High blood pressure (BP) is a major independent risk factor for CVD( Reference Lim, Vos and Flaxman 1 ). Meta-analyses of prospective cohort studies have shown that higher intake of total dietary fibre is associated with a lower risk of fatal and non-fatal coronary events( Reference Chen, Lv and Pang 2 , Reference Pereira, O’Reilly and Augustsson 3 ). Reported cross-sectional findings of total fibre intake and BP, however, were inconsistent: some showed inverse associations( Reference Ascherio 4 – Reference Stamler, Caggiula and Grandits 6 ), whereas others observed no association( Reference He, Klag and Whelton 7 , Reference Masala, Bendinelli and Versari 8 ). The limited available prospective cohort studies found inverse relations between total fibre intake and BP rise( Reference Ludwig, Pereira and Kroenke 9 ), or risk of hypertension( Reference Ascherio 4 , Reference Ascherio, Hennekens and Willett 5 ). Methodological limitations of these studies include validity of dietary assessment methods( Reference Ascherio 4 – Reference Stamler, Caggiula and Grandits 6 , Reference Masala, Bendinelli and Versari 8 ), absent or limited adjustment for dietary and other lifestyle confounders( Reference Stamler, Caggiula and Grandits 6 , Reference Masala, Bendinelli and Versari 8 , Reference Elliott, Fehily and Sweetnam 10 ), substitution of fibre supplements rather than dietary fibre sources( Reference Streppel, Arends and Van't Veer 11 , Reference Whelton, Hyre and Pedersen 12 ) and inadequate frequency of BP measurement( Reference Stamler, Caggiula and Grandits 6 – Reference Masala, Bendinelli and Versari 8 ). Meta-analyses of randomised controlled intervention studies showed that fibre supplementation (average dose, 11·5 g/d) did not significantly reduce BP( Reference Streppel, Arends and Van't Veer 11 , Reference Whelton, Hyre and Pedersen 12 ), but significant BP-lowering effects were found in hypertensive participants( Reference Whelton, Hyre and Pedersen 12 ). It has been suggested that the mechanism by which higher dietary fibre intakes may lower BP is attributed to enhanced insulin sensitivity that may improve endothelial function and other CVD risk factors( Reference Streppel, Arends and Van't Veer 11 ). The potential effect of insoluble fibre on BP has been less thoroughly investigated. Soluble fibre may have a favourable effect on BP by lowering postprandial glucose responses and LDL-cholesterol levels, stimulating the absorption of minerals in the gastrointestinal system, and reducing body weight( Reference Streppel, Arends and Van't Veer 11 , Reference Whelton, Hyre and Pedersen 12 ). Inconsistent findings on the effect of dietary fibre on BP may relate to differences in study design( Reference Birketvedt, Aaseth and Florholmen 13 – Reference Swain, Rouse and Curley 17 ): BP responses to fibre intake may depend on type (insoluble or soluble) or dose of fibre, and whether supplemental fibre or high-fibre dietary sources were consumed (e.g. whole-grain bread)( Reference Streppel, Arends and Van't Veer 11 ). To our knowledge, only one study examined cross-sectional associations between types of fibre and CVD risk factors. The results showed significant lower risks of hypertension for total and insoluble fibre intakes, but not for soluble fibre intake( Reference Lairon, Arnault and Bertrais 18 ).
In the present study, we investigated cross-sectional relations to systolic blood pressure (SBP) and diastolic blood pressure (DBP) of total dietary fibre and its components among the 2195 participants of the INTERMAP study in the USA, using high-quality dietary data from four multipass 24 h dietary recalls, eight BP measurements and regression models adjusted extensively for dietary and lifestyle factors.
Methods
Population
The INTERnational study on MAcro/micronutrients and blood Pressure (INTERMAP) included 4680 men and women aged between 40 and 59 years. Participants were randomly recruited from community and workforce populations (seventeen population samples) in Japan, the People’s Republic of China, the UK and the USA( Reference Stamler, Elliott and Dennis 19 ). Between 1996 and 1999, participants attended four clinic visits, two on consecutive days and two on consecutive days approximately 3 weeks later. Dietary and non-dietary data collection underwent extensive quality control, including national and international checks to ensure completeness and accuracy. This study was approved by institutional ethics committees at all sites. Each participant consented in writing.
