CVD contributes to a significant burden of disease in both high-income and low- and middle-income countries(Reference Joseph, Leong and McKee1). In 2015 more than half a million adult Australians reported living with the most common form of CVD, IHD(2). While CVD risk factor reductions and advances in medical treatment have contributed to very significant CVD mortality declines since the 1970s(Reference O’Flaherty, Allender and Taylor3), it remains the number one cause of mortality in Australia(2). CVD presents a large cost burden to health systems; Australian estimates from 2012–2013 indicate that CVD was responsible for $AU 5 billion, or 11·1% of all inpatient Australian health-care costs(4). Australia’s public health guidelines(5) promote healthy diets and physical activity, underpinned by evidence showing that meeting these guidelines will reduce the risk of CVD(Reference He, Nowson and Lucas6, 7). Most Australians do not meet these guidelines, with only 4% of Australians meeting recommended intakes for vegetables and legumes in 2011–2012(8) and 11% meeting the guidelines for sufficient physical activity(7), representing a clear opportunity for reducing CVD and broader non-communicable disease burden in Australia. Risk factors have been shown to differ between major cities and rural areas in Australia with most risk factors being less favourable in rural areas, with the exception of vegetable intake(Reference Alston, Peterson and Jacobs9).
Modelling studies allow quantification of the benefit of improving population risks to inform resource allocation and prioritisation(Reference Belanger, Poirier and Jbilou10, Reference Scarborough, Allender and Clarke11). A study in Canada(Reference Belanger, Poirier and Jbilou10) showed that 30 540 deaths from non-communicable diseases could be averted annually if the Canadian population were able to attain the recommended dietary intake levels. The study found that if the population could meet vegetable and fruit guidelines alone this would account for 72% of the deaths prevented(Reference Belanger, Poirier and Jbilou10). A study in the UK that modelled the impact of the entire population meeting the physical activity guidelines (150 min of moderate-to-vigorous physical activity per week) showed that life expectancy (at birth) would increase by a mean of 95 (95% CI 68, 128) d and incidence of IHD in the UK would reduce by approximately 5%(Reference Mytton, Tainio and Ogilvie12).
Australian estimates of benefits arising from meeting health guidelines rarely consider the heterogeneity of risk or outcome profiles across population geography(13, 14). Rural populations in Australia are under-researched in comparison to need, with a dominance of urban-centric research in the Australian literature(Reference Barclay, Phillips and Lyle15). This has resulted in limited evidence specific to rural populations to drive policy priority setting for the prevention of non-communicable diseases(Reference Laatikainen, Janus and Kilkkinen16). Large differences in access to health care, health service structures, community and social norms and geographical isolation have been documented when comparing rural and urban populations, and are known to influence health(Reference Bourke, Humphreys and Wakerman17). Differences in CVD risk factors are evident between rural and metropolitan Australia which could mean that differentiation in public health priorities of targeting recommendations is warranted(Reference Alston, Peterson and Jacobs9).
Given that health promotion resources are limited, knowledge on which recommendations would yield the most benefit (if attained) could assist with policy prioritisation. Understanding how these benefits and relative priorities may differ between metropolitan and rural populations in Australia may help development of targeted interventions.
Therefore, the aims of the present study were to:
1. determine how many deaths from CVD and IHD would be delayed/averted if Australians met public health recommendations in both metropolitan and rural areas;
2. determine which recommendations would be the highest priority in metropolitan and rural populations, based on potential mortality reductions; and
3. ascertain the extent to which absolute and relative CVD and IHD mortality inequalities would persist between rural and metropolitan Australia if public health recommendations were met.
Methods
The Preventable Risk Integrated Model
The Preventable Risk Integrated Model (PRIME) has been used to understand how potential changes from current population risk factor levels would impact on chronic disease mortality in the UK, Canada and Australia(Reference Alston, Peterson and Jacobs9–Reference Scarborough, Allender and Clarke11, Reference Nichols, Scarborough and Allender18, Reference Scarborough, Morgan and Webster19). PRIME uses population estimates, disease-specific mortality data and risk factor data for diet, physical activity smoking and BMI by sex and 5-year age groups to generate estimates on the effect of population behaviour change on changes in mortality(Reference Scarborough, Harrington and Mizdrak20). Estimates are generated by comparison of a ‘baseline’ scenario comprising existing mortality rates and risk factor levels with a ‘counterfactual’ scenario comprising alternative risk factor levels. PRIME is built on a parameterised framework between modifiable risk factors (such as smoking, diet and physical activity levels), clinical risk factors (such as blood pressure) and mortality outcomes (changes in numbers and rates of disease-specific deaths due to non-communicable diseases). PRIME parameters are derived from meta-analyses of published studies and are described in detail elsewhere(Reference Scarborough, Harrington and Mizdrak20); see the online supplementary material, Supplemental Table S1, for the key assumptions of the model.
