Since 1980, the prevalence of overweight and obesity in children and adolescents has increased dramatically in developed countries, and overweight and obesity is now reaching lower- and middle-income countries, with prevalence rates among these populations growing relatively faster( Reference Ng, Fleming and Robinson 1 – 4 ). In Brazil, 22·1 % of boys and 24·3 % of girls under 20 years of age were overweight or obese in 2013( Reference Ng, Fleming and Robinson 1 ). This has serious health implications because obesity is an established risk factor for diseases such as type 2 diabetes, CVD, cancer and numerous psychological and physiological issues, especially in childhood( Reference Ng, Fleming and Robinson 1 – 4 ). Changes in dietary intake, such as higher consumption of ultra-processed foods including artificial juices, fast foods and sugary snacks, and lower consumption of traditional foods such as fruits and vegetables, are important contributors to current pandemics in obesity and related chronic diseases( Reference Monteiro, Levy and Claro 5 – Reference Mondini and Gimeno 7 ).
Broad changes in the wider food and physical activity environment certainly influence children’s eating behaviour and weight( Reference Monteiro, Levy and Claro 5 – 8 ). However, parents are also important environmental agents, as children depend on them for food availability, access and preparation( Reference Gevers, Kremers and de Vries 9 – Reference Birch and Doub 11 ). Child eating behaviour is moulded from the first years of life and is known to be associated with parental feeding practices such as ‘Modelling’, ‘Restriction’, ‘Pressure to Eat’, ‘Monitoring’ and using ‘Food as Reward’( Reference Birch and Doub 11 , Reference Musher-Eizenman and Kiefner 12 ). Specifically, research suggests that the use of ‘Monitoring’ is related to positive outcomes, such as lower consumption of non-core foods( Reference Haycraft and Blissett 13 ), higher consumption of healthy foods( Reference Haszard, Skidmore and Williams 14 ) and greater physical activity( Reference Arredondo, Elder and Ayala 15 ). ‘Healthy Eating Guidance’ has also been associated with higher intake of fruits and vegetables, and lower intake of junk food( Reference Haszard, Skidmore and Williams 14 , Reference Bost, Wiley and Fiese 16 ). In contrast, less frequent use of these practices has been associated with greater weight gain in children( Reference Bost, Wiley and Fiese 16 ).
Relatively little is known about how such parental feeding practices contribute to broader dietary patterns associated with overweight. The WHO( 17 ) recommends taking a dietary pattern approach to dietary analysis rather than examining nutrients or foods in isolation. Studying complete diets by examining whole food patterns may provide a more accurate picture of the real world, since people eat meals comprised of a variety of foods and nutrients in combination, and is likely to be more informative in the investigation of diet–disease relationships as the interactions and synergistic effects of foods and nutrients are accounted for( Reference Choi, Joung and Lee 18 – Reference Zhang, Wang and Wang 20 ). In addition, translating population food behaviours into a simple measure of dietary patterns provides a public health message that is clearer and easier to follow than recommendations on individual foods and nutrients( Reference Slattery 21 ).
The aim of the present was therefore to identify food patterns of 2–9-year-olds and then to investigate sociodemographic, anthropometric and behavioural predictors of less healthy food patterns, including parental feeding practices. We hypothesized first that a pattern of ultra-processed food intake would emerge from the factor analysis, and second that the ultra-processed food pattern would be associated with (i) greater use of the parental feeding practices ‘Restriction’ and ‘Emotion Regulation/Food as Reward’ and (ii) lesser use of the parental feeding practices ‘Healthy Eating Guidance’ and ‘Monitoring’.
Methods
Participants
Parents of children aged 2–9 years were eligible for the present study. Children with diseases that were related to nutrition and/or could influence parental feeding practices were excluded, as were older siblings, to avoid sample unit duplication (155 were excluded). To estimate sample size, a type I and a type II probability of error of 0·05 and 0·20, respectively, were considered. The prevalence of overweight among children was used for this estimation, which resulted in a required sample size of 320 respondents, incorporating over-recruitment to accommodate an anticipated loss of 10 % of the original sample.
