Progressively fewer people are eating breakfast(Reference Siega-Riz, Popkin and Carson1, Reference Nicklas, Reger and Myers2), with up to 30 % of adults in the West typically skipping this meal(Reference Leidy and Tacki3, Reference Haines, Guilkey and Popkin4). Reasons given for skipping breakfast include lack of time and late rising(Reference Ortega, Requejo and Redondo5), lack of motivation to prepare breakfast(Reference Moore, Tapper and Murphy6), desire to lose weight(Reference Sjoberg, Hallberg and Hoglund7), lack of appetite(Reference Rampersaud, Pereira and Girard8), feeling nauseated or weak and tired(Reference Unusan, Sanlier and Danisik9), and smoking (which can suppress appetite in the morning(Reference Keski-Rahkonen, Kaprio and Rissanen10)).
However, many studies have indicated that skipping breakfast is a risk factor for weight gain and obesity(Reference Croezen, Visscher and ter Bogt11) and that consumption of breakfast is inversely associated with BMI(Reference Kosti, Panagiotakos and Zampelas12, Reference Dubois, Girard and Potvin-Kent13). In their study investigating breakfast, BMI and physical activity and fitness, Sandercock et al. (Reference Sandercock, Voss and Dye14) succinctly summarised the relationship between eating breakfast and BMI: breakfast eaters have a lower BMI and better long-term weight control. However, as Sandercock et al.(Reference Sandercock, Voss and Dye14) pointed out, the mechanisms by which breakfast influences BMI have so far not been identified. One likely reason for this is the cross-sectional design of the majority of studies, relying largely on self-reports, which cannot explore cause-and-effect relationships. Some of these studies have indicated that individuals who skip breakfast consume larger amounts later in the day, which is likely to contribute to greater BMI. For example, Hubert et al.(Reference Hubert, King and Blundell15) reported that participants given low-energy breakfasts had greater energy intakes at lunch compared with those given high-energy breakfasts, whereas it has been observed that there is a greater consumption of unhealthy snacks in teenagers who skip breakfast(Reference Utter, Scragg and Mhurchu16). However, most other cross-sectional surveys have reported no significant difference in overall energy intakes between breakfast eaters and skippers(Reference Song, Chun and Kerver17–Reference Ruxton and Kirk19), some even noting an increase in energy intake(Reference Timlin, Pereira and Story20).
In addition to differences in energy intakes, breakfast skippers often have less than adequate dietary profiles(Reference Galvin, Kiely and Flynn21). It has been shown(Reference Vossenaar, Montenegro-Bethancourt and Kuijper22) that breakfast is the meal that can provide the greatest amounts of vitamins A and D, thiamin, riboflavin, folate, Ca and Fe. In Western countries, ready-to-eat breakfast cereals (RTEBC) are frequently consumed at breakfast time(Reference Ruxton and Kirk19) and these have been associated with higher intakes of many micronutrients including Ca, Fe, riboflavin and folate(Reference Galvin, Kiely and Flynn21). Consumption of RTEBC during breakfast has also been associated with greater daily intakes of milk and Ca in both genders and at all ages in the USA(Reference Song, Chun and Kerver17). Other studies have confirmed that breakfast skippers tend to have lower intakes of most vitamins and minerals(Reference Nicklas, Myers and Reger23).
Timlin et al.(Reference Timlin, Pereira and Story20) found that, although the adolescents who ate breakfast in their study consumed greater amounts of energy per day, they had a lower BMI. The present study also observed that significantly more breakfast eaters regularly participated in strenuous activity than did intermittent breakfast eaters and hypothesised that breakfast eaters could be more active and would thus expend more energy compared with breakfast skippers. Further evidence to support this theory comes from surveys that have studied the frequency of episodes of high physical activity; for example, it was reported(Reference Keski-Rahkonen, Kaprio and Rissanen10, Reference Wyatt, Grunwald and Mosca24) that breakfast skippers participated in less exercise and had lower levels of physical activity compared with breakfast eaters. Cohen et al.(Reference Cohen, Evers and Manske25) also observed that a greater percentage of breakfast eaters exercised more than 3 times/week (85 % v. 69 %). Furthermore, an intervention study using breakfasting and physical activity to achieve a negative energy balance(Reference Carels, Young and Coit26) showed that, on days when breakfast was consumed, participants exercised for longer durations and consequently had greater energy expenditures as measured by accelerometers, while also ingesting a larger amount of food and drink.
