Overconsumption of energy is a known risk factor for the development and progression of type 2 diabetes( Reference Pan, Li and Hu 1 ). However, dietary modification, including energy restriction, is a challenging aspect of diabetes management( Reference Clark 2 ). Thus, understanding dietary habits that are associated with reduced daily energy intake is important for optimizing management of type 2 diabetes. Consuming a healthy breakfast might be one such habit. The benefit of eating breakfast has been studied primarily compared with not consuming breakfast. Yet, it is unclear whether a higher-energy breakfast is associated with lower total daily energy intake.
Several studies have shown associations between breakfast eating v. skipping and a decreased risk of type 2 diabetes( Reference Mekary, Giovannucci and Willett 3 ), less weight gain( Reference van der Heijden, Hu and Rimm 4 ) and better insulin sensitivity and lipid profiles( Reference Farshchi, Taylor and Macdonald 5 ). A possible explanation is that breakfast consumption may prevent subsequent overeating( Reference Pereira, Erickson and McKee 6 ). However, while some studies reported that people who eat breakfast consume less energy( Reference Farshchi, Taylor and Macdonald 5 ), data from other studies did not support this finding( Reference Nicklas, Myers and Reger 7 – Reference Dubois, Girard and Potvin Kent 9 ). This inconsistency suggests that, beyond just eating breakfast, the energy content of breakfast may influence daily energy intake( Reference Timlin and Pereira 10 ).
Few studies have tested the association between breakfast energy and daily energy intake in free-living conditions, using absolute (amount of energy eaten at breakfast) and relative (proportion of breakfast energy to total daily energy) measures. Data from observational studies showed that consuming a higher-energy breakfast (absolute measure) was associated with a greater daily energy intake( Reference Schusdziarra, Hausmann and Wittke 11 ). Similarly, in a trial with a crossover design among ten healthy men, consuming a high-energy v. a low-energy breakfast over a 2-week period was associated with a greater daily energy intake( Reference Martin, Normand and Sothier 12 ). Accordingly, it has been recommended to eat less or even no breakfast as a strategy to decrease daily energy intake. Conversely, some researchers have argued against using the absolute measure, stating that breakfast is a component of daily intake, and that there would be a false association between breakfast energy and daily energy intake( Reference de Castro 13 ). With using the relative measure of breakfast, however, a breakfast that comprised a greater percentage of daily energy intake was associated with a lower( Reference de Castro 13 , Reference de Castro 14 ) or a higher( Reference Purslow, Sandhu and Forouhi 15 ) daily energy intake. Thus, another recommended strategy to decrease daily energy intake is to eat a greater proportion of daily energy at breakfast. It appears that the expression of breakfast energy in absolute v. relative terms has generally yielded opposite results with respect to daily energy intake. While the absolute measure reflects only breakfast energy, the relative measure reflects energy eaten at subsequent meals as well.
The objectives of the present study were to evaluate the effects of absolute and relative breakfast energy on (i) daily energy intake and (ii) subsequent meals (lunch, dinner and snacks) among people with type 2 diabetes.
Methods
Study population
We used data from the 1999–2004 National Health and Nutrition Examination Survey (NHANES). NHANES is a continuous cross-sectional survey of a nationally representative sample of the non-institutionalized civilian US population( 16 ). The data were collected through household interviews and physical examinations in mobile examination centres. As part of the medical history, participants were asked about their history of diabetes: ‘Other than during pregnancy, have you ever been told by a doctor or health professional that you have diabetes or sugar diabetes?’ For the current analysis we included participants with a positive history of diabetes. Previous studies have shown the specificity of self-reported diabetes to be 97 %( Reference Kehoe, Wu and Leske 17 ). Since the questionnaire did not distinguish between type 1 and type 2 diabetes, respondents were excluded if they were aged less than 30 years or had onset of diabetes or insulin treatment before age 30 years, so that our sample primarily includes individuals with type 2 diabetes. In addition, we excluded individuals with values for energy intake outside the range of 2092–14644 kJ (500–3500 kcal) for women and 3347–16736 kJ (800–4000 kcal) for men( Reference Willett 18 ).
