Ductal stenting can be offered in duct-dependent pulmonary circulation, as an alternative to surgical palliation with a modified Blalock–Taussig shunt. Ductal stenting can however be challenging in case of discontinuity of the pulmonary artery branches. Bilateral ductus arteriosus feeding discontinuous pulmonary arteries is scarce. We herein report successful bilateral ductal stenting in an infant with tetralogy of Fallot with pulmonary atresia and discontinuous right and left pulmonary arteries.
Case description
A 2500-gram term newborn was admitted in our department from the delivery room for the management of a prenatally diagnosed tetralogy of Fallot with pulmonary atresia. His peripheral oxygen saturation level was 80% on pulse oximetry in room air. Transthoracic echocardiography showed a normal atrial arrangement and confirmed a tetralogy of Fallot with pulmonary atresia and discontinuous pulmonary artery branches. At day-of-life 1, saturation dropped to 60%. Echocardiogram showed normally supplied right pulmonary artery but a constricted left ductus and functionally closed left pulmonary artery. Prostaglandin (PGE-1, 10 ng/kg/min) infusion was started and allowed restoration of the left pulmonary artery perfusion and subsequent improvement in oxygen saturation. A CT scan was performed to delineate ductal anatomy (Fig 1). After multidisciplinary team discussion, a transcatheter approach was preferred and the baby was transferred to the catheterisation laboratory. The left ventricular angiogram showed that the left pulmonary artery was supplied by a ductus arteriosus arising from the aortic arch, whilst the right pulmonary artery came straight from the brachiocephalic artery (Fig 1). There was no major aorto-pulmonary collateral artery. An elective ductal stenting with a 3.5 × 13 mm bare metal coronary stent was performed on the fifth postnatal day, with a 5-French Judkins Left 3.5 coronary guide catheter advanced through right ventricle into the aortic arch from the right femoral vein (Fig 2). PGE-1 had been stopped 6 hours before ductal stenting to allow the ductus to be well constricted. After ductal stenting, the baby was started on aspirin and clopidogrel. Four days later, oxygen saturation suddenly dropped again, up to 55%. Echocardiogram showed a well-positioned stent on the origin of the left pulmonary artery with an unrestrictive blood flow, but no right pulmonary artery was seen anymore. The patient was sent back to the catheterisation laboratory, where hand contrast injection demonstrated sub-occlusion of the proximal segment of the right pulmonary artery, which was consistent with ductal constriction of a second, right ductus arteriosus supplying the right pulmonary artery. Emergent ductal stenting of the right ductus was performed using a 3.5 × 24 mm bare metal coronary stent with a 5-French Judkins Right 3.0 coronary guide catheter into the brachiocephalic artery from the right femoral artery (Fig 2). This allowed clinical improvement and saturation increase up to 88%. Both stenting were uneventful, and the patient remained on aspirin and clopidogrel till surgical repair with pulmonary artery reimplantation 10 months later.
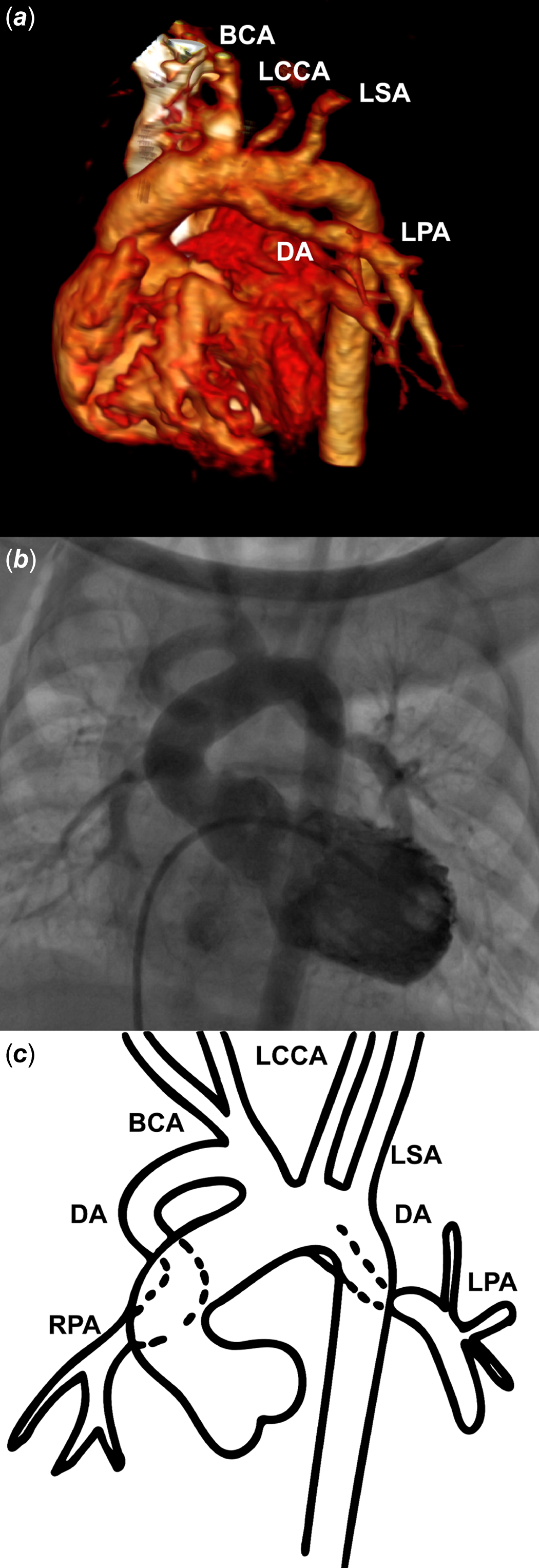
Figure 1. Multimodality imaging of bilateral arterial duct. Three-dimensional volume-rendering CT scan ( a ), left ventricular angiography ( b ), and a picture ( c ) showing bilateral ductus arteriosus feeding discontinuous pulmonary arteries. The left pulmonary artery is supplied by a left ductus arteriosus arising from the aortic arch. The right pulmonary artery is supplied by a right ductus arteriosus coming from the brachiocephalic trunk. RPA = right pulmonary artery; DA = ductus arteriosus; BCA = brachiocephalic artery; LCCA = left common carotid artery; LSA = left subclavian artery; LPA = left pulmonary artery.