Information on types of fibre (insoluble, soluble) is only available for the US samples; therefore, we analysed data on 2195 participants (1103 men and 1092 women) from eight US population samples. Of 2281 US participants initially surveyed, individuals were excluded when they did not attend all four visits or had incomplete/missing data, presented unreliable dietary data, or unavailable 24 h urine samples (n 65) or had extreme total energy intake from any 24 h recall of <2092 kJ/d (<500 kcal/d) or >20 920 kJ/d (>5000 kcal/d) for women and <2092 kJ/d (<500 kcal/d) or >33 472 kJ/d (>8000 kcal/d) for men (n 21).
Clinic visits
Visits were randomly spread over the year. On each of the four visits, BP was measured twice and 24 h dietary recalls were performed once. Two-timed 24 h urine collections were obtained on the second and fourth visits. Height and body weight were measured twice on the first and third visits. On the first visit, a health history questionnaire was completed to collect information on medical history, medication intake, smoking and physical activity. On each of the four visits, participants provided information on their vitamin and supplement intakes.
Dietary assessment
Four 24 h dietary recalls were collected from each participant using a standardised multipass method reported in detail elsewhere( Reference Dennis, Stamler and Buzzard 20 ). In brief, trained interviewers collected in-depth data on all foods, beverages and supplements consumed in the past 24 h in face-to-face interviews. In the USA, dietary data were transferred to software (the Nutrition Data System (NDS), Nutrition Coordinating Centre (NCC), version 2.91, University of Minnesota) for on-screen coding during an interview( Reference Dennis, Stamler and Buzzard 20 ). Daily nutrient intakes were obtained using the NDS for research, version 4.01( Reference Dennis, Stamler and Buzzard 20 , Reference Schakel, Dennis and Wold 21 ). For quality control assessment, dietary recall data were compared with urinary excretion data. Pearson’s partial correlation coefficients adjusted for sample and sex between dietary and urinary total protein, Na and K were 0·52, 0·46 and 0·58, respectively( Reference Dennis, Stamler and Buzzard 20 ).
According to the NCC, insoluble dietary fibre includes cellulose, non-cellulose insoluble polysaccharides (mostly hemicellulose), lignin and some resistant starch. Soluble dietary fibre includes pectins, gums, muscilages and non-cellulose soluble polysaccharides (some hemicelluloses). We identified all sources of dietary fibre reported by participants: whole grains (bread and bread products, brown rice and pasta), refined grains (bread and bread products, pasta and rice), cereal products (ready-to-eat cereal, cooked cereal and granola bars), legumes, vegetables (cooked and raw vegetables), raw fruits, dried fruits, nuts and seeds.
The reliability of fibre intake for individuals was estimated using the following formula: 1/[1+(ratio/2)]×100. The ratio is intra-individual variance divided by the inter-individual variance, estimated separately by gender, and combined. The averages of the first two and second two visits were used to account for higher correlation between dietary intakes on consecutive days. This gives an indication of the effect of random error (day-to-day variability) on the associations with BP( Reference Dyer, Shipley and Elliott 22 ).
Measurement of blood pressure
SBP and DBP were measured by trained staff using a random-zero sphygmomanometer. Participants refrained from food, drinks, smoking and physical activity for 30 min. They were seated in a quiet room for at least 5 min, their bladders were emptied and their feet were placed flat on the floor. BP was measured twice on the right arm at each of the four clinic visits, using first and fifth Korotkoff sounds, totalling eight BP readings.
Other variables
During two visits, weight and height measurements without shoes or heavy clothing were collected four times and the BMI (kg/m2) was calculated. Urinary Na, Mg, Ca and K levels were measured from two-timed 24 h urinary samples collected between consecutive visits. Data on lifestyle factors were assessed using interviewer-guided questionnaires on smoking, education, hours of physical activity, adherence to a weight-reduction diet, use of antihypertensive and lipid-lowering drugs, individual and family history of CVD and diabetes mellitus and daily alcohol intake during the past 7 d.
Statistical methods
Statistical analyses were conducted using SAS software version 9.3 (SAS Institute Inc.). Dietary data were energy-adjusted using the nutrient density method. Dietary intake was estimated as a mean of the four dietary recalls. The mean value of eight BP measurements was used in the analysis. Urinary data were averaged across the two 24 h urinary collections( Reference Willett, Howe and Kushi 23 ). Isoenergitic models were adjusted for total protein, fat and sugar (% energy) to enable assessment of the independent relation of fibre intake (g/4184 kJ (g/1000 kcal)) with BP, including control for total energy intake( Reference Willett, Howe and Kushi 23 ).