Dietary information
Participants completed a 24 h dietary recall using a computer-assisted dietary interview in NHANES 1999–2001 and a fully computerized recall method in NHANES 2002–2004. In addition to recalling everything consumed during the prior 24 h, participants were asked to name each eating occasion. Dietary information, including energy and nutrient contents of each food item, was estimated by NHANES using US Department of Agriculture food composition data( 19 ). We computed daily energy intake, overall and by meal (breakfast, lunch, dinner) and snack, based on what participants named each eating occasion.
Breakfast energy intake was expressed in absolute (kilojoules) and relative (percentage of daily energy intake) terms. We chose to compare these two different approaches due to conflicting dietary recommendations. The absolute measure allows for a more meaningful and sensible recommendation than the relative measure. The relative measure, on the other hand, might be more useful when comparing individuals with different daily intake, in whom using the absolute measure may produce false results. For example, a 1674 kJ (400 kcal) breakfast comprises only 13 % of daily intake in a person consuming 12552 kJ (3000 kcal), but 22 % in a person consuming 7531 kJ (1800 kcal) daily. We categorized each measure in quartiles in order to test for non-linear associations and trends. For the absolute measure, breakfast energy was categorized using sex-specific quartiles (Q) to account for the difference in energy intake between men and women, with Q1 indicating lowest and Q4 indicating highest energy intake. For the relative measure, percentage of daily energy intake at breakfast was calculated and categorized as quartiles. We treated the absolute and relative measures equally, using separate statistical regression models, as described below. Descriptive statistics were presented for the quartiles of the relative measure.
Covariates
Covariates were factors previously found to be associated with breakfast consumption or daily energy intake, including age, sex, race/ethnicity, physical activity, BMI and smoking( Reference Song, Chun and Obayashi 8 , Reference Ruxton and Kirk 20 ). Age and BMI were continuous variables. Physical activity was estimated by questions about leisure-time activity. For moderate and vigorous activities, NHANES assigned metabolic equivalent of task (MET) scores( 16 ). Using the MET-h/week values, levels of physical activity were defined as inactive (0), slightly active (>0 and <9) and active (≥9), based on the recommendation for moderate physical activity of 150 min/week( 21 ), which is about 9 MET-h/week. BMI was calculated from measured weight and height. Self-reported smoking status was either ‘current smoker’ or ‘non-smoker/ex-smoker’. Clinical information, including diabetes duration and oral diabetes medications, were used for descriptive statistics.
Statistical analysis
Statistical analyses were performed using the SAS statistical software package version 9·2. For all analyses we used ‘proc survey’ procedures, which included sampling weight to account for the complex sampling design in NHANES. Basic characteristics were compared between quartiles of relative breakfast energy using χ 2 analysis for frequencies and ANOVA for means. We constructed age-adjusted linear regression models to estimate the regression coefficients (β) and corresponding 95 % confidence intervals for the independent variable of quartiles of either absolute or relative breakfast energy, with daily energy intake as outcome. Models were controlled for the covariates sex, race/ethnicity, physical activity, BMI and smoking, as described above. Orthogonal polynomial contrasts were used to test daily energy intake across quartiles of either absolute or relative breakfast energy for linear and quadratic trends. In addition, we used separate multiple regression models for dependent variables (energy intake for lunch, dinner, snacks), besides the main outcome of interest (total daily energy intake), to test the effect of quartiles of absolute and relative breakfast energy on intake at each eating occasion, using the same covariates (age, sex, race/ethnicity, physical activity, BMI and smoking).
Results
Of 1576 individuals with self-reported history of diabetes, 1146 persons were eligible for the current analysis. Of the final study sample, 584 (51 %) were women. On average, the mean energy consumed at breakfast and the mean total daily energy intake were 1561 (sd 1134) kJ and 7142 (sd 2782) kJ, respectively. The mean relative contribution of breakfast to total daily energy intake was 23 (sd 15) %. Individuals in the highest quartile of relative breakfast energy were, on average, older than those in the lowest quartile (P<0·0001; Table 1). Also, there was a significant relationship between quartiles of absolute and relative breakfast energy (P<0·0001). The distribution of clinical and lifestyle factors did not differ between quartiles of relative breakfast energy.
