The Mediterranean diet (MD) pattern is widely known and considered a healthy diet option that involves the consumption of a wide variety of vegetables and cereals, low consumption of meat and dairy products, moderate consumption of wine during some meals, and olive oil as a source of fat. In overall terms, the MD pattern has been of great interest to many researchers because it seems to be positively associated with better health( Reference Sofi, Macchi and Abbate 1 ). In specific terms, the MD pattern has been observed to reduce the risk of CVD, metabolic syndrome, diabetes mellitus, chronic degenerative diseases, allergies and asthma, and has even been shown to reduce the risk of mental illnesses such as depression, anxiety and binge eating disorders( Reference Bertoli, Spadafranca and Bes-Rastrollo 2 – Reference Tangney, Kwasny and Li 9 ). Despite this, some authors conclude that it seems Mediterranean inhabitants are replacing MD healthy eating habits by consumption of more processed foods and saturated fat, and decreasing their intakes of plant foods and MUFA( Reference Farajian, Risvas and Karasouli 10 , Reference Naska and Trichopoulou 11 ). This trend is particularly evident among children and adolescents, who presented low rates of MD adherence( Reference Farajian, Risvas and Karasouli 10 , Reference Antonogeorgos, Panagiotakos and Grigoropoulou 12 – Reference Santomauro, Lorini and Tanini 16 ). Several authors have shown that about 50 % of Spanish children and adolescents presented good MD adherence( Reference Arriscado, Muros and Zabala 17 – Reference Martínez, Llull and Bibiloni 19 ), whereas in a recent study with participants from eight European countries, Tognon et al.( Reference Tognon, Hebestreit and Lanfer 20 ) found that Spanish school-aged girls showed the lowest prevalence of MD adherence. Furthermore, childhood and adolescence are considered critical periods for acquiring dietary and other important health habits. In this regard, several studies have observed that adherence to the characteristic MD pattern could be determined by a wide range of individual or social factors such as individuals’ nutritional knowledge, age, gender, food pricing, information provided on television, family habits, family socio-economic status (SES), parental education, parental birthplace and type of school, among others( Reference Cutler, Flood and Hannan 21 – Reference Lazarou and Kalavana 26 ). Arriscado et al.( Reference Arriscado, Muros and Zabala 17 ) found that children who attended state schools, children from immigrant families and children from families with medium-to-low SES were less likely to follow the MD pattern. Moreover, Grosso et al.( Reference Grosso, Marventano and Giorgianni 27 ) showed that adolescents living in urban areas presented less MD adherence. On the other hand, Costarelli et al.( Reference Costarelli, Koretsi and Georgitsogianni 28 ) found that children and adolescents with good adherence to the MD pattern also showed physical well-being, psychological well-being, a greater feeling of having enough age-appropriate freedom and a good perception of their parents and school environment. On the basis of these results, we agree with Arriscado et al.( Reference Arriscado, Muros and Zabala 17 ) who highlight the importance of identifying the factors that influence the level of adherence to the MD in order to be able to develop effective interventions and to reverse the unfortunate trend of young people giving up healthy eating habits related to the MD pattern( Reference Serra-Majem Ll and Ngo 29 ).