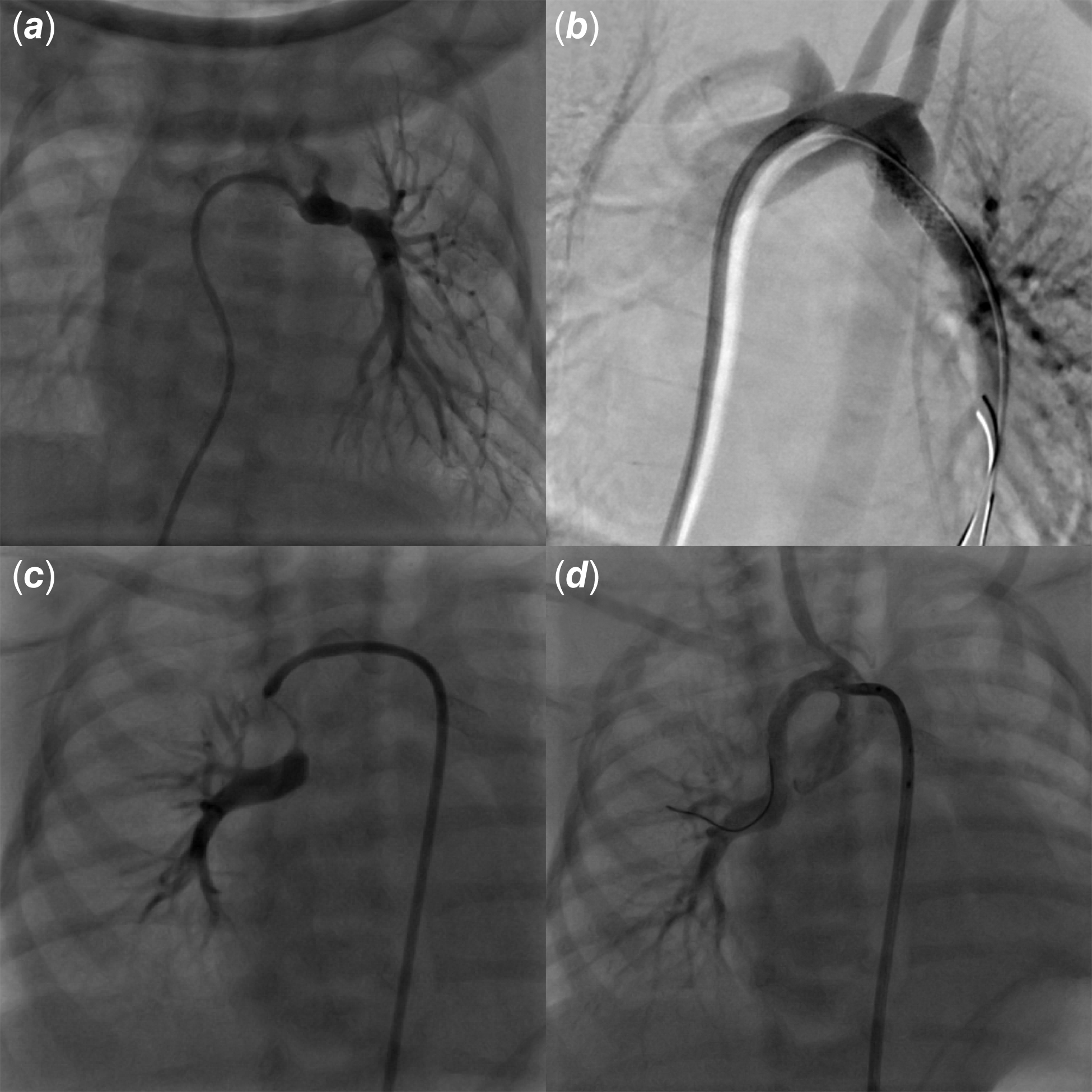
Figure 2. Bilateral arterial duct constriction and stenting. Hand injection via a 4-fr judkins right catheter engaged into the left ductus arteriosus delineating the left pulmonary artery ( a ). The left ductus was stented using a 3.5 × 13 bare metal coronary stent leading to successful recanalisation of the left pulmonary artery ( b ). Four days later, hand injection showing constricted right ductus arteriosus and functionally closed right pulmonary artery ( c ). The right ductus was stented using a 3.5 × 24 bare metal coronary stent leading to successful recanalisation of the right pulmonary artery ( d ).