Table 1 Baseline characteristics of participants according to relative energy intake at breakfast (percentage of total daily energy intake)Footnote †; adults aged ≥30 years with self-reported history of type 2 diabetes (n 1146), the 1999–2004 National Health and Nutrition Examination Survey (NHANES)
MET, metabolic equivalent of task.
† Means and percentages were estimated by using sampling weight. Numbers for some variables do not add up to the total because of missing data.
‡ Relative breakfast energy reflects breakfast energy as a percentage of total daily energy intake.
§ P value for the difference between the means of Q1 and Q4 groups, or the distribution among the four quartiles.
|| Because of the cells with frequency <5, cells were combined as Q1+Q2 and Q3+Q4 for both rows and columns, making a 2×2 table.
As absolute breakfast energy increased, daily energy intake increased (Table 2). In multivariable analysis, daily energy showed significant linear (P<0·0001) and quadratic (P=0·02) trends with breakfast energy. Compared with the first quartile (Q1), Q3 and Q4 of breakfast energy were associated with higher daily energy intake, with a sharp increase beginning at Q3.
Table 2 Estimated linear regression coefficients (β) and 95 % confidence intervals for absolute breakfast energy (kJ) and relative breakfast energy (percentage of total daily energy intake), with total daily energy intake as the outcome; adults aged ≥30 years with self-reported history of type 2 diabetes (n 1146), the 1999–2004 National Health and Nutrition Examination Survey (NHANES)
Ref., referent category.
† Covariates: BMI, race/ethnicity, physical activity, smoking, age and sex.
As relative breakfast energy increased, daily energy intake decreased linearly, both in age-adjusted (P for trend=0·0002) and multivariable (P for trend <0·0001) analyses (Table 2). The inverse association between breakfast energy and daily energy intake was observed when breakfast comprised 22 % or more of total daily energy intake (i.e. Q3 and Q4 of relative breakfast energy compared with Q1). Among the covariates included in the model, greater relative breakfast consumption was associated with male sex (P<0·0001) and older age (P<0·0001).
We also assessed the influence of absolute and relative breakfast energy on lunch, dinner and snack energy using multivariate regression models (Fig. 1). Higher quartiles of absolute breakfast energy had no observed associations with lunch or dinner energy; whereas snack energy was slightly lower (Fig. 1(a)). In contrast, higher quartiles of relative breakfast energy were associated with lower total daily energy intake, as well as lower energy intake at each subsequent meal and snacks (Fig. 1(b)). Interestingly, mean energy intakes at breakfast for the quartiles of relative breakfast energy were similar to those of the absolute measure. For example, mean energy consumed at breakfast was 1715 kJ for Q3 of absolute intake and 1782 kJ for Q3 of relative intake; corresponding values for Q4 absolute and Q4 relative were 3025 kJ and 2741 kJ, respectively. Despite these similarities in breakfast energy intake, the associations of breakfast quartiles with total daily energy intake were opposite for the absolute and relative measures, i.e. a positive association between quartiles of absolute breakfast energy and total daily energy intake, but an inverse association between quartiles of relative breakfast energy and total daily energy intake.