In addition to these studies, several other authors have also studied the relationship between MD adherence and anthropometric factors. There is some controversy regarding the relationship between obesity and MD adherence( Reference Buckland, Bach and Serra-Majem 30 ). Several studies have reported that overweight or obese children and adolescents showed significantly lower levels of MD adherence( Reference Tognon, Hebestreit and Lanfer 20 , Reference Lydakis, Stefanaki and Stefanaki 31 , Reference Schröder, Fitó and Estruch 32 ). Lydakis et al.( Reference Lydakis, Stefanaki and Stefanaki 31 ) conducted a cross-sectional study which concluded that overweight and obese children had significantly lower MD adherence levels in comparison to children with a normal BMI. Schröder et al.( Reference Schröder, Fitó and Estruch 32 ) also found the same tendency for the waist circumference variable. By contrast, Jennings et al.( Reference Jennings, Welch and Van Sluijs 33 ) suggested that diet quality is independently associated with children’s weight status. Following these results, Farajian et al.( Reference Farajian, Risvas and Karasouli 10 ) conducted a cross-sectional study with children from ten regions in Greece and they too found no association between MD adherence and anthropometric factors. On the other hand, Tognon et al.( Reference Tognon, Hebestreit and Lanfer 20 ) conducted a follow-up study and found that the MD pattern was inversely associated with childhood obesity. In this regard, in order to clarify the relationship between MD adherence levels and BMI, more follow-up studies should be conducted with large samples of children and adolescents to study their eating and lifestyle habits and their weight and psychological characteristics. It is important to highlight that overweight and obesity among children and adolescents is an increasingly serious public health problem worldwide( Reference Han, Lawlor and Kimm 34 ). Furthermore, it is not only related to physical health; several studies have found a relationship between overweight and obesity and the presence of emotional disorders in adults as well as children and adolescents( Reference Aparicio, Canals and Voltas 35 – Reference Goodman and Whitaker 37 ), although this relationship has yet to be established unequivocally( Reference Benson, Williams and Novick 38 ).
In the light of the above, the present study aimed to describe the prevalence of MD adherence in a community sample of adolescents, to determine the adolescents’ anthropometric, sociodemographic and psychopathological characteristics in relation to their level of MD adherence, and to assess the extent to which these factors contribute to or are associated with the risk of low MD adherence. Moreover, taking into account the possible relationship between emotional symptoms and BMI, we also aimed to use a mediational model to test whether low MD adherence may be a partial mediator of the association between emotional symptoms and high BMI. We hypothesized that the prevalence of MD adherence would be similar to that reported in other studies. We also hypothesized that individuals with lower MD adherence would present anthropometric alterations such as high BMI, more mental health problems such as an increased presence of emotional disorders or eating disorder symptoms, lower family SES or foreign nationality.
Materials and methods
Participants and procedure
A three-year longitudinal study was conducted among 245 subjects (147 girls and ninety-eight boys aged 12–15 years; mean age 13·5 (sd 0·9) years). The participants were recruited from a three-phase epidemiological study of anxiety and depression disorders in the town of Reus (a Spanish town of 100 000 inhabitants). The first phase took place during the 2006/2007 academic year, the second phase during the 2007/2008 academic year and the third phase during the 2009/2010 academic year.
Before beginning the study, the project was approved by the Universitat Rovira i Virgili’s ethics committee for research on individuals and by the Catalan Government’s Department of Education. A sample of subjects was then selected, and cluster sampling was conducted by randomly selecting a set of thirteen primary schools (seven state schools and six state-subsidized private schools) out of a total of twenty-six schools from all five representative areas of Reus (Catalonia, Spain). We then contacted the school boards, all of whom agreed to participate. After that, a letter was sent to all parents to inform them about the study and to ask for their written informed consent. We then conducted the study in three phases.
In the first phase of the study, the baseline sample was a group of 1514 subjects (794 girls and 720 boys; mean age 10·2 (sd 1·2) years). The subjects were selected from grades four (9–10 years old), five (10–11 years old) and six (11–12 years old) of primary school. Screening questionnaires for emotional disorder symptoms (the Screen for Child Anxiety Related Emotional Disorders (SCARED) and the Children’s Depression Inventory (CDI)) were used to select a sample at risk of emotional disorders and a risk-free control sample. Also, in the first phase we assessed anthropometric and sociodemographic data. In the second phase, the sample consisted of 562 subjects (308 girls and 254 boys), of whom 405 were at risk of emotional disorders and 157 were controls. In the control group, one child without risk of emotional psychopathology was selected for every three children at risk of emotional psychopathology, matching for age, gender and type of school. All the participants of the second phase were contacted in the three-year follow-up although 43·6 % dropped out. Of the 245 subjects who agreed to participate in the third phase, 241 (147 girls and ninety-four boys) completed the Krece Plus food questionnaire to determine MD adherence, and they also answered four subscales of the Eating Disorder Inventory-2 (EDI-2), five categories of the Youth’s Inventory-4 (YI-4) and the Krece Plus short physical activity test. We also assessed their anthropometric and body composition data.
