Overweight is considered an important risk factor for morbidity and mortality from CVD. Although there are some ways to diagnose excess body fat, abdominal fat is considered by the WHO as a more accurate predictor of cardiovascular risk, metabolic disorders and death than other anthropometric measures such as BMI( 1 , Reference Huxley, Mendis and Zheleznyakov 2 ). The measurement of waist circumference (WC), as an indirect measure of visceral fat, is easy, inexpensive, non-invasive and directly related to BMI. It is also one of the recommended diagnostic procedures to assess abdominal adiposity and risk of CVD, both in clinical practice and in epidemiological studies( Reference Pouliot, Despres and Lemieux 3 , Reference Oka, Miura and Sakurai 4 ).
The WC cut-off points currently recommended to identify the risk of CVD (80 cm and 88 cm for women and 94 cm and 102 cm for men, to identify increased and substantially increased risk, respectively) are derived mainly from studies in predominantly European populations( Reference Han, van Leer and Seidell 5 ). Thus, their universal use results in a limiting factor for clinical and epidemiological studies because, as well as sex, age and reproductive history, ethnic characteristics also affect fat distribution, thus influencing body structure and the most appropriate cut-off points which set up the risk of CVD( 6 ). The need to adopt different cut-off points for different populations was discussed in 2005 by the International Diabetes Federation in its consensus statement for the diagnosis of metabolic syndrome( Reference Alberti, Zimmet and Shaw 7 ). Likewise, in 2008, the WHO published a technical report to reassess the most appropriate WC cut-off points and waist:hip ratios. The report reinforced the recommendation that ethnic or specific differences in certain sub-populations must be taken into account to assess these cut-off points in defining the risk of CVD( 6 ).
Although several studies have evaluated the values of WC which best predict the risk of CVD in different ethnic groups( Reference Herrera, Casas and Miranda 8 , Reference Lear, James and Ko 9 ), the current evidence in South America is insufficient and indicates to keep using the same cut-off points recommended for the European population( Reference Lear, James and Ko 9 ). Only six population-based studies conducted in adults in Brazil which aimed to identify these cut-off values were found. Five were cross-sectional studies( Reference Peixoto Mdo, Benicio and Latorre Mdo 10 – Reference Velásquez-Meléndez, Kac and Valente 14 ) and only one had a longitudinal design( Reference Gus, Cichelero and Moreira 15 ). The outcomes considered in these studies were cardiovascular risk factors (hypertension and/or diabetes mellitus), and the values of WC with higher sensitivity and specificity ranged from 85 to 88 cm in men and from 80 to 86 cm in women.
The present study assessed the WC cut-off points that best predicted the presence of at least two out of three known risk factors for CVD (hypertension, diabetes mellitus and/or dyslipidaemia, taken as the gold standard for identifying individuals with increased cardiovascular risk) from the use of two different criteria based on analysis of receiver operating characteristic (ROC) curves (Youden index and points of optimal sensitivity and specificity).
Experimental methods
Between January and June 2010, a cross-sectional population-based study was conducted with adults aged ≥20 years living in the urban area of Pelotas, a city located in southern Brazil with approximately 350 000 inhabitants. The study was conducted by the Postgraduate Programme in Epidemiology of the Federal University of Pelotas, as part of a consortium system which included fourteen master's projects, all of which had data collection gathered on a common instrument.
The sample size was set at 2842 individuals, based on the needs of the studies which comprised the research consortium. From this, there was the need to visit 1300 households. The sampling process took place in multiple stages, based on data from the 2000 Census. The 404 census tracts in the city were ordered according to average income of household heads and thereafter 130 sectors were drawn with probability proportional to the number of households. From the identification of the residences of each of the selected tracts, systematic sampling occurred at home. Accordingly, all individuals aged ≥20 years were considered eligible, provided that the following exclusion criteria were not present: inability to stand, limb amputation, and pregnant currently or within the previous 6 months. The interviews were conducted face to face in the household. All interviewers were trained during 40 h. Anthropometric measurements were performed by a team of evaluators trained and standardized in measurement techniques. The acceptable technical errors of measurement were calculated based on the publication of Habicht( Reference Habicht 16 ) and the technique for measuring WC followed the recommendations of Lohman et al. ( Reference Lohman, Roche and Martorell 17 ). The maximum acceptable technical errors of measurement within and between observers, used in the process of standardization for the measurement of WC, were respectively two and three times the error observed by the gold standard. Weight and height were also measured using the same methodology.
