Cu, an essential mineral nutrient, plays important roles in many metabolic processes, including neuropeptide synthesis, antioxidant defense and immunologic functions(Reference Bonham, O’Connor and Hannigan1,Reference Uriu-Adams and Keen2) . At the same time, Cu can also be toxic in excessive amounts via oxidation and production of free radicals(Reference Cai, Koropatnick and Cherian3,Reference Cai, Tsiapalis and Cherian4) , which have the potential to cause oxidative damage to lipids, proteins, DNA and other molecules. Accordingly, a recent study in general Chinese adults found that there was a U-shaped relation of dietary Cu intake with new-onset hypertension(Reference He, Li and Liu5), which is one of the most important causes of morbidity and mortality. However, although mortality is the most important indicator of health, findings about the relation between Cu levels and mortality risk from prospective cohort studies are still mixed and limited(Reference Bates, Hamer and Mishra6–Reference Grammer, Kleber and Silbernagel13). Some studies had examined the association between blood Cu concentrations and the risk of mortality, but the results were inconsistent(Reference Mohammadifard, Humphries and Gotay9–Reference Grammer, Kleber and Silbernagel13). The prior studies(Reference Bates, Hamer and Mishra6–Reference Kałuza, Dołowa and Roszkowski8) that examined the relation of dietary Cu intake and mortality also reported discrepant findings. Of note, few related studies, using the dietary Cu intake data continuously, have been conducted, which may provide more granular information and allow for the possibility of non-linear relation of dietary Cu intake and mortality. Overall, to date, the association between dietary Cu intake and mortality risk remains uncertain.
To provide evidence to bridge the above knowledge gaps, our current study aimed to evaluate the association between dietary Cu intake and the risk of all-cause mortality in general population, using data from the China Health and Nutrition Survey (CHNS) – a national ongoing open cohort in China.
Methods
Population and study designs
The data and materials that support the discoveries of this study are available at the official website (http://www.cpc.unc.edu/projects/china) of the CHNS, which is an ongoing multipurpose, prospective open-cohort project initiated in 1989 in China, with a response rate of 88 % at individual level(Reference Popkin, Du and Zhai14). The CHNS was scheduled for follow-up every 2 to 4 years, with its implementation in 1989, 1991, 1993, 1997, 2000, 2004, 2006, 2009, 2011 and 2015, respectively. By 2011, twelve provinces/autonomous cities and 288 communities were included, and people in these areas consisted of 47 % of the Chinese population(Reference Zhang, Zhai and Du15). The cohort profile and some of the major findings had been reported elsewhere(Reference Popkin, Du and Zhai14–Reference Zhang, Liu and Zhou20) in detail.
The current study included seven rounds of the CHNS data from 1997 to 2015. Person-waves were calculated as the sum of waves for each individual from entry to the last visit prior to the date of death, date of loss to follow-up or the end of follow-up. As shown in online Supplementary Fig. 1, among a total of 94 532 person-waves, we first excluded participants who were pregnant, <18 years of age (17 672 person-waves). Among the remaining participants, those who were surveyed in at least two study rounds were included (n 17 517, 68 057 person-waves), and the first survey round is considered as baseline. The included population did not differ in most of the baseline characteristics from those excluded (n 8443, 8443 person-waves) (online Supplementary Fig. 1, online Supplementary Table 1). Furthermore, individuals with missing dietary Cu intake, or with extreme dietary energy intakes (<600 kcal or >4200 kcal/d for males and <500 kcal or >3600 kcal/d for females) were also excluded(Reference Seidelmann, Claggett and Cheng21). At last, a total of 17 310 participants were included in the final analysis (online Supplementary Fig. 1).
The CHNS was approved by the National Institute of Nutrition and Food Safety, Chinese Center for Disease Control and Prevention and Institutional Review Boards at the University of North Carolina at Chapel Hill. Each participant provided written informed consent.