However, the nature of the studies reviewed above makes it impossible to uncover the mechanisms linking the consumption of breakfast with energy balance, or, alternatively, determine whether breakfast is simply a marker of a healthy lifestyle. The present study takes an experimental approach to begin addressing why breakfast eaters typically have lower BMI compared with non-breakfast eaters by investigating whether eating or not eating breakfast affects dietary intake and energy expenditure. The possible confounding effects of morningness(Reference Nakade, Takeuchi and Kurotani27) and habitual breakfast eating habits are also explored.
Methods
A randomised cross-over experimental design tested whether breakfast affects activity, energy expenditure and daily energy intake. Participants were given breakfast during one week and had no breakfast or snacks until noon during the other week.
Forty-nine participants were recruited into the study (twenty-six female and twenty-three male participants) with a mean age of 22·6 (sd 3·9) years. Thirty-two of the participants (twenty-six female and six male participants) were students at Roehampton University and lived on or near the university campus. Seventeen male participants lived outside the campus, in the London area, and were recruited subsequent to data collection on the student cohort to increase the number of male participants. Participants were recruited using posters and by word of mouth. The entire study was conducted between January and November 2009.
Ethical approval to undertake the study was obtained from the Roehampton University Ethics Board. Before their acceptance into the study, interested individuals read and signed a participant consent form that included a statement that they had no illness or medical condition that might affect their full participation in the study. To obtain standard data on the relevant lifestyle and health of the participants, they were also asked to complete the International Physical Activity Questionnaire (IPAQ) to assess general activity levels(Reference Craig, Marshall and Sjöström28); general health was assessed using the Short Form 36 version 2 (SF-36v2)(Reference Ware, Kosinski and Bjorner29). During the second week of the study, participants completed the ‘Morningness’ questionnaire, which assessed human circadian rhythms in terms of morning and evening preferences(Reference Barton, Spelten and Totterdell30).
The majority of participants undertook the study for two consecutive working weeks in groups of either six or seven. During one of the working weeks, participants were provided with a breakfast in the designated food laboratory at the university between 08.00 and 09.00 hours (‘breakfast condition’). During the other week, although participants were still required to arrive at the food laboratory between 08.00 and 09.00 hours each day, no breakfast was provided (‘no-breakfast condition’). For each group of participants the order of the two weeks was randomised. Breakfast consisted of high-carbohydrate breakfast cereals with milk, and/or toast with butter and/or jam if requested. Participants were allowed to eat as much as they desired. In both conditions they were offered water, tea or coffee in the morning. Thus, breakfast was defined as food ingested between 08.00 and 09.15 hours. In both conditions, upon leaving the food laboratory, the participants were required to abstain from eating until mid-day; however, they were allowed to drink tea, coffee and water. From mid-day onwards, they were allowed to eat as and when they pleased. In both conditions, participants were informed that they could undertake whatever activities they wished to during the day.
On each day of the experiment, and in both conditions, participants were fitted with a heart rate monitor (s625x and RS400, Polar, Finland) and a pedometer (Yamax Digiwalker SW-200, Tokyo, Japan) on arrival at the food laboratory. The pedometer was clipped either to the waistband if available or to the front pocket of the participants’ clothing. Participants were required to wear both of these devices until they returned to the food laboratory between 17.00 and 18.00 hours each day, at which time the devices were removed and stopped. The exact time that the devices were started in the morning and stopped in the evening was recorded.
For three consecutive days of the week, matched across conditions, participants completed a food diary, following verbal and written instructions. They were asked to carry the diary with them at all times and record all that they ate and drank. A full description of the foods consumed was requested, including the type and brand, how the food was cooked and the amount consumed. For each group, the first day of completing the food diary was randomised. The nutritional information provided by the food diaries was analysed using Dietplan 6 (Forestfield Software, Horsham, UK) to produce estimates of nutrient and energy intake per day (kJ/d) and energy intake per hour of the day. Day was defined as starting when a participant awoke in the morning and ending when they went to bed at night.