Two PRIME models were run separately: (i) the ‘metropolitan’ model was used to determine expected changes in CVD and IHD mortality within the metropolitan population of Australia if they were to meet public health recommendations for diet, alcohol intakes, physical activity and tobacco smoking (see Table 1); and (ii) the ‘rural’ model was used to determine changes in CVD and IHD mortality in rural populations under the same counterfactual scenario, where everyone met public health recommendations in rural areas.
Table 1 PRIME risk factor data requirements and the public health counterfactual scenario level entered into both the metropolitan and rural model
The metropolitan population was defined as all individuals living in areas classified as a ‘major city’ by the 2011 Australian Statistical Geography Standard Remoteness Areas (ASGS-RA)(21). The rural population was defined as individuals living in areas classified as outside a major city by the same standards, which includes inner regional, outer regional, remote and very remote areas.
Population data
Population estimates by sex and 5-year age groups (from 15–19 years up to ≥ 85 years) for Australian major cities (metropolitan) and outside major cities (rural) were obtained from the 2011 Australian census(22).
Risk factor data
The metropolitan model baseline scenario was the observed level of modifiable risk factors as reported by the 2011–2012 National Nutrition and Physical Activity Survey (NNPAS), a component of the Australian Health Survey (AHS), for individuals classified as living in a major city(14). The AHS is the largest, most comprehensive survey ever conducted in Australia and includes sampling of private dwellings across all population subgroups in order to obtain a representative sample(14). The sampling is across all socio-economic groups, ethnicities, cultural backgrounds and geographical areas (excluding very remote areas)(14). The rural model was the same risk factor data for individuals living outside a major city. Data for alcohol intake, smoking and physical activity were obtained using the Australian Bureau of Statistics’ TableBuilder platform to obtain mean risk factor levels by 5-year age groups, sex and rurality. Dietary data were obtained by request from the Australian Bureau of Statistics’ Microdata, and means and standard deviations for energy (kcal/d), fruit (g/d), vegetables (g/d), fibre (g/d), dietary cholesterol (mg/d), salt (g/d), total fat (% of energy intake), saturated fat (% of energy intake), monounsaturated fat (% of energy intake) and polyunsaturated fat (% of energy intake), and the percentage of people who consumed less than one serving of fruit and vegetables daily, were derived using the statistical software package Stata SE version 15 (2017). Table 1 shows the PRIME inputs required for each risk factor, by 5-year age bracket and sex. Implausible dietary intakes were excluded if the participant had a ratio of reported energy intake to BMR of less than 0·9, as recommended by the Australian Bureau of Statistics(14). Mean BMI by 5-year age group and sex was also calculated from the AHS for the metropolitan and rural populations and entered into the separate models.
Mortality data
Data on the number of deaths due to CVD (International Classification of Diseases, tenth revision (ICD-10) codes: I00–I99) and IHD (ICD-10 codes: I20–I25) by state or territory and remoteness by sex and 5-year age group, for the year 2011, were requested from the Australian Institute of Health and Welfare’s National Mortality Database. Cause of Death Unit Record File data are provided to the Australian Institute of Health and Welfare by the Registries of Births, Deaths and Marriages and the National Coronial Information System (managed by the Victorian Department of Justice) and include cause of death coded by the Australian Bureau of Statistics. The data are maintained by the Australian Institute of Health and Welfare in the National Mortality Database. Remoteness area is based on area of usual residence – Statistical Area Level 2 (SA2) – classified according to the Australian Statistical Geography Standard (ASGS) 2011 Remoteness Structure. The PRIME model accounts for all CVD under the ICD codes 100–199, and less preventable conditions are accounted for internally in the model (e.g. rheumatic heart disease and pulmonary embolism)(Reference Scarborough, Harrington and Mizdrak20).