Procedures
Forty-eight private schools in Campinas and São Paulo, SP, Brazil were invited to participate in the study. Of the sixteen schools that accepted the invitation, fourteen were selected for the current sample, while the other two were selected for piloting. Survey packets containing the questionnaire and instructions requesting completion within two weeks by one of the parents were left in each classroom for distribution to eligible children. In one school, the questionnaires were administered and completed by parents before a parent–teacher meeting. More details about the procedures are described elsewhere( Reference Mais, Warkentin and Latorre 22 , Reference Warkentin, Mais and Latorre 23 ).
Measures
Dietary data were obtained using an FFQ especially developed for the present study and tested in a pilot study, since there was no instrument validated in Brazil that met our criteria of being both brief and appropriate for this age group. Parents were asked to answer the FFQ with reference to their child’s food intake for the 7d before the interview. Nineteen categories of foods were included, based on their association with obesity, their high intake frequency in the Brazilian population and recommendations of the Dietary Guidelines for the Brazilian Population( Reference Louzada, Martins and Canella 24 , 25 ). These were: artificial juice, beans, breakfast cereal, cereal, chips, chocolate milk, crackers/biscuits/cakes with and without filling, dairy desserts, fast food, fruits, ice cream/popsicles, instant noodles, meat and eggs, milk and dairy, processed meat, soft drinks, sugary snacks and vegetables. The response format was: ‘not consumed’, ‘1–2 times/week’, ‘3–4 times/week’, ‘5–6 times/week’ and ‘every day’.
Parents additionally completed questions on sociodemographic factors (maternal and child age, child’s sex, maternal education, family income) and provided anthropometric information (height and weight) for mother and child. Questions regarding parental perceived responsibility for child feeding were taken from the Child Feeding Questionnaire (CFQ)( Reference Birch, Fisher and Grimm-Thomas 26 ); responses were given on a 5-point Likert scale ranging from ‘never’ to ‘always’. Parental feeding practices were measured using a validated Brazilian adaptation of the Comprehensive Feeding Practices Questionnaire (CFPQ)( Reference Mais, Warkentin and Latorre 22 , Reference Warkentin, Mais and Latorre 23 ), which included the following six factors.
-
1. ‘Healthy Eating Guidance’: assesses how parents guide their child through encouragement, modelling and teaching about nutrition, as well as the influence of parents’ involvement and healthy environments; e.g. ‘Do you encourage your child to eat healthy foods before unhealthy ones?’
-
2. ‘Monitoring’: assesses how much parents keep track of the unhealthy foods their child eats; e.g. ‘How much do you keep track of the sweets (candy, ice cream, cake, pies, pastries) that your child eats?’
-
3. ‘Restriction for Weight Control’: assesses the degree to which parents restrict their child’s food intake to limit or control their child’s weight gain; e.g. ‘I encourage my child to eat less so he/she won’t get fat’.
-
4. ‘Restriction for Health’: assesses how much parents restrict their child’s food intake to influence their child’s health; e.g. ‘If I did not guide or regulate my child’s eating, he/she would eat too much of his/her favourite foods’.
-
5. ‘Emotion Regulation/Food as Reward’: assesses parents’ use of food to regulate their child’s emotions and/or as a reward for desirable behaviours; e.g. ‘When your child gets fussy, is giving him/her something to eat or drink the first thing you do?’
-
6. ‘Pressure’: investigates how much a parent pressures their child to eat; e.g. ‘My child should always eat all of the food on his/her plate’.
Responses were given on a 5-point Likert scale ranging from 1=‘never’ to 5=‘always’ or from 1=‘disagree’ to 5=‘agree’. Additional behavioural questions assessed screen time (hours during a day) and screen use during mealtimes (yes or no) by the child. All data were double-entered with the help of two trained assistant researchers.