The cohort of non-students followed the same procedure as described above, with the exception that they did not go to the food laboratory on campus and did not wear a heart rate monitor. These participants noted down the time of day when they started the study and when they attached and later detached the pedometer each day. A separate analysis of this cohort compared with the other male participants in the study did not reveal any differences in dietary intake, nor in responses to the health-related questionnaires.
The pedometers recorded a unit score each time the subject moved sufficiently such that the pedometer moved more than a threshold value. Thus, the count on the pedometers provided an approximate reading of the amount of bodily movement performed by the wearer during the time the pedometer was attached, which could be compared among participants. To account for differences in the duration for which the pedometer was worn, a ‘pedometer score’ was calculated for each participant for each day by dividing the count by the length of attachment time.
The heart rate monitors sampled and recorded heart rate every 5 s. From these data, the mean heart rate in the morning (from the time the monitor was started until mid-day) and during the day (from the time the monitor was started until it was stopped) was calculated. The mean morning heart rate and the mean day heart rate were calculated on the basis of the periods when heart rate was recorded for at least 80 % of the respective time frames; when more than 20 % of the data were missing, mean heart rate was not calculated.
Statistical analyses
All variables analysed were normally distributed, as determined by Kolmogorov–Smirnov tests, with α = 0·05, except for some of the questionnaire data that were non-parametric; further details are provided where pertinent. Pedometer score, mean morning heart rate and mean daily heart rate were each averaged within participant and condition. For each variable, a paired t test was used to test for differences between conditions. Energy ingested per day, and from noon until the end of the day, was averaged within participant and condition. A value hereafter referred to as the ‘energy intake-time index’ was calculated per participant to provide an overall relative indication per day of whether and at what time post noon (defined as 12.00 hours until the end of the day) energy was ingested. The index was calculated from the hourly energy intake data by summing, for each hour of the day, the multiple of the hour and the energy intake during that hour and dividing the result by 1000. The hours after midnight continued the 24 h clock up to and including 05.00 hours (i.e. 02.00 hours was represented as 26 h). Thus, participants who tended to eat later in the day had a higher energy intake-time index. The index was averaged within participant and condition. Again using paired t tests, the breakfast and no-breakfast conditions were compared in terms of both energy intake and the energy intake-time index, initially for all participants together. Thereafter, the conditions were compared considering male and female participants separately, in combination with high-frequency breakfast eaters and low-frequency breakfast eaters separately. High-frequency breakfast eaters were defined as those participants who stated in the self-completion questionnaire that they ate breakfast ≥5 times/week, and vice-versa for low-frequency breakfast eaters. Nutrient intakes per day were compared between conditions for all participants together and then for male and female participants separately. Nutrient intakes were compared with reference nutrient intakes(Reference Jenkinson, Stewart-Brown and Petersen32) using single sample t tests. The nutrients considered are listed in Table 3.
Questionnaires (IPAQ, SF-36v2 and morningness) were scored according to published guidelines(Reference Nakade, Takeuchi and Kurotani27–Reference Ware, Kosinski and Bjorner29). Data on physical activity and health status dimensions were not normally distributed, as is typical for data of this type(Reference Supina, Feeny and Carroll31). A data set containing representative SF-36v2 data for the UK was made available by Jenkinson (Oxford, UK)(Reference Jenkinson, Stewart-Brown and Petersen32); age- and gender-specific norms, mean, sd and 95 % CI were derived from this data set and used to assess the health status of our sample relative to these UK norms. Spearman's correlations were run to explore relationships between questionnaire variables. All statistical analyses were performed using Excel (Microsoft Corp., Seattle, WA, USA) and the Statistical Package for the Social Sciences statistical software package version 16·0 (2008; SPSS Inc., Chicago, IL, USA).
Results
The questionnaires revealed that a considerable number of participants never drank alcohol (male participants: 39 %; female participants: 42 %). On average, participants consumed breakfast 5 times/week; male and female participants did not differ in this respect. The percentage of participants who undertook low, moderate and high levels of activity was 22, 44 and 34 %, respectively. The SF-36v2 results (see Table 1) indicated that the sample had a health status similar to UK norms, except for relatively low scores in the category ‘general health’ and ‘bodily pain’ for female participants (P < 0·05).
Table 1 SF-36v2 results for breakfast sample in comparison with UK normative data for adults aged <40 years and without a chronic condition
SF-36v2, Short Form 36 version 2.
