Food insecurity is defined as limited or uncertain access to sufficient nutritious food(Reference Bickel, Nord and Price1). Food insecurity is associated with various infectious and non-communicable health outcomes and is a major public health issue for people living with HIV (PLHIV)(Reference Masa, Chowa and Nyirenda2,Reference Palar, Napoles and Hufstedler3) . Food insecurity is associated with poor HIV outcomes through psychosocial, behavioural and nutritional pathways(Reference Weiser, Young and Cohen4). Moreover, nutrition has a direct impact on viral load beyond behavioural pathways (i.e. antiretroviral therapy (ART) adherence and missed clinic appointments)(Reference Weiser, Young and Cohen4). Food insecurity is associated with decreased efficacy of ART and reduced ART adherence, which can lead to the immunologic decline and progression to AIDS, and increased morbidity and mortality for PLHIV(Reference Bangsberg, Perry and Charlebois5,Reference Martin, Palar and Derose6) . A study among PLHIV experiencing food insecurity in Honduras found that nutritional counselling improved ART adherence, HIV outcomes and reduced food insecurity for participants regardless of nutrition status(Reference Derose, Felician and Han7–Reference Martinez, Palar and Linnemayr9).
Relatedly, self-management behaviours such as consuming a quality diet, with quality defined as how well an individual conforms to dietary recommendations(Reference Alkerwi10), are positively associated with improved health outcomes for PLHIV(Reference Webel, Perazzo and Dawson-Rose11). A multinational qualitative study found that among PLHIV in resource-poor settings, chronic stress and structural barriers such as poor food diversity, unemployment and poverty impeded engagement with dietary behaviours(Reference Webel, Perazzo and Dawson-Rose11). An intervention that targeted food insecurity by providing community-based food assistance found decreased consumption of fats, increased consumption of fresh fruits and vegetables and increased adherence to ART(Reference Weiser, Young and Cohen4).
The Dominican Republic has the highest overall prevalence of HIV among Spanish-speaking countries in Latin American and the Caribbean at 1 % of the population as of 2017(12), with cases concentrated in urban centres, where 81 % of the population lives, a pattern that is consistent across Latin America and the Caribbean(13). Adherence to ART treatment in the country is estimated at 53 %(14). Previous work in the Dominican Republic found that 69 % of PLHIV reported moderate to severe food insecurity(Reference Derose, Ríos-Castillo and Fulcar15). To inform future nutritional counselling interventions among PLHIV who experience food insecurity in urban and peri-urban areas of the Dominican Republic, we sought to elucidate what factors influence dietary decisions and behaviours in relation to HIV self-management.
Methods
Study
This qualitative study comes from a formative research component of a larger study conducted by the RAND Corporation, a non-profit research organisation and the Universidad Autónoma de Santo Domingo, in collaboration with other Dominican partners: The Ministries of Agriculture and Public Health, the Dominican National HIV/AIDS Council (CONAVIHSIDA) and the World Food Programme. The aim of this larger study was to develop and pilot test an integrated urban gardens and peer nutritional counselling intervention with food insecure PLHIV to improve ART adherence and treatment outcomes. The formative research component of the study involved qualitative interviews with patients at the two study clinics to explore food insecurity, nutritional knowledge and behaviours, ART adherence and other factors influencing HIV outcomes to inform the development of the integrated intervention. Interviews also explored participants’ understanding of recommended dietary behaviours for PLHIV. Recommended dietary behaviours are constructed from the ‘pilón de la alimentación’, national nutritional guidelines or food-based dietary guidelines and the World Food Programme’s guide for nutrition for PLHIV, such as eating smaller meals more frequently and taking medications with food to minimise side effects(16,17) . The information on nutritional knowledge, beliefs and behaviours would be used for the parent study to adapt a peer nutritional counselling guide developed in prior work in Honduras(Reference Martinez, Palar and Linnemayr9).