Baseline characteristics of US participants and P trend across quartiles of total fibre intake were calculated using a generalised linear model adjusted for age, sex, total energy intake (kJ/24 h (kcal/24 h)), total protein (% energy), total fat (% energy) and population sample.
Multivariable linear regression analyses were used to examine associations between total, insoluble and soluble fibre (per2 sd 6·8, 4·6, and 2·2 g/4184 kJ (2·2 g/1000 kcal), respectively) and BP, including the total US cohort (n 2195). In addition, we also applied linear regression analyses in a sub-cohort, excluding participants with hypertension and use of antihypertensive drugs (n 1477). Three models were used, adjusted extensively for lifestyle and dietary factors, with and without adjustment for BMI. Potential confounders of the association of fibre intake with BP were selected from the literature. Model 1 was adjusted for age (years), sex (male or female), total energy intake (kJ/24 h (kcal/24 h)), total protein (% energy), total fat (% energy) and population sample (i.e. centre). Model 2 was adjusted for variables in model 1 plus adherence to a special diet (yes or no), physical activity during leisure time (a lot, moderate, little or none), dietary supplement use (yes or no), smoking (never, former or current), years of education (years completed), alcohol intake (g/24 h), history of CVD or diabetes mellitus (yes or no), family history of CVD (yes or no). Model 3 was fully adjusted, including variables in model 2 plus 24 h urinary excretion of Na (mmol/24 h). In addition, we sequentially investigated the influence of nutrients strongly related to fibre intake on the association, including 24 h urinary excretion (mmol/24 h) of Mg, Ca and K (mmol/24 h). No missing values were observed.
Analyses were repeated for two sub-cohorts with characteristics that may bias relationships between fibre intake and BP Reference Lim, Vos and Flaxman : a sub-cohort of non-hypertensive participants (n 1421) additionally excluding participants with elevated SBP (≥140 mmHg) or DBP (≥90 mmHg) Reference Chen, Lv and Pang ; and a sub-cohort free of major chronic diseases (n 1262) additionally excluding those diagnosed with CVD or diabetes.
Interactions by age and sex were examined by inclusion of separate terms in each regression model; there was no evidence for interaction. Two-tailed probability values (P<0·05) were considered statistically significant.
Results
Descriptive statistics
Across quartiles of total fibre intake, participants in the highest quartile of total fibre intake were older, had more years of education, had greater intakes of total protein, vegetables, raw fruits and dried fruits, had lower levels of BMI and BP and lower intakes of alcohol, total sugar, total fat and refined grains compared with those in the lowest quartile (Table 1). The predominant dietary source of total and insoluble fibre was raw fruits (54 and 57 %), followed by refined grains (16 and 14 %), vegetables (15 and 12 %) and whole-grain cereal products (12 and 13 %). For soluble fibre, dietary sources were raw fruits (48 %), vegetables (21 %), refined grains (19 %) and whole grains and cereal products (9 %). The reliability estimate for total fibre intake (g/d) was 82 % overall, 80 % in men and 83 % in women.
Table 1 Baseline characteristics of US INTERMAP participants by quartiles of total fibre intake (Mean values with their standard errors; percentages; n 2195)Footnote *

BP, blood pressure.
* The generalised linear model was adjusted for age, sex, total energy (kJ/24 h (kcal/24 h)), total protein (% energy), total fat (% energy), total sugar (% energy) and population sample.
Associations of total fibre with blood pressure
After adjustment for lifestyle factors and BMI, total dietary fibre intake higher by 2sd (6·8 g/4184 kJ (6·8 g/1000 kcal)) was associated with a SBP lower by 1·69 mmHg (95 % CI −2·97, −0·41) (Table 2). Additional adjustment for urinary K excretion attenuated this association and did not remain statistically significant (−1·01 mmHg; 95 % CI −2·35, 0·34).
Table 2 Estimated mean difference in blood pressure associated with 2 sd higher intakes of total fibre, insoluble fibre and soluble fibre in US INTERMAP participants (Mean differences and 95 % confidence intervals; n 2195)Footnote *

DBP, diastolic blood pressure; SBP, systolic blood pressure.
* 2 sd fibres (g/4184 kJ (g/1000 kcal)) total fibre (6·8); insoluble fibre (4·6); soluble fibre (2·2). Model 1 was adjusted for age, gender, total energy (kJ/24 h (kcal/24 h)), total protein (% energy), total fat (% energy), total sugar (% energy) and population sample. Model 2 was adjusted as model 1 variables plus adherence to energy-restricted diet, smoking, alcohol intake (g/24 h), hours engaged in moderate and heavy physical activity, dietary supplement use, educational level, CVD or diabetes diagnosis and family history of high blood pressure. Model 3 was adjusted as model 2 plus urinary Na (mmol/24 h). Model 4 was adjusted as model 3 plus urinary Mg (mmol/24 h). Model 5 was adjusted as model 3 plus urinary calcium (mmol/24 h). Model 6 was adjusted as model 3 plus urinary K (mmol/24 h).