***P < 0·001.
Four participants were classified as evening types, three as morning individuals, with all others as neither; variation in morningness was small in the study sample. Morningness type could not be analysed further because of small numbers of morning and evening types. However, a significant, positive correlation was found between degree of morningness and frequency of breakfast consumption (ρ = 0·41; P = 0·005), which was not affected by gender or age. This correlation indicates that participants who tend to rise earlier and experience morning as a more active period of the day have breakfast on more days compared with those whose activity peak is towards the later part of the day.
Table 2 shows measures of activity (i.e. daily heart rate, morning heart rate and pedometer score). Mean morning heart rate was significantly higher during the breakfast condition across all participants (t 30 = 4·81, P < 0·001). This was also the case for female participants (t 24 = 4·532, P < 0·001). However, there were not enough data points to test for this difference within male participants (n 6). Across all participants, the mean daily heart rate and pedometer scores were not significantly different between the two conditions (t 30 = 1·21, P = 0·235 and t 43 = 0·18, P = 0·858, respectively). In addition, considering genders separately, the mean daily heart rate was not significantly different between conditions for female participants (t 24 = 0·690, P = 0·497), nor was pedometer score for either male or female participants (t 18 = 0·56, P = 0·583 and t 24 = 0·38, P = 0·710, respectively).
Table 2 Measures of activity level in male and female participants during weeks when breakfast was eaten and during weeks when breakfast was not eaten
***P < 0·001.
Table 3 shows energy intake, the energy intake-time index and nutrient intakes of participants. The energy consumed per day did not vary with condition (t 43 = 1·540, P = 0·131), either among male participants (t 20 = 1·593, P = 0·127) or among female participants (t 22 = 0·581, P = 0·567). Furthermore, no difference was found when high-frequency breakfast eaters were considered (male participants: t 13 = 0·883, P = 0·393; female participants: t 15 = 0·274, P = 0·788). However, in contrast to female participants, male low-frequency breakfast eaters consumed more energy per day during the breakfast condition (male participants: t 6 = 2·855, P = 0·029; female participants: t 6 = 0·999, P = 0·356; Fig. 1).
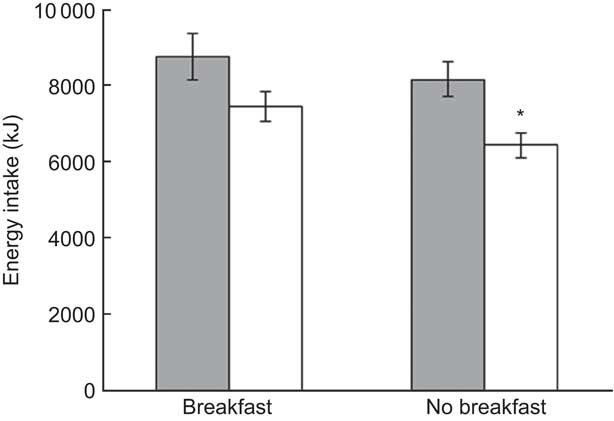
Fig. 1 Mean and sem of energy intake over 24 h for male participants who typically eat breakfast at least 5 times/week (![]() , high frequency) and for those who typically eat breakfast <5 times/week (
, high frequency) and for those who typically eat breakfast <5 times/week (![]() , low frequency), during the breakfast and no-breakfast conditions. *Significant difference (P < 0·05) between conditions
, low frequency), during the breakfast and no-breakfast conditions. *Significant difference (P < 0·05) between conditions
Table 3 Energy and nutrient intakes for male and female participants on breakfast and no-breakfast days
Significant difference between conditions, within gender: *P < 0·05, **P < 0·001; more consumed on breakfast days.
No significant difference was found in the energy intake-time index among male participants (t 20 = 1·725, P = 0·100); however, a significant difference was observed among female participants (t 22 = 2·235, P = 0·036). Considering high- and low-frequency breakfast eaters separately, high-frequency breakfast eaters had a higher energy intake-time index during the no-breakfast condition across all participants (t 29 = 3·696, P = 0·001); however, no difference was observed among low-frequency breakfast eaters (t 13 = 0·147, P = 0·886; Fig. 2). Female participants who habitually ate breakfast frequently had a significantly higher energy intake-time index during the no-breakfast condition (t 15 = 3·867, P = 0·002). Female participants who ate breakfast infrequently showed no difference between the breakfast and no-breakfast conditions (t 6 = 0·125, P = 0·905). There was no difference in the energy intake-time index in male participants who ate breakfast frequently, nor in those who did not (t 13 = 1·864, P = 0·085 and t 6 = 0·066, P = 0·949, respectively).