Recruitment and sampling strategy
The Dominican Republic has a total of seventy HIV clinics and twenty-six are located in the capital of Santo Domingo. RAND, together with local partners, identified two urban, government-operated clinics in central and northwestern Dominican Republic that are of similar size (500–800 patients on ART), offer similar standards of care and have comparable staff composition (i.e. 1–2 primary care providers, 1–2 nurses and 1+ peer counsellors) for the study. Both clinics were about a two-hour drive from each other to facilitate study coordination but avoid cross-contamination.
Adults living with HIV were screened for eligibility by two Dominican research assistants, one per clinic, using a structured questionnaire. Eligibility criteria included (i) being a registered patient at the HIV clinic, (ii) residing in an urban or semi-urban area, (iii) being 18 years and older and (iv) having moderate or severe household food insecurity according to the Escala Latinoamericana y Caribeña de Seguridad Alimentaria (α = 0.91–0.96 across LAC countries)(18). The study team purposefully recruited a gender-balanced and ART adherence-balanced sample (i.e. self-reported adherence problems v. not). Participants who met the criteria were provided with additional information about the study and, if interested, were invited to participate. Participants were recruited until thematic saturation was reached.
Data collection
The semi-structured interview guide was developed collaboratively by the research team and local partners. The guide covered topics related to frequently consumed foods, knowledge, attitudes and beliefs about dietary behaviours, acquisition and intra-household distribution of food, food insecurity experiences, economic security, access to health services and ART adherence. Some items were drawn from a prior study examining food insecurity among women living with HIV in the Dominican Republic(Reference Derose, Payán and Fulcar19), and questions included, ‘what does a healthy diet mean to you?’ The interview guide can be in the online supplementary materials for reference. Socio-demographic data were collected using a structured questionnaire, which included age, gender, nationality, educational attainment, occupation, civil status, composition of the household and monthly household income.
In-depth interviews were completed between May and September 2017 by two trained local interviewers. All interviews were conducted in Spanish, lasted between 60 and 90 min, and were audio recorded with permission from participants. Audio recordings were transcribed verbatim by a Dominican research assistant and verified by team members. Institutional Review Boards from RAND, Universidad Autónoma de Santo Domingo and the Dominican Ministry of Public Health approved the study protocols. All study participants provided oral consent.
Data analysis
Transcripts were uploaded to Dedoose(20), a web-based text management and analysis software. Two coders (G.A. and D.P.) read and coded the transcripts independently and used a multi-stage exploratory approach to develop a codebook that corresponded to the main topics of interest included in the interview guide. This approach involved creating initial codes based on the interview guide, coding the data and then grouping similar codes to create categories(Reference Hickey and Kipping21,Reference Klaus22) . In re-reading the interviews, coders wrote memos of text that did not adhere to the established coding structure. These memos were used to generate emergent codes related to the larger phenomenon of food insecurity among PLHIV in the Dominican Republic(Reference Ellis, Strauss and Corbin23). All coding and analyses were completed in Spanish. Any discrepancies in coding were resolved by consensus.
For the current study, the codes of interest focused on participants’ perceptions of the benefits of eating healthy food, the impact of a poor diet for PLHIV, where food can be obtained, and financial considerations. Using content analysis to describe what a ‘healthy diet’ meant among PLHIV(Reference Hsieh and Shannon24), the first author read through each code report and developed analytical memos describing prominent themes. All excerpts were analysed using matrixes organised by participant and code, which allowed for constant comparison of patterns across participants and within codes(Reference Hsieh and Shannon24). Preliminary themes were discussed among co-authors and partners in the Dominican Republic for feedback. Selected exemplary quotations were translated to English by the first author and reviewed by other bilingual authors (D.P., G.A. and K.P.D.) for inclusion in this paper. Themes were arranged using constructs adapted from three health behaviour frameworks and theories. The social ecological framework posits that factors at multiple, interacting levels, individual, interpersonal, community/organisational and policy can influence health behaviours(Reference Glanz, Rimer and Viswanath25). The theory of reasoned action aims to understand attitudes and beliefs individuals have towards their health and the health of others(Reference Glanz, Rimer and Viswanath25). Knowledge is a statement of facts about health behaviours or outcomes, whereas attitudes are an individual’s beliefs about the positive or negative outcomes that result from performing a behaviour(Reference Glanz, Rimer and Viswanath25). The health belief model argues that health behaviours function via perception, including perceptions of susceptibility or severity of a condition as well as benefits of engaging in a behaviour(Reference Glanz, Rimer and Viswanath25).