WC was measured using a flexible tape (brand Graham Field) with an accuracy of 0·1 cm at the narrowest part of the trunk, identified as the midpoint between the lowest rib margin and the iliac crest. The measurement was taken after expiration. To optimize data quality, we used the average of two measures of WC, obtained at different moments of the interview. Participants were weighed to the nearest 100 g using a previously calibrated digital scale. Standing height of the barefoot participants was measured to the nearest 1 mm, using aluminium stadiometers of 2 m length.
In the interview, the participants were also asked about economic, demographic and general health characteristics. Among these data, the ones considered in the present study were gender, skin colour (collected as white, black, brown, yellow or indigenous, subsequently categorized as white or non-white), age, schooling (years of study), current smoking and physical activity during leisure time (from the leisure section of the International Physical Activity Questionnaire( Reference Craig, Marshall and Sjostrom 18 )). Current smokers were participants who smoked at least one cigarette daily over the past 30 d and participants were considered active if they reached the physical activity guidelines of 150 min of moderate-to-vigorous physical activity in the last 7 d.
The variables corresponding to the clinical conditions for risk of CVD (hypertension, diabetes mellitus and dyslipidaemia) were collected by the question: ‘Has any doctor ever told you that you have…?’. The respondent could answer yes or no for each of the following: ‘…hypertension or high blood pressure?’, ‘…diabetes mellitus or high sugar?’ and ‘…high cholesterol or triglycerides?’. In order to reduce the likelihood of survival bias in the results and to include only individuals at risk of CVD, information was also collected about previous medical diagnosis of angina pectoris, acute myocardial infarction or stroke through the options ‘…angina or heart attack?’ and ‘…stroke or cerebral ischaemia?’.
The process of data collection was performed by Personal Digital Assistant (PDA) and the variables (demographic, socio-economic and behavioural) were directly exported to the database. The anthropometric measurements were recorded on paper and were added to the database after a process of double entry and analysis of inconsistencies.
Data analysis was performed using the STATA statistical software package version 12·0. After sample description, mean WC was calculated according to age group (20–39 years, 40–49 years, 50–59 years and ≥60 years) and sex for each of the CVD risk factors considered in the study (hypertension, diabetes mellitus and dyslipidaemia) and for the presence of two or more of these factors. The mean WC values obtained were plotted on graphs, stratified by sex and age group, and compared with the cut-off points of WC currently used in the identification of ‘increased’ and ‘substantially increased’ risk of CVD( 19 , 20 ) (respectively, 94 and 102 cm for men and 80 and 88 cm for women).
ROC curves were constructed( Reference Zweig and Campbell 21 , Reference Akobeng 22 ) to estimate the predictive ability of WC for identifying cardiovascular risk. The Youden index was calculated (highest sensitivity + specificity−1) to identify the best cut-off point based on the largest vertical distance between the ROC curve and the diagonal curve, separately for men and women. Cut-off points based on values closer to the point (0, 1) or with higher optimal sensitivity and specificity (lowest value (1−sensitivity)2 + (1−specificity)2) were also calculated. Prevalence, sensitivity, specificity and positive predictive value (PPV) were calculated for WC values closest to the left corner of the curve in relation to CVD risk factors (hypertension, diabetes mellitus and dyslipidaemia). Sensitivity was defined as the proportion of individuals with at least two out of the three risk factors correctly identified by the cut-off values of WC. Specificity was defined as the probability of the point chosen to correctly identify individuals with low risk (none or one risk factor). PPV was defined as the proportion of individuals who, after being identified as high risk by the WC, actually had this high risk (presence of at least two of the three risk factors). The 95 % confidence intervals were calculated for these parameters.
The study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects/patients were approved by the Ethics Committee in Research of the Faculty of Medicine at Federal University of Pelotas. Written informed consent was obtained from all participants.
Results
From a total sample of 3024, we obtained interviews and measured WC for 2454 participants (response rate = 81·2 %). The losses were greater in males (23·4 %) than females (17·4 %). The distribution of age, schooling, physical activity and smoking was not different between interviewed and losses or refusals. To avoid survival bias, we included in the analysis only those individuals with risk of developing CVD. Accordingly, we excluded those who reported previous medical diagnoses for angina pectoris, acute myocardial infarction or vascular brain injury (n = 375). After exclusions, 2112 individuals participated in our study (57·1 % females).