Assessments of dietary nutrient intakes
Dietary data in the study were obtained by well-trained nutritionists through an interview face to face in each survey round. The dietary diets were repeatedly assessed via three consecutive 24-h dietary recalls at the individual level and a food-weighing approach over the same 3 d at the household level. The three consecutive days were distributed from Monday to Sunday randomly and were almost equally in balance across the 7 d of the week. Nutrient intakes were calculated using the China food composition tables. The accuracy of 24-h dietary recall designed to evaluate the intake of energy and nutrient has been proven(Reference Zhai, Guo and Popkin22,Reference Zhai, Du and Wang23) . In each round, the average intakes of the 3-d dietary macronutrients and micronutrients were calculated.
Moreover, the cumulative average intake values of each nutrient were calculated for each subject, using all results up to the last visit prior to the date of death, or using all results among those alive throughout the follow-up (number of waves included during follow-up, median: 3·3; interquartile range, 2·0–5·0), to reflect long-term intake levels and minimise within-person variation. In our study, the residual method(Reference Willett and Stampfer24) was used to assess energy-adjusted intake for dietary Cu.
Assessments of covariates
Information on socio-demographic characteristics (age, sex, urban/rural residents, regions, education levels and occupations) and lifestyle behaviours (smoking and alcohol drinking status) were obtained through the structured questionnaires. Ever smokers and ever alcohol drinkers included former and current smokers and former and alcohol drinkers, respectively. Height and weight were measured based on a standard procedure with calibrated equipment. BMI was calculated as one’s weight in kilograms divided by the square of his height in metres (kg/m2).
Seated blood pressure was measured by trained research staff after the participants had rested for 5 min, using a mercury manometer, following the standard method. Triplicate measurements on the same arm were taken in a quiet and bright room. The mean systolic blood pressure (SBP) and diastolic blood pressure (DBP) of the measures in three independent days were used in analysis.
Study outcome
The study outcome was all-cause mortality. In each wave, information on health and death for every participant was recorded. The death status was recorded based on the report of household members in each survey wave. If someone died, household members were asked for the exact time of death. For any deaths reported more than once in different waves, the first report was chosen.
Statistical analysis
Population characteristics, presented as means (SD) for continuous variables and proportions for categorical variables according to quartiles of energy-adjusted dietary Cu intake, were compared by χ 2 tests for categorical variables and ANOVA tests for continuous variables.
The year of each participant’s first entry into the survey was considered as baseline. The follow-up person-time for each participant was calculated from baseline until the time of death, the last survey round before the participant’s departure from the survey or the end of the latest survey, whichever came first. Cox proportional-hazards model was used to estimate the relation of energy-adjusted dietary Cu intake with all-cause mortality, without and with adjustments for sex (males and females), age in years, BMI in kg/m2, ever alcohol drinking (yes and no), ever smoking (yes and no), education levels (illiteracy, primary school, middle school and high school or above), occupations (farmer, worker, unemployed and other), urban or rural residents (urban and rural), SBP in mmHg, DBP in mmHg, as well as the intakes of fat in g/d, protein in g/d and carbohydrate in g/d. To assess the proportional-hazards assumption, the significance of the interaction between exposures and follow-up time was assessed, and no clear evidence of violation was detected. Restricted cubic spline with three knots (at the 25th, 50th and 75th percentiles of energy-adjusted dietary Cu intake) was performed to test for linearity and visualise the dose–response relation of Cu intake and all-cause mortality.
Furthermore, possible modifications of the association between energy-adjusted dietary Cu intake and all-cause mortality were evaluated for the following variables: sex (males or females), age (<45 or ≥45 years), BMI (<24 or ≥24 kg/m2), ever alcohol drinkers (no or yes), ever smokers (no or yes), SBP (<120 or ≥120 mmHg), Zn intake (<10·7 (median) or ≥10·7 mg/d), protein intake (<64·2 (median) or ≥64·2 g/d), carbohydrate intake (<293·4 (median) or ≥293·4 g/d) and fat intake (<71·0 (median) or ≥71·0 g/d). Interactions between subgroups and dietary Cu intake were examined by likelihood ratio testing.
Sensitivity analyses were additionally conducted to examine the robustness of the results. First, further adjustments for the intakes of major food sources of Cu, including legumes, nuts, vegetables, fruits, seafoods and whole grains. Second, other micronutrients that are known as traditional or suspected risk factors for all-cause mortality, or related to energy-adjusted dietary Cu intake, were further adjusted, including dietary intakes of Na, potassium, Zn, Ca, Fe, Mg, Se, vitamin A, vitamin B1, vitamin B2, vitamin E and niacin. Third, we have further explored the association between dietary Cu intake (without energy adjustment) and all-cause mortality. Fourth, instead of using the cumulative average of diet, the association between baseline energy-adjusted dietary intake and all-cause mortality was also examined.