Statistical analysis
First, we ran descriptive analyses to explore the data set and choose appropriate cut-offs for dichotomization of variables of interest. Then, to derive food patterns, we conducted factor analysis on FFQ data, using oblique rotation, since the factors were hypothesized to correlate. To retain a factor, we required eigenvalues greater than 1 and coefficients greater than 0·30 in the correlation matrix. Since the ultra-processed food pattern emerging from this analysis included foods high in fat, sugar and salt, whose frequent and excessive consumption increases the risk for non-communicable diseases, we then conducted analyses of predictors of this food pattern. Specifically, we calculated factor scores by taking the mean of the factor and transforming it to a scale ranging from 0 to 100, where greater scores represented higher consumption of foods comprising the factor. Since these factor scores were not normally distributed according to the Kolmogorov–Smirnov test, we decided to dichotomize the score, using the 33rd centile as the cut-off, based on the data distribution. The same method was used to dichotomize CFPQ factors into groups representing scores ≤66th centile v. >66th centile for positive feeding practices (‘Healthy Eating Guidance’ and ‘Monitoring’) and scores of ≤33rd centile and >33rd centile for negative feeding practices (‘Restriction for Weight Control’, ‘Restriction for Health’, ‘Emotion Regulation/Food as Reward’ and ‘Pressure’), such that greater scores represented higher use of the parental feeding practice. We then ran a series of univariate analyses using ultra-processed food pattern score group as the dependent variable, and dichotomized sociodemographic, anthropometric and behavioural characteristics, including the factors derived from the Brazilian version of the CFPQ, as independent variables. Finally, to establish independent effects of implicated factors, we ran a multivariate logistic regression model, requiring P≤0·20 for the inclusion of predictor variables, using the stepwise forward entering method. Statistical significance in the final model was defined as P≤0·05. All statistical analyses were performed using the statistical software package Stata version 14.0 (2015).
Results
Response rates at the school level ranged from 32 to 46 %, resulting in an average of 38 %. Of the total of 2426 distributed survey packets, 1084 (44·68 %) were returned. Of the remaining 1342 (55·32 %) questionnaires, 1273 were not returned, ten could not be used due to very incomplete data and fifty-nine could not be used due to missing data from the FFQ. Of the returned questionnaires, a total of 155 were excluded. Of these 155, exclusions occurred due to the index child having a disease related to nutrition and/or that may interfere in parental feeding practices (n 28), or due to the questionnaire being completed about a child not in the eligible age range (n 30), by a respondent who was not the parent of the child (n 11), by parents not born in Brazil (n 3), about a sibling of another child in the survey (n 79), about a child for whom a questionnaire had already been completed (n 2), or due to responses being evidently copied from the questionnaire of another participant (n 2). This resulted in 929 valid questionnaires, which represented 85·70 % of the returned questionnaires and 38·29 % of those distributed. The majority of the respondents were mothers (91·39 %; data not shown).
As shown in Table 1, almost 32 and 20 % of the children drank chocolate milk and artificial juice every day, respectively, while less than half of the sample reported a daily intake of vegetables and almost one in every four children did not consume this food group three or more times per week. Almost a quarter of children were frequent consumers (three or more times per week) of processed meat and more than a third were frequent consumers of sugary snacks. Consumption of both fruits, and milk and dairy was high among our sample, with about 60 and 75 %, respectively, consuming these food categories three or more times per week.
Table 1 Children’s food intake in the 7d preceding questionnaire completion, as assessed by parent-reported FFQ, in a sample of 2–9-year-old children (n 929) from Campinas and São Paulo, SP, Brazil, April–June 2014

Two food patterns emerged from the factor analysis, as demonstrated in Fig. 1. The first pattern (‘traditional food’) consisted of six food groups: meat, grains, beans, milk and dairy, vegetables and fruits. The second (‘ultra-processed food’) included six different food groups: fast food, artificial juice, chips, sugary snacks, crackers/biscuits/cakes with filling and vegetables (reversed coded); 621 children showed a high intake of ultra-processed foods.