There were no psychopathological differences between the subjects who participated in the third phase and the subjects who dropped out in this last phase of the study. However, there were differences related to SES: participants with a low SES were associated with higher drop-out rates than medium- or high-SES participants (P=0·001).
The participants completed the questionnaires in groups of three or four. Researchers were present to instruct the children on how to answer the surveys and to answer any queries. The anthropometric and body composition measurements were made individually to ensure the participants’ privacy.
Instruments and measurements
Krece Plus food questionnaire
The Krece Plus food questionnaire( Reference Serra-Majem, Aranceta-Bartrina and Ribas-Barba 39 ) determines dietary quality. It consists of sixteen items, with a score of 1 or −1 for each item. The maximum possible score is 11 and the minimum is −5. The participants were classified into three categories according to their total score on the questionnaire; their adherence to the MD was thus classified as high (total score ≥9), medium (total score 6–8) or low (total score ≤5). This test was administered in phase 3.
Krece Plus short physical activity test
The Krece Plus short physical activity test( Reference Román-Viñas, Serra-Majem and Ribas-Barba 40 ) consists of two questions for quick screening of the physical activity/inactivity level. Each question has six possible responses, with a score of 0–5. The maximum score for the test is 10 and the minimum is 0. According to the total score on the questionnaire, individuals are classified into three categories of physical activity level: good (total score of 9–10 for boys and 8–10 for girls), fair (total score of 6–8 for boys and 5–7 for girls) and bad (total score ≤5 for boys and ≤4 for girls). This test was administered in phase 3.
Anthropometry
The anthropometric parameters evaluated in the initial and final phase were weight, height and waist circumference. Weight was measured using the Tanita® TBF-300 scale, which has an accuracy of 100 g and a maximum weight of 200 kg. Waist circumference was measured using a flexible tape and height was measured using an inextensible tape measure, with a variation of 1 mm considered acceptable. Waist was measured at the midpoint between the iliac crest and the lower costal margin, without clothes. Weight and height were measured in a school room, with participants in bare feet, wearing light clothing and with no heavy objects in their pockets. BMI (kg/m2) was then calculated. We used the International Obesity Task Force cut-off points to classify participants according to their BMI as underweight, normal weight, overweight and obese( Reference Cole, Bellizzi and Flegal 41 , Reference Cole, Flegal and Nicholls 42 ).
Bioelectrical impedance
The Tanita® TBF-300 body composition analyser was used to assess body composition. The results were expressed as body fat percentage.
Screen for Childhood Anxiety and Related Emotional Disorders
The SCARED( Reference Birmaher, Khetarpal and Brent 43 ) is a forty-one-item self-report questionnaire that assesses anxiety disorder symptoms in children and adolescents aged 8–18 years. Participants were asked about the frequency of each symptom on a 3-point Likert-type scale: 0 (almost never), 1 (sometimes) and 2 (often). The Spanish version has a reliability of α=0·86 and consists of four factors: somatic/panic, social phobia, generalized anxiety and separation anxiety( Reference Vigil-Colet, Canals and Cosi 44 ). A score of 25 was considered to be the cut-off point for risk of anxiety( Reference Birmaher, Brent and Chiappetta 45 , Reference Canals, Hernández-Martínez and Cosi 46 ). The SCARED was administered in all three phases.
Children’s Depression Inventory
The CDI( Reference Kovacs 47 , Reference Del Barrio and Carrasco 48 ) is a twenty-seven-item self-report inventory for assessing depression in individuals aged 7–17 years old. The children selected the sentence that best described them over the two previous weeks. The reliability of this version has been reported to be good (α=0·81–0·85)( Reference Figueras, Amador-Campos and Gómez-Benito 49 ) and was shown to be so in the present study (α=0·83). A score of 17 was considered to be the cut-off point for risk of depression( Reference Canals, Martí-Henneberg and Fernández-Ballart 50 ). The CDI was administered in phases 1 and 2.
Youth’s Inventory-4
The YI-4( Reference Gadow and Sprafkin 51 ) is a 120-item self-report rating scale that evaluates the symptoms described in the Diagnostic and Statistical Manual of Mental Disorders IV for emotional and behaviour disorders in youths aged 12–18 years. To obtain our results, we considered the following categories: attention deficit hyperactivity disorder, anxiety, depression, conduct disorder and eating disorder. In the present study we used the Spanish version of the YI-4, which demonstrated satisfactory internal consistency (α=0·95) in our sample. The YI-4 was administered in phase 3.
