Adolescents (10–19 years of age) are at high risk for Fe deficiency and anaemia due to increased Fe requirements during this life stage, poor dietary intake of Fe, the onset of menstruation, teenage pregnancy among girls, risk of helminth infections and other factors(Reference Beard1,2) . Further, folate deficiency can cause megaloblastic anaemia and increase the risk of neural tube defects for adolescents who become pregnant(Reference Pitkin3,Reference Aslinia, Mazza and Yale4) . In India, the 2015–2016 National Family Health Survey estimated that the prevalence of anaemia among adult women and men aged 15–49 years was 53·1 and 22·7 %, respectively; the 2015–2016 National Family Health Survey sample did not include the full 10–19 years age range of adolescents(5). Studies in India and other low- and middle-income countries have documented that adolescents with Fe deficiency or anaemia on average have lower IQ scores, poorer attention and poorer productivity as compared with their non-anaemic or Fe-deficient peers(Reference Balarajan, Ramakrishnan and Ozaltin6,Reference More, Shivkumar and Gangane7) .
In order to address the large burden and consequences of adolescent anaemia in India, the Federal Ministry of Health and Family Welfare launched the national weekly iron and folic acid supplementation (WIFS) programme for in-school adolescents and out-of-school adolescent girls in 2012(8). The WIFS programme currently targets over 100 million adolescents for once WIFS of 100 mg elemental Fe and 500 μg folic acid(Reference Aguayo, Paintal and Singh9). Adolescents attending school in grades 6–12 are to receive WIFS tablets once weekly at school, while out-of-school adolescent girls receive community-based WIFS through Anganwadi centres(8). Anganwadi centres are a community-based, service-delivery component of the Indian public health care system that offers basic health care services(Reference Sachdev and Dasgupta10). Anganwadi centre activities primarily focus on women and children beneficiaries and services including contraceptive counselling, nutrition education and supplementation and early child development support. Early WIFS projects in India closely engaged communities, obtained high levels of supplementation coverage and found marked reductions in adolescent anaemia; however, when the WIFS programme was implemented nationally, there has been documented resistance in some communities and a few studies have documented low uptake among in-school adolescents(Reference Malhotra, Yadav and Kusuma11,Reference Dhikale, Suguna and Thamizharasi12) .
In order to address the need for population-based estimates of WIFS programme coverage in India, we conducted a cross-sectional survey of in-school adolescents and out-of-school adolescent girls residing in the Birbhum Health & Demographic Surveillance System (HDSS) in rural West Bengal, India.
Methods
We conducted a population-based cross-sectional household survey of adolescents residing in the Birbhum HDSS between December 2017 and March 2018. The Birbhum HDSS is located in the district of Birbhum in West Bengal, India, and is overseen by the Society for Health and Demographic Surveillance. The HDSS is primarily rural with the majority of households partaking in agriculture. The Birbhum HDSS was established in 2008, and during its first survey in 2009, the 2001 census sampling frame was used to select the HDSS study population using a simple stratified self-weighted random sample of 59 395 individuals from 13 053 household residing in 351 villages of four administrative blocks of Birbhum district. A full description of the Birbhum HDSS and population characteristics has been published elsewhere(Reference Ghosh, Barik and Majumder13). According to the 2011 data, 29·5 % of the population belong to the scheduled castes and 6·9 % to the scheduled tribes. In 2012, the mean age of marriage for girls was 18·1 years, and 16·2 % of all pregnancies were adolescent girls below 19 years of age.(Reference Ghosh, Barik and Majumder13)
We conducted a population-based survey of potential WIFS programme beneficiaries, which include adolescent boys and girls in 6th–12th grades (middle and lower/higher secondary school) and out-of-school adolescent girls(8). During the study period, the WIFS was exclusively provided to adolescents by the national programme through the local District Health Authority. Data from the 2017–2018 HDSS survey round were used to identify all households with adolescents aged 10–19 years. The 2017–2018 Birbhum HDSS survey round included 12 255 households and 52 716 individuals; we selected all 6693 individuals estimated to be 10–19 years old for potential participation in the WIFS survey. Study interviewers then visited the selected households, assessed eligibility of adolescents for participation in the survey and sought informed consent and assent for minors among those who were eligible. The inclusion criteria for the WIFS survey were male or female adolescents in grades 6–12 and out-of-school adolescent females (10–19 years of age) based on the intended WIFS programme beneficiaries. Exclusion criteria were out-of-school males (not intended beneficiaries of WIFS programme) and adolescents for whom parental consent or adolescent assent was not obtained. Written informed consent was obtained from all participants. For minors, written informed consent was obtained from a parent/guardian, and written assent was obtained from minors.