† Additionally adjusted for soluble fibre (g/4184 kJ (g/1000 kcal)).
‡ Additionally adjusted for insoluble fibre (g/4184 kJ (g/1000 kcal)).
Associations of types of fibre with blood pressure
Insoluble fibre intake higher by 2sd (4·6 g/4184 kJ (4·6 g/1000 kcal)) was associated with a 2·07 mmHg lower SBP (95 % CI −3·92, −0·23), after adjustment for lifestyle factors, BMI and soluble fibre (Table 2). Adjustment for urinary K attenuated the association and did not remain statistically significant (−1·81 mmHg; 95 % CI −3·65, 0·04). Insoluble fibre intake was also inversely associated with DBP (−1·32 mmHg; 95 % CI −2·60, −0·04); this association was also attenuated with adjustment for urinary Mg (−1·23 mmHg; 95 % CI −2·51, 0·06). Soluble fibre intake was not associated with SBP or DBP.
Associations of fibre intakes with blood pressure, excluding participants with hypertension and use of antihypertensive drugs
We repeated the regression analyses in a cohort, excluding participants with hypertension and use of antihypertensive drugs (Table 3). The results showed that total dietary fibre intake higher by 2sd (6·9 g/4184 kJ (6·9 g/1000 kcal)) was associated with a SBP lower by 1·85 mmHg (95 % CI −3·13, −0·57). The inverse association between total fibre intake and SBP was independent of urinary K excretion (−1·69 mmHg; 95 % CI −3·04, −0·34).
Table 3 Estimated mean difference in blood pressure associated with 2 sd higher intakes of total fibre, insoluble fibre and soluble fibre in US INTERMAP participants, excluding those with hypertension and users of antihypertensive drugs (Mean differences and 95 % confidence intervals; n 1477)Footnote *
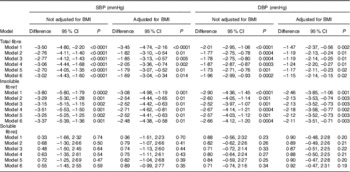
DBP, diastolic blood pressure; SBP, systolic blood pressure.
* 2 sd fibres (g/4184 kJ (g/1000 kcal)) total fibre (6·9); insoluble fibre (4·8); soluble fibre (2·2). Model 1 was adjusted for age, gender, total energy (kJ/24 h (kcal/24 h)), total protein (% energy), total fat (% energy), total sugar (% energy) and population sample. Model 2 was adjusted as model 1 variables plus adherence to energy-restricted diet, smoking, alcohol intake (g/24 h), hours engaged in moderate and heavy physical activity, dietary supplement use, educational level, CVD or diabetes diagnosis and family history of high blood pressure. Model 3 was adjusted as model 2 plus urinary Na (mmol/24 h). Model 4 was adjusted as model 2 plus urinary Mg (mmol/24 h). Model 5 was adjusted as model 2 plus urinary calcium (mmol/24 h). Model 6 was adjusted as model 2 plus urinary K (mmol/24 h).
† Additionally adjusted for soluble fibre (g/4184 kJ (g/1000 kcal)).
‡ Additionally adjusted for insoluble fibre (g/4184 kJ (g/1000 kcal)).
Insoluble fibre intake higher by 2sd (4·8 g/4184 kJ (4·8 g/1000 kcal)) was associated with a 2·52 mmHg lower SBP (95 % CI −4·42, −0·63), after adjustment for lifestyle factors, BMI and soluble fibre. The association remained significant after adjustment for urinary K (−2·48 mmHg; 95 % CI −4·38, −0·58). Soluble fibre intake was not associated with SBP or DBP, as in the main analyses.
Associations of fibre intakes with blood pressure in sub-cohorts
We repeated the regression analyses in other sub-cohorts, excluding participants with characteristics that may bias associations between fibre intake and BP (online Supplementary Table S2): a sub-cohort of non-hypertensive participants and a sub-cohort free of major chronic diseases (additionally excluding those with CVD and diabetes). Associations between total, insoluble fibre intake and BP in the two sub-cohorts were comparable with those from the main analyses. Although the association between SBP and insoluble fibre was slightly attenuated in non-hypertensive participants, it remained significant (−1·89 mmHg; 95 % CI −3·63, −0·15). After further exclusion of participants previously diagnosed with CVD or diabetes, the association between insoluble fibre and SBP did not remain statistically significant. Furthermore, the analyses were repeated, excluding participants who were taking fibre supplements (n 78). Results were compatible to the main analyses (data not shown).