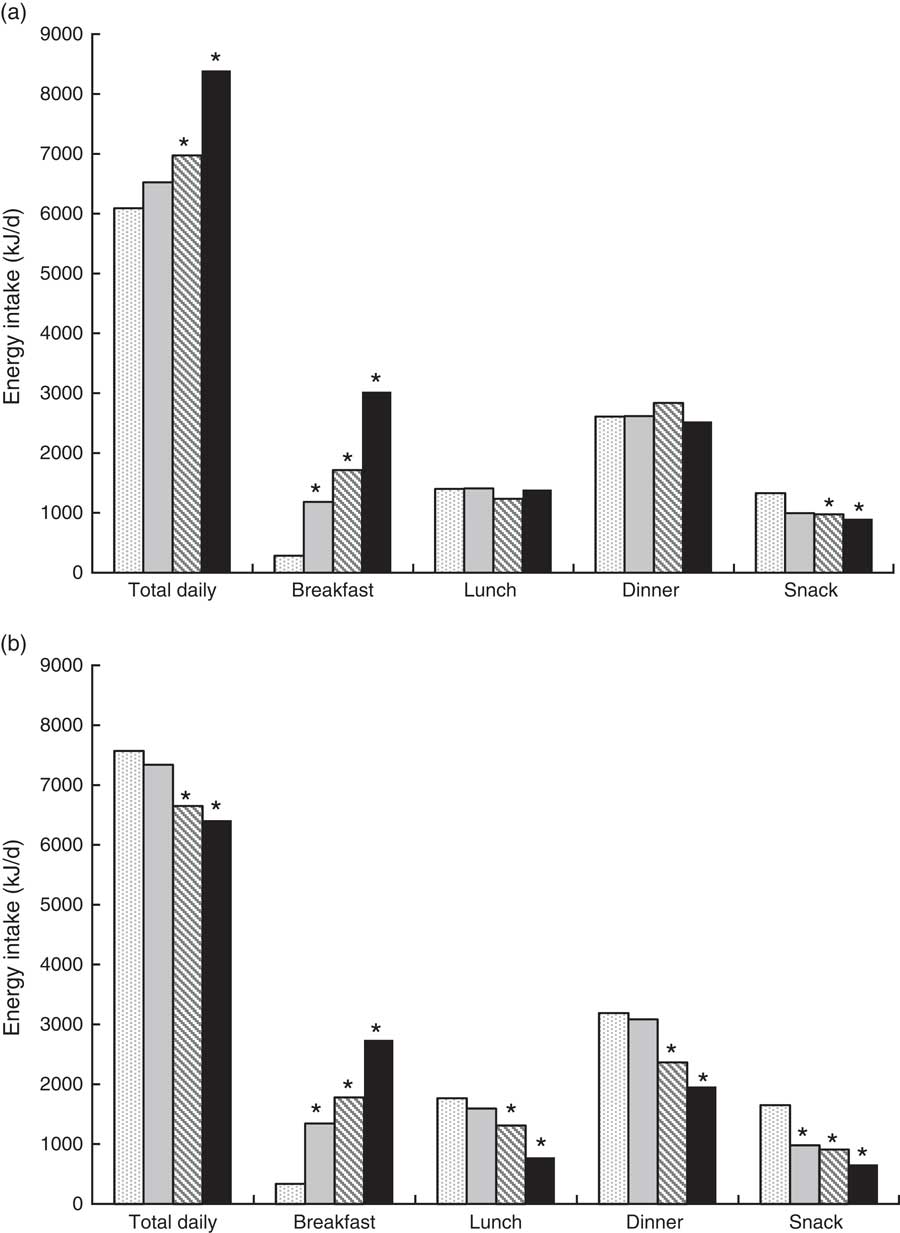
Fig. 1 Least square means from multivariable regression models for total daily energy intake and energy intakes at breakfast, lunch, dinner and snacks, based on quartiles of (a) absolute breakfast energy (kJ; females, males: ![]() , Q1, 0–745, 0–987;
, Q1, 0–745, 0–987; ![]() , Q2, 766–1259, 1008–1653;
, Q2, 766–1259, 1008–1653; ![]() , Q3, 1264–1766, 1657–2335;
, Q3, 1264–1766, 1657–2335; ![]() , Q4, 1770–6079, 2339–7293) or (b) relative breakfast energy (percentage of total daily energy intake:
, Q4, 1770–6079, 2339–7293) or (b) relative breakfast energy (percentage of total daily energy intake: ![]() , Q1, <13 %;
, Q1, <13 %; ![]() , Q2, 13 % to <22 %;
, Q2, 13 % to <22 %; ![]() , Q3, 22 % to <31 %;
, Q3, 22 % to <31 %; ![]() , Q4, ≥31 %); adults aged ≥30 years with self-reported history of type 2 diabetes (n 1146), the 1999–2004 National Health and Nutrition Examination Survey (NHANES). *P<0·05 in comparison to mean intake for the same meal occasion in the first quartile (Q1) of breakfast energy
, Q4, ≥31 %); adults aged ≥30 years with self-reported history of type 2 diabetes (n 1146), the 1999–2004 National Health and Nutrition Examination Survey (NHANES). *P<0·05 in comparison to mean intake for the same meal occasion in the first quartile (Q1) of breakfast energy
Discussion
We assessed the association between breakfast energy and daily energy intake among individuals with self-reported diabetes from the NHANES 1999–2004 population. The key findings were that, depending on whether breakfast energy was expressed as an absolute or a relative quantity, breakfast energy had a positive or inverse association, respectively, with daily energy intake. In addition, consuming more absolute energy at breakfast was not predictive of energy intake during subsequent meals and snacks, which suggests that individuals may not compensate for a high-energy breakfast by eating less throughout the rest of the day. However, consuming a relatively large breakfast, expressed as a proportion of daily energy intake, appeared to be associated with lower energy intake at each subsequent eating occasion throughout the rest of the day.