Table 1 shows the description of the sample, stratified by sex. About 40 % of participants of both sexes were younger than 40 years old and the majority of the sample was made up of white people. More than 70 % of those interviewed had level of schooling up to complete secondary education. As for behavioural characteristics, almost 80 % of females and 69 % of males did not achieve the current guidelines for physical activity during leisure time (≥150 min/week). One-quarter of males and 18 % of females were smokers. Over half of the participants were overweight, with more than 20 % being obese. Concerning cardiovascular risk factors, about one-third of the participants reported systemic arterial hypertension (30·4 % of males and 32·5 % of females), while about 8 % were classified with diabetes (6·3 % of males and 8·4 % of females) and almost 25 % reported dyslipidaemia (17·1 % of males and 24·1 % of females). The frequency of participants with at least two out of the three cardiovascular risk factors (hypertension, diabetes and/or dyslipidaemia) was 15·8 % (95 % CI 14·2, 17·3 %) and the prevalence was lower in males (14·1 %; 95 % CI 11·8, 16·4 %) than females (17·0 %; 95 % CI 14·9, 19·1 %).
Table 1 Description of the sample according to demographic, socio-economic and behavioural characteristics and prevalence of risk factors for CVD, stratified by sex, Pelotas, southern Brazil, 2010
*Brazilian Association of Research Institute criterion.
†Two or more risk factors for CVD: hypertension, diabetes and/or dyslipidaemia.
The adequacy of current cut-off points of WC recommended by WHO is shown in Figs 1 and 2. Figure 1 shows the mean WC, according to age and sex, for participants who had one of the three cardiovascular risk factors (hypertension, diabetes or dyslipidaemia) and participants who had none. Participants of both sexes with each risk factor for CVD had greater WC than participants without each risk factor. In males, except those younger than 40 years with hypertension or dyslipidaemia, the cut-off points currently recommended by WHO discriminated individuals with increased risk for CVD. In males without these risk factors, WC increased according to age (P < 0·001) such that, in general, only in those aged 60 years or more was mean WC close to 94 cm. In males who were older than 40 years and with the cardiovascular risk factors, mean WC was always greater than the cut-off value currently recommended by WHO for increased risk for CVD. However, for females, mean WC was lower than the cut-off point for increased CVD risk only in the youngest group and in those who did not show hypertension, diabetes or dyslipidaemia. Every other group of women had WC greater than 80 cm, including those without hypertension, diabetes or dyslipidaemia. On the other hand, hypertensive females aged 60 years or more and diabetic women who were older than 40 years had mean WC greater than the value for substantially increased risk of CVD (88 cm). Among females without the risk factors for CVD, a positive association between WC and age (P < 0·001) was seen in all cases.