Discussion
In this cross-sectional, population-based study of 2195 Americans participating in the INTERMAP Study, a higher intake of total dietary fibre was associated with lower BP; this finding may be attributable to the observed inverse association between insoluble fibre and SBP but not with soluble fibre. The associations between total, insoluble dietary fibre and SBP were attenuated with adjustment for urinary K levels. Results remained significant with adjustment of BMI, and are therefore independent of BMI influence. In the sub-cohort, excluding participants with hypertension and the use of antihypertensive drugs, the associations between total, insoluble dietary fibre and BP were independent of nutrients associated with higher intakes of fibre-rich foods, including K.
Previous cross-sectional( Reference Ascherio 4 – Reference Masala, Bendinelli and Versari 8 , Reference Fehily, Milbank and Yarnell 24 , Reference Joffres, Reed and Yano 25 ) and prospective( Reference Ascherio 4 , Reference Ascherio, Hennekens and Willett 5 , Reference Ludwig, Pereira and Kroenke 9 ) analyses have reported inconsistent findings on the association between total dietary fibre intake and BP. Some studies analysed cross-sectionally found inverse associations between total fibre intake and BP( Reference Ascherio 4 – Reference Stamler, Caggiula and Grandits 6 ), and some reported no association( Reference He, Klag and Whelton 7 , Reference Masala, Bendinelli and Versari 8 ). In prospective cohort studies, inverse relations between total fibre intake and BP change( Reference Ludwig, Pereira and Kroenke 9 ), or risk of developing hypertension( Reference Ascherio 4 , Reference Ascherio, Hennekens and Willett 5 ), were significant in white men and white women only( Reference Ascherio, Hennekens and Willett 5 , Reference Ludwig, Pereira and Kroenke 9 ) or no longer significant after adjustment for dietary confounders( Reference Ascherio, Hennekens and Willett 5 ). The inconsistent results may be explained by methodological issues and differences. First, in most of the studies, results were based on models that were mainly adjusted for non-dietary confounders( Reference Fehily, Milbank and Yarnell 24 , Reference Joffres, Reed and Yano 25 ) or included few dietary confounders( Reference Stamler, Caggiula and Grandits 6 , Reference Masala, Bendinelli and Versari 8 , Reference Elliott, Fehily and Sweetnam 10 ). Second, for most studies that examined the association of total fibre and BP, the frequency of BP measurements was typically low (one( Reference He, Klag and Whelton 7 ) or two( Reference Stamler, Caggiula and Grandits 6 , Reference Masala, Bendinelli and Versari 8 ) BP measures) or even based on self-reported data( Reference Ascherio 4 , Reference Ascherio, Hennekens and Willett 5 ). Third, most studies calculated fibre intakes from single( Reference Stamler, Caggiula and Grandits 6 , Reference Masala, Bendinelli and Versari 8 ), self-administered food frequency questionnaires( Reference Ascherio 4 , Reference Ascherio, Hennekens and Willett 5 ) or, alternatively, single 24 h dietary recalls( Reference Stamler, Caggiula and Grandits 6 , Reference He, Klag and Whelton 7 ). Our findings were derived from eight averaged BP measurements and four high-quality 24 h multipass dietary recalls per person collected over four visits. Moreover, we found stronger correlations between dietary and urinary variables from two-timed 24 h urinary collections in comparison with previously reported values( Reference Bingham, Gill and Welch 26 ). Dietary intakes were also energy-adjusted using the nutrient density method and an isoenergetic analysis that allows for interpretation of the relation of the nutrient composition of the diet with the outcome – that is, BP – while controlling for total energy intake( Reference Willett, Howe and Kushi 23 ). The availability of urine samples enabled us to adjust multivariate models for objective dietary intake measures, which in most other studies is not available.