In order to assess the WIFS coverage, we asked all adolescent participants whether they received any WIFS tablets during the last month (30 d) and, if yes, the number of WIFS tablets they received. We then asked the number of WIFS tablets consumed among those who reported to have received tablets. We also asked adolescents for the primary reasons they decided to take the WIFS tablets as well as reasons for not consuming WIFS tablets among those who did not report consuming the tablets they had received. A demographic questionnaire was used to determine adolescent sex and grade level. Household wealth quintiles were constructed using a principal component analysis of adolescent reported household water source, toilet and household assets(Reference Vyas and Kumaranayake14).
We assessed the WIFS coverage by calculating the prevalence of consumption of four WIFS tablets during the last month for the full survey sample and by school status and sex. In order to assess the provision of WIFS, we then calculated the prevalence of adolescents who reported receiving at least one WIFS tablet in the last month and those receiving four WIFS tablets in the last month. We also assessed the adherence by calculating the percentage of adolescents who reported taking all WIFS tablets they received. We then examined predictors of reported receipt of at least one WIFS tablet in the last month and then consumption of all WIFS tablets received among in-school adolescents using log-binomial models to produce relative risk estimates(Reference Spiegelman and Hertzmark15). P-values for trend for categorical wealth quintiles were calculated by treating the median value of each category as a continuous variable. Missing indicators were used for missing data. Statistical analyses were performed using the SAS version 9.4.
Results
Of the 6693 adolescents attempted to be contacted, we were not able to contact 934 (14·0 %) of these individuals for participation. Among 5759 adolescents contacted for participation, 359 in-school adolescents who were not in grades 6–12 and 952 out-of-school boys were excluded from participation since they were not eligible for the WIFS programme. There were some differences in sex (contacted 52·8 % male; unable to be contacted 47·1 % male) and mean age (contacted 14·8 ± 2·8 years; unable to be contacted 16·4 ± 2·8 years) between adolescents who were contacted as compared with those who were unable to be contacted. A total of 4448 adolescents 10–19 years of age were determined to be eligible and participated in the WIFS survey. The sample included 1903 (42·8 %) in-school girls, 1898 (42·7 %) in-school boys and 647 out-of-school girls (14·5 %). Among in-school adolescents, 74·0 % were in the middle school, 16·0 % were in the lower secondary school and 10·0 % were in the higher secondary school.
The percentage of adolescents that reported taking four WIFS tablets during the last month as intended by the national programme was 9·4 % (95 % CI 8·1, 10·7 %) for in-school girls, 7·1 % (95 % CI 6·0, 8·3 %) for in-school boys and 2·3 % (95 % CI 1·7, 4·1 %) for out-of-school girls (Fig. 1). The effective coverage of the WIFS programme was low due to the combination of large gaps in the provision of WIFS as well as poor adherence. Among in-school adolescent girls, 38·3 % received at least one WIFS tablet during the last month and only 20·2 % received four WIFS tablets as intended by the programme. These percentages were slightly lower for in-school adolescent boys at 26·7 and 16·1 %, respectively. In addition, there was low reported adherence to WIFS tablets. Among adolescents who received WIFS tablets during the last month, the percentage that took all tablets they received was 41·6 % for in-school girls, 38·1 % for in-school boys and 47·4 % for out-of-school girls.
