Maternal characteristics such as education, health and nutrition knowledge, empowerment, and physical and mental health are critical resources for child survival, growth and development( 1 ). The recent Lancet series on maternal and child undernutrition highlighted maternal depression as a significant risk factor for poor child growth and recommended interventions to address the problem through maternal and child health and nutrition programmes( Reference Bhutta, Ahmed and Black 2 ). Maternal behaviours and practices are important elements for translating resources for care, such as household food security and health-care resources, into child well-being( Reference Engle and Lhotska 3 , 4 ). Impaired mental health reduces a mother's ability to take adequate care of her child, which in turn can have negative effects on the child's growth and development( Reference Stewart 5 – Reference Walker, Wachs and Gardner 7 ). Alternatively, the presence of a sick or poorly growing child could undermine a mother's well-being, thereby increasing her vulnerability to depressive symptoms due to the worry and stress of the additional effort required to take care of her child and the pressure of disappointment or even overt criticism expressed by family members or others( Reference Stewart 5 ).
Poor maternal mental health has been shown to be associated with suboptimal breast-feeding and complementary feeding practices( Reference Patel, Wheatcroft and Park 8 ), compromised parenting behaviours, reduced mother–child interactions and a higher prevalence of medical and emotional problems among children. Studies in India, Bangladesh and Pakistan demonstrated consistent associations between maternal common mental disorders (CMD) and child undernutrition( Reference Patel, DeSouza and Rodrigues 9 – Reference Rahman, Lovel and Bunn 11 ). Results from cross-country studies indicated that in India and Vietnam, mothers with CMD had higher likelihood of having a stunted and underweight child, respectively, compared with mothers who did not suffer from CMD. In Peru and Ethiopia, however, these associations were not statistically significant( Reference Harpham, Huttly and De Silva 12 ). Studies in Latin America and Africa also revealed mixed results. Maternal mental health was associated with child nutrition in Brazil( Reference Surkan, Kawachi and Ryan 13 , Reference Santos, Santos and de Cassia Ribeiro Silva 14 ) and Malawi( Reference Stewart, Umar and Kauye 15 ), but not in South Africa( Reference Tomlinson, Cooper and Stein 16 ) and Ethiopia( Reference Medhin, Hanlon and Dewey 17 ). A recent meta-analysis of seventeen studies in eleven countries also provided evidence of the association between maternal depression and early childhood underweight and stunting in both cross-sectional and longitudinal studies( Reference Surkan, Kennedy and Hurley 18 ).
Few studies have examined the association between maternal mental health and child illnesses. In a cohort study in Pakistan, pre- and postnatal depression were found to increase the risk of having diarrhoea in infants( Reference Rahman, Iqbal and Bunn 19 , Reference Rahman, Bunn and Lovel 20 ). Results from a case study in Nigeria also showed that infants of depressed mothers were more likely to have episodes of diarrhoea and other infectious illnesses( Reference Adewuya, Ola and Aloba 21 ). In a recent study in Ethiopia, infants of mothers with persistent perinatal CMD symptoms were at more than double the risk of having diarrhoea. However, such associations were not observed between perinatal CMD symptoms and fever or acute respiratory infection (ARI)( Reference Ross, Hanlon and Medhin 22 ).
In the present study, we examined the associations of maternal CMD with child undernutrition and illnesses in Bangladesh, Vietnam and Ethiopia. We proposed that maternal CMD would be associated with greater levels of undernutrition and common illnesses in children. Use of the same measurement tools and analytical techniques was useful to demonstrate the associations of maternal CMD with child undernutrition and illnesses across the three countries.
Materials and methods
Data source and study population
We used data from the baseline household survey of Alive & Thrive (A&T), which is an initiative funded by the Bill & Melinda Gates Foundation to reduce undernutrition and death caused by suboptimal infant and young child feeding (IYCF) practices in Bangladesh, Vietnam and Ethiopia over a period of six years (2008–2014). The Vietnam baseline survey covered 4029 households in forty communes in four provinces where the A&T project is being implemented( Reference Nguyen, Manohar and Mai 23 ). The Bangladesh baseline survey covered 4400 households in twenty selected upazilas (sub-districts)( Reference Saha, Bamezai and Khaled 24 ). The baseline survey in Ethiopia included a total of 3000 households from seventy-five enumeration areas( Reference Ali, Tedla and Subandoro 25 ). All households with children aged 0–5 years and their mothers were included in the survey. There were no exclusion criteria except for those who refused to participate (refusal was minimal across the three countries). All three surveys received ethical approval from the Institutional Review Board of the designated countries and from the International Food Policy Research Institute.
Anthropometry
The first outcome in the present study was child undernutrition – stunting, underweight and wasting. Weight and height/length measurements were taken by trained fieldworkers using recommended protocols( Reference Cogill 26 ). Weight of children and mothers was measured using electronic scales accurate to 100 g. Locally manufactured length/height boards, which were precise to 1 mm, were used to measure the recumbent length of children aged 0–24 months and the standing height of children aged ≥24 months and of mothers.