A two-tailed P < 0·05 was set to be statistically significant, and Bonferroni corrections were performed for multiple comparisons in Table 1 and Supplementary Table 2. Statistical analyses were performed by using R software, version 4.0.5 (http://www.R-project.org).
Table 1. Population characteristics by quartiles of energy-adjusted dietary copper intake
(Numbers and percentages; mean values and standard deviations)

Q, quartile.
* A P < 0·0014 was set to be statistically significant.
Results
Study participants and population characteristics
As shown in the flow chart (online Supplementary Fig. 1), a total of 17 310 participants were included in the current study. The average age of the study participants was 44·0 (sd 15·9) years. The mean dietary Cu intake was 1·9 (sd 0·5) mg/d.
Population characteristics of the study participants by dietary Cu intake quartiles are presented in Table 1 and Supplementary Table 2. Participants with higher dietary Cu intake were less likely to be urban residents and live in south regions, tended to have lower fat intake levels and higher intakes of carbohydrate, protein, potassium, Ca, Mg, Fe, Zn, Se, vitamin B1, legumes, nuts, vegetables, fruits, seafoods and whole grains.
Association between energy-adjusted dietary copper intake and risk of all-cause mortality
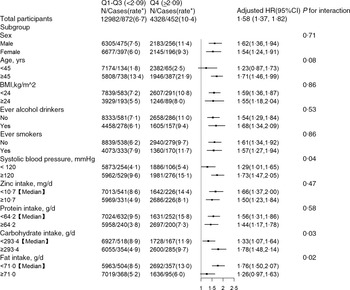
A total of 1324 (7·6 %) participants died during a median follow-up duration of 9·0 years (interquartile range, 4·1–15·2 years). Overall, the association between energy-adjusted dietary Cu intake and the risk of all-cause mortality followed a J-shape (Fig. 1, P for nonlinearity = 0·047). Accordingly, when energy-adjusted dietary Cu intake was assessed as quartiles, compared with those in the first quartile (<1·60 mg/d), the adjusted hazard ratios for all-cause mortality were 0·87 (95 % CI (0·71, 1·07)), 0·98 (95 % CI (0·79, 1·21)) and 1·49 (95 % CI (1·19, 1·86)), respectively, in participants in the second (1·60–<1·83 mg/d), third (1·83–<2·09 mg/d) and fourth (≥2·09 mg/d) quartiles (Table 2).
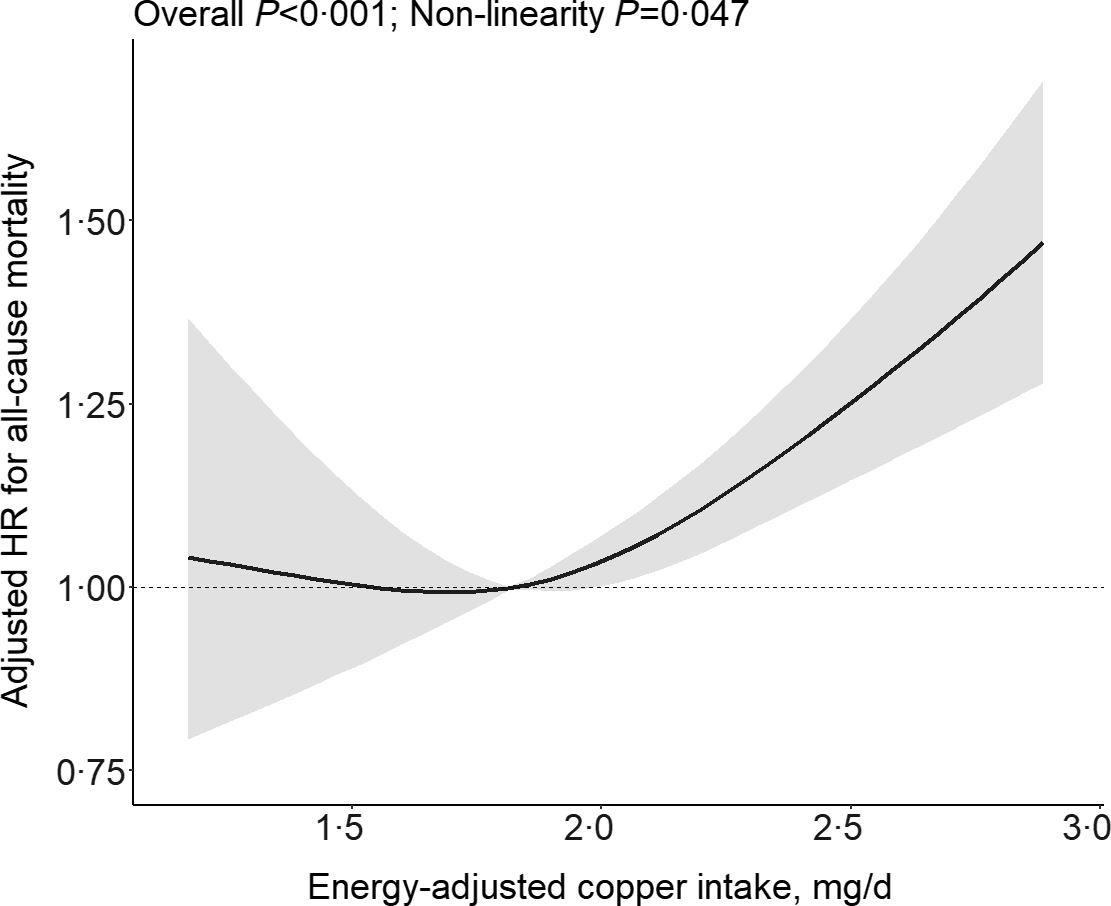
Fig. 1. Relation of energy-adjusted dietary Cu intake with risk of all-cause mortality based on restricted cubic splines. *Adjusted for sex, age, BMI, ever alcohol drinking, ever smoking, education levels, occupations, urban or rural residents, systolic blood pressure (SBP), diastolic blood pressure (DBP), as well as dietary intakes of fat, protein and carbohydrate.
