Despite the decrease in classical cardiovascular risk factors as well as in cardiovascular morbidity and mortality in recent decades, the prevalence of type 2 diabetes has continued to increase in Finland. In 2008, over half a million Finnish people were estimated to have type 2 diabetes, half of them not yet aware that they have the disease(Reference Puska, Peltonen and Reunanen1). The largest relative increase in drug-treated type 2 diabetes over the 12-year period from 1994 to 2006 was seen in the youngest age groups: among 15–29-year-olds the increase in prevalence was 9·5-fold, among 30–44-year-olds 3·3-fold, among 45–74-year-olds 85 % and among those over 75 years the increase was 48 %(Reference Reunanen, Virta and Klaukka2). A study completed in young adults (aged 15–39 years) utilising several data sources revealed alarming results: although absolute incidence, and thus also the prevalence of type 2 diabetes among young adults was still low between 1992 and 1996 (11·8 cases per 100 000/year) the incidence increased on average by 7·9 % per year(Reference Lammi, Taskinen and Moltchanova3).
The most important lifestyle-related risk factors for type 2 diabetes are (abdominal) obesity, a sedentary lifestyle and a dietary pattern with high saturated fat, refined carbohydrate and total energy and low fibre content(Reference Hu, Lindström and Valle4–Reference Montonen, Knekt and Järvinen7). Beneficial changes in dietary composition, especially related to the intake of total and saturated fat, have occurred in Finland during the past decades. On the other hand, the increasing trend in the prevalence of obesity has persisted, indicating that in general, energy expenditure on physical activity has decreased more than dietary energy intake. In 2007, in total 70 % of men and 57 % of women were overweight or obese(Reference Vartiainen, Peltonen and Laatikainen8).
Type 2 diabetes is a serious illness complicated by micro- and macro-vascular diseases such as, renal failure, retinopathy, CVD and lower limb amputations(Reference Gerstein9). Diabetes without any prior evidence of coronary heart disease indicates a comparable or higher myocardial infarction and mortality risk than prior coronary heart disease in non-diabetic subjects, especially in women(Reference Juutilainen, Lehto and Rönnemaa10–Reference Hu, Jousilahti and Qiao12). Furthermore, the risk of cardiovascular complications has been shown to increase linearly by increasing blood glucose across the intermediate stage (impaired glucose tolerance (IGT)) between ‘normal’ and ‘diabetic’ glucose values(13). Therefore, the main justification for activities, which prevent type 2 diabetes is the assumed concurrent prevention of complications related to diabetes.
Prevention of type 2 diabetes: clinical evidence
The Finnish diabetes prevention study
The very first controlled, individually randomised trial to test the possibility of type 2 diabetes prevention by lifestyle intervention to be carried out in the world was the Finnish diabetes prevention study (DPS)(Reference Tuomilehto, Lindström and Eriksson14). The DPS is a multi-centre study started in 1993, coordinated by the National Public Health Institute (at present, National Institute for Health and Welfare), and completed in five centres (Helsinki, Kuopio, Turku, Tampere and Oulu) in Finland. Altogether 522 middle-aged, overweight men and women with high type 2 diabetes risk (defined as IGT detected during two consecutive 75 g oral glucose tolerance tests) were recruited and randomly allocated into a ‘standard care’ control group or intensive lifestyle intervention group(Reference Lindström, Louheranta and Mannelin15, Reference Eriksson, Lindström and Valle16).