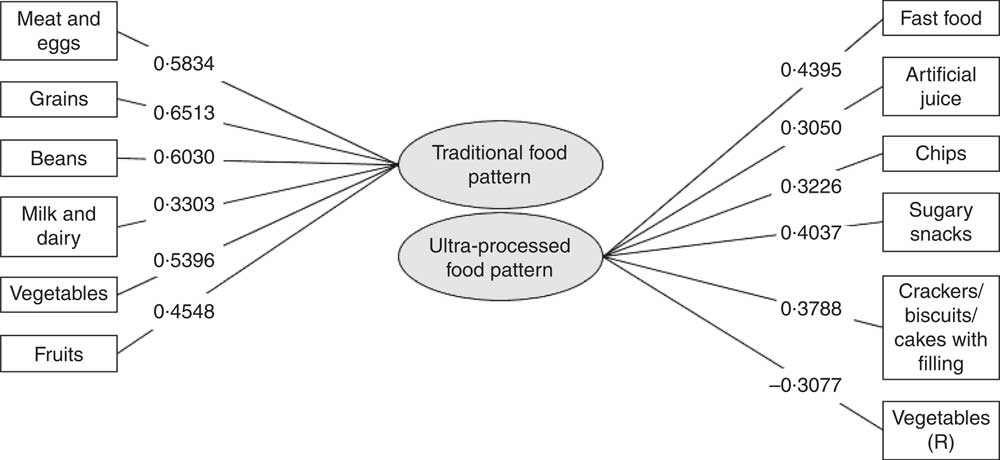
Fig. 1 Factor loadings for selected foods loading on the two major dietary patterns identified from FFQ data in a sample of 2–9-year-old children (n 929) from Campinas and São Paulo, SP, Brazil, April–June 2014 (note: R=reversed item)
Descriptive statistics and bivariate analyses of relationships between high scores on the ultra-processed food pattern and hypothesized sociodemographic, anthropometric and behavioural predictors are shown in Table 2. Regarding child sociodemographic, anthropometric and behavioural characteristics, children who were older, had higher body mass (BMI Z-score), used screen devices for more than 2 h/d or used screen devices while eating demonstrated greater risk of high ultra-processed food intake. Regarding parent sociodemographic, anthropometric and behavioural characteristics, lower maternal education, lower income and higher maternal BMI were associated with a greater likelihood of high ultra-processed food intake. Parents who perceived themselves as less responsible for child’s portion size and child’s adequacy of food group intake were more likely to have a child with high ultra-processed food intake. Among the parental feeding variables, lower scores in ‘Healthy Eating Guidance’ and ‘Monitoring’ were both associated with a higher likelihood of high ultra-processed food intake by the children of the sample.
Table 2 Descriptive statistics and bivariate analyses of relationships between parent and child predictors and likelihood of high ultra-processed food intake in a sample of 2–9-year-old children (n 929) from Campinas and São Paulo-SP, Brazil, April–June 2014
Values in bold are P≤0·05.
* Chi-square test.
† Brazilian minimum wage in 2014: R$724·00 ($US 321·77).
Table 3 shows the final multivariate model for prediction of the ultra-processed food pattern adjusted for child’s sex and BMI Z-score, and maternal age. This model revealed that children who used screen devices during mealtimes had a greater likelihood of high ultra-processed food intake. Further, less educated and overweight mothers had children with a greater risk of high ultra-processed food intake. Parents who perceived themselves as less responsible for child’s adequacy of food group intake and who used less ‘Healthy Eating Guidance’ and ‘Monitoring’ also had children with increased risk.
Table 3 Multivariate analyses showing independent predictors of the ultra-processed food pattern in a sample of 2–9-year-old children (n 886) from Campinas and São Paulo, SP, Brazil, April–June 2014

Adjusted for child’s sex and BMI Z-score, and maternal age.
Discussion
The present study aimed to use data from a large survey of parents of 2–9-year-olds in Brazil to identify food patterns among children and to investigate associations between an emerging ultra-processed food pattern and a range of child and parental predictors, namely child and maternal sociodemographic and anthropometric characteristics, and behavioural characteristics including parental feeding practices. As hypothesized, the factor analysis resulted in two food patterns: ‘traditional food’ and ‘ultra-processed food’. The latter was negatively associated with positive parental feeding practices such as ‘Healthy Eating Guidance’ and ‘Monitoring’, and positively associated with lower maternal education, higher maternal weight status, lower perceived parental responsibility for adequacy of food group intake and higher child’s screen use during mealtimes. However, we did not find any association between coercive parental feeding practices, such as both kinds of ‘Restriction’ and ‘Emotion Regulation/Food as Reward’, and the less healthy food pattern.