Baseline and counterfactual scenarios entered into the models
For both models (metropolitan and rural), the baseline scenario was the current level of risk factor data. The counterfactual scenarios (or scenario under investigation) was that the population achieved the level of modifiable risk factors recommended for optimal public health in Australia (Table 1). The ‘recommended’ levels for the counterfactual scenarios were based on the current Australian Guide to Healthy Eating(5), Nutrient Reference Values(23) and the Australian Government Department of Health guidelines for physical activity(24) and alcohol intake(25). The proportion of the population reported to be current smokers in the AHS became ex-smokers in the counterfactual scenario and added to the current ex-smoking rate in both the rural and metropolitan models, so there were 0% current smokers in the population under the counterfactual scenario. Table 1 includes the modelled recommendations and sources. The counterfactual scenarios assumed that total energy intake, energy balance and weight status did not change as a result of the changes to other behaviours.
Secondary analysis: 100% of population ‘never smoked’
A secondary counterfactual analysis was used to understand the impact of a 100% non-smoking scenario, in which no one in the population had ever taken up smoking. This scenario was a completely non-smoking scenario, where there would be 100% non-smokers in the population.
Uncertainty analysis
Monte Carlo simulations are built into PRIME to generate 95% credible intervals (CrI) around the outputs of mortality estimates generated under the counterfactual scenario. CrI for the current analysis were generated using 10 000 iterations. The intervals produced are based only on the uncertainty within the PRIME parameters, and not on the variability of the data used as inputs for the model. Due to the scope of the current analysis, it was not feasible to calculate t tests of proportions between proportions of deaths save by different risk factors. Hypothesis tests are not feasible to conduct with simulated data, as there are many sources of uncertainty that are not related to probability theory and assumptions in the structure of models like PRIME.
Results
Changes in mortality
Under the counterfactual scenario, in which the Australian population met all public health recommendations, CVD deaths were reduced by 40% in both metropolitan and rural areas (Table 2). The models estimated that each year 9673 (95% CrI 8135, 11 044) CVD deaths would be avoided in metropolitan Australia and 5219 (95% CrI 4491, 5852) CVD deaths in rural Australia. Significantly greater reductions in the number of CVD deaths among males than females were predicted in both metropolitan and rural populations (P < 0·001). Greater proportional reductions in IHD were predicted but were again similar between metropolitan (−52·8%) and rural (−52·9%) areas. Males living in metropolitan areas would experience the greatest reduction in IHD deaths (−55·9%).
Table 2 CVD and IHD deaths in rural and metropolitan Australia by sex at baseline and the changes observed under the counterfactual scenario that the population achieved the level of modifiable risk factors recommended for optimal public health, in adults over 15 years, 2011
CrI, credible interval.
Proportion of deaths delayed or averted attributable to meeting each of the recommendations
Figure 1 shows differences in the proportions of deaths saved for CVD and IHD by each recommendation for both rural and metropolitan areas. Under the counterfactual scenario, rural populations would save a higher proportion of CVD deaths as a result of meeting recommendations for fat and salt intakes when compared with their metropolitan counterparts (Fig. 1 and Table 3). Conversely, a higher proportion of CVD deaths would be averted in metropolitan areas as a result of meeting recommendations for fruit and vegetable servings, fibre intake and alcohol consumption. For IHD there were no differences in the proportion of IHD deaths saved as a result of meeting recommended levels of alcohol consumption and fibre; however, more deaths would be saved from reducing smoking, fats and salt in rural areas.
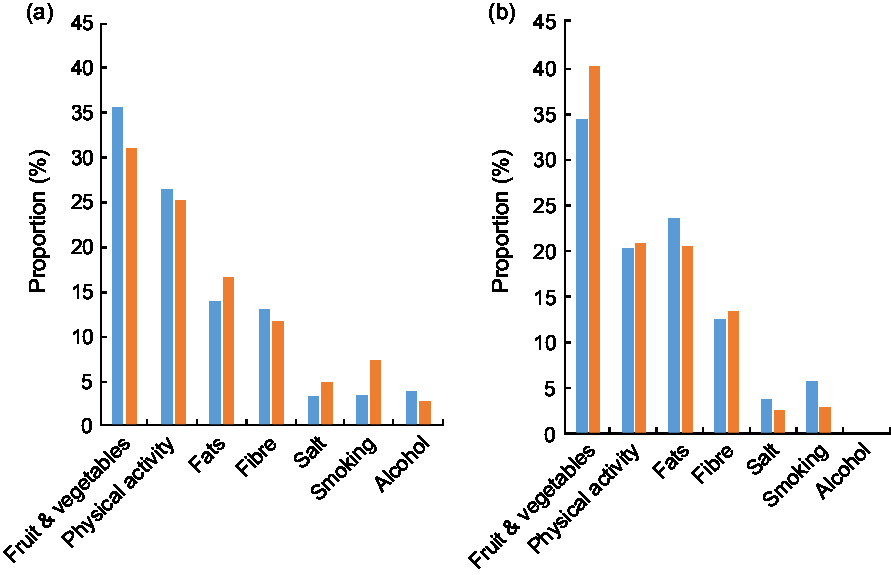
Fig. 1 Proportions of total (a) CVD deaths and (b) IHD deaths saved by rurality (![]() , metropolitan areas;
, metropolitan areas; ![]() , rural areas) and public health recommendation under the counterfactual scenario that the population achieved the level of modifiable risk factors recommended for optimal public health in Australia
, rural areas) and public health recommendation under the counterfactual scenario that the population achieved the level of modifiable risk factors recommended for optimal public health in Australia
Table 3 Differences in the order of priorities to prevent both CVD and IHD in rural and metropolitan Australia based on differences in proportions of deaths averted attributable to recommendations
Bold font indicates differences in the order of priority for risk factors between rural and metropolitan Australia.