Children's weight and length/height measurements were used to derive Z-scores by comparing each child's anthropometric measurements with the WHO child growth standards for his/her age and gender( 27 ). Three indicators were calculated using child's weight and length/height: length/height-for-age Z-score (HAZ), weight-for-age Z-score (WAZ) and weight-for-length/height Z-score (WHZ). Stunting was defined as HAZ <−2, underweight as WAZ <−2 and wasting as WHZ <−2( 27 ). Maternal weight and height were used to calculate BMI (kg/m2). Maternal undernutrition was defined as BMI <18·5 kg/m2.
Child illness
The second outcome was child illness, which was measured through maternal recall of symptoms of diarrhoea and upper ARI in the two weeks prior to the survey. Diarrhoea was defined as three or more loose stools passed in a 24-h period( 28 ) and ARI was defined as the presence of cough/cold with fever and/or fast breathing( 29 ).
Maternal common mental disorders
Maternal CMD was measured using the WHO-recommended screening tool called the Self-Reporting Questionnaire-20 (SRQ-20) that includes twenty questions with a recall period of 30 d prior to the administration of the questionnaire( 30 ). The SRQ-20 measures several symptoms of depression, including headache, poor appetite, sleep disturbance, depressed mood, unhappiness, helplessness and psychomotor retardation. Each question is given a score of 0 or 1 depending on the ‘no’ or ‘yes’ response, respectively. The scores are added to generate an overall SRQ-20 scale, where higher scores indicate higher levels of maternal CMD and vice versa. This tool has been found to be reliable, valid and adaptable for screening mental disorders in the developing world( 30 ) including Ethiopia( Reference Hanlon, Medhin and Alem 31 ) and Vietnam( Reference Giang, Allebeck and Kullgren 32 ). We used a cut-off of 7 to classify women with low or high level of CMD, as suggested by several validation studies( Reference Hanlon, Medhin and Alem 31 , Reference Giang, Allebeck and Kullgren 32 ).
Socio-economic status index
The socio-economic status (SES) index was constructed using principal components analysis. Variables that were included in the SES index were ownership of house and land, housing quality (e.g. house construction materials), access to services (water, electricity, gas and sanitation services) and household assets (different types of durable goods, productive assets, animals and livestock)( Reference Vyas and Kumaranayake 33 , Reference Gwatkin, Rutstein and Johnson 34 ). Factor scores derived from the first factor (which explained 47 %, 33 % and 39 % of the variance for Bangladesh, Vietnam and Ethiopia, respectively) were then used to characterize the SES of each household. Households were categorized into SES quintiles based on their individual SES index score.
Household food security
Household food security was measured using the Household Food Insecurity Access Scale( Reference Coates, Swindale and Bilinsky 35 ) of the Food and Nutrition Technical Assistance Project/US Agency for International Development, which provides information on behaviour and perceptions related to household food insecurity – anxiety and uncertainty, insufficient quality of intake, insufficient food intake and its consequences. All the questions were asked for a reference period of 30 d preceding the survey. The households were categorized into four groups: food secure, mildly food insecure, moderately food insecure and severely food insecure( Reference Coates, Swindale and Bilinsky 35 ). These categories were then collapsed into two groups of households: food secure and food insecure (which included the mildly, moderately and severely food-insecure groups).
Infant and young child feeding practices
IYCF practice indicators were described using the WHO recommendation( Reference Daelmans, Dewey and Arimond 36 , 37 ). The six core IYCF indicators used in the present analysis were: (i) early initiation of breast-feeding (the proportion of children born in the last 24 months who were put to the breast within 1 h of birth); (ii) exclusive breast-feeding (the proportion of infants 0–5 months of age who are fed exclusively with breast milk); (iii) minimum dietary diversity (the proportion of children 6–23 months of age who receive foods from four or more food groups); (iv) minimum meal frequency (the proportion of breast-fed and non-breast-fed children 6–23 months of age who receive solid/semi-solid food, the minimum number of times or more); (v) minimum acceptable diet (the proportion of children 6–23 months of age who receive at least the minimum dietary diversity and the minimum meal frequency, apart from breast milk); and (vi) consumption of Fe-rich foods (the proportion of children 6–23 months of age who received an Fe-rich food or a food that was fortified with Fe).