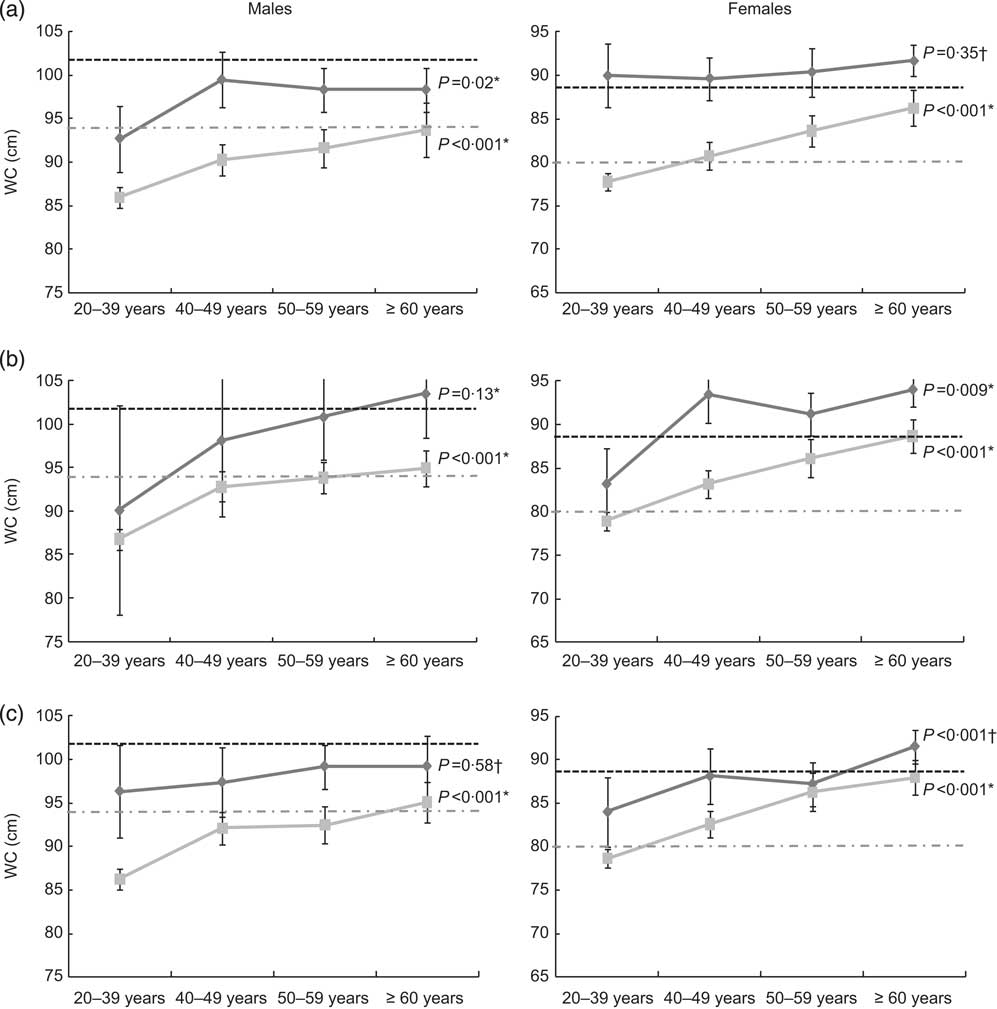
Fig. 1 Waist circumference (WC) according to age among males and females with (![]() ) or without (
) or without (![]() ) a risk factor for CVD: (a) hypertension, (b) diabetes mellitus and (c) dyslipidaemia; Pelotas, southern Brazil, 2010. Values are means with their standard deviations represented by vertical bars;
) a risk factor for CVD: (a) hypertension, (b) diabetes mellitus and (c) dyslipidaemia; Pelotas, southern Brazil, 2010. Values are means with their standard deviations represented by vertical bars; ![]() represents the WHO cut-off for increased risk of CVD (94 cm for men, 80 cm for women);
represents the WHO cut-off for increased risk of CVD (94 cm for men, 80 cm for women); ![]() represents the WHO cut-off for substantially increased risk of CVD (102 cm for men, 88 cm for women). P values for the variation in WC according to age among those with/without risk from *ANOVA test for heterogeneity or †Kruskal–Wallis test
represents the WHO cut-off for substantially increased risk of CVD (102 cm for men, 88 cm for women). P values for the variation in WC according to age among those with/without risk from *ANOVA test for heterogeneity or †Kruskal–Wallis test
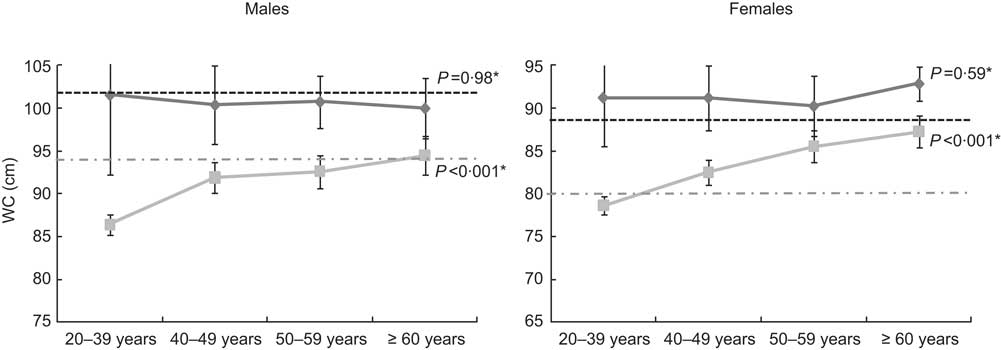
Fig. 2 Waist circumference (WC) according to age among males and females with (⩾2 risk factors, ![]() ) or without (0 or 1 risk factor,
) or without (0 or 1 risk factor, ![]() ) two or more risk factors for CVD (hypertension, diabetes and/or dyslipidaemia), Pelotas, southern Brazil, 2010. Values are means with their standard deviations represented by vertical bars;
) two or more risk factors for CVD (hypertension, diabetes and/or dyslipidaemia), Pelotas, southern Brazil, 2010. Values are means with their standard deviations represented by vertical bars; ![]() represents the WHO cut-off for increased risk of CVD (94 cm for men, 80 cm for women);
represents the WHO cut-off for increased risk of CVD (94 cm for men, 80 cm for women); ![]() represents the WHO cut-off for substantially increased risk of CVD (102 cm for men, 88 cm for women). P values for the variation in WC according to age among those with/without risk from *ANOVA test for heterogeneity
represents the WHO cut-off for substantially increased risk of CVD (102 cm for men, 88 cm for women). P values for the variation in WC according to age among those with/without risk from *ANOVA test for heterogeneity
Figure 2 compares the mean WC in males and females with at least two or more cardiovascular risk factors and the mean WC in males and females without or with only one risk factor, stratified by age. At all ages, mean WC was greater among those with two or more risk factors for CVD, in both sexes. Among males without or with only one risk factor for CVD, WC increased with age and mean WC was always lower than 94 cm, except in men aged 60 years or more. Nevertheless, males with at least two risk factors for CVD had mean WC close to the cut-off value for substantially increased risk for CVD (102 cm), regardless of age. Concerning females, those with two or more risk factors had mean WC greater than 88 cm, regardless of age. Among females without or with only one risk factor, WC increased according to age and only the youngest women had WC lower than the cut-off value for increased risk for CVD (80 cm).