Table 2. The association between energy-adjusted dietary copper intake and the risk of all-cause mortality
(Cases and incident rate; hazard ratio and 95 % confidence intervals)

Q, quartile.
* Incident rate is presented per 1000 person-years of follow-up.
† Adjusted for sex, age, BMI, ever alcohol drinking, ever smoking, education levels, occupations, urban or rural residents, systolic blood pressure (SBP), diastolic blood pressure (DBP), as well as dietary intakes of fat, protein and carbohydrate.
Further adjustments for the intakes of legumes, nuts, vegetables, fruits, seafoods and whole grains or dietary intakes of Na, potassium, Zn, Ca, Fe, Mg, Se, vitamin A, vitamin B1, vitamin B2, vitamin E and niacin did not materially alter the results (online Supplementary Table 3). Similar results were found for the relation of dietary Cu intake without energy adjustment (online Supplementary Fig. 2) and baseline energy-adjusted dietary Cu intake with all-cause mortality (online Supplementary Table 4).
Stratified analyses by potential effect modifiers
Due to the similar mortality risks in the 1–3 quartiles of dietary Cu, we combined the three quartiles into one group in the stratified analyses. Stratified analyses were performed to further assess the relations of energy-adjusted dietary Cu intake (≥2·09 mg/d (the 4 quartile) v < 2·09 (the 1–3 quartiles) mg/d) with the risk of all-cause mortality in total participants and various subgroups.
A significantly higher risk of all-cause mortality was found in participants in the fourth quartile of dietary Cu intake (≥2·09 mg/d) (HR 1·58; 95 % CI (1·37, 1·82)), compared with those in the 1–3 quartiles. Moreover, a stronger positive association between Cu intake and all-cause mortality was found in those with higher SBP (P for interaction = 0·04), lower dietary fat intake (P for interaction = 0·02) and higher dietary carbohydrate intake (P for interaction = 0·03). None of other variables, including sex, age, BMI, ever smokers, ever alcohol drinkers, Zn intake and protein intake, significantly modified the association between energy-adjusted dietary Cu intake and all-cause mortality (Fig. 2).
