaviours after controlling for age, education, functional health, gender, self-rated health and race (Levy and Myers, Reference Levy and Myers2004). Addressing views about ageing rather than knowledge could help to improve the efforts to increase the preventive health behaviours in the older population.
Motivation appears to be the key to changing behaviour, but the findings of studies in motivation are paradoxical. In one US study ‘intrinsically’ motivated older persons (those who motivated themselves) attended fewer health promotion programmes than those who were more extrinsically motivated (ie, motivated by others) (Loeb et al., Reference Loeb, O’Neill and Gueldner2001). Having a higher educational level and fewer health problems emerged as significant predictor variables for intrinsic health motivation. Those with less formal education attended more health promotion programmes. This is relevant to our studies of the HRA-O system in two respects. Those who participated in nominal groups about the HRA-O system after completing the questionnaires on at least two occasions may well have been more educated and less unwell than those who did not take part in the evaluation. Also, repeated completion of the HRA-O questionnaire (defined as three completions over four years) is associated with higher levels of education, younger age and fewer chronic diseases (Kharicha et al., Reference Kharicha, Iliffe, Harari, Swift, Gilman and Stuck2007). In other words, those most likely to take up the HRA-O approach may also be those least likely to utilise its recommendations.
3) Necessary and appropriate involvement of professionals in reinforcement. The professionals focused on their own concerns (about being able to meet newly revealed need, or having information in formats consistent with their data systems) as much as on the potential benefits of the HRA-O system to older people. Their exposure to older people with substantial needs was reflected in their perceptions of the HRA-O questionnaire being too burdensome for older people and only suited to ‘nice little old ladies’. This ‘pathological gaze’ contrasts with the high levels of response to the HRA-O questionnaire from relatively well community-dwelling older people, from 88% at the first completion to just over 60% at the third.
The professionals were perceptive about the need for social reinforcement of the advice given by the HRA-O system. Motivating change in older people appears to require face-to-face encounters to be effective. A systematic review of qualitative and quantitative studies and reviews that focussed on older people’s views and experiences of falls prevention programmes (McInnes and Askie, Reference McInnes and Askie2004) illustrates this. The review found preferences (among some groups of older people) for falls prevention strategies that did not involve behaviour change, a need to promote the social benefits of falls prevention programmes, and the importance of identifying and addressing factors associated with activity avoidance. The authors concluded that although trials of multi-factorial falls prevention packages have reported beneficial results, in clinical practice it is important to consult with individual potential participants and find out what characteristics they are willing to modify, and what changes they are prepared to make to reduce their risk of falling. Otherwise, there is the risk that expensive programmes are not properly targeted or fail to achieve maximum participation rates.
Social settings may be more appropriate to health promotion for older people than the computerised and interactive environment proposed by Prochaska and colleagues. For example, two trials in US senior centres appeared to affect health status positively, with improved physical and psychosocial functioning (Wallace et al., Reference Wallace, Buchner, Grothaus, Leveille, Tyll, LaCroix and Wagner1998), and a reduction in disability risk factors, improvement in health status, no decrements in functional status and no increase in self-reported healthcare use, respectively (Phelan et al., Reference Phelan, Williams, Leveille, Snyder, Wagner and LoGerfo2002).
Reinforcement of health promotion advice for older people through primary care is an alternative strategy that we believe is worth exploring, but the findings of this study suggest that a computerised and interactive health promotion environment is not likely to be a powerful engine for primary and secondary prevention of disability in older people, without such supplementation. There is some evidence from the Swiss arm of the ProAge trial that intervention by nurses to reinforce the advice given did modify health risk behaviour (Stuck et al., Reference Stuck, Swift, Gillmann, Iliffe, Kruse, Beck and Egger2004b). This needs to be tested in different settings.
Acknowledgements
We thank all those who completed the HRA-O questionnaire or participated in groups or interviews.
Funding source
Department of Health Modernising Adult Social Care (MASC) programme.