Results
Thirty-two PLHIV participated in the current study (Clinic 1 = 18; Clinic 2 = 14). The mean age of participants was 45 (sd 10·5) years, ranging from 26 to 72 years. Half of the sample were women, and a majority (62·5 %) reported completing at least primary school. Most participants were unmarried but living with a partner and 37 % reported a monthly household income of <5000 Dominican pesos (typical monthly income about $US 105 or $US 3·50/d; lower middle-income class poverty line $US 3·20/d per capita(26)). About 68 % of participants had experienced severe food insecurity and 32 % experienced moderate food insecurity (Table 1).
Table 1 Participant demographics across two Dominican HIV clinics (n 32)

Several factors contributed to how food insecure PLHIV engaged in dietary behaviours to self-manage their HIV. We present the results organised by the social ecological framework to demonstrate how unpredictability and lack of control impacted individual decision making and dietary behaviours and PLHIV’s interactions within larger social, cultural and environmental contexts (Table 2)(Reference Sallis, Cervero and Ascher27).
Table 2 Multi-level factors influencing dietary behaviours among people living with HIV (PLHIV) who experience moderate to severe food insecurity
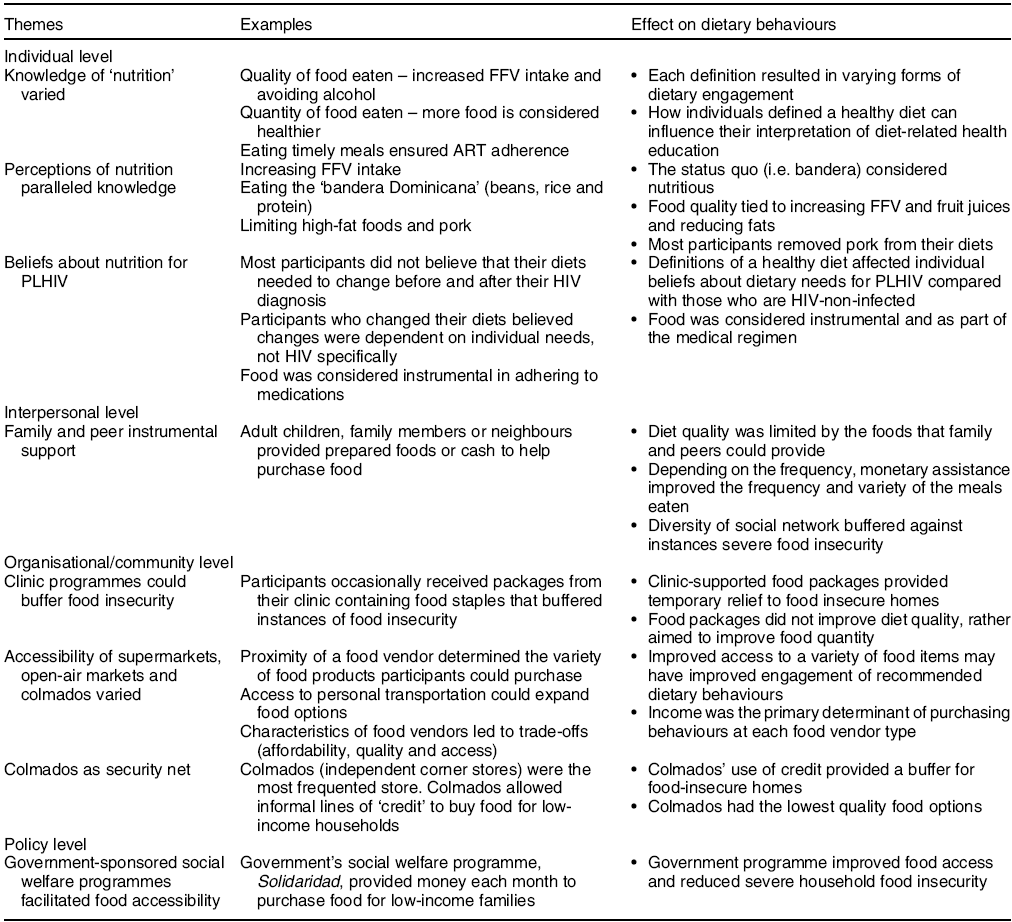
FFV, fresh fruit and vegetable.