Eating Disorder Inventory-2
The EDI-2( Reference Garner 52 ) is a ninety-one-item self-report measure of the cognitive and behavioural characteristics commonly associated with anorexia nervosa and bulimia nervosa. Responses are made on a 6-point Likert-type scale ranging from ‘never’ to ‘always’. We used twenty-nine of the ninety-one items from the four subscales (‘Drive for thinness’, ‘Bulimia’, ‘Body dissatisfaction’ and ‘Perfectionism’). In the present study the EDI-2’s internal consistency was α=0·80. The EDI-2 was administered in phase 3.
Sociodemographic questionnaire
A sociodemographic questionnaire designed by the authors for the study was used to assess the sociodemographic characteristics of the sample. The children answered questions about age, gender, place and date of birth, family type and parental occupation. This information was corroborated by their parents. SES was established using the Hollingshead index( Reference Hollingshead 53 ), which determines an individual’s social status by placing his/her occupation into one of nine categories (from unskilled work to highly skilled work) and his/her level of education into one of seven categories (from non-completed primary education to completed higher education). The status score is estimated by multiplying the occupation scale value by a weight of 5, the education scale value by a weight of 3 and then combining the two scores. For the current study, family SES was determined by combining the data obtained from the father and the mother. The scores ranged from 0 to 66; therefore, to obtain three categories (low, medium and high) we considered scores below 22 to be low SES, those between 23 and 44 to be medium SES, and those above 44 to be high SES. This questionnaire was administered in phase 1.
Statistical analyses
Statistical analysis was performed using the statistical software package IBM SPSS Statistics Version 22·0.
We analysed descriptive data of the sociodemographic, anthropometric, MD adherence, physical activity and psychopathological variables by gender. We therefore used the χ 2 test and Student’s t test depending on the types of variables compared.
The χ 2 test was also applied to study the relationship between sociodemographic and anthropometric characteristics from the third phase and MD adherence level. We carried out ANOVA, adjusted for the Bonferroni multiple comparisons, by gender, to explore the way in which physical activity and psychopathological factors may be related to MD adherence.
Logistic regression models adjusted for age, gender, SES and the risk/control variable were applied in order to assess which variables predicted low MD adherence in our sample. The risk/control variable was created in order to neutralize the possible bias of the sample, due to a high proportion of participants being at risk of emotional disorders from the second phase. Before performing the regression models, collinearity between the variables was assessed by computing Pearson correlations between the candidate variables. We used two models. Model 1 used first-phase variables as predictors (birthplace, family type, school type, BMI, SCARED total score and CDI total score). In model 2, the predictors were the following third-phase variables: EDI-2 total score, YI-4 scores in conduct disorder, attention deficit hyperactivity disorder, anxiety and depressive symptoms, body fat percentage, BMI and the physical activity factor.
A series of regression analyses was conducted to determine if MD adherence mediates the relationship found in some studies between emotional symptoms and overweight and obesity. Gender, age and SES were included as covariables. The analysis was consistent with recommendations regarding mediational analyses in population-based research( Reference Hafeman and Schwartz 54 ).
In all the analyses, the level of statistical significance was a P value <0·05.
Results
Table 1 shows the descriptive data by gender for sociodemographic factors (age, SES, family type, birthplace and school type), anthropometric factors (BMI and body fat percentage), MD adherence factor, physical activity factor and psychopathological factors (SCARED, CDI, EDI-2 and YI-4). In this sample, 48·1% of adolescents presented low MD adherence, 41·9% medium MD adherence and 10·0% presented high MD adherence. As seen in Table 1, significant differences between genders were found only for body fat percentage and psychopathological symptoms. Girls showed higher levels of body fat than boys and also obtained higher scores than boys in symptoms related to eating disorders (EDI-2 total and YI-4 scores, drive for thinness and body dissatisfaction). As for MD adherence level (see Table 2), statistically significant results were found for SES; 54·2% of the adolescents with low SES showed low MD adherence, whereas 72·6% of those with high SES showed medium and high MD adherence. There were no significant differences in MD adherence level according to BMI although the results showed that no boy or girl with obesity presented a high level of MD adherence (see Table 3). Regarding physical activity, only boys showed statistically significant differences for MD adherence level. In relation to psychopathological factors, Table 3 shows that girls with low MD adherence presented significantly higher scores for eating disorders, and in particular for drive for thinness, anxiety and depressive symptoms, than girls with medium or high MD adherence. However, the post hoc analyses did not show statistically significant results for YI-4 anxiety symptoms or for EDI-2 drive for thinness factor scores.