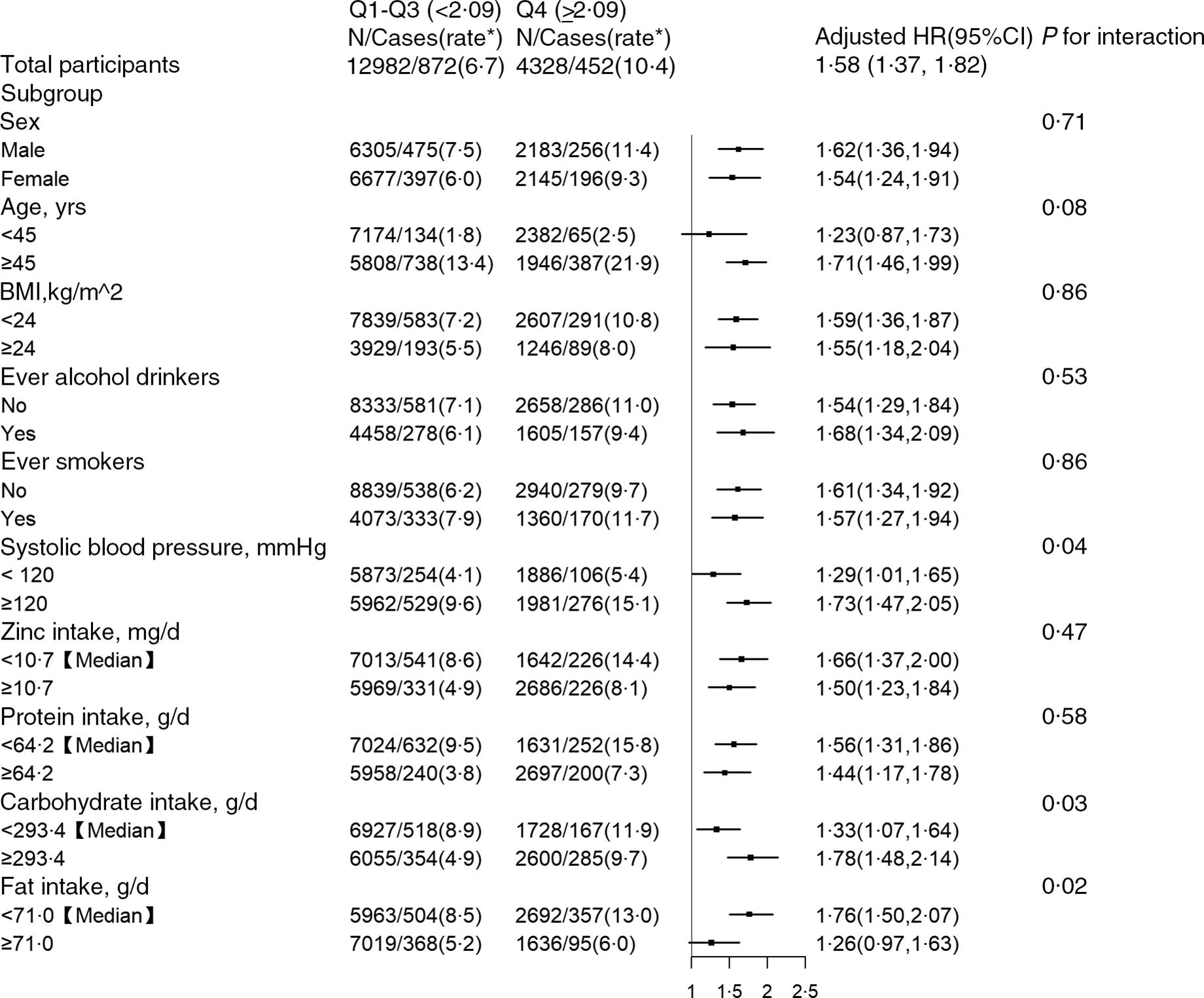
Fig. 2. Stratified analyses by potential effect modifiers for the associations between energy-adjusted dietary Cu intake and the risk of all-cause mortality in various subgroups. *Incident rate is presented per 1000 person-years of follow-up. Adjusted, if not stratified, for sex, age, BMI, ever alcohol drinking, ever smoking, education levels, occupations, urban or rural residents, systolic blood pressure (SBP), diastolic blood pressure (DBP), as well as dietary intakes of fat, protein and carbohydrate.