Individual
Individual-level factors affecting dietary behaviours to self-manage HIV consisted of knowledge, perceptions and beliefs regarding what constitutes a ‘healthy diet’. Across all three domains, participants interpreted their nutritional needs in three ways: quality, quantity and timeliness.
Dietary knowledge
A majority of participants (n 18) primarily interpreted a healthy diet as being synonymous with quality. Quality meant consuming fresh fruits and vegetables and avoiding ‘vices’, particularly alcohol. Less than a third of participants interpreted a healthy diet as the quantity of food consumed. Participants described needing to feel full or avoid hunger throughout the day to manage their HIV. Participants said they consumed larger portions to counteract the amount of HIV medication in their body, as described by a 38-year-old female participant:
Yes, you have to eat much more, depending on the amount of medication, or the number of pills you’re taking.
Timeliness, described as eating meals on a regular schedule, was also emphasised by some participants. Eating regular and, ideally, three meals a day, at the same time every day, was deemed necessary for successfully ART adherence and essentially served as a feedback loop to remind participants to regularly eat and take their daily medications, as explained by a 36-year-old female participant:
To not be careless or neglectful [of my diet] means that at 7:00 a.m. I have to eat breakfast, and I have to be punctual – at 7:00 a.m. exactly – because it is something that my body needs in order to take the medication.
Participants’ knowledge about a healthy diet came from multiple sources, and around half of participants mentioned clinic staff during health talks and appointments (n 16). The second, but a much less common source of information, were friends and family who were familiar with HIV. A couple of participants described getting dietary information from national programming, or ‘from the street’. About one-quarter of participants stated that they did not get nutritional information from any external source.
Perceptions about a healthy diet
Behaviours that comprised a healthy diet for PLHIV conformed with how participants defined nutrition. Most participants perceived diet quality and quantity as complementary, for example, increasing water and natural fruit juice consumption and reducing alcohol consumption. Relatedly, participants stated that PLHIV needed to increase their consumption of fresh fruits and vegetables because they provided nutrients to improve physical health. Additional beneficial foods mentioned included beans, rice, dairy products and protein, which form the traditional, daily Dominican meal known as the ‘bandera Dominicana’. Equally emphasised was the need to limit fat consumption and avoid high-fat foods. Almost half of the participants explicitly mentioned avoiding pork and pork-derived foods because they were perceived to be ‘unhealthy’ or ‘dirty’ and therefore bad for health. A 58-year-old female participant further explained how pork had a direct effect on HIV: ‘You can eat anything, except pork because pork gives strength to the [HIV] virus’.
Additionally, street foods (i.e. fried foods with little nutritional content) were identified as foods that should be avoided due to their high fat content and preparation. Street foods were perceived to make PLHIV more susceptible to adverse outcomes, as described by this 39-year-old female participant:
You can’t eat street food. Because the cooking oil is not the same as what we use at home. Maybe they re-use the oil multiple times and that’s harmful. If not, then they may cook with too much oil. I just think that it’s not healthy to eat street food for those of us that have HIV.
Overall, increasing or decreasing the quantity of healthy and non-healthy foods, respectively, was how PLHIV perceived engaging in dietary behaviours to benefit their HIV self-management.
Beliefs about healthy eating for people living with HIV
Variability in how participants defined a ‘healthy diet’ may have influenced whether or not they believed there were differences in dietary recommendations for PLHIV compared with those without HIV. About half of participants believed that there are differences and described not changing their own dietary habits before and after learning of their HIV diagnosis. A 40-year-old male participant reiterated this and said he had instead focused on moderating the quality of food:
Interviewer: How is your nutrition different?