Descriptive analyses of intake frequency for individual food groups demonstrated high consumption of sugary snacks, chocolate milk and processed meat, which is likely to be distally driven by factors such as their palatability and aggressive promotion in large portions, motivated in turn by their profitability due to extended shelf-life and ease of transportation in parallel with their inherent appeal( Reference Martins, Levy and Claro 27 ). Notably, chocolate milk and artificial juice were the most consumed foods in our sample. This might be because parents associate these products with milk and fruit and consider them a part of a healthy diet( Reference Ferrarezi, Santos and Monteiro 28 ). However, this provides some cause for concern as both products are actually considered sugar-sweetened beverages, which contribute significantly to empty calories in the diet( Reference Te Morenga, Mallard and Mann 29 ). That said, traditional foods from the Brazilian diet (milk and dairy, grains, meat and eggs, fruits, beans and vegetables), which are rich in a variety of micronutrients essential for child growth and development, were consumed by most of the children almost every day. We cannot rule out the possibility that these reports were driven by social desirability( Reference Falcão-Gomes, Coelho and Schmitz 30 ). However, the relatively high intake frequency we observed could also be explained by awareness of the benefits of a healthier diet in this relatively well educated, high-income sample( Reference Fernández-Alvira, Mouratidou and Bammann 31 , Reference Farias Júnior and Osório 32 ).
Factor analysis of FFQ data resulted in two food patterns. The first pattern was composed of meat and eggs, grains, beans, milk and dairy, vegetables and fruits, all of which categories represent a traditional Brazilian diet and include natural and minimally processed foods from the ‘basic food basket’ (an attempt to ensure minimal nutrition for low-income populations( Reference Dishchekenian, Escrivão and Palma 33 )). Notably, although cheese and bread are technically classified as processed foods( 25 , Reference Dishchekenian, Escrivão and Palma 33 ), these items were also present in this emerging food pattern, which we labelled the ‘traditional food’ pattern.
The second food pattern was composed of fast food, artificial juice, chips, sugary snacks, crackers/biscuits/cakes with filling and vegetables (reverse coded), and was therefore labelled the ‘ultra-processed food’ pattern. The presence of this last item in the ultra-processed food pattern reflects the inverse relationship between vegetables and ultra-processed food intake in this sample, which was also demonstrated in a recent Brazilian study of dietary trends over the last three decades( Reference Martins, Levy and Claro 27 ). Some foods that were expected to load on this factor, such as chocolate milk, crackers/biscuits/cakes without filling, breakfast cereal, dairy desserts, processed meat, soft drinks, instant noodles and ice cream/popsicles, did not show high enough correlations with the remaining foods to reach the minimum loading value, suggesting that the six surviving products were sufficient to represent the ultra-processed food pattern here( Reference Salvatti, Escrivão and Taddei 34 ). All the products with positive loadings are commonly consumed away from home (e.g. at school, during leisure time)( Reference Dishchekenian, Escrivão and Palma 33 ) and contain large amounts of sugar, salt, saturated and total fat, and small quantities of protein and fibre( Reference Martins, Levy and Claro 27 ) – a pattern of dietary composition which can lead to high levels of LDL cholesterol and blood pressure, and low levels of HDL cholesterol( Reference Dishchekenian, Escrivão and Palma 33 ). Consistent with our results, many other dietary pattern studies have extracted factors similar to the ultra-processed food pattern we found here, although different labels have been used (e.g. ‘Western’( Reference Choi, Joung and Lee 18 ), ‘junk food’( Reference Pinho, Silveira and Botelho 35 ), ‘processed food’( Reference Rothausen, Matthiessen and Andersen 36 ), ‘obesogenic’( Reference Santos, Fiaccone and Barreto 37 ), ‘snacking’( Reference McDonald, Baylin and Arsenault 38 ), ‘unhealthy diet’( Reference Borghese, Tremblay and Katzmarzyk 39 ), ‘fast/convenience’( Reference Kaiser, Aguilera and Horowitz 40 ) and ‘high fat and sugar’( Reference McNaughton, Mishra and Stephen 41 )).