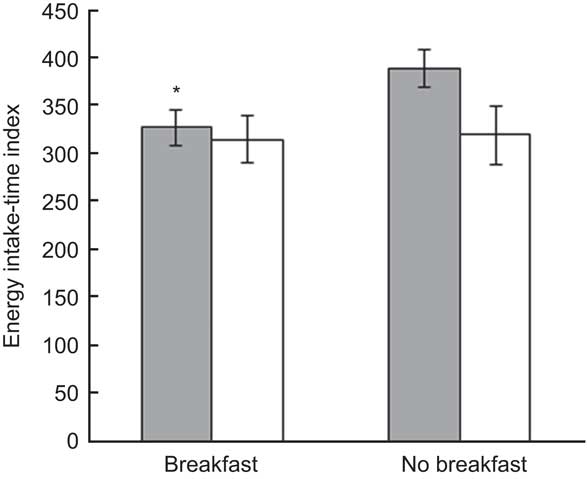
Fig. 2 Mean and sem of energy intake-time index (indicating how late in the evening food and drink was ingested) for participants who typically eat breakfast at least 5 times/week (![]() , high frequency) and for those who typically eat breakfast <5 times/week (
, high frequency) and for those who typically eat breakfast <5 times/week (![]() , low frequency), during the breakfast and no-breakfast conditions. *Significant difference (P < 0·01) between conditions
, low frequency), during the breakfast and no-breakfast conditions. *Significant difference (P < 0·01) between conditions
Intakes of both Ca and folate were significantly lower in female participants during the no-breakfast condition than during the breakfast condition (Ca: t 21 = 3·77, P = 0·001; folate: t 21 = 4·358, P < 0·001). Folate intake was also significantly lower in male participants during the no-breakfast condition (t 21 = 2·275, P = 0·033). However, there was no difference in Ca intake between the groups (t 21 = 1·949, P = 0·065). The reference intakes for these nutrients are 700 mg Ca and 200 μg folate(33). In both breakfast and no-breakfast conditions, Ca and folate intakes for male participants were not significantly lower than the reference intakes (breakfast: 979 and 814 mg; no-breakfast: 257 and 209 μg, respectively). For female participants as well, Ca intake was not significantly lower than the reference value in either condition (breakfast: t 21 = 1·110, P = 0·280; no-breakfast: t 21 = 1·380, P = 0·182). However, folate intake for female participants in the no-breakfast condition was significantly lower than the reference value (t 21 = 3·769, P < 0·001).
Discussion
In the present study, physical activity was assessed using heart rate monitors and pedometers; these measures did not provide any experimental evidence of a difference in physical activity levels between days when breakfast was consumed and not consumed. Although the mean heart rate in the morning was significantly higher in participants on days when they had consumed breakfast, the average increase was only 5 bpm, which can be accounted for by the thermic effect of food(Reference Yi, Fullwood and Stainer34).
Studies comparing the daily energy intakes of breakfast eaters and non-breakfast eaters have revealed conflicting results. Some authors(Reference Ruxton and Kirk19, Reference Song, Chun and Obayashi35) have reported no differences in the amount of energy consumed; the findings of the present study support this conclusion since there were no significant differences in daily energy intakes between the breakfast and no-breakfast conditions. Generally, when breakfast was not eaten, participants consumed more energy during the remainder of the day in sufficient quantity to compensate for the morning fast. Similar compensatory behaviour has been reported previously(Reference Hubert, King and Blundell15). In contrast, certain other studies have shown that breakfast consumption leads to the ingestion of more energy than when skipped(Reference Timlin, Pereira and Story20, Reference Martin, Normand and Sothier36), and that reducing the amount of energy consumed at breakfast can lower total daily energy intakes(Reference Schusdziarra, Hausmann and Wittke37). In the present study, one group of participants fits this pattern; male participants who infrequently consumed breakfast consumed more energy per 24 h during the study period when they consumed breakfast. A plot of the hourly distribution of energy intake per 24 h for this group suggests that they ate more during the evening meal on days when they consumed breakfast, perhaps because they had not eaten a particularly large lunch because of having eaten breakfast (Fig. 3). It has been reported that people are less able to compensate for an energy surplus than they are for an energy deficit(Reference Levitsky38); this may explain to a certain extent why the male low-frequency breakfast eaters in the present study consumed greater amounts when provided with breakfast. The differences in compensatory behaviour observed in the male infrequent breakfast eaters compared with the other groups suggest that routine and habitual eating habits may modify how participants respond to the addition or omission of breakfast.