We observed a quadratic association between breakfast energy and total daily energy intake. Although we did not include breakfast skipping as a separate group, our data provide some information to explain the previous conflicting results that eating v. skipping breakfast was associated with similar( Reference Halsey, Huber and Low 22 , Reference Leidy and Racki 23 ), higher( Reference Song, Chun and Obayashi 8 , Reference Timlin, Pereira and Story 24 ) or lower( Reference Farshchi, Taylor and Macdonald 5 ) daily energy intake. We found that energy consumed at breakfast is positively associated with daily energy intake at the higher quartiles (Q3, Q4), but not the lower quartiles (Q1, Q2) of breakfast energy. In other words, our results of a quadratic trend with a near J-shaped association between energy eaten at breakfast and daily energy intake suggest that the direction of the association between breakfast and daily energy intake depends on the number of kilojoules eaten at breakfast. This indicates a threshold breakfast energy level, for example in our sample 1715 kJ (Q3 mean), beyond which consuming more energy is associated with higher daily energy intake. Thus, contrary to a high-energy breakfast, a low- to medium-energy breakfast may not contribute to higher daily energy intake.
Two clinical trials have evaluated the influence of breakfast energy on daily energy intake. In one study, compared with skipping breakfast, consuming breakfast ad libitum with an average of 2929 kJ (700 kcal) resulted in greater daily energy intake( Reference Levitsky and Paconowski 25 ). Similarly, in a crossover trial, participants had significantly higher daily energy intake when they consumed a high-energy breakfast (2920 kJ) compared with either a low-energy (418 kJ) or an ad libitum (mean 1923 kJ) breakfast( Reference Martin, Normand and Sothier 12 ). Consistent with these findings, previous research also has shown that eating more energy due to larger portion sizes at a meal/snack is not completely compensated for during subsequent meals throughout the day, and thus can contribute to an overall higher energy intake( Reference Rolls, Roe and Meengs 26 ), especially in overweight persons( Reference Ebbeling, Sinclair and Pereira 27 ).
When breakfast energy was expressed as a percentage of daily energy intake, our results were consistent with some( Reference de Castro 13 , Reference de Castro 14 ), but not all studies( Reference Purslow, Sandhu and Forouhi 15 ) showing that consuming a higher proportion of daily energy at breakfast was associated with lower daily energy intake. When interpreting relative intake, an important and practical question is whether a higher relative breakfast intake corresponds to a higher absolute energy intake at breakfast. One study addressed this question by using both absolute and relative measures of breakfast in an intra-individual analysis( Reference Schusdziarra, Hausmann and Wittke 11 ). The authors reported that higher relative breakfast energy was attributable primarily to lower energy intake during other meals rather than to more energy at breakfast. Therefore, our finding of an inverse association between quartiles of relative breakfast energy and total daily energy intake may not be merely because of a higher absolute energy intake at breakfast.
It should be noted that with a fixed daily energy intake, consuming a high-energy breakfast and a low-energy dinner may be beneficial for managing body weight and improving insulin resistance( Reference Jakubowicz, Barnea and Wainstein 28 ). However, to our knowledge, there is no evidence in free-living persons indicating that eating more energy at breakfast will result in a spontaneous decrease in subsequent food intake to an extent at least equal to the breakfast energy. Thus, recommendations about breakfast consumption in adults with type 2 diabetes should include consideration of energy content. In addition, consuming a high-energy breakfast may need to be combined with an intentional restriction of other meals throughout the day.