Figure 3 shows the ROC curves for males and females. We found that the area under the ROC curve (AUC) showed moderate accuracy of WC to discriminate participants with at least two out of three cardiovascular risk factors studied, in both males (0·74; 95 % CI 0·71, 0·76) and females (0·75; 95 % CI 0·73, 0·77). The Youden index (defined as the maximum vertical distance between the ROC curve and the diagonal line)( Reference Akobeng 22 ) showed that the more adequate cut-off values of WC for prediction of at least two risk factors for CVD were 89 cm in males and 81 cm in females. On the other hand, using the method of optimal sensitivity and specificity (point on the curve closest to the (0, 1) point( Reference Akobeng 22 )), we found that the most adequate cut-off points for prediction of presence of two or more cardiovascular risk factors for males and females were 95 cm and 87 cm, respectively.
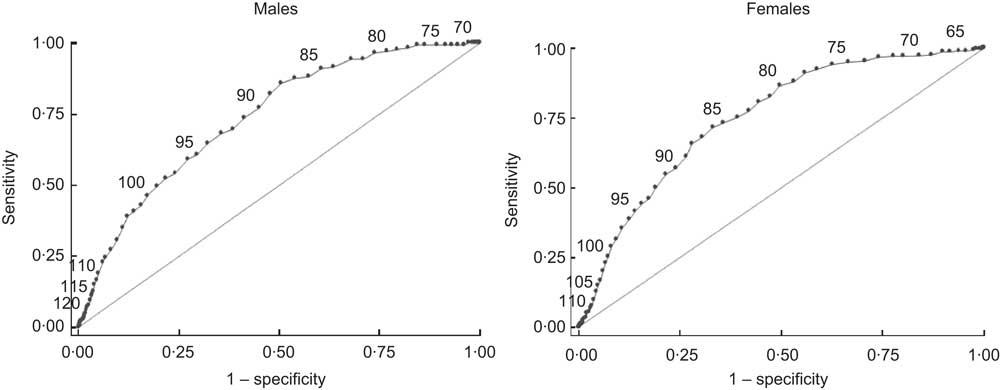
Fig. 3 Receiver operator characteristic (ROC) curves for the predictive value of waist circumference considering two or more cardiovascular risk factors (hypertension, dyslipidaemia and/or diabetes) as the outcome, stratified by sex, Pelotas, southern Brazil, 2010. Area under the ROC curve (AUC) = 0·7364 for males, AUC = 0·7492 for females
From WC values closest to the (0, 1) point of ROC curves (84 to 104 cm in males and 78 to 98 cm in females), we calculated the prevalence of participants with WC greater than or equal to each value, as well as sensitivity, specificity and PPV of these points to predict the presence of at least two cardiovascular risk factors (Table 2). In males, sensitivity and specificity values ranged from 45·3 % to 95·6 % and from 28·7 % to 77·4 %, respectively. Among females, sensitivity ranged from 36·2 % to 92·2 %, while specificity ranged from 39·3 % to 82·5 %. Considering the optimal sensitivity and specificity criterion, in males the WC value of 95 cm showed sensitivity of 67·2 % and specificity of 60·6 %. The prevalence at this point was 43·2 %, and 21·1 % were correctly classified with two or more cardiovascular risk factors (PPV). In females, 42·5 % had WC greater than or equal to the cut-off value of 87 cm. This point showed sensitivity of 69·7 %, specificity of 62·9 % and PPV of 27·3 %. Using the Youden index, the cut-off values of ≥89 cm in males and ≥81 cm in females increased the sensitivity to a little more than 85 %, but other validity parameters decreased (specificity lower than 50 %, PPV of 19·8 % in males and 24·7 % in females) and prevalence of abdominal obesity increased (almost 60 % in both sexes).