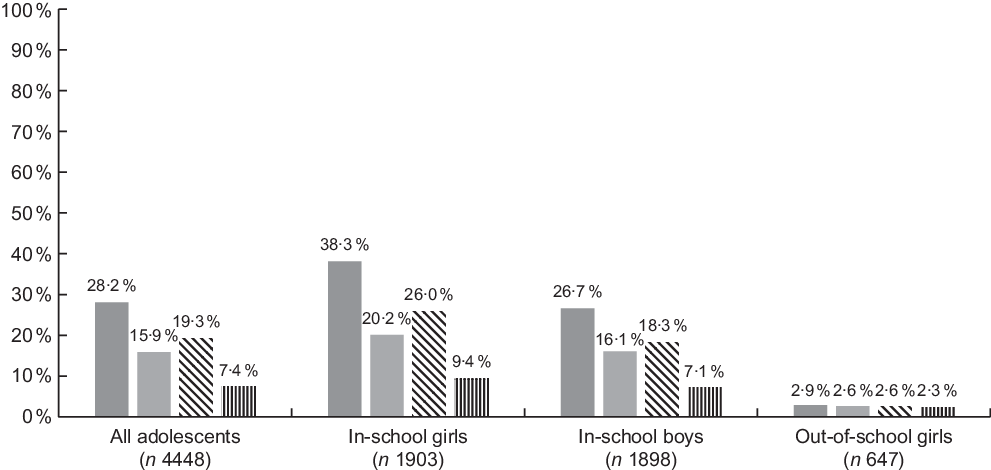
Fig. 1 Effective coverage of weekly iron and folic acid supplementation (WIFS) among adolescents overall and stratified by schooling status and sex in rural Birbhum, India (n 4448). ![]() , received at least one WIFS tablet during the last month;
, received at least one WIFS tablet during the last month; ![]() , took at least one WIFS tablet during the last month;
, took at least one WIFS tablet during the last month; ![]() , received four WIFS tablet during the last month;
, received four WIFS tablet during the last month; ![]() , took four WIFS tablets during the last month
, took four WIFS tablets during the last month
We then examined factors associated with receipt of at least one WIFS tablet during the last month and consumption of all WIFS tablets received (Table 1). In multivariate analyses, in-school boys were 29 % (95 % CI 20, 37 %) less likely to report they received at least one WIFS tablet during the last month as compared with in-school girls. Lower secondary school students (relative risk 0·78, 95 % CI 0·65, 0·94) and higher secondary students (relative risk 0·16, 95 % CI 0·10, 0·27) were less likely to report having received WIFS as compared with middle school students. In terms of reported consumption of tablets received, there was no difference by schooling level, sex and age. However, there was some indication that lower wealth quintiles may be associated with increased adherence to WIFS (P-value for trend 0·07).
Table 1 Association of school level, adolescent sex and household wealth with receipt of at least one weekly iron and folic acid supplementation (WIFS) tablets in last month and reported consumption of all WIFS tablets received among in-school adolescents (n 4160)
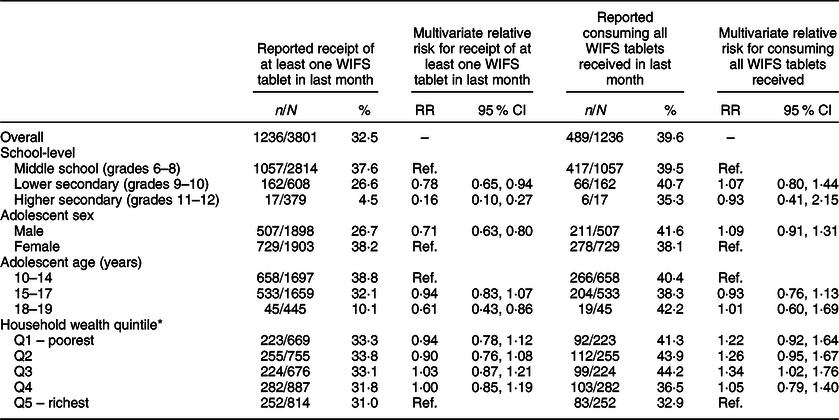
RR, relative risk.
* Calculated by water source, toilet and household assets among all adolescent households.
We also assessed the primary reasons in-school adolescents reported for adhering or not adhering to WIFS. Among in-school adolescents who consumed all WIFS tablets they received, 95·1 % reported the primary reason they took the tablets was counselling from teachers, school principals, vice principals or other school staff. As for students who did not take the WIFS tablets they received, 47·7 % reported they did not think WIFS was beneficial, 20·2 % said their peers suggested they should not take the tablets and 16·6 % reported they had experienced side effects.
Discussion
Overall, the population-level coverage of the WIFS programme in rural Birbhum, India was low. We found that the lack of WIFS tablet supply was a major contributor to low coverage. We found that among in-school adolescents, boys and adolescents in higher secondary school were less likely to report having received WIFS tablets. The suboptimal adherence also contributed to low coverage as adolescents reported taking <50 % of the WIFS tablets they received.