Discussion
In this prospective cohort of Chinese adults, we observed that there was a nonlinear, J-shaped association between energy-adjusted dietary Cu and all-cause mortality, where the rate of all-cause mortality seemed to plateaued at less than 2·09 mg/d, beyond which the rate monotonically increased.
The role of dietary Cu intake on the risk of all-cause mortality had been reported in a few previous studies and reported inconsistent results(Reference Bates, Hamer and Mishra6–Reference Kałuza, Dołowa and Roszkowski8). In the British National Diet and Nutrition Survey, higher dietary intakes of Cu (measured by a 4-d weighed diet estimate and without energy adjustment) were associated with lower all-cause mortality (HR 0·91; 95 % CI (0·84, 1·00)) in 1054 community-living participants aged 65 years and over during a follow-up period of 13–14 years(Reference Bates, Hamer and Mishra6). In the National Health and Nutrition Examination Survey from 1999 to 2010(Reference Chen, Du and Blumberg7), there was no significant association between dietary Cu intake (using 24-h diet recalls and without energy adjustment) and all-cause mortality in 30 899 USA adults aged 20 years or older during a median follow-up of 6·1 years. A previous study(Reference Kałuza, Dołowa and Roszkowski8) in the Warsaw region during spring 1999–31 December 2003 found that the all-cause mortality was higher among subgroup of elderly men with lower intake of Cu, which was collected using a 3-d record method, in 146 male participants. Overall, the above studies suggested that the association between dietary Cu intake and all-cause mortality remains uncertain. Of note, most of the previous studies did not consider the possible modifying effect of other dietary nutrients or other components of the primary dietary sources of Cu. More importantly, most of the previous studies reported mortality risk based on the categories of dietary Cu intake. Few related studies, using the dietary Cu intake data continuously, have been conducted, which may allow for presenting the non-linear association between Cu intake and all-cause mortality and provide more granular information. With a prospective cohort design, a relatively longer follow-up period and the use of three consecutive 24-h dietary recalls, our current study provided an opportunity to examine the continuous association between energy-adjusted dietary Cu intake and all-cause mortality in Chinese general population, with relatively comprehensive adjustments for a number of potential confounding factors and a series of stratified analyses.
Of note, the Cu levels (median: 1·83 mg/d) in our current study were higher than the dietary reference intakes for Cu (0·9 mg/d in adults)(Reference Mohammadifard, Humphries and Gotay9) of the Institute of Medicine and also was higher than that in French adults (means: male: 1·53 mg/d and female: 1·30 mg/d)(Reference Bost, Houdart and Oberli25) or USA adults (means:1·4 mg/d)(Reference Chen, Du and Blumberg7). The higher dietary Cu intake may be related to the different dietary habits of adults in Western countries and China. Chinese diets tend to include large amounts of grains and legumes(Reference Batis, Sotres-Alvarez and Gordon-Larsen26), which are major sources of dietary Cu(Reference Cui, Zhou and Liu27), while Western diets are animal-based and rich in red and processed meats(Reference Malesza, Malesza and Walkowiak28). It is giving us an opportunity to explore the association between relatively high levels of dietary Cu intake and all-cause mortality.
Our study yields some new insights. First, there was a nonlinear relation of Cu intake with all-cause mortality. Higher risk of all-cause mortality was found only in the highest quartile of Cu intake, and the effect of dietary Cu intake on the risk of all-cause mortality seemed to plateau in those in the 1–3 quartiles of dietary Cu intake, who may already have an adequate Cu intake. Consistently, our previous study also showed that in Chinese hypertensive patients, a significantly higher risks of first stroke were found in participants in the four quartile of plasma Cu, compared with those in the first quartile(Reference Zhang, Cao and Zhang29). Higher Cu may participate in reactions that result in the production of highly reactive oxygen species, leading to DNA damage, and direct oxidation proteins(Reference Cai, Koropatnick and Cherian3,Reference Tapiero, Townsend and Tew30,Reference Jomova and Valko31) . Moreover, Cu concentrations were directly associated with high-sensitivity C-reactive protein levels(Reference Bo, Durazzo and Gambino32). In addition, Cu may manifest the detrimental effects by substituting other metal cofactors from their natural ligands(Reference Tapiero, Townsend and Tew30,Reference Sarkar33) . Therefore, in excess of cellular demand, Cu can be detrimental.