Table 2 Prevalence, sensitivity (ST), specificity (SP) and positive predictive value (PPV) of cut-off points of waist circumference (WC) for prediction of two or more cardiovascular risk factors (hypertension, diabetes and/or dyslipidaemia) in males and females from Pelotas, southern Brazil, in 2010
Discussion
The present study showed that the currently recommended cut-off points to detect increased risk (≥94 cm in men and ≥80 cm in women) or substantially increased risk (≥102 and ≥88 cm, respectively) for CVD( Reference Lean, Han and Morrison 23 ) seem to have different power of discrimination between sexes. These cut-off points discriminate males at risk better than females at risk, either in the individual assessment of each of the risk factors (hypertension, diabetes mellitus or dyslipidaemia) or when analysed for the presence of at least two of these three factors. Thus, the use of these cut-off points in females leads to a high percentage of misclassification, increasing the number of women diagnosed with abdominal obesity (60·5 % for values of WC ≥80 cm) compared with males (46·1 % for values of WC ≥94 cm). This higher prevalence of abdominal obesity in females is not consistent with the data of morbidity and mortality from CVD, which most often affects males, or with the prevalence of excess body fat assessed by anthropometric indicators such as BMI.
Evaluation of the adequacy of cut-off points for WC recommended by WHO in the Brazilian population is important, since these points were adopted based on individuals of European origin( Reference Lean, Han and Morrison 23 ). The accumulation of abdominal fat differs between ethnic groups( Reference Lear, Humphries and Kohli 24 ), which has led to several studies to assess the most appropriate cut-off points for different populations( Reference Lear, James and Ko 9 ). A greater number of studies have been performed in countries such as China and Japan, with consistent evidence as to the best cut-off points for WC, and new values have been recommended (80 cm in women and 85 cm in men)( Reference Lear, James and Ko 9 ). However, in South America, these studies are limited and it is still recommended to maintain the same values as for the European population.
In Brazil, the values found suitable for the prediction of cardiovascular risk from WC ranged from 85 to 88 cm in males( Reference Peixoto Mdo, Benicio and Latorre Mdo 10 – Reference Ferreira, Valente and Goncalves-Silva 13 , Reference Gus, Cichelero and Moreira 15 ) and from 80 to 86 cm in females( Reference Peixoto Mdo, Benicio and Latorre Mdo 10 – Reference Gus, Cichelero and Moreira 15 ). These cut-off points were similar to those found in the present study when considering the Youden index (89 cm for men and 81 cm for women), i.e. greater vertical distance between the ROC curve and the diagonal( Reference Akobeng 22 ), but lower than those observed with the criterion of optimal sensitivity and specificity values (95 and 87 cm, respectively). Among the Brazilian studies, the procedures used to identify these cut-off points were the intersection of the curves of sensitivity and specificity( Reference Peixoto Mdo, Benicio and Latorre Mdo 10 – Reference Ferreira, Valente and Goncalves-Silva 13 ) or the Youden index( Reference Gus, Cichelero and Moreira 15 ). The procedures used to define the best cut-off points affect the comparability between studies( 6 ). A systematic review published in 2010 on the values of WC for the prediction of CVD risk( Reference Wang, Ma and Si 25 ) showed that, depending on the procedure used, the cut-off points can fluctuate widely in studies conducted in the same country. Despite this limitation, there is no consensus on the best procedure to be used to define the best cut-off points( 6 ).