Our findings suggest that the reason for the opposite associations between the absolute and relative measures of breakfast energy and total daily energy intake is due to the difference between the two measures. In our study, although quartiles of absolute and relative measures of breakfast energy were related, breakfast energy in 310 participants (18 %) was in lower quartiles (Q1, Q2) with one measure but in higher quartiles (Q3, Q4) with the other measure, as shown in Table 1. This indicates that consuming a large proportion of daily intake at breakfast does not necessarily reflect consuming more energy at breakfast and vice versa. What distinguishes the relative measure from the absolute measure is that the relative measure provides a measure of not only energy content of breakfast, but also intake during subsequent meals. Moreover, the association between breakfast energy and total daily intake may depend more on the intake during the subsequent meals, than on the absolute breakfast energy per se.
One possible factor in suppression of subsequent intake, and so increasing the relative contribution of breakfast, is the protein content. Protein is the most satiating macronutrient( Reference Weigle, Breen and Matthys 29 ). Recent studies have shown that a high-protein breakfast has additional benefits over a regular breakfast on appetite control and energy intake among overweight adolescents( Reference Leidy and Racki 23 , Reference Leidy, Ortinau and Douglas 30 ). To our knowledge, no trial tested the effect of breakfast protein content in people with type 2 diabetes. However, studies have shown that a high-protein diet resulted in better metabolic control among people with type 2 diabetes( Reference Gannon, Nuttall and Saeed 31 ). Another possible factor in suppression of subsequent intake is the glycaemic index. Consuming a low-glycaemic-index breakfast induced satiety, compared with a high-glycaemic-index breakfast, among overweight and obese individuals( Reference Sebely, Lim and Egger 32 ). Thus, consuming a low-energy, low-glycaemic-index breakfast containing relatively higher protein may be a useful strategy to decrease daily energy intake and to improve metabolic control in individuals with diabetes.
The present study has limitations, including the cross-sectional design and reliance on self-reported dietary intake based on a single 24 h recall. It is possible that actual intakes were underestimated, especially because obese individuals, who compromised about half of our sample, tend to under-report their energy intake( Reference Johnson, Goran and Poehlman 33 ). However, it is unlikely that under-reporting affected our conclusions because breakfast intake was likely under-reported to a similar extent as other eating occasions throughout the day. Despite these limitations, the major strengths of the study include a large sample from a nationally representative data set, evaluation of both absolute and relative measures of breakfast intake and statistical models that explored both linear and quadratic trends.
Conclusion
In conclusion, the present study indicates that higher relative breakfast energy intake was associated with lower total daily energy intake in a national sample of individuals with type 2 diabetes. Breakfast characteristics that were associated with lower total daily energy intake were either a rather low-energy breakfast or a breakfast of any energy level that comprised a greater proportion of daily energy intake. Thus, recommendations regarding breakfast intake need to be more specific, particularly in individuals with type 2 diabetes. Recommendations should consider breakfast intake in relation to the other meals of the day (e.g. increasing the contribution of breakfast to total daily energy intake). Intervention studies are needed to evaluate the observed associations. In addition, future studies in individuals with type 2 diabetes should examine other dietary factors that influence energy intake and metabolic control, such as breakfast macronutrient content and energy density.
Acknowledgements
Financial support: S.J. was supported by the Washington University School of Medicine. M.S. was supported by a grant from the National Cancer Institute at the National Institutes of Health (grant number CA112159). The funding agencies had no role in the design, analysis or writing of this article. Conflict of interest: None. Authorship: S.J. and M.S. designed the research; S.J. and S.B.R. conducted the research; S.J. analysed the data; S.J. and S.B.R. wrote the paper; S.J. had primary responsibility for final content. All authors read and approved the final manuscript. Ethics of human subject participation: NHANES was reviewed and approved by the National Center for Health Statistics institutional review board, and all participants provided written informed consent before participation.