The lifestyle intervention was delivered primarily by study nutritionists through individual counselling sessions, and highlighted by study physicians at annual clinical visits(Reference Lindström, Louheranta and Mannelin15). The intervention goals were to reduce body weight (5 % or greater reduction from baseline weight), limit dietary fat (<30 % of total energy consumed) and saturated fat (<10 % of total energy consumed), and to increase both dietary fibre intake (≥15 g/4184 kJ (1000 kcal)) and physical activity (≥30 min/d). The participants had face-to-face consultation sessions, each lasting for 30 min/h; altogether seven sessions during the first year and sessions every 3 months thereafter. The first year sessions had a pre-planned topic (e.g. what are diabetes risk factors, how to reduce saturated fat, how to increase dietary fibre, how to increase physical activity), but the discussions were individualised, focusing on specific individual problems and needs. Printed material was used to illustrate the message and to serve as a reminder at home. In addition, there were some voluntary group sessions, expert lectures, low-fat cooking lessons, visits to local supermarkets, between-visit phone calls and letters. The goal was to build and strengthen motivation, to equip the subjects with necessary knowledge and skills, and thereby to achieve gradual, permanent behavioural changes. The dietary advice was based on 3 d food records, which were completed by the intervention participants four times yearly. The participants were encouraged to make intermediate goals for themselves by thinking about practical things they would try to change (e.g. instead of an abstract goal ‘increase fibre intake’ a practical goal would be ‘eat a slice of rye bread during every meal’). The spouse was invited to join the sessions, especially if she/he was the one responsible for shopping and cooking in the family. Furthermore, the participants were individually guided to increase their overall level of physical activity. Endurance exercise was recommended to increase aerobic capacity and cardiorespiratory fitness. Supervised, progressive, individually tailored circuit-type moderate intensity resistance training sessions to improve the functional capacity and strength of the large muscle groups of the upper and lower body were also offered free-of-charge. In addition, voluntary group walking and hiking were organised in some centres.
The intervention group showed significantly greater improvement in each intervention goal. After 1 and 3 years, mean weight reductions were, respectively, 4·5 and 3·5 kg in the intervention group, and 1·0 and 0·9 kg in the control group. Cardiovascular risk factors improved more in the intervention group(Reference Lindström, Louheranta and Mannelin15, Reference Ilanne-Parikka, Eriksson and Lindström17). After a mean follow-up of 3·2 years, the risk of diabetes was reduced by 58 % in the intervention group compared with the control group(Reference Tuomilehto, Lindström and Eriksson14). The reduction in the incidence of diabetes was directly associated with the number of achieved lifestyle goals: among those who achieved four or all five of the pre-defined goals at year 1, there were no diabetes cases diagnosed during the whole intervention period. Increasing physical activity was shown to be an independent predictor of diabetes risk reduction(Reference Laaksonen, Lindström and Lakka18). Furthermore, those who consumed a moderate fat, high-fibre diet achieved the largest weight reduction and, even after adjustment for weight reduction, had the lowest diabetes risk during the intervention period(Reference Lindström, Peltonen and Eriksson19). After discontinuation of the counselling, the differences in lifestyle variables between the groups still remained favourable in the intervention group. During the post-intervention follow-up period of 3 years, the risk of diabetes was still 36 % lower among the former intervention group participants, compared with the former control group participants(Reference Lindström, Ilanne-Parikka and Peltonen20). The effect was seen in both men and women (Fig. 1).

Fig. 1 Type 2 diabetes incidence by gender and treatment group during the extended follow-up of the Finnish diabetes prevention study (DPS) participants with impaired glucose tolerance at baseline (![]() , control;
, control; ![]() , intervention)
, intervention)
After the DPS, several clinical studies have confirmed the finding, most importantly the US diabetes prevention programme. In 2002, it reported exactly the same risk reduction of 58 %(21). It has also reported that lifestyle intervention is both more effective and cost-efficient than prevention using glucose lowering medication(Reference Herman, Hoerger and Brandle22).