In the present study, use of the Youden index obtained a high sensitivity and low specificity in predicting the risk of hypertension, diabetes and dyslipidaemia in both males and females. As a result, there was a greater misclassification of individuals with only one risk factor, who ended up being classified as having an increased cardiovascular risk. The use of the optimal sensitivity and specificity criterion may better distinguish between individuals with two or more cardiovascular risk factors and those with up to one factor (highest PPV for both sexes).
As a practical matter, despite the high sensitivity obtained by using the Youden index, its low specificity and high misclassification rate (false positives) limit its use in screening the population, since more than half of the adult population would be identified as having increased risk for developing CVD. Consequently, there is a greater impact on health services, as well as higher costs arising subsequently in the diagnostic evaluation of individuals at low risk with positive screening. This could be visually assessed by applying the cut-off points obtained from both procedures to Figs 1 and 2 in this paper. Using the values of optimal sensitivity and specificity in males (95 cm) would maintain the ability to discriminate between individuals with and without hypertension, diabetes mellitus and/or dyslipidaemia at different ages. In females, with the cut-off point of 87 cm it would be possible to identify more clearly who are the people having or not having these risk factors (individual or combined factors).
Another aspect to be considered in comparison with other studies is the different end points used. In 2005, Pitanga and Lessa conducted a cross-sectional study in north-eastern Brazil that compared various anthropometric indicators, including WC, to identify which one best discriminated high coronary risk (determined based on an index that included age, blood pressure, total cholesterol, HDL-cholesterol, smoking and diagnosis of diabetes mellitus)( Reference Pitanga and Lessa 11 ). In the same sample, other authors identified the best cut-off points of WC for the diagnosis of diabetes mellitus and obesity( Reference Barbosa, Lessa and de Almeida Filho 12 ). Two other studies used just hypertension as the outcome, being a longitudinal type study performed in southern Brazil( Reference Gus, Cichelero and Moreira 15 ) and a cross-sectional study in the mid-west( Reference Peixoto Mdo, Benicio and Latorre Mdo 10 ). In 2006, Ferreira et al. used only dyslipidaemia as outcome( Reference Ferreira, Valente and Goncalves-Silva 13 ). Among those who have used various criteria to define the risk of CVD( Reference Pitanga and Lessa 11 , Reference Barbosa, Lessa and de Almeida Filho 12 , Reference Almeida, Almeida and Araujo 26 ), the cut-off point of WC among females was higher than that provided by studies using a single health condition( Reference Peixoto Mdo, Benicio and Latorre Mdo 10 , Reference Ferreira, Valente and Goncalves-Silva 13 , Reference Gus, Cichelero and Moreira 15 ). The first three studies agreed on the procedure used to measure WC based on the narrowest point of the trunk, rather than the midpoint between the costal margin and the iliac crest – criteria used by other Brazilian papers – which can also influence the results( 6 ). It is also important to note that only four studies used population-based samples( Reference Peixoto Mdo, Benicio and Latorre Mdo 10 – Reference Barbosa, Lessa and de Almeida Filho 12 , Reference Gus, Cichelero and Moreira 15 ), which can also affect the comparability of results.
Regarding the predictive ability of WC for cardiovascular risk assessment, the AUC observed was 0·73 (95 % CI 0·71, 0·76) for males and 0·74 (95 % CI 0·73, 0·77) for females in the present study. The prediction of cardiovascular risk from WC has been considered more applicable than from other anthropometric indices such as BMI( Reference Lee, Huxley and Wildman 27 ), the main limitation of this last indicator being its inability to distinguish between muscle and adipose tissue( Reference Yajnik and Yudkin 28 ). The AUC in that study( Reference Lee, Huxley and Wildman 27 ) was higher for WC than for BMI, in males (AUC for BMI = 0·69; 95 % CI 0·65, 0·74) and females (AUC for BMI = 0·70; 95 % CI 0·67, 0·74; P value of the difference with AUC for WC <0·001 in both cases), suggesting that the former was a better test to evaluate cardiovascular risk. The AUC values for WC that we found were also similar to those reported in a meta-analysis published recently( Reference Lee, Huxley and Wildman 27 ). However, the meta-analysis evaluated the predictive ability of WC for each cardiovascular risk factor, whereas the data presented here for the ROC curves refer to the presence of two or more cardiovascular risk factors. Nevertheless, results from prospective studies suggest that BMI has similar ability to predict CVD risk factors as measurements of central adiposity. The Caerphilly Prospective Study, a British cohort of men, showed no differences in the strengths of association with incident diabetes between BMI, WC and two other indicators of abdominal obesity( Reference Taylor, Ebrahim and Ben-Shlomo 29 ). On the other hand, the British Women's Heart and Health Study( Reference Lawlor, Ebrahim and Davey Smith 30 ) found that WC and waist:height ratio were more strongly associated with diabetes than BMI. New prospective studies are necessary to elucidate these differences.