Discussion
Bilateral arterial duct is a very rare anomaly, presumably due to maldevelopment of the sixth aortic arch during early embryogenesis. It has been more frequently described in pulmonary atresia, usually with non-confluent pulmonary arteries, with a high association with heterotaxy syndrome. Reference Peirone, Abdullah, Dicke, Freedom and Smallhorn1 It has been more rarely reported in the setting of other complex CHDs such as hypoplastic left heart syndrome. Reference Gray, Sorabella, Berry, Padilla, Law and Dabal2 In pulmonary atresia with ventricular septal defect, non-confluent pulmonary arteries, and in the absence of major aorto-pulmonary collateral artery, each branch pulmonary artery is supplied independently by its ipsilateral ductus arteriosus, as seen in our case. Isolation of the pulmonary artery may occur early within the first days of life, or later on up to 12 months of age. Reference Waldman, Karp, Gittenberger-de Groot, Agarwala and Glagov3 Early neonatal physiologic ductal closure may result in abrupt pulmonary hypoperfusion and life-threatening hypoxia, thereby prompting emergent intervention. Surgical management has been applied successfully, consisting in either bilateral modified Blalock–Taussig shunt or unifocalisation of the non-confluent pulmonary arteries under cardiopulmonary bypass. Reference Nakamura, Kanno and Nishioka4,Reference Stamm, Friehs and Zurakowski5 Both surgical strategies are challenging, especially in low-birth-weight infants, and may result in pulmonary arteries distortion and decreased long-term patency due to excessive tension on surgical anastomoses. Reference Stamm, Friehs and Zurakowski5 Ductal stenting carries a < 1% procedure-related mortality rate but a 9%–13% complication rate in the current era, with reported major acute (ductal spasm, stent malposition or embolisation, and acute stent thrombosis) and late (pulmonary overflow and neointimal proliferation) complications. Reference Valdeomillos, Jalal, Boudjemline and Thambo6 Because of their flexibility and low profile, we used balloon-expandable coronary stents with favourable results and long-term patency of both pulmonary arteries. Ductal stenting in duct-dependent pulmonary circulation has however become widely accepted as a safe and efficient alternative to surgery, carrying a lower risk of postprocedural complications, extracorporeal membrane oxygenation (ECMO) use or mortality, as well as higher postprocedural oxygen saturation and Nakata index as compared to modified Blalock–Taussig shunt; Reference Abdelmassih, Menshawey and Menshawey7 it has also been shown to be effective in promoting a significant catch-up growth of duct-dependent discontinuous pulmonary arteries. Reference Santoro, Capozzi and Giordano8 The benefits-to-risks ratio for ductal stenting has been shown to be less favourable in infants with a tortuous ductus, a body weight< 2.5 kg, and/or an insufficiently constricted ductus. Reference Alwi and Mood9 High success rates have been achieved in experienced hands, and in a recent report of 38 ductal stenting in low-body-weight infants with duct-dependent pulmonary circulation, Al Nasef et al. showed that ductal stenting is feasible and effective in neonates < 2.5 kg, promoting adequate pulmonary artery growth. Reference Nasef, Shahbah and Batlivala10 Reintervention rates are relatively high in this weight group, though many are planned to allow for optimal pulmonary artery growth before a definitive operation. According to ductal origin, ductal morphology, and ductal length, various techniques and vascular approaches may be considered. In tetralogy of Fallot with pulmonary atresia, the ductal morphology is often complex and ductal stenting is usually performed via an antegrade approach through the femoral vein, or a retrograde route via the femoral artery, or even via a common carotid or axillary artery surgical cut-down.
Conclusion
Although rarely observed, clinicians should be aware of the possibility of bilateral ducts with non-confluent pulmonary arteries, especially in the setting of pulmonary atresia, and that bilateral ductal stenting may be a feasible, safe, and effective first-step palliation towards further lower-risk cardiac surgery.
Acknowledgements
We gratefully acknowledge Dr Luc Morin, GCS HUGO, AVIESAN, and FHU PRECICARE.
Financial support
A.-E.B is supported by the French Government as part of the “Investments of the future” programme managed by the National Research Agency (grant reference ANR-16-IDEX-0007), FHU PRECICARE.
Competing interests
None.
Ethical standards
The authors assert that all procedures contributing to this work comply with the Helsinki Declaration of 1975, as revised in 2008.