Practical implementation of prevention
The implementation project for the prevention of type 2 diabetes in Finland – the FIN-D2D
Finland was one of the first countries in the world to set up a national programme for the prevention and better care of patients with type 2 diabetes, called DEHKO(23). Related to one of the three aims of DEHKO, the programme for the prevention of type 2 diabetes in Finland was launched in 2003 to deal with the emerging diabetes epidemic. The programme comprises three concurrent strategies: (i) the population strategy covering the general population; (ii) the high-risk strategy that is based on individual-orientated measures targeted at those at particularly high risk of developing type 2 diabetes; and (iii) the strategy of early diagnosis and management of type 2 diabetes. As a part of the nationwide promotion of these programme components, an implementation project, FIN-D2D, was carried out in five of the twenty-one hospital districts in Finland during 2003–2007(24). The project was carried out as collaboration between the hospital districts, the Finnish Diabetes Association and the National Public Health Institute. The role of the National Public Health Institute was to provide expertise on primary prevention of type 2 diabetes, and to evaluate the effectiveness of the project. The main objective of the implementation project was to organise and develop prevention models that would be feasible within the regular primary and occupational health-care system. These prevention models are largely based on findings and experiences from the DPS study. The principal screening tool to identify individuals with high type 2 diabetes risk was the Finnish diabetes risk score (FINDRISC)(Reference Lindström and Tuomilehto25) that was developed in the National Public Health Institute based on follow-up data from large population-based cohorts (Fig. 2). High-risk individuals underwent an oral glucose tolerance test and were referred to lifestyle interventions, delivered mostly by public health nurses in collaboration with local multi-professional teams. The nurses were trained to use the stages of change approach(Reference Prochaska, DiClemente and Norcross26) to motivate and instruct the participants to make beneficial changes in their lifestyles. Weight management and physical activity were the basis for prevention. As the resources in the primary health-care are scarce, the advised strategy was group intervention; individual and self-acting interventions could also be used.
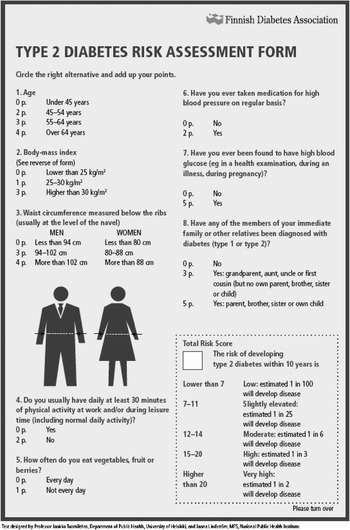
Fig. 2 The Finnish diabetes risk score (FINDRISC)
The implementation project proved that large-scale screening was possible; 10 000 high-risk individuals and 10 000 moderate-risk individuals were identified(Reference Saaristo, Oksa and Peltonen27). In both of these cohorts, the proportion of men was less than that of women. According to preliminary results after 1-year follow-up, there were desirable changes in CVD risk factors and glucose tolerance in the high-risk cohort in both sexes. In the high-risk women, a modest but statistically significant weight loss was achieved and associated with a decrease in the incidence of diabetes, verified by drug-reimbursement register data. Most importantly, the project showed that implementing effective large-scale lifestyle interventions in primary health-care is possible. However, certain problems and challenges were encountered, especially in relation to the limited resources allotted to preventive health-care. Furthermore, even though group intervention was initially considered to be cost-saving compared with individual intervention, and was therefore recommended as the principal mode of intervention, it proved unappealing to the patients, especially to men.
Screening and prevention of type 2 diabetes in an airline company – FINNAIR
Another example of implementation of type 2 diabetes prevention in primary health-care is the FINNAIR Project that is being undertaken in collaboration with Finnair Health Services, the National Institute for Health and Welfare (formerly the National Public Health Institute), and the Institute for Occupational Health. In the Finnair Airline Company, shift work adds to the conventional risk factors for type 2 diabetes. The aims of the project were to renew Finnair occupational health services’ health check-up process to cover evaluation of lifestyle-related risk factors among the Finnair workforce, to assess the prevalence of glucose metabolism disorders among employees with varying working hours, and to clarify whether experiences of intervention trials could be implemented in the preventive work practiced in occupational health services in a cost-effective manner. The role of the National Institute for Health and Welfare is to act as a consultant in planning and developing screening and intervention activities, to participate in intervention delivery and to conduct the evaluation of the project.