Table 1 Characteristics of the community sample of Spanish adolescents in terms of sociodemographic, anthropometric, MD adherence, physical activity and psychopathological factors
MD, Mediterranean diet; SES, socio-economic status; SCARED, Screen for Child Anxiety Related Disorders; CDI, Children’s Depression Inventory; EDI-2, Eating Disorder Inventory-2; YI-4, Youth’s Inventory-4; ADHD, attention deficit hyperactivity disorder.
P values <0·05 are highlighted in bold font.
† Data are expressed as mean and standard deviation, or as a percentage where shown.
Table 2 MD adherence according to sociodemographic factors in phase 3 in the community sample of Spanish adolescents (n 241)
MD, Mediterranean diet; SES, socio-economic status.
P values <0·05 are highlighted in bold font.
Table 3 MD adherence in relation to anthropometric, physical activity and psychopathological factors in phase 3 in the community sample of Spanish adolescents (n 241)
MD, Mediterranean diet; EDI-2, Eating Disorder Inventory-2; YI-4, Youth’s Inventory-4; ADHD, attention deficit hyperactivity disorder.
P values <0·05 are highlighted in bold font.
bc,ac,abMean values that were significantly different by Bonferroni analysis.
Table 4 reports on the analysis of the risk of low MD adherence. In specific terms, we performed two logistic regression multivariate models, both of which were adjusted for age, gender, SES and the risk/control variable. Model 1 was performed to find risk factors for presenting low MD adherence and model 2 was performed to support the univariate associations found in the third phase. The EDI-2 factors and the YI-4 eating disorder symptoms were found to be collinear with the EDI-2 total score. Because of this, we introduced only the EDI-2 total score to the model as a predictor. For model 1, the results showed that high SES was a protective factor against presenting a low MD adherence level (OR=0·805, P=0·003). Likewise, the results for model 2 also showed that high SES was a protective factor (OR=0·772, P=0·001) and that depressive symptoms were related to the risk of presenting low MD levels (OR=1·069, P=0·021).
Table 4 Logistic regression models to predict risk of low MD adherence according to sociodemographic, anthropometric, physical activity and psychopathological factors in the community sample of Spanish adolescents (n 241)
MD, Mediterranean diet; SES, socio-economic status; SCARED, Screen for Child Anxiety Related Emotional Disorders; CDI, Children’s Depression Inventory; EDI-2, Eating Disorder Inventory-2; YI-4, Youth’s Inventory-4; ADHD, attention deficit hyperactivity disorder.
Models are adjusted for gender, age, SES and risk/control; P values <0·05 are highlighted in bold font.
Scores were assigned to quantitative variables as follows (no score for categorical variables): age; SES; 1st phase BMI; total SCARED; CDI; total EDI; YI-4 conduct disorder symptoms; YI-4 anxiety symptoms; YI-4 depressive symptoms; body fat; 3rd phase BMI; physical activity factor; gender (1=boy; 2=girl); birthplace (0=foreign; 1=native); family type (0=single-parent; 1=nuclear); school type (1=state school; 2=state-subsidized private school); risk/control (1=risk; 2=control).
We performed a mediational model adjusted by gender, age and SES (Fig. 1) given the possible relationship between emotional symptoms, low SES and high BMI, and the possibility that low MD adherence is a mediator between these variables and overweight/obesity. The results revealed that the risk of low MD adherence was not a mediator between depressive symptoms and overweight/obesity, or between SES and overweight/obesity. Furthermore, on the basis of the results of model 2 we tested another mediational model that positioned depressive symptoms as a partial mediator of the association between SES and risk of low MD adherence. Although depressive symptoms were related to MD adherence, they were not a mediator variable. The results revealed that lower SES was a predictor for the risk of low MD adherence and for overweight/obesity.