In terms of child characteristics, we found that screen use during mealtimes was associated with a greater likelihood of high ultra-processed food intake (OR=1·61; P=0·004). This may be partly attributable to exposure to television advertisements for foods which are high in fat, sugar and salt, poor in fibre and micronutrients, and have been shown to be linked to sedentary activities such as the use of electronic devices (televisions, tablets and computers)( Reference Borghese, Tremblay and Katzmarzyk 39 , Reference Lioret, Touvier and Lafay 42 , Reference Araújo, Teixeira and Gaio 43 ). Additionally, the excessive use of screen devices during mealtimes could be an indicator of parents’ lack of interaction with the child during mealtimes( Reference Bost, Wiley and Fiese 16 ), which could reflect a more general lack of household structure, which has been shown to be a risk factor for poor quality of diet( Reference Bost, Wiley and Fiese 16 , Reference Lloyd, Lubans and Plotnikoff 44 , Reference Jarman, Inskip and Ntani 45 ).
Regarding maternal factors, low maternal education conferred twice the risk of the child engaging in high ultra-processed food intake (OR=2·05; P=0·010). Similar relationships have been observed in other studies( Reference Fernández-Alvira, Mouratidou and Bammann 31 , Reference Araújo, Teixeira and Gaio 43 , Reference Kalantari and Doaei 46 – Reference Smith, Emmett and Newby 49 ), and may be because education is related to beliefs and leads to greater access to information and knowledge, which in turn leads to greater awareness of the negative consequences of ultra-processed food intake and the importance of healthy diets in early childhood( Reference Peters, Dollman and Petkov 50 – Reference Shrewsbury and Wardle 52 ). Notably, because of its relative stability, greater validity and easiness to measure, education has been used as a good indicator of socio-economic status, while income is more liable to change and more likely to have non-response( Reference Shrewsbury and Wardle 52 , Reference Krieger, Williams and Moss 53 ). Income includes several components other than wage earnings, which makes it hard to measure it. Besides, income tends to be poorly reported by individuals with high incomes, such as those included in the present sample( Reference Krieger, Williams and Moss 53 ). Socio-economic status could influence ultra-processed food intake since healthy foods are more expensive than ultra-processed foods. However, maternal education, not family income, emerged as the independent predictor in our multivariate model, possibly because this was a sample with relatively high socio-economic status and we did not have sufficient variance in income to observe income effects. Moreover, parental education has been found to be more consistently protective against adiposity, which is linked to dietary intake, when compared with other socio-economic status markers( Reference Krieger, Williams and Moss 53 ).
Additionally, we found that overweight/obese mothers tend to have children who consume more ultra-processed foods (OR=1·43; P=0·044). This was also reported by Araújo and colleagues (2015) in a study of Portuguese adolescents( Reference Araújo, Teixeira and Gaio 43 ), and could be due to the higher probability of obese mothers modelling unhealthy diets to their children, as well as providing greater amounts of these foods in the home( Reference Canella, Levy and Martins 54 ). Such processes could underlie the strong relationship between mother and child obesity, which has been observed elsewhere, including in another Brazilian study based in São Paulo using school-aged children( Reference Ribeiro, Taddei and Colugnatti 55 ).
Our observation of a relationship between healthier child eating patterns and parents’ perceived responsibility for child’s adequacy of food group intake further suggests that the parental involvement and supportive behaviour for child nutrition reflected by the endorsement of this item is likely to confer benefits to the child’s diet. In support of this theory, recent literature suggests that uninvolved parents have children who are more willing to eat energy-dense foods and less willing to eat fruits, vegetables and dairy foods( Reference Gevers, Kremers and de Vries 9 , Reference Hoerr, Hughes and Fisher 56 ).