The low coverage of the WIFS programme in rural West Bengal is consistent with other reports that have noted suboptimal coverage(Reference Malhotra, Yadav and Kusuma11). A recent mixed-methods study of in-school adolescents in North Kerala found about 25 % coverage of WIFS and noted that fear of side effects was a major contributor to low adherence in this setting(Reference Sarada and Thilak16). A study in Pondicherry also indicated <50 % coverage of WIFS and identified similar reasons for non-adherence, including fear of side effects, lack of perceived benefits and irregular supply of WIFS(Reference Priya, Bahurupi and Narayan17). Nevertheless, there are some reports of relatively high coverage of WIFS in some settings, such as a school-based study conducted in a different part of Pondicherry that found 86 % of adolescents reported taking four WIFS tablets in the last month; the authors noted that counselling from teachers appeared to be an important factor which is consistent with our findings(Reference Dhikale, Suguna and Thamizharasi12). To the best of our knowledge, our study is the first to assess the WIFS programme coverage among out-of-school adolescent girls and we determined that coverage in this group was very low and largely driven by a lack of provision of WIFS tablets.
In terms of potential interventions to increase coverage and adherence, studies have documented that important components of the successful WIFS pilot in India have not been fully translated and incorporated into the national WIFS programme roll-out, including close engagement of stakeholders, timely and quality communication on programme issues between stakeholders, availability of WIFS supplements, technical and supervisory support and peer group advocacy(Reference Malhotra, Yadav and Kusuma11). There is also evidence that adolescent girl-to-girl peer counselling has been shown to be very effective in increasing WIFS coverage and decrease anaemia in Uttar Pradesh(Reference Vir, Singh and Nigam18). As a result, it is likely a multi-component intervention will be needed to activate the complex enablers to high coverage of WIFS.
The current study has a few limitations. Firstly, we assessed the WIFS coverage using adolescent self-report, and therefore we may have overestimated both provision and adherence due to social desirability bias. We also found that girls and older adolescents were more likely to not be reached for participation in the survey, and therefore there is the potential for some degree of selection bias in our study. It is possible that these harder to reach adolescents could have decreased access to WIFS as compared with their peers who were able to be contacted for study participation. In addition, we did not assess Hb concentrations and were therefore unable to link WIFS programme coverage and tablet adherence to anaemia prevalence. Future studies would benefit from assessing Hb as well as Fe biomarkers to assess the prevalence of Fe deficiency anaemia. In addition, we did not collect information on the WIFS supply chain and therefore were not able to provide details on specific issues affecting distribution at schools or Anganwadi centres. Lastly, the provision of WIFS among out-of-school girls was too low to assess risk factors for provision and adherence as well as reasons for taking or not the tablets.
The population-level coverage of the WIFS programme was low among in-school adolescents and out-of-school girls in rural Birbhum. Our findings and the literature suggest that integrated supply- and demand-side strategies that closely engage the adolescents, school staff and the community will be needed to increase the effective coverage of WIFS. These strategies should take into account potential differences in the needs of in-school adolescents and out-of-school adolescent girls. The technical and supervisory support may increase WIFS supply and provision in schools and Anganwadi centres, while engagement of teachers, administrators and school staff, as well as peer support groups for both in-school and out-of-school adolescents, may improve adherence. Implementation research can inform and evaluate strategies and policies to fully realise the potential benefits of the WIFS programme in India.
Acknowledgements
Acknowledgements: None. Financial support: The current work was supported by the West Bengal State Department of Health and Family Welfare, India (memo no. 114-P&B/HFW-27011/114/2019-NHM SEC). The funders had no role in the design or conduct of the study, collection or analysis or interpretation of the data and reparation or review or approval of the manuscript. Conflict of interests: There are no conflicts of interest. Authorship: C.R.S., A.B., R.K.R. and W.W.F. conceived the study. A.B., R.K.R., J.J.V. and W.W.F. developed the questionnaire, and A.B. and R.K.R. supervised the survey. C.R.S. analysed the data and prepared the first draft. All authors critically reviewed the paper and approved of the final manuscript. Ethics of human subject participation: The current study was conducted according to the guidelines laid down in the Declaration of Helsinki, as revised in 2008, and all procedures involving study participants were approved by the Institutional Ethics Review Board appointed by the Governing body of Society for Health and Demographic Surveillance. Written informed consent was obtained from all participants. For minors under the age of 18 years, written consent was obtained from a parent/guardian, and written assent was obtained from minors.