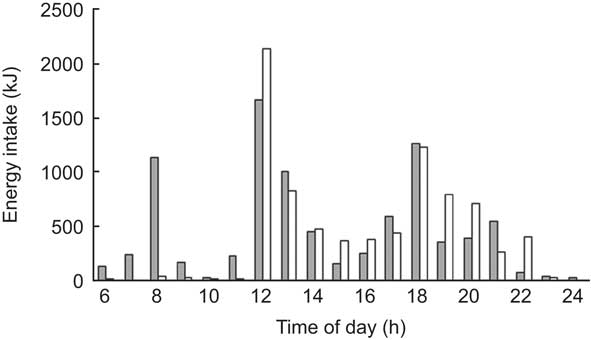
Fig. 3 Hourly distribution of energy intake per 24 h during the breakfast (![]() ) and no-breakfast (
) and no-breakfast (![]() ) conditions for male participants who typically eat breakfast <5 times/week
) conditions for male participants who typically eat breakfast <5 times/week
In terms of the timing of meals, some groups within the present study exhibited variation in their post-noon eating habits in response to whether or not breakfast was consumed. The literature also reports such responsive variations in changes in eating habits. For example, in the first experiment reported by Levitsky(Reference Levitsky39), there was no difference in the amounts consumed at lunch when breakfast was omitted, whereas in the second experiment the participants consumed greater amounts at lunch. This difference was believed to be a result of a greater quantity of breakfast being provided in the latter experiment. In the present study there was no difference in the energy intake-time index between the two experimental conditions for male infrequent breakfast eaters, suggesting that in addition to not changing their energy intake from noon onwards they also did not change their timing of meals. Moreover, the energy intake-time index did not differ for male high-frequency breakfast eaters, which is interesting given that they consumed more energy post noon on days when breakfast was not eaten. An hourly distribution of energy intake for this group (Fig. 4) suggests that they tended to eat a greater proportion of their post-noon food earlier in the day when breakfast was not eaten, probably because of heightened hunger levels around lunch time(Reference Hubert, King and Blundell15, Reference Levitsky38). In contrast, when breakfast was not eaten, the energy intake-time index indicated that female participants who were habitual breakfast eaters tended not only to eat more but also to move their eating to later in the day. However, similar to the male participants, the energy intake-time index was independent of experimental condition in female participants who did not habitually eat breakfast frequently, the explanation most likely being the same as that for the male frequent breakfast eaters, which is that heightened lunchtime hunger during the no-breakfast condition resulted in a large food intake at this time of the day. Female participants who habitually consumed breakfast frequently may have eaten more and later in the day during the no-breakfast condition either to make up for the energy deficit in the morning and/or in anticipation of a future deficit that they are not accustomed to, that is, not eating during the subsequent day until at least noon. It has been shown that, compared with male participants, the food intakes of female participants are more likely to be influenced by cognitive and environmental factors(Reference Davy, Van Walleghen and Orr40). Although it should be noted that stronger effects are typically observed in experimental situations compared with free-living surveys(Reference Martin, Normand and Sothier36), this psychological difference between male and female participants could account for the different responses between the female high-frequency breakfast eaters and the male participants. Differences between the female high- and low-frequency breakfast eaters may be linked to differences in routine-driven eating habits and/or to dietary restraint between regular and irregular breakfast eaters(Reference Nakade, Takeuchi and Kurotani27, Reference Schlundt, Hill and Sbrocco41).