Finally, our study revealed that children whose parents reported lower use of ‘Healthy Eating Guidance’ (guiding the child through encouragement, modelling and teaching about nutrition, as well as providing a healthy food environment) and ‘Monitoring’ (keeping track of the unhealthy foods their child eats) had a greater chance of having a high ultra-processed food intake (OR=1·83; P<0·001 and OR=2·52; P<0·001, respectively). It is also consistent with the results of studies using the CFPQ in other populations showing associations between higher ‘Healthy Eating Guidance’ and ‘Monitoring’ scores and child unhealthy snack food intake( Reference Haszard, Skidmore and Williams 14 ) and between higher ‘Modelling’ scores and lower intake of chips( Reference Kalantari and Doaei 46 ). Additionally, the consumption of grains in that study was related to the use of ‘Encourage Balance and Variety’, ‘Modelling’ and ‘Teaching about Nutrition’, CFPQ factors that compose the ‘Healthy Eating Guidance’ factor emerging in the current data set, while higher consumption of soft drinks was associated with the lower use of ‘Involvement’( Reference Kalantari and Doaei 46 ). Using other tools to measure parental feeding practices, some studies have also observed positive relationships between ‘Monitoring’ and ‘Modelling’ and healthy eating habits, and negative associations between these positive practices and unhealthy eating habits( Reference Arredondo, Elder and Ayala 15 , Reference Kröller and Warschburger 57 , Reference Vereecken, Haerens and De Bourdeaudhuij 58 ). Studies focusing on positive parental feeding practices are scarce and our results therefore contribute to the literature by suggesting that these types of behaviour could have positive effects in terms of decreasing children’s unhealthy food intake( Reference Kröller and Warschburger 57 ).
Contrary to expectations, we did not find associations between dietary patterns and coercive feeding practices. A possible explanation is that in our sample, positive parental feeding practices had more impact on child food intake than negative parental feeding practices. Also, we did not see an association between dietary patterns and child weight status. Previous findings have also been inconsistent regarding this result: while some studies have also been unable to find this relationship( Reference Field, Austin and Gillman 59 , Reference Coelho, Cândido and Machado-Coelho 60 ), others have reported a positive association between overweight and unhealthy dietary patterns( Reference Santos, Fiaccone and Barreto 37 , Reference McDonald, Baylin and Arsenault 38 , Reference Lioret, Touvier and Lafay 42 ) or a negative relationship with healthy dietary patterns( Reference Lioret, Touvier and Lafay 42 ). Different findings may be due to different definitions of food patterns or statistical method used to extract factors. However, another possible explanation for the lack of association in our data could be that young children have not been exposed to unhealthy diets long enough for an effect on weight to be apparent. Nevertheless, the cumulative effect of inadequate food intake and lifestyle could still be important for the later development of obesity and cardiovascular risk( Reference Mikkilä, Räsänen and Raitakari 61 ).
The present study had some limitations. For example, these cross-sectional results cannot demonstrate cause-and-effect relationships between dietary patterns and obesity risk. Our response rate was relatively low, and unfortunately we did not have access to information on the parents and students who did not return the questionnaires, so are unable to evaluate the degree to which our study sample was representative of the schools selected. However, notably, other studies involving parents in private schools published in the literature have achieved similar response rates( Reference Nowicka, Sorjonen and Pietrobelli 62 , Reference Musher-Eizenman, Lauzon-Guillaim and Holub 63 ) and the large sample size we obtained gave us enough power to detect associations of interest. The homogeneity of our sample, although it allows a good estimate of behaviours among this relatively high socio-economic status sample, precludes generalization to low-income populations.
Child food intake was assessed using an FFQ, which is liable to recall bias and social desirability, but is widely used in epidemiological research( Reference Pereira and Sichieri 64 ). As we could not find an FFQ validated within a Brazilian population that was short and specific for pre-school and school-aged children, we had to create one for the present study. However, we included the most frequent foods consumed by the Brazilian population and ultra-processed foods known to be obesity markers based on a literature review( Reference Louzada, Martins and Canella 24 ). Although the FFQ we used does not measure food portions, previous research has demonstrated that the majority of variation in food intakes is captured by frequency of consumption( Reference Noethlings, Hoffmann and Bergmann 65 ). Since the food intake data in the present study were provided by the parents, we were unable to measure children’s food consumption at times when they were away from home. We may therefore underestimate children’s food intake, particularly of unhealthy snacks, and our data could reflect parents’ impressions rather than real diets( Reference Entin, Kaufman-Shriqui and Naggan 66 ). However, parents of young children tend to keep close track of their child’s food intake and the types of foods eaten outside the home tend to be similar to those eaten at home( Reference Northstone and Emmett 47 ). Additionally, it is difficult for young children to report on their own food consumption due to cognitive and attentional limitations, as well as a lack of vocabulary for types of foods and food portions( Reference Falcão-Gomes, Coelho and Schmitz 30 ).