Participant: No, it’s not different, because you live a normal life.
I: Normal how? What do you mean by a normal life?
P: Normal, well, I have a condition, but I can eat anything in moderation and not overeat. Because the quality of food not the quantity is more important.
Remaining participants expressed a belief that there were differences in dietary behaviours between PLHIV and those with HIV negative status or that dietary changes depended on individual needs as described by a 36-year-old female participant:
Due to HIV, we do not achieve homeostasis because not everything interacts well with the body. We have to understand that foods that we have been prohibited to eat [by doctors] are limited because they could cause a shock to our health.
Participants believed that poor dietary habits, stemming from a lack of access, increased susceptibility to illnesses, worsened health outcomes and contributed to premature mortality. Gendered beliefs were espoused about the risks of poor nutrition while living with HIV. Men noted that poor nutrition affected their ability to be ‘healthy for working’, whereas women explained that poor nutrition negatively impacted their ability to take care of others.
Most participants said their primary motivation for engaging in a healthy diet was adherence to medication. Medications were often prescribed to be taken with food and thus incentivised eating in a timely fashion to increase ART effectiveness and reduce side effects. Several participants said the medications were very ‘strong’ and placed a heavy burden on the body. Overall, participants expressed a belief that food played an integral role in maintaining a satisfactory quality of life.
Interpersonal
Family and peers were the most cited sources of social support for reducing instances of food insecurity and promoting the ‘healthy diet’ participants desired. Most participants described receiving groceries or meals from family and neighbours at varying frequencies. Family members (n 11) were the single most referenced source of support and often purchased and/or delivered groceries for participants. Although family provided instrumental support by providing food, this provision came along with uncertainty, as it was inconsistent, and provided only short-term relief from food insecurity. Neighbours played a similar role to family members, but reciprocity was understood, as described below by a 26-year-old female participant:
P: Sometimes [my neighbors] gift me with a hand of bananas.
I: How often do you receive bananas?
P: Depends. Always share with others, so that when you don’t have enough food then someone will always come by with something to share.
However, some participants described receiving food consistently from kin or other members of their social network. A 72-year-old woman described getting a midday meal delivered nearly every day from her daughter who lived a town away. More commonly, a family member would send groceries each month. Regardless of the frequency of the provision of food, participants’ diet variability was restricted to what members of their social network could provide, thus suggesting that participants had limited autonomy or control, to engage in recommended dietary behaviours in the face of food insecurity.
Assistance was not only evident in the provision and preparation of food from others but also money such that participants could purchase their own food. While this form of economic support was less common, one-fifth of participants explained how they used these monies to purchase food, exercising greater control in dietary purchasing behaviours and more involvement in their own decision-making. The following 45-year-old female participant described receiving money from her son each pay period to buy food.
P: I have a son and sometimes he gives me a hand.
I: What type of help do you receive from him?
P: He gives me about $1,000 pesos [approximately US$20], and with that I buy my food.
I: How frequently does he send you money?
P: When he gets his money…sometimes each payday.
Having direct access to funds allowed participants to purchase preferred foods that were deemed appropriate, but it did not thwart concerns about food insecurity. The few participants that received financial support were still constrained by a fixed income; therefore, as funds depleted, so did their food options.
While actively receiving food directly or through monetary assistance were the most commonly described form of interpersonal support, its unpredictability did affect dietary behaviours. Participants sometimes described this support passively, stating that they ‘wait for food to appear’ and therefore would delay eating.
This idea of waiting was sometimes tied to Christian sensibilities such that patients felt that food availability was outside of their control, but that ‘God will provide’, as described by a 45-year-old female participant:
I: Do you believe that you have sufficient food available to you?
P: I have what God provides…sometimes we do not have enough, but you have to take what God gives you.
The reality of food insecurity for PLHIV required leaning on an extensive social network to mitigate severe manifestations. These sources of support were diverse and served a central role in dietary behaviours ranging from what foods were available, the quantity of the food for each meal and the predictability of food access. There were no differences in support between partnered and non-partnered participants.