During the years 2006–2008 one-fifth of the Finnair employees were called on each year for a health examination. The examination included physical examinations, laboratory tests and questionnaires on working hours, sleeping habits, lifestyle and dietary factors as well as counselling by an occupational health nurse or physician. The FINDRISC(Reference Lindström and Tuomilehto25) diabetes risk score (Fig. 2), fasting blood glucose and/or glucose tolerance test were used to classify the participants as having a low, increased or high risk of type 2 diabetes. Those with an increased or high diabetes risk were referred to a diabetes nurse or a nutritionist for counselling. Possibly due to shift work employees were not able or willing to participate in small group sessions that were offered and therefore individual counselling (one to two sessions) was the primary intervention delivery method.
The renewed health check-up process proved to be effective in identifying workers with an increased type 2 diabetes risk. The follow-up health survey, which will be completed after 3 years (starting in 2009), will give information on the effectiveness of the lifestyle counselling with regard to diabetes and cardiovascular risk factors.
Good ageing in Lahti region programme for good aging – building a regional model for preventing type 2 diabetes
Implementation of effective lifestyle interventions in routine health-care poses a very big challenge(Reference Glasgow, Lichtenstein and Marcus28). In the published efficacy trials, the lifestyle interventions have all lasted for several years(Reference Tuomilehto, Lindström and Eriksson14, Reference Lindström, Ilanne-Parikka and Peltonen20, 21, Reference Kosaka, Noda and Kuzuya29, Reference Ramachandran, Snehalatha and Mary30), and e.g. in the DPS, the counselling was delivered by highly skilled experts with a median of twenty sessions during a 4-year intervention(Reference Lindström, Ilanne-Parikka and Peltonen20). A crucial question is whether the results obtained in the efficacy trials can be replicated in routine health-care, which has much more limited resources available for delivery.
At the time when the results from the DPS were published, the municipalities and regional and local health-care organisations in the Päijät-Häme Province in Southern Finland had set out a health promotion programme, the GOAL Programme, together with the National Public Health Institute, the UKK Institute for Health Promotion, the Lahti University of Applied Sciences and the University of Helsinki. Within the GOAL Programme framework, a lifestyle implementation trial(Reference Uutela, Absetz and Nissinen31, Reference Fogelholm, Valve and Absetz32) was designed for the primary health-care setting with lifestyle objectives derived from the DPS(Reference Tuomilehto, Lindström and Eriksson14).
The lifestyle implementation trial differed from the other Finnish implementation trials in that in addition to the evidence-base from efficacy trials, it was also strongly based on health behavioural change theories(Reference Schwarzer and Fuchs33). Programme components especially targeted self-efficacy and self-regulation in changing diet and physical activity, using information provision, group discussions, self-monitoring of behaviour and goal setting and planning.
In Finland, routine preventive health services including risk factor control measures and health education are typically delivered by public health nurses. The GOAL intervention was also delivered by these professionals. Depending on each centre’s resources, the nurses facilitated groups either independently or together with another nurse or a physiotherapist. Facilitators received 2 d of training with a standardised training programme, training manuals and practical exercises. A project dietician supported facilitators throughout the project and also gave dietary counselling during one group session. In another session, municipal sports and recreation officers introduced the groups to local sports facilities and guided exercise training (e.g. gym, aquatic exercise, nordic walking). The programme extended over a time period of 8 months, with the first five sessions held at 2-week intervals and one booster session after a 6-month break. The protocol included no other contacts with the participants after the programme delivery except for those involved with measurements at 1 and 3 years, including clinical risk factors, nutrition and physical activity and psychosocial determinants. More detailed descriptions of the programme can be found in our previous papers(Reference Uutela, Absetz and Nissinen31, Reference Absetz, Valve and Oldenburg34) and at http://www.palmenia.helsinki.fi/ikihyva/InEnglish.html.
Among the 352 participants in the GOAL lifestyle implementation trial, the average FINDRISC(Reference Lindström and Tuomilehto25) score was 16·2 (sd 3·3) and baseline BMI was 32·6 (sd 5·0) kg/m2 . Using the DPS results as a benchmark for 1-year results, nutritional objectives were well attained, but physical activity and weight loss results were more modest(Reference Absetz, Valve and Oldenburg34). The average mean weight loss of −0·8 (sd 4·5) kg at 1-year follow-up was statistically significant (P = 0·002) and maintained also at the 3-year follow-up (−1·0 (sd 5·6) kg, P = 0·003)(Reference Absetz, Oldenburg and Hankonen35).