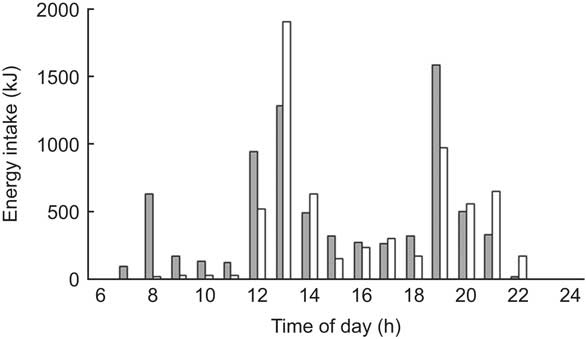
Fig. 4 Hourly distribution of energy intake per 24 h during the breakfast (![]() ) and no-breakfast (
) and no-breakfast (![]() ) conditions for male participants who typically eat breakfast at least 5 times/week
) conditions for male participants who typically eat breakfast at least 5 times/week
The daily amount of folate consumed by male and female participants and the amount of Ca consumed by female participants were lower on days when breakfast was not consumed. Female participants consumed significantly less folate than the recommended nutrient intake on days when they did not eat breakfast, highlighting the important contribution that breakfast makes to folate and Ca intakes. Similarly, in a study focusing on cereal consumption in children of both genders, Barton et al.(Reference Barton, Eldridge and Thompson42) found lower intakes of Ca, folate and also fibre by children who did not consume breakfast. In the present study, clearly the greater intakes of folate and Ca during the breakfast condition were due to RTEBC provided since they are typically fortified with folic acid and their consumption facilitates milk and hence Ca intakes(Reference Song, Chun and Kerver17). Williamson(Reference Williamson43) comments that RTEBC may be important for certain population groups, particularly for women of child-bearing age, because when consumed with milk they can provide protein, riboflavin, Ca, Zn, folic acid, Fe and fibre. The consumption of wholegrain cereals at breakfast may also affect insulin sensitivity since high-fibre foods can blunt postprandial glucose and insulin responses(Reference Clark, Gardiner and McBurney44), reducing between-meal hypoglycaemia(Reference Timlin and Pereira45), which may also affect hunger levels later in the day and even have a role in weight maintenance.
Many authors have suggested that the link between consumption of breakfast and lower BMI is due to confounding lifestyle factors(Reference De la Hunty and Ashwell46) and that breakfast is merely a behavioural marker for appropriate dietary and physical activity patterns. However, they have been unable to separate this from any metabolic effect that breakfast consumption may have(Reference Ruxton and Kirk19, Reference Cohen, Evers and Manske25, Reference Huang, Hu and Fan47). The present study does not refute the suggestion that breakfast may be a marker of a healthy lifestyle since energy expenditure, activity levels and eating habits were primarily found to be independent of breakfast consumption. However, although recognising the limitations of collecting dietary information through self-reported 3 d food diaries(Reference Andersen, Pollestad and Jacobs48, Reference Margetts and Nelson49), some interesting differences in responses to imposed breakfast regimes, both between genders and between habitual breakfast eaters and habitual non-breakfast eaters, have been uncovered. Male participants who did not habitually eat breakfast in fact consumed more energy per day when consuming a morning meal, whereas female participants who habitually ate breakfast tended to eat more and later in the day when not consuming a morning meal. Thus, the effect that breakfast consumption has on energy intake and eating behaviour may vary depending on gender and morning eating habits; hence, aside from the mechanisms that link BMI and the behaviour of consuming breakfast, the relationship between these two factors could be different for different groups. Perhaps, most importantly, groups that do not reduce energy intake during the remainder of the day when breakfast is consumed may exhibit an increase in BMI over time, although further studies are required to ascertain whether such non-compensatory behaviour continues in the long term. The present experimental study also suggests tentatively that morningness relates to the frequency of consuming breakfast. Future work should investigate what behavioural, physiological or psychological factors are associated with a preference for eating or not eating breakfast (such as eating habits, morning glucose levels and morningness) and whether these factors are affected by changes in eating habits.
Acknowledgements
The present study was funded by Roehampton University. The authors have no conflict of interest to declare. L.G.H. and J.W.H. designed the original study; L.G.H., J.W.H. and S.R. carried out data collection, performed statistical analyses and wrote the manuscript; T.L., C.I. and P.W. collected and compiled the data. All authors critically reviewed the manuscript and approved the final version submitted for publication. The authors thank Roehampton University for funding the present study. The authors also thank Peter Shaw for discussions on study design and Caroline Ross for her thoughts on testing for morningness, as well as Crispin Jenkinson for providing normative SF-36v2 data.