There were no differences in the proportion of deaths saved from CVD and IHD as a result of meeting physical activity recommendations between the two populations, showing that if physical activity recommendations were met across Australia, rural and metropolitan areas would benefit equally.
Overall, the order of policy priorities in meeting recommendations to achieve the highest reduction in CVD and IHD mortality was different for rural and metropolitan populations, based on the proportion of deaths saved due to changes in each risk factor. Achieving recommended fruit and vegetable intakes alone would lead to the highest benefit for rural and metropolitan populations for both CVD and IHD (Table 3).
Achieving sufficient physical activity would be the second priority for both populations for the greatest CVD reductions, followed by meeting recommendations for fat and fibre intake. Reducing smoking would be a higher priority in rural Australia and conversely meeting alcohol recommendations would be a higher priority for metropolitan areas.
For larger reductions in IHD, after meeting fruit and vegetable intakes, reducing consumption of fats would be a higher priority in rural Australia when compared with metropolitan areas.
Inequalities between rural and metropolitan areas under the modelled scenarios
Figure 2 shows the baseline relative risks (RR) for both CVD and IHD mortality in rural compared with metropolitan areas and the change in absolute deaths rates per 100 000 population under both the baseline and counterfactual scenarios. Under the counterfactual scenario, the RR for CVD among the rural population would be unchanged due to similar proportional reductions in mortality from CVD in both areas. The online supplementary material, Supplemental Table S2, details baseline and counterfactual death rates per 100 000 by sex, with corresponding RR. Among males, the rural–metropolitan RR of CVD death would increase slightly under the counterfactual scenario from 1·34 to 1·35, but among females would stay essentially stable.
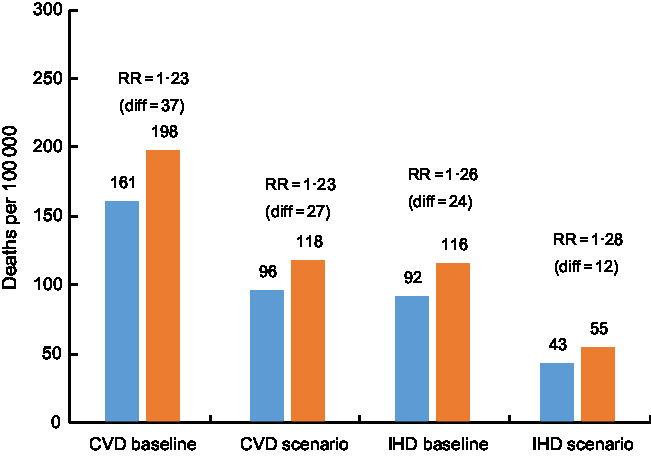
Fig. 2 Deaths per 100 000 from CVD and IHD by rurality (![]() , metropolitan areas;
, metropolitan areas; ![]() , rural areas) at baseline and under the counterfactual scenario that the population achieved the level of modifiable risk factors recommended for optimal public health in Australia. See online supplementary material, Supplemental Table S2, for full data and breakdown by sex (diff, absolute difference in death rates per 100 000 between rural and metropolitan areas; RR, relative risk)
, rural areas) at baseline and under the counterfactual scenario that the population achieved the level of modifiable risk factors recommended for optimal public health in Australia. See online supplementary material, Supplemental Table S2, for full data and breakdown by sex (diff, absolute difference in death rates per 100 000 between rural and metropolitan areas; RR, relative risk)
The difference in CVD death rates between metropolitan and rural Australia would reduce from 37 deaths per 100 000 to 22 deaths per 100 000 under the counterfactual scenario. For IHD the absolute mortality gap would halve, from 24 deaths per 100 000 people to 12 deaths per 100 000 (Fig. 2).