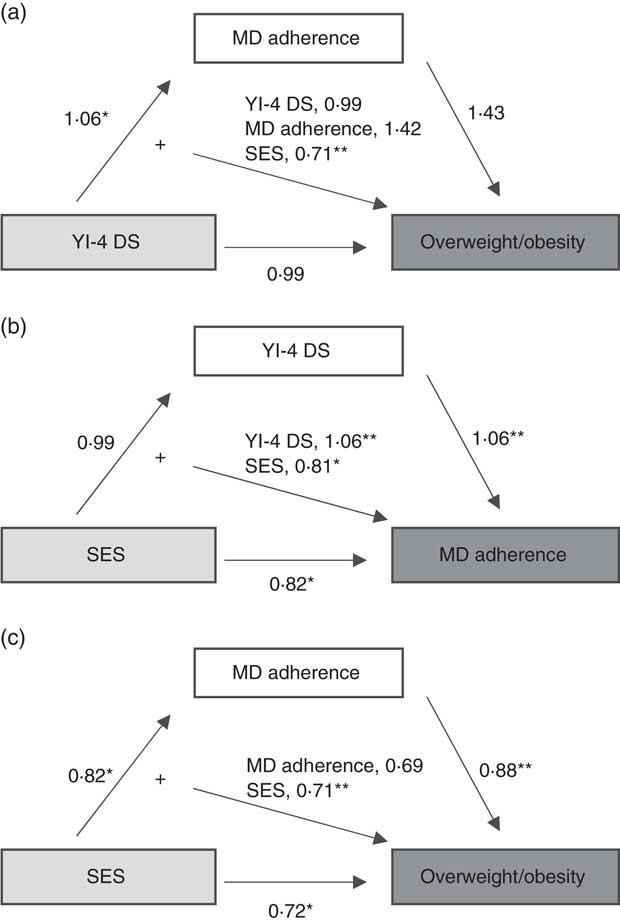
Fig. 1 Results of regression analyses conducted to determine if MD adherence mediates the relationship between emotional symptoms and overweight/obesity in a community sample of Spanish adolescents (n 241). All analyses of mediation controlled for age, gender and/or SES. Independent variables are shown in light grey boxes, mediator variables in white boxes and dependent variables in dark grey boxes; *P<0·05, **P<0·01 (MD, Mediterranean diet; SES, socio-economic status; YI-4 DS, Youth’s Inventory-4 depressive symptoms)
Discussion
In the present study, only 10·0 % of our adolescent participants showed high levels of MD adherence as determined by the Krece Plus food questionnaire. Likewise, a study performed by De Rufino et al.( Reference De Rufino Rivas, Antolín Guerra and Casuso Ruiz 55 ) with a sample of adolescents aged between 10 and 17 years also found a low nutritional risk of 15 %. Both these sets of results are low, particularly if they are compared with the levels of MD adherence found in the study by Serra-Majem et al.( Reference Serra-Majem Ll and Ngo 29 ) or the results of a recent study conducted with Spanish school-aged children( Reference Arriscado, Muros and Zabala 17 ), although those studies used the KIDMED questionnaire, which has different cut-off points. The results from the present study may be lower because it studied a population with a considerable number of individuals at risk of emotional disorders. In order to prevent this factor from distorting the results, we controlled for this variable in the multivariate models. Almost 50% of the participants presented low MD adherence and, although we found no relationship with anthropometric data, this is of concern given the high rates of overweight and obesity affecting the Spanish population( Reference Gutiérrez-Fisac, Guallar-Castillón and León-Muñoz 56 , Reference Sánchez-Cruz, Jiménez-Moleón and Fernández-Quesada 57 ) and the health benefits of the MD( Reference Sofi, Macchi and Abbate 1 ).