The determination of dietary patterns is necessarily affected by sample characteristics and dietary assessment methods used (e.g. FFQ, 24 h dietary recall, food record). Because of that, any comparisons with previous results should be made with caution. Statistical procedures for factor extraction (e.g. factor analysis, principal component analysis, cluster analysis) can also affect results, especially since the details of factor analysis methods are based on subjective and arbitrary decisions including grouping of food items, the number of factors to be extracted, the method of rotation and the labelling of the dietary patterns( Reference Martínez, Marshall and Sechrest 67 ). For example, using a different factor loading cut-off could reveal other dietary patterns within the data set, although these would explain less variance than the first emerging patterns( Reference Rothausen, Matthiessen and Andersen 36 ). It should also be noted that results from factor analysis have proven difficult to replicate in other populations, although our dietary patterns are certainly comparable to those emerging in other populations using the same method( Reference Denova-Gutiérrez, Castañón and Talavera 68 ).
On the other hand, it is also important to highlight some strengths of the present study. Our large sample size of parents of 2–9-year-old Brazilian children maximized our ability to detect reliable dietary patterns and robust associations with our hypothesized predictors. Further, the present study is the first to evaluate associations between dietary patterns among pre-school and school-aged children in Brazil and parental feeding practices assessed by a comprehensive questionnaire that was translated and validated for this specific population.
Conclusions
The present study identified two different dietary patterns among 2–9-year-old children: ‘traditional food’ and ‘ultra-processed food’, and highlighted a number of sociodemographic, anthropometric and behavioural predictors of high ultra-processed food intake, namely maternal education, maternal BMI, perceived responsibility for child’s adequacy of food group intake, the parental feeding behaviours ‘Healthy Eating Guidance’ and ‘Monitoring’, and child’s screen use during mealtimes. Because eating habits develop during childhood and contribute to lifelong food consumption, it is important to understand which practices promote healthy food patterns and which populations are at risk of unhealthy food patterns, so that tailored policies and programmes can be developed and then targeted at populations who stand to benefit the most. Our results suggest that intervention efforts should be developed for high-risk groups such as families with overweight and less educated mothers, focusing on encouraging parents to take responsibility for promoting healthy eating for their children and to use positive feeding practices such as encouragement and modelling of healthy eating, teaching about nutrition, provision of a healthy food environment and keeping track of unhealthy foods their child eats. Further studies using longitudinal designs will be necessary to fully explore the impact of such behaviours on children’s long-term dietary patterns and weight trajectories.
Acknowledgements
Acknowledgements: Data collection was performed at schools in Campinas and São Paulo, SP, Brazil. The authors thank the participating schools, parents and children for their valuable contribution. Financial support: This work was supported by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), with scholarships for L.A.M. and S.W.; by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK; grant number R00DK088360) with funding for S.C.; by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) and by the Office of the Director (OD), National Institutes of Health (NIH; grant number U54HD070725) to the Global Obesity Prevention Center (GOPC) at Johns Hopkins University with funding for S.C., L.A.M. and S.W.; and by the Conselho Nacional de Pesquisa (CNPq) with a productivity scholarship for J.A.A.C.T. The funders had no role in the design, analysis or writing of this article. Conflict of interest: None. Authorship: L.A.M., S.W. and J.A.A.C.T. designed the research; L.A.M., S.W. and J.B.V. conducted the research; L.A.M., S.W., M.R.D.O.L., S.C. and J.A.A.C.T. analysed the data; and L.A.M., S.W., J.B.V. and S.C. wrote the paper. All authors read and approved the final manuscript. Ethics of human subject participation: This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects/patients were approved by the Federal University of São Paulo (UNIFESP) ethics committee. Written informed consent was obtained from all subjects/patients.