The independent association between different types of dietary fibre and BP has been less thoroughly explored. To our knowledge, this is the first report on possible cross-sectional associations between total, insoluble and soluble dietary fibre intakes and BP, measured eight times, using models adjusted extensively for possible dietary and other lifestyle confounders. Previously, a cross-sectional analysis including 5961 middle-aged men and women of the SUVIMAX study reported that participants in the highest quartiles had a lower risk of hypertension of 29 % for total and 32 % for insoluble dietary fibre intakes, with no association reported for soluble fibre intake. The study showed that 5 g/d higher total fibre intake was associated with a 12 % lower risk of hypertension( Reference Lairon, Arnault and Bertrais 18 ). Although dietary fibre intakes were estimated by six 24 h dietary recalls, this study used only one BP measurement. Another limitation is that analyses were not controlled for several confounding factors including family history of CVD or high BP. Our results are also compatible with findings of a recent meta-analysis of twenty-two cohort studies that showed inverse associations between insoluble fibre intake and CVD, with no significant associations for soluble fibre intake, which may be attributed to low soluble fibre intake( Reference Threapleton, Greenwood and Evans 27 ).
BP-lowering effects of fibre have previously been attributed to a variety of factors, including increased nitric oxide release (a vasodilator)( Reference Brock, Davis and Irving 28 ); improvement in endothelial function by inhibiting Na absorption( Reference Brock, Davis and Irving 28 ), although inconclusiveReference Pal, Khossousi and Binns (29) ; improvement of other CVD risk factorsReference Kelly, Summerbell and Brynes (30 ); and improved insulin sensitivity and hyperglycaemia( Reference Chandalia, Garg and Lutjohann 31 , Reference Anderson, Baird and Davis 32 ).
Participants with diagnosed high BP, CVD or diabetes may have changed their dietary habits after their diagnosis towards a healthier pattern. Moreover, those participants have presumably lower BP levels due to their use of BP-lowering medication, which may distort the relationship between fibre intake and BP level. However, when those participants were excluded, results were consistently inverse. Based on these findings, it can be posited that the inverse associations between total, insoluble fibre and BP observed in our study are independent of BMI and of nutrients associated with higher intakes of high-fibre foods, including K.
Limitations of our study include its cross-sectional design making causal inferences not possible, regression dilution bias related to imprecise measures and the reliability estimate has been calculated to show the potential of bias (despite repeated measures), systematic bias from including multiple centres and possible residual confounding. However, extensive efforts were made to minimise these limitations (extensive observer training, repeated measurements of BP, standardised methods in dietary collection and BP measures, open-end questions and on-going quality control). In addition, although four 24 h dietary recalls were made, the dietary data may not be representative of a participant’s long-term habitual intake. In addition, although the associations between total, insoluble fibre intake and BP were independent of highly correlated nutrient intakes including K, we cannot rule out that other nutrients and phytochemicals abundant in high-fibre foods may be responsible for the observed inverse fibre–BP association( Reference Hooper, Kroon and Rimm 33 ).
In conclusion, in this cross-sectional study of free-living US participants, higher intakes of total fibre and insoluble fibre were associated with lower BP. Therefore, it may be a favourable approach to choose fibre-rich foods to prevent elevated BP. Confirmation from large-scale, prospective population studies with high-quality dietary data and BP measurements and intervention studies is, however, needed.
Acknowledgements
The authors thank all INTERMAP staff at local, national and international centres for their invaluable efforts. A partial listing of these colleagues is given in Holmes et al.( Reference Holmes, Loo and Stamler 34 ).
This study was supported by grants (R01-HL65461, R01-HL50490 and R01-HL84228) from the National Heart, Lung and Blood Institute, National Institutes of Health and by the National Institutes of Health Office on Dietary Supplements (Bethesda, MD, USA); also by national agencies in Japan, People’s Republic of China and the UK. P. E. acknowledges support from the National Institute for Health Research (NIHR) Imperial College Healthcare NHS Trust and Imperial College Biomedical Research Centre (grant number P38084), the MRC-PHE Centre for Environment and Health and the NIHR Health Protection Research Unit on Health Impact of Environmental Hazards; he is an NIHR Senior Investigator. The views expressed are those of the author and not necessarily those of the NHS, the NIHR or the UK Department of Health.
P. E. and J. S. are the principal investigators of INTERMAP and carried out the study set-up, design and methodology. G. A. carried out the writing of the paper. G. A. and L. O. G. carried out the analyses and methodology. G. F., Q. C., P. E., M. D. and L. V. H. were constantly involved in writing and editing the paper. All the authors were involved in writing the paper and gave their final approval for the submitted and published versions.
There are no conflicts of interest.
Supplementary material
For supplementary material/s referred to in this article, please visit http://dx.doi.org/doi:10.1017/S0007114515003098