The results showed that 54·2 % of adolescents with low SES reported low MD adherence and 72·6 % of those with high SES reported medium to high MD adherence. We also found that high SES was a protective factor against presenting low MD adherence and overweight/obesity. Therefore, as in other studies, it seems that families with higher SES have better MD patterns than those with lower SES( Reference Arriscado, Muros and Zabala 17 , Reference Grosso, Marventano and Giorgianni 27 , Reference Bonaccio, Bonanni and Di Castelnuovo 58 ). This result is open to multiple interpretations. First, families with high incomes usually have high levels of education which may increase their awareness of healthy dietary habits and, therefore, may make them more likely to follow MD patterns. Second, their better economic opportunities may lead them to consume higher-quality and healthier products. Regarding the other sociodemographic factors, our results did not show any statistically significant differences for MD adherence according to school type or nationality, as were found by Arriscado et al.( Reference Arriscado, Muros and Zabala 17 ). This may be because our sample has a small number of foreigners.
We observed no significant relationships between the past and current BMI factor and MD adherence. Despite this, our results showed that no boy or girl with obesity presented high MD adherence. However, although our results are not statistically significant, it is worth pointing out that all participants with a BMI indicative of obesity followed diet patterns that deviated from the MD and that, as shown by Grosso et al.( Reference Grosso, Marventano and Giorgianni 27 ), these participants probably ate unhealthy food which affected their BMI. This may be supported by the relationship found between high BMI and low SES, and the interpretations mentioned above. Our findings also showed that risk factors for low MD adherence were independent of anthropometric data such as past and current BMI or body fat. In this regard, Rossi et al.( Reference Rossi, Negri and Bosetti 59 ) showed that, in adults, being classified as underweight, normal weight, overweight and obese had no significant effect on MD adherence. In relation to the controversy surrounding the relationship between anthropometric data and MD adherence during childhood and adolescence, the present results are consistent with other studies which have found no evidence of such a relationship( Reference Farajian, Risvas and Karasouli 10 , Reference Jennings, Welch and Van Sluijs 33 ). However, although no relationship between MD adherence and anthropometric factors was found, we cannot rule out this relationship being observed in the future. We believe that not following the MD pattern may lead to undesirable life habits or habits which may lead to negative anthropometric effects in the long term, such as higher BMI( Reference Martínez-González, García-Arellano and Toledo 60 , Reference Schröder, Marrugat and Vila 61 ). Furthermore, although physical activity was not related to MD adherence in the multivariate analyses, we found that boys with high MD adherence presented high levels of physical activity. Our results also showed that girls presented lower physical activity and higher levels of body fat than boys, coinciding with data in recent studies which concluded that girls are less active and more sedentary than boys, even after taking into account physiological differences in body fat between the genders( Reference Al-Hazzaa, Al-Sobayel and Abahussain 62 , Reference Leech, McNaughton and Timperio 63 ). However, although healthy dietary habits are known to be mostly associated with physical activity( Reference Al-Hazzaa, Al-Sobayel and Abahussain 62 ), the present study showed no significant differences between boys and girls in terms of MD adherence level.
Several authors have suggested that there is a significant association between unhealthy dietary patterns and poor mental health in children, adolescents and adults, and this is especially true for depression and anxiety( Reference Sánchez-Villegas, Delgado-Rodríguez and Alonso 7 , Reference Akbaraly, Brunner and Ferrie 64 – Reference Rienks, Dobson and Mishra 66 ). In a recent large national longitudinal survey of Canadians aged 18 years and older, Kingsbury et al.( Reference Kingsbury, Dupuis and Jacka 67 ) suggested that relationships between healthy intake (fruit and vegetables) and depression are complex. Behaviours such as smoking and poor physical activity may have a more important impact on depression than fruit and vegetable intake. From a biological point of view, there are several potential pathways by which diet quality may be related to mental health( Reference O’Neil, Quirk and Housden 68 ). In specific terms, isolated nutrients or foods in the MD, such as B-vitamins, folate and n-3 fatty acids, are known to have preventive effects on depression in adults. The MD is also related to reductions in vascular, inflammatory and metabolic processes in patients with depression. For example, folate is required to synthesize methionine, which is a precursor of S-adenosylmethionine, and it acts in methylation reactions such as those involving neurotransmitters with antidepressant characteristics( Reference Sánchez-Villegas, Delgado-Rodríguez and Alonso 7 , Reference Bottiglieri 69 – Reference Salas-Salvadó, Fernández-Ballart and Ros 73 ). When we studied the psychopathological characteristics of the sample in relation to their MD adherence level, the results showed that girls with low MD adherence reported high mean scores of depression and eating disorder symptoms. Regardless of gender, in data from multivariate analyses Fulkerson et al.