Other variables
We collected information on the child's birth weight. Low birth weight was defined as birth weight <2500 g for Vietnam, and mother's perception that the child was very small or smaller than average for Bangladesh and Ethiopia. In addition, mother's and child's cleanliness was assessed based on a hygiene spot check( Reference Ruel and Arimond 38 ) of the general appearance of the face, hands, hair and body/clothes. Each question was given a score of 0 or 1 depending on the ‘dirty’ or ‘clean’ observation, respectively. The scores were added to generate an overall hygiene scale (range: 0–4), where higher scores indicated higher levels of cleanliness. Women's education was measured as the years of schooling completed. As women's education levels varied across the three countries, different cut-offs were used for maternal education based on their suitability to the country's context. Whereas ‘primary education’ was used as the reference group in Vietnam, ‘no schooling’ was the reference group for Bangladesh and Ethiopia.
Statistical analysis
Descriptive analyses were used to report background characteristics of the study sample. Bivariate analysis was done to examine the association of maternal CMD with child undernutrition and child illness, and also with maternal and household characteristics, child feeding practices, hygiene and health-seeking behaviours, using the t test for continuous variables and the χ 2 test for categorical variables. Logistic regression models were used to examine the relationship of maternal CMD with child undernutrition and child illness, adjusting for several potential confounding factors at child (age, gender, low birth weight), maternal (age, height, BMI, education, mother as household head) and household levels (SES, food security). These models were also adjusted for mother's and child's cleanliness. The ‘cluster’ command in Stata was used to adjust for clustering effects at the sub-district level in Bangladesh, communes in Vietnam and region in Ethiopia. All statistical analyses were carried out using the statistical software package Stata version 11.
Results
Sample characteristics
Characteristics of the study population in Bangladesh, Vietnam and Ethiopia are presented in Table 1. Levels of undernutrition were high across the three countries. The prevalence of stunting was highest in Ethiopia (44 %) followed by Bangladesh (40 %) and Vietnam (17 %). Rates of underweight and wasting were highest in Bangladesh followed by Ethiopia and Vietnam (39 %, 24 % and 13 % for underweight and 18 %, 7 % and 5 % for wasting, respectively). A large number of children had symptoms of upper ARI during the previous two weeks (33 % in Bangladesh, 16 % in Vietnam and 20 % in Ethiopia). The prevalence of diarrhoea in Bangladesh (8 %) was lower than in the other two countries (9 % in Vietnam and 16 % in Ethiopia). Maternal CMD was high in all three countries, affecting nearly half of women in Bangladesh, 39 % of women in Ethiopia and 31 % of women in Vietnam.
Table 1 Baseline characteristics of the study population in Bangladesh, Vietnam and Ethiopia; baseline data from Alive & Thrive
HAZ, length/height-for-age Z-score; WAZ, weight-for-age Z-score; WHZ, weight-for-length/height Z-score; ARI, acute respiratory infections; CMD, common mental disorders; SES, socio-economic status.
Bivariate associations between maternal common mental disorders and child undernutrition and illness
The prevalence of undernutrition and child illnesses by maternal CMD is shown in Fig. 1(a) and (b). Compared with children of mothers with low CMD, children of mothers with high CMD had a significantly higher proportion of stunting, underweight and wasting in Bangladesh and Vietnam, and a higher proportion of underweight in Ethiopia. Similarly, children of mothers with high CMD also had more illnesses (both diarrhoea and ARI) than their counterparts across the three countries.