We also found that SBP and dietary intakes of fat and carbohydrate may modify the relation between dietary Cu intake and all-cause mortality. A stronger positive association was found in those with higher SBP, lower dietary fat intake and higher carbohydrate intake, which suggested some protection against the apparent harm of high dietary Cu intake by lower SBP, higher fat intake and lower carbohydrate intake. However, in view of multiple testing and similar directionality of the associations, more studies are need to confirm our results and further examine the underlying mechanisms.
Notably, the relation of dietary Cu intake with all-cause mortality might be attributed to other components or some unclear nutrients of the primary dietary sources of Cu. However, our study showed that further adjustments for other major nutrients or the major food sources of Cu did not materially change our findings. In addition, a series of stratified analyses showed similar associations. These findings suggested that the relationship of Cu intake with all-cause mortality may be at least partly independent of these factors.
Potential limitations warrant consideration. First, although a number of dietary and non-dietary covariates had been adjusted, unmeasured and residual confounding factors remain possible. Second, there was no detailed data about dietary supplement use in our study. However, only 0·71 %, 0·03 % and 0·11 % of the Chinese population were reported taking nutrient supplements, multi-mineral and Cu supplements, respectively, according to the 2010–2012 China Nutrition and Health Surveillance(Reference Gong, Liu and Yao34) – a nationally representative and comprehensive cross-sectional study covering China’s thirty-one provinces, autonomous regions and municipalities. Given the low supplement proportion of nutrients, especially Cu, we speculated that our results may not be materially altered by the limited usage of dietary supplements. Third, the current study depended on the Cu data from the China food composition tables, which is unlikely to be able to account for regional variation in Cu contents of foods that might be caused by local conditions, including soil and water Cu concentration, slurry/manure spreading, agricultural and industrial contamination. Fourth, the data for cause-specific mortality in CHNS are lacking, which may provide additional implications for health promotion and prevention. Last but not least, our study was conducted in general Chinese population, whether the findings can be extrapolated to other populations with different characteristics needs further investigations. Owing to these limitations, further confirmation of the reported findings in future studies is necessary.
Conclusions
In the current study, there was a J-shaped association between dietary Cu intake and the risk of all-cause mortality in general Chinese adults. If further confirmed, we need to pay more attention to maintaining optimal dietary Cu intake levels for the prevention of premature death.
Acknowledgements
This research uses data from the CHNS. We thank the National Institute for Nutrition and Health, China Center for Disease Control and Prevention, Carolina Population Center (P2C HD050924 and T32 HD007168), the University of North Carolina at Chapel Hill, the National Institutes of Health (NIH; R01-HD30880, DK056350, R24 HD050924 and R01-HD38700) and the NIH Fogarty International Center (D43 TW009077 and D43 TW007709) for financial support for the CHNS data collection and analysis files from 1989 to 2015 and future surveys, and the China-Japan Friendship Hospital, Ministry of Health for support for CHNS 2009, Chinese National Human Genome Center at Shanghai since 2009 and Beijing Municipal Center for Disease Prevention and Control since 2011.
The study was supported by the National Key Research and Development Program [2022YFC2009600] and the National Natural Science Foundation of China [81973133, 81730019].
Dr. X. Q. had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. X. G., C. L. and X. Q. designed the research; X. G., P. H., M. L., C. Z., Q. M., Y. Z., C. Z., S. Y., Y. Z., Z. Y., R. L., Q. W. and X. Q. conducted the research; X. G., C. Z., C. Z. and C. L. performed the data management and statistical analyses; X. G. and X. Q. wrote the manuscript; all authors reviewed/edited the manuscript for important intellectual content. All authors read and approved the final manuscript.
There are no conflicts of interest.
Supplementary material
For supplementary material/s referred to in this article, please visit https://doi.org/10.1017/S0007114522002732