( Reference Fulkerson, Sherwood and Perry 74 ) found that poor dietary quality was cross-sectionally associated with depression symptoms. As in Jacka et al.( Reference Jacka, Kremer and Berk 75 ), our results did not show that baseline depression was a predictive factor for diet quality during follow-up. The relationship found leads us to believe that girls with depressive symptoms are more likely to consume comfort foods, such as sweet snack foods, rather than healthy MD foods as a way to reduce feelings of sadness( Reference Mooreville, Shomaker and Reina 76 , Reference Wurtman and Wurtman 77 ). In fact, this behaviour is also observed in eating disorders characterized by binge eating episodes. Consequently, several of the variables studied may be bidirectionally related and therefore we performed three mediational models to explain whether MD adherence or depressive symptoms were mediators of overweight/obesity and diet quality respectively. In this regard, despite depressive symptoms being related to MD adherence and SES, this variable was not a mediator for high BMI. Low SES was also a predictor of risk for overweight and obesity. These results suggest that children’s diet patterns and BMI depend on their family’s socio-economic and educational level and their parent’s health awareness, as argued by Sotos-Prieto et al.( Reference Sotos-Prieto, Santos-Beneit and Pocock 78 ). In a large percentage of cases, when a child comes from a low socio-economic environment his/her diet quality is worse, and this was not mediated by depressive symptoms. Likewise, the relationship between low SES and overweight/obesity may be explained by other factors as well as diet, such as physical activity.
The current study has both strengths and limitations. In terms of its strengths, it presents a prospective study of data found in a community sample of adolescents, although unfortunately we have no data on the participants’ MD adherence in the first phase that would allow us examine whether the MD has a potential role in preventing mental health problems in children. Furthermore, a larger sample would be preferable. Also, there were differences in the SES factor between adolescents who participated in the third phase and adolescents who decided to not participate, but this was taken into account by using the SES variable as a control variable during the analyses. Moreover, we think that the Krece Plus short physical activity test may be too simple to evaluate physical activity habits and that it would have been better to use another tool.
As we had hypothesized, we observed significant differences in MD adherence level when SES was taken into account. However, none of the other variables such as age, nationality, family type or school type were found to be related to or influenced by MD adherence level. As for the findings on depressive symptoms, and especially in the case of girls, we conclude that this factor and low SES are related to low diet quality and we believe that these two factors should be taken into consideration in programmes designed to prevent obesity and promote dietary health. In short, the results highlighted the influence of psychosocial factors on MD adherence level. In our opinion, abandoning the MD pattern may have long-term negative anthropometric consequences. Strategies are needed to help children and adolescents obtain more knowledge about healthy nutritional habits, the benefits of the MD pattern and other healthy dietary patterns, and other healthy habits such as regular physical activity. These kinds of initiative could be carried out in schools and could involve families as a whole.
Acknowledgements
Acknowledgements: The authors are grateful to all the schools and children that participated in the study. Financial support: This research was supported by a grant from the ‘Fondo de Investigaciones Sanitarias’ (PI07/0839) of the Instituto de Salud Carlos III of the Spanish Ministry of Health, Social Services and Equality. The funder had no role in the design, analysis or writing of this article. Conflict of interest: None. Authorship: The authors contributed as follows. N.V., psychological assessment during data collection, statistical analysis, author of the draft manuscript; V.A., statistical assessment and discussion of nutritional data, reviewed and approved the final version of the manuscript; E.A., nutritional assessment during data collection; J.C., managed and designed the study, psychological assessment during the first phase, collaborated in writing the manuscript and approved the final version. Ethics of human subject participation: The project was approved by the Universitat Rovira i Virgili’s ethics committee for research on individuals and by the Catalan Government’s Department of Education. All parents were informed about the study and gave written informed consent for their child’s participation.