In Päijät-Häme, the results and experiences of the GOAL lifestyle implementation trial were found encouraging and measures were taken to sustain the programme and integrate it into routine practice at the regional level. The programme provided a feasible tool for counselling, but also pointed out a need for a systematised, multi-professional process for prevention. Within the GOAL Programme, a regional working group VALTIT was established to develop preventive processes using National Current Care Guidelines on adult obesity, hypertension, dyslipideamia and smoking cessation as the starting point. The processes were locally tested in an implementation trial during the years 2004–2007(Reference Kuronen, Jallinoja and Airola36). Subsequently, a regional process for preventing CVD including identification of patients at risk, a system of counselling for all those at risk with a task-oriented group approach as the default method, and appropriate follow-up and evaluation, was integrated into the routine processes of the region’s primary health-care organisations from the beginning of the year 2008. Furthermore, infrastructure has been built to support the application of this process including modifications of the electronic patient database for registration of, e.g. lifestyle data, updated versions of risk screening measures and tools for lifestyle counselling as well as training for group facilitators(Reference Absetz and Patja37).
Discussion
The current situation with regard to type 2 diabetes can well be compared with the epidemic of coronary heart disease in the 1960s in Finland. Primary prevention measures at the population level targeted to control the known modifiable risk factors of coronary heart disease have been shown to be very successful(Reference Vartiainen, Korhonen and Pietinen38). For type 2 diabetes, the effects of lifestyle intervention to prevent type 2 diabetes in high-risk individuals have been firmly demonstrated in clinical trials. Furthermore, the extension of the DPS study demonstrated that lifestyle intervention lasting for a limited duration can lead to sustained lifestyle change and prevention of the development of diabetes also in the long term(Reference Lindström, Ilanne-Parikka and Peltonen20). These experiences indicate that there is great potential in using lifestyle intervention to reduce the burden of type 2 diabetes among high-risk individuals.
However, there are still some unanswered questions concerning the prevention of type 2 diabetes by lifestyle intervention. First, it is not clear whether the prevention of diabetes also prevents diabetes-related comorbidities, i.e. CVD. The recent results from the DPS trial reveal that even though risk of diabetes was significantly reduced by lifestyle intervention(Reference Lindström, Ilanne-Parikka and Peltonen20) and total mortality and cardiovascular morbidity were significantly lower compared with a population-based high-risk cohort with IGT at baseline, there was no difference in cardiovascular morbidity between the intensive intervention and control groups(Reference Uusitupa, Peltonen and Lindström39). Second, although the implementation trials described above have been reasonably successful, we still need to learn more about the implementation of effective diabetes prevention programmes in different settings, cultures, regions and age groups. Furthermore, not only the feasibility and the effects but also the cost-effectiveness of the applied intervention strategies needs to be assessed. At the moment, some evidence suggests that the preventive effect of lifestyle interventions achieved in a clinical trial setting is, in general, attenuated when prevention is pursued within health-care settings with less selected patient groups.
The currently available evidence strongly indicates that prevention of type 2 diabetes among high-risk individuals is effective. On the basis of clinical trials, the risk reduction is clearly associated with the magnitude of achieved lifestyle changes. However, it is clear that the diabetes epidemic cannot be solved by concentrating on high-risk strategies and preventive actions carried out by the health-care system. Primary prevention programmes targeting the population as a whole need to be developed and implemented. In particular, the importance of co-operation and of a multi-sectorial approach should be emphasised. Citizens’ awareness of the importance of a healthy lifestyle has to be increased, and there is a need to address social inequalities in diet, physical activity and obesity. We have to work together with the educational system, food industry, media, urban planning and non-governmental organisations to make healthy lifestyle choices available, affordable and enjoyable.