Secondary analysis: 100% non-smoking scenario
In the secondary analysis of 100% non-smoking in the population (a potential future scenario in Australia), the results showed an additional 5% of CVD deaths would be delayed or averted in rural areas (total reduction 45·1% from baseline) compared with an additional 3% in metropolitan areas (−43·3% from baseline; online supplementary material, Supplemental Table S3).
Discussion
If the Australian population met public health recommendations for diet, physical activity, alcohol consumption and smoking, there would be similar reductions in the total proportion of CVD and IHD deaths in rural areas when compared with metropolitan areas. Despite large estimated reductions in mortality for both populations, meeting public health recommendations would not eradicate the mortality gap that exists for both CVD and IHD between rural and metropolitan Australia. Due to similar proportional improvements in both areas, the total relative risk for CVD mortality in the rural population would remain the same under the counterfactual scenario and the IHD mortality RR would increase slightly. However, the absolute difference in death rates for CVD and IHD between metropolitan and rural areas would reduce by up to half, demonstrating that achieving recommendations for modifiable risk factors would reduce but not fully eradicate the substantial inequalities in CVD and IHD between the two populations. This is consistent with earlier modelling work which demonstrated that a substantial proportion of excess risk in rural areas could not be attributed to modifiable risk factors(Reference Alston, Peterson and Jacobs9).
The present study showed that achieving the recommended levels of fruit and vegetable intakes would achieve the highest benefit for reducing CVD and IHD across both metropolitan and rural Australia, a finding supported by earlier estimates showing that low fruit and vegetable consumption contributes a substantial amount (22%) of the total fatal and non-fatal IHD burden in Australia(13) and preventable disease mortality in Canada(Reference Belanger, Poirier and Jbilou10). A similar modelling study, using PRIME in the UK, also found fruit and vegetable intakes to be the most significant modifiable contributor to the burden of CVD, with fruit, vegetable and energy intakes being the principal determinants of geographic inequalities across Scotland, Wales and Ireland(Reference Scarborough, Morgan and Webster19). The current study predicted significant differences by rurality in the reductions in deaths attributable to specific risk factor improvements, showing higher benefit in rural areas from addressing fat and salt intakes when compared with their metropolitan counterparts.
Critically, for the risk factors considered here, the present study provides evidence that the order of policy priorities for public health recommendations to reduce CVD and IHD may be different between rural and metropolitan areas. Priority setting for the prevention of CVD and IHD needs to acknowledge differences between rural and metropolitan areas and the differing barriers to meeting public health recommendations. Meeting dietary guidelines has been shown to be more difficult in rural areas due to reduced access to the core food groups and the increased expense of these foods(Reference Cuttler, Evans and McClusky26, Reference Godrich, Lo, Davies and Darby27). A recent study in regional areas in the state of Victoria showed that the cost of a healthy food basket was highest in areas more than 15 km from a major regional centre(Reference Cuttler, Evans and McClusky26), with similar results shown in other studies in different states across regional and remote Australia(Reference Godrich, Lo, Davies and Darby27). Similarly, populations in rural areas may experience different constraints to metropolitan areas in meeting physical activity recommendations of 30 min of moderate physical activity five times per week(Reference Cleland, Hughes and Thornton28). A recent study by Cleland et al. (Reference Cleland, Hughes and Thornton28) highlighted that urban-centric interventions aimed at increasing physical activity are unlikely to be applicable to rural Australia, due to differences in the socio-ecological environments and subsequent influence on exercise behaviours in rural areas(Reference Cleland, Hughes and Thornton28, Reference Cleland, Hughes and Thornton29).