Community/organisational
Dietary behaviours were also affected by community or organisational factors. Some participants said their dietary behaviours were influenced by their respective clinics who also provided food; however, these provisions were unpredictable. Participants mentioned receiving supplementary foods at different intervals – either once a month, every few months or even once a year for holidays – showcasing an inconsistency in food assistance.
In the broader community, dietary behaviours were influenced by the availability of food stores, as stated by a 28-year-old female participant:
On Saturday I go to the mercado and buy the fruit and vegetables for the week. Then I go to the supermarket and buy the staples: rice, oil, beans, spaghetti, and whatever else we need. If something runs out, then I go to the colmado.
As this participant explained, people can frequent supermarkets, open-air markets (mercado) and colmados, independently owned corner stores. According to participants, supermarkets provide the greatest variety compared with mercados and colmados, but both supermarkets and mercados have greater quality foods such as fresh fruits and vegetables and lean proteins than colmados, which tend to carry a limited selection of staple items such as rice, beans, canned meats, seasonings, and at times, some fruit.
Accessibility – described in terms of both physical distance and food affordability – was another factor influencing food-purchasing behaviours. A participant described regularly buying food at a mercado where they could purchase rice, beans, oil and other necessary items, but public transportation was needed to access the mercado, which meant an additional cost of 100 pesos ($US 2) roundtrip. Transportation is costly considering the minimum wage of $US 6–8/d. Therefore, when participants did not have money for transportation, they were limited to their local colmados for food. As described below by a 30-year-old female participant, colmados did not always carry the food items of interest:
What happens is that sometimes the colmado does not have items I need, so then I have to go to mercado instead.
Despite some of the limitations described, colmados were the most cited food store among all participants (n 19). Colmados served as either the sole location for food purchases or as a complementary location. One unique benefit, as described by several participants, was that colmado owners would provide customers with an informal line of credit. As colmados are embedded within communities and patrons tend to be local and can establish rapport, this allowed patrons to obtain food in advance of payment, as described below by a 59-year-old male participant:
That’s why sometimes I tell the colmado owner, when I have money, I will buy food and if I come up short, then I’ll bring the rest of the money on Sunday afternoon or Saturday in the afternoon.
As such, colmados served as a safety net for food purchases. While over two-thirds of participants described purchasing food from stores, some did not. Participants lamented their limited access to fresh fruits and vegetables in their communities; however, several described growing their own fruits and vegetables because of the inaccessibility of stores or unavailability of items at colmados (n 7). The accessibility of food vendors, by distance and price, as well as the availability of a variety of foods was important factors influencing participants’ dietary behaviours.
Structural/policy
Labour market engagement
The majority of participants were not actively engaged in the formal sector, which appeared to affect their dietary behaviours. Participants explained how their limited household income constrained their ability to buy staples like rice. One participant noted that if he had access to more money, he would prefer to buy more perishable foods such as salami or cheese, a common accompaniment for meals.
Food quantity was a common indicator of financial constraints. Participants described moments when they were unable to purchase all the necessary groceries due to scarce financial resources, which meant participants managed multiple priorities. Dietary behaviours were described within the context of experiencing hunger, which was in direct contrast to how participants ideally wanted to engage in ‘healthy’ dietary behaviours. As one participant noted, even if he could purchase rice and beans, he could still lack the money to pay for the gas to cook the food. Other participants admitted they went hungry because the household had to prioritise other basic needs, such as utilities and rent above food.
The notion of ‘waiting for food to appear’ emerged when participants described economic constraints. Some participants explained that unemployment reduced their self-efficacy to nourish themselves as they saw fit and constrained their ability to purchase the quality of food they required, the quantity of food they desired and eating meals on a regular schedule. A 37-year-old male participant explained how his control over dietary decisions changed when he became unemployed:
Whereas before, when I had a job, if I needed to buy a banana, I could. I did not have to wait for someone to bring me banana. But now that I do not have a job, things are much harder…harder to get…you have to wait for people to help out.