One possible limitation of our study was the use of self-reported data for the diagnosis of hypertension, diabetes and dyslipidaemia. The choice of these diseases was based on their relevance in the prediction of cardiovascular risk and they are recommended in studies to this end by the WHO( 6 ). Although this is self-reported information, a previous study in Pelotas showed that self-report to identify the prevalence of hypertension had a sensitivity of 84·3 %, specificity of 87·5 % and reliability of 80·0 %( Reference Chrestani, Santos Ida and Matijasevich 31 ). Another study in Minas Gerais also assessed the self-report of hypertension in older adults and found a sensitivity of 72·1 % and specificity of 86·4 %( Reference Lima-Costa, Peixoto and Firmo 32 ). In relation to diabetes, Dode and Santos studied the validity of self-reported gestational diabetes in 2009, and found a relevant sensitivity (72·9 %) and high specificity (99·0 %) and accuracy (97·9 %)( Reference Dode and Santos 33 ). Even with higher accuracy, a possible bias due to self-reported compared with measured outcomes would be a higher misclassification of the disease in young compared with older age groups( Reference Chrestani, Santos Ida and Matijasevich 31 , Reference Lima-Costa, Peixoto and Firmo 32 ). This possible bias could explain the greater accuracy of WC at older ages.
There were losses of almost 20 % of individuals eligible for the study, which were higher among males. Even if these losses are considered a limitation of the study, they only influence the accuracy of the results, resulting in no bias, since the main findings consist of descriptive and predictive analysis of the cut-off points of WC. Another important issue to consider is the study design. Longitudinal studies are better for assessment of disease risks than cross-sectional ones that cannot distinguish between risk factors and prognostic factors. However, the exclusion of individuals with pre-existing CVD is a strong point of the study, which could affect the results to represent the surviving cases, possibly related to good prognosis. Other strengths were the two methodological steps to reduce errors in the measurements of WC, as well as the use of two different criteria for assessing the best cut-off points. Finally, we have to consider the external validity of our results. Brazil is a country with more than 190 million inhabitants and, according to the Brazilian census of 2010, skin colour was self-classified as white for 47·7 % and black for 7·6 % of the citizens( 34 ). In Pelotas, most of the inhabitants self-reported their skin colour as white (80·3 %), but the proportion of blacks (10·7 %) is higher than in other cities in southern Brazil. These demographic differences should be considered when comparing our results, as previous studies have shown that body composition and cut-offs depend on race/ethnicity( 6 , Reference Lear, James and Ko 9 , Reference Lear, Humphries and Kohli 24 ).
Conclusions
The results of our study suggest that the cut-off values of WC currently recommended for screening for CVD risk are more appropriate for males than females, incurring an overestimation of the risk of CVD among females, due to low cut-off values of this population. This error causes the positive screening of women without a real high risk, which in terms of public health would lead to greater demand for consultations and diagnostic tests, resulting in overloading existing professionals and higher spending on health. Thus, it is important that further studies be conducted in other regions of Brazil, considering not only the different ethnic origins that Brazil presents, but also the methodology used, thus helping to identify the cut-off points of WC best suited for the prediction of CVD risk.
Acknowledgements
Sources of funding: The authors wish to acknowledge the Brazilian agency Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) for funding and scholarship support to R.M.B. Conflicts of interest: The authors report no conflict of interest. Authors’ contributions: C.A.V., R.S.L., R.M.B. and E.C.M. conceptualized the study, coordinated the field work, ran the analyses and wrote the manuscript. D.P.G., A.M.M. and I.S.S. contributed to the writing and revision of the manuscript. D.A.G.-C. conceptualized the study, ran the analyses and contributed to the writing and revision of the manuscript.