The use of three comprehensive, high-quality and nationally representative data sets as inputs for this model (Census, AHS and Australian Institute of Health and Welfare’s National Mortality Database) is a significant strength of the present study. The AHS did not, however, sample remote and very remote populations, where remoteness is known to be associated with reduced access to fresh foods and impact on health behaviours(Reference Godrich, Lo, Davies and Darby27, Reference Rogers, Ferguson and Ritchie30). As remote and very remote areas include 2·3% of Australia’s population, the number of deaths from CVD and IHD that could be prevented may be underestimated if the levels of risk factors among populations in these areas are not considered(21). The risk factor data used in the current analysis were self-reported, which carries multiple limitations and includes the potential for underestimations of risk factors for both populations(14). Detailed national population data on nutrient intakes are not routinely collected in Australia; the most recent suitable data, as used in the present study, were collected in 2011–2013 and may not accurately represent current dietary patterns in Australia. Dietary intake data on refined sugars(Reference Narain, Kwok and Mamas31) and trans-fat intakes(Reference de Souza, Mente and Maroleanu32) that are associated with increased CVD mortality are also not accounted for in the model and may lead to underestimations of potential lives saved. PRIME uses the strongest available evidence on the links between modifiable risk factors and chronic disease mortality; however, in many cases, where systematic reviews of randomised controlled trials are not available, the parameters are still subject to the limitations of observational epidemiology, leaving some of the estimates vulnerable to substantial uncertainty. The model also assumes a steady state without consideration of the time taken to achieve either the behaviour changes or the expected benefits, and there may be substantial lag times between population behaviour change and impact on mortality rates, and these lag times may impact on the assessment of priorities. The model also only considers mortality; therefore policy priorities may be very different if considering the total health burden in rural and metropolitan Australia. Although there are important differences between these populations, there are equally very many similarities and there is no expectation of any meaningful differences that may be likely to induce bias. The data used for risk factor estimates between rural and metropolitan Australia had largely the same distributions and differences in correlation structure; however, these are not likely to significantly affect the results of the separately run models.
To achieve public health recommendations for diet, physical activity, smoking and alcohol remains an ongoing challenge across the globe, regardless of rurality. The present study shows that achievement of these recommendations would have very substantial benefits, potentially saving tens of thousands of lives annually, providing support for prioritising policies and programmes to support these behaviours, even in the context of limited financial resources. Modelling studies stratifying analyses by rurality provide additional insights to understand how behaviour change interventions may maximise benefits of public health interventions and consider the unique circumstances of rural populations. Analysis by rurality assists with evidence to promote the incorporation of differences between metropolitan and rural populations into health policy and action.
Finally, it is important to note that public health recommendations do not necessarily reflect the absolute minimum risk that can be achieved and further benefits may accrue with additional improvements in risk behaviours. Recommendations are set based on scientific evidence of associations in risk reductions for chronic disease, but are also influenced by a range of other factors including, for instance, public acceptability, evidence on population-level nutritional deficiencies and food supply assessments(5, 23). For example, additional vegetable consumption beyond the recommended minimum level (5 servings/d) would be expected to result in even larger mortality reductions than the results presented here. A recent meta-analysis of thirteen studies showed that with every 400 g/d increment of vegetable intake, IHD risk was reduced by 18%, suggesting further mortality reductions could be achieved by exceeding the guidelines(Reference Gan, Tong and Li33). A similar case is observed for fibre, with every 10 g increase of fibre intake resulting in continued decreases in the RR for IHD mortality, and therefore exceeding this modelled scenario would translate to a further decrease in risk(Reference Pereira, O’Reilly and Augustsson34).
Conclusion
The achievement of public health recommendations for diet, physical activity and smoking in Australia would result in large decreases in CVD and IHD mortality for both rural and metropolitan populations. Despite improvements in overall CVD and IHD mortality under this scenario, an excess burden of CVD burden would persist for rural populations. Increasing vegetable intake would have by far the largest impact on mortality rates in both populations; however, additional priorities differ between rural and metropolitan Australia and higher priority should be placed on addressing fat intake in rural areas.
Acknowledgements
Acknowledgments: The authors thank Peter Scarborough and the team who created the PRIME model used in this research. Financial support: S.A. is a researcher on the National Health and Medical Research Council (NHMRC) Centre for Research Excellence in Obesity Policy and Food Systems (grant number APP1041020) and the NHMRC Centre for Research Excellence in Food Retail Environments for Health (grant number APP1152968). The NHMRC had no role in the design, analysis or writing of this article. Conflict of interest: None to declare. Authorship: All of the authors contributed substantially to the manuscript and meet criteria for authorship. Ethics of human subject participation: This study was approved for exemption from ethics review by the Deakin University Ethics Committee due to the use of publicly available, de-identified data in the study.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/S136898001900199X