Government support
The Dominican government oversees a social welfare programme called Solidaridad, which provides qualified households with a monthly stipend of 800 pesos (approximately $US 18) to purchase food and other household essentials. Less than one-third of participants indicated they had access to the Solidaridad card. These participants described the benefits of the programme and how useful it was for purchasing staple foods (e.g. rice, beans) each month.
For the others, like this 36-year-old female participant, receiving government assistance was unpredictable and outside of her control.
I: Have you received food or assistance from the government or private organization?
P: No, it was a while back that they collected my information but I’ve never been selected.
I: They only took your information? Who took your information?
P: Yes. It was the government. But they have never called me…I don’t have card or anything.
A few participants explained that they received other forms of government support, specifically ‘food baskets’ containing essentials such as rice, oil, canned foods and sugar. These offerings were unpredictable and were provided anytime from a few to once a year.
Participants described how access to consistent labour market opportunities and reliable government assistance could improve the capacity of individuals to eat a greater variety of foods items with greater consistency. Consistent access to food was described as a way of reducing food insecurity severity for PLHIV and their households.
Discussion
Our findings demonstrate that dietary behaviours among PLHIV in the Dominican Republic who experience food insecurity are affected by multiple levels of influence, which can affect HIV-related outcomes including ART adherence. These factors do not work in silos, rather they interact at the individual, social and structural levels and are amplified by the unpredictability and lack of control that stem from experiencing food insecurity. At the individual level, we found that participants had varying definitions of a healthy diet, which in turn may have affected how they understood and engaged in recommended dietary behaviours. Notions of a healthy diet encompassing quantity, quality and timeliness is a cultural phenomenon that can be applied to Dominican populations managing other chronic conditions that require taking medications with food, such as type 2 diabetes(Reference Gonzalez Rodriguez, Wallace and Barrington28). Differences in perceptions of a healthy diet were supported by a qualitative study conducted in the United States, Puerto Rico and Botswana, in which PLHIV varied in their consideration of whether engaging in a healthy diet was as important as ART adherence or of lesser importance(Reference Webel, Perazzo and Dawson-Rose11). Participants also designated diet in a functional sense, particularly as a way to remain adherent. Our results demonstrate the value of nutritional counselling for PLHIV to improve dietary knowledge, beliefs, perceptions and behaviours to improve HIV-related outcomes.
While participants wanted to engage in what they considered to be a healthy diet through quality, quantity and timeliness for the sake of their ART self-management; social and environmental contexts demonstrated how unpredictability and lack of control due to food insecurity impeded engagement in their recommended dietary behaviours. Social networks were important in providing instrumental support for PLHIV. Instrumental support alleviated instances of food uncertainty for participants depending on the consistency of this assistance. Studies conducted in resource-limited areas found that instrumental support was associated with food security and it protected against seasonal food insecurity(Reference Hadley, Mulder and Fitzherbert29). Studies have shown that households of PLHIV with greater social capital more easily obtain meals or groceries from neighbours or receive rides to the supermarket(Reference Tsai, Bangsberg and Frongillo30). However, the inherent unpredictability of social support suggests that it is not a permanent solution for ensuring adherence to recommended dietary behaviours. While instrumental support does help alleviate instances of food uncertainty, it does not address the larger, structural concern of food insecurity. Also, while different members of the social network provide groceries or meals, this assistance may not always fall in line with recommended dietary behaviours.
Colmados served as one of the primary food stores for participants, despite their limited food variety and quality. Participants qualitatively indicated that food was most expensive in colmados, followed by supermarkets, then mercados. High food prices, lack of food variety and transportation difficulties all contributed to low-quality food purchases for participants. This is line with research conducted on food insecurity in low-income, rural communities in the United States, which found that local food environments contributed to food insecurity(Reference Garasky, Morton and Greder31). Although participants described their limited food variability, several participants had fruit trees on their own or a neighbour’s land or urban gardens to increase access to fresh fruits and vegetables. As colmados are ubiquitous across the country, the Ministry of Public Health could focus their efforts on reducing the salt, trans-fat and sugar content in foods produced in country and work with colmado owners to improve the quality of items sold. This may help to increase the quality and variety of foods at colmados.
Due to HIV-related stigma in the labour market, PLHIV may experience a disproportionate adverse socio-economic impact, thereby increasing PLHIV’s vulnerability to food insecurity(Reference Derose, Payán and Fulcar19,Reference Conyers, Richardson and Datti32) . For some participants, government-sponsored welfare programmes, such as Solidaridad, were sources of institutional aid that helped address food insecurity(33). The benefits associated with the Solidaridad programme include monthly funds for the purchase of food, two gallons of gas to cook food and an electricity subsidy. For patients enrolled in this programme, trained staff or peer counsellors can provide education on food budgeting and selection, tailored by household budget. However, most participants were not enrolled in the Solidaridad or similar programmes; therefore, expanding the programme’s reach and increasing transparency around the enrollment process could increase the proportion of PLHIV enrolled, thereby addressing the high levels of food insecurity PLHIV in the Dominican Republic.
Our participants resided in resource-poor communities, resulting in their dietary needs competing against other necessities such as housing and transportation. Qualitative studies suggest that PLHIV face challenges and various life stressors that may affect how they engage with dietary behaviours, such that competing needs take precedent over self-management behaviours(Reference Webel, Perazzo and Dawson-Rose11,Reference Payán, Derose and Fulcar34) . A retrospective cohort study in La Romana, Dominican Republic, found that participants often had to prioritise necessities such as food and housing over their self-management behaviours, primarily adherence to ARV(Reference Winter, Halpern and Brozovich35).
Limitations
The findings represent the experiences of the participants and may not be generalisable to other PLHIV in the Caribbean. Furthermore, we conveniently sampled adults at clinics where they received care; therefore, the full range of experiences for PLHIV who were linked and not linked to care may not be fully represented. The current study was also constrained to PLHIV who reside in urban and peri-urban settings and therefore may not reflect the experiences of those living in rural settings. Additionally, information on social exclusion, work unions, and educational access were limited due to the paucity of national and sub-national information available, and the information we were able to reliably collect from participants, which would have provided additional context regarding the vulnerability of this population.
Conclusion
Dietary behaviours are influenced by unpredictability and lack of control at multiple levels of influence. Primary among them are the dimensions of a healthy diet (quantity, quality and timeliness), leveraging social and community networks to reduce incidents of food insecurity, and the role of government programmes to counteract the socio-economic vulnerabilities that are a reality for PLHIV. Interventions that address one or various of these levels can improve the dietary behaviours of PLHIV in the Dominican Republic who experience food insecurity.
Acknowledgements
Acknowledgements: The authors thank the participants for their generosity in providing their time as well as the health clinic staff and providers who participated. The authors would also like to thank Dr Victor Terrero, Director of CONVIHSIDA, for their ongoing support for our efforts to understand and address food insecurity among people living with HIV. The authors thank colleagues from the Universidad Autónoma de Santo Domingo Universidad Autónoma de Santo Domingo and Ministry of Public Health Nutrition Program for providing feedback on preliminary results as well as Dr Yarovis N. Ortíz Rivera and Dr Eves Priscila Reyes Pujols who provided data collection support as research interns with the Ministry of Public Health. Financial support: The current work was supported by the National Institute of Mental Health of the National Institutes of Health under Award No. R34MH110325. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Conflict of interest: None. Authorship: D.D.W. formulated the research questions, conducted the analysis and wrote the article. D.D.P. formulated the research questions and provided extensive edits. A.T.P. provided extensive edits and confirmed contextual assumptions throughout the writing process as well as served as nutrition expert for the project. G.A. conducted the analysis and provided extensive edits. M.A.F. provided extensive edits and contextual feedback throughout the writing process. R.A. provided extensive edits and contextual feedback throughout the writing process. K.P.D. formulated the research questions, provided extensive edits and contextual feedback throughout the writing process. Ethics of human subject participation: The current study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving research study participants were approved by the RAND Corporation Institutional Review Board and the Universidad Autónoma de Santo Domingo ethical review board. Verbal informed consent was obtained from all subjects/patients. Verbal consent was witnessed and formally recorded by research team.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980020002694