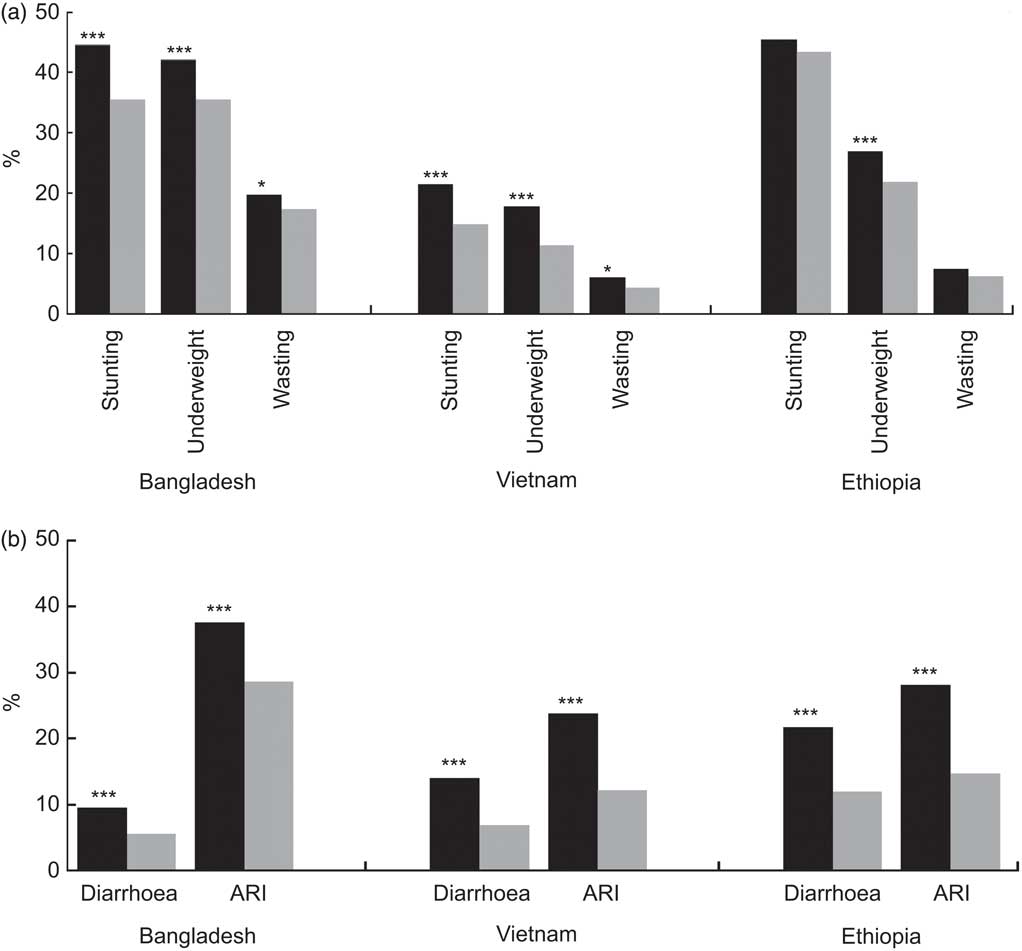
Fig. 1 Bivariate association of maternal common mental disorders (CMD) (
![]() , high CMD;
, high CMD;
![]() , low CMD) with (a) child undernutrition (stunting, underweight and wasting) and (b) child illnesses (diarrhoea and upper acute respiratory infections (ARI) in the past two weeks) in Bangladesh, Vietnam and Ethiopia; baseline data from Alive & Thrive. *P < 0·05, ***P < 0·001
, low CMD) with (a) child undernutrition (stunting, underweight and wasting) and (b) child illnesses (diarrhoea and upper acute respiratory infections (ARI) in the past two weeks) in Bangladesh, Vietnam and Ethiopia; baseline data from Alive & Thrive. *P < 0·05, ***P < 0·001
Multivariate analyses of the association between maternal common mental disorders and child undernutrition and illness
The results from logistic regression models on the association between maternal CMD and child undernutrition are presented in Table 2. The reference category was mothers with low CMD. When adjusting for child, maternal and household factors, mothers with high levels of CMD had significantly higher odds of having a stunted child compared with mothers with low levels of CMD in Bangladesh (adjusted OR = 1·21; 95 % CI 1·03, 1·41), but not in Vietnam and Ethiopia. Similarly, mothers with high CMD were 1·27 times (95 % CI 1·01, 1·61) more likely to have underweight children than mothers with low CMD in Vietnam. There was no significant association between maternal CMD and wasting in any of the countries when adjusting for confounding factors.
Table 2 Results of multivariate analyses of the association between maternal CMD and child undernutrition in Bangladesh, Vietnam and Ethiopia†; baseline data from Alive & Thrive
CMD, common mental disorders; ref., referent category; ARI, acute respiratory infections; SES, socio-economic status.
(*) P < 0·10, *P < 0·05, **P < 0·01, ***P < 0·001.
† Results presented are odds ratios. Models were also adjusted for age squared and cluster effects.
‡Maternal BMI was used for the wasting model.
Among other factors, ARI was significantly associated with child undernutrition (stunting, underweight and wasting) in Bangladesh, but not in other two countries. Low birth weight was strongly associated with all three indicators of child undernutrition across the three countries. Boys were more likely than girls to be wasted in all three countries, and were more likely to be stunted and underweight in Bangladesh and Ethiopia. As expected, lower household SES was associated with higher odds of child undernutrition in all three countries; and household food insecurity was associated with higher odds of stunting in Bangladesh and Ethiopia. Higher maternal education was associated with lower odds of stunting, and taller women had lower odds of having undernourished children in all three countries.
The results of multivariable logistic regression of the association between maternal CMD and child illness symptoms showed that maternal CMD was strongly associated with both child diarrhoea and upper ARI in all three countries (Fig. 1 and Table 3). Compared with children of mothers without CMD, those whose mothers had CMD had 1·67 (95 % CI 1·22, 2·25), 2·11 (95 % CI 1·61, 2·76) and 1·83 (95 % CI 1·47, 2·27) times higher odds of experiencing diarrhoea in the two weeks prior to the survey, and 1·41 (95 % CI 1·15, 1·73), 2·05 (95 % CI 1·61, 2·62) and 2·10 (95 % CI 1·72, 2·57) times higher odds of having had upper ARI, in Bangladesh, Vietnam and Ethiopia, respectively.
Table 3 Results of multivariate analyses of the association between maternal CMD and child illness in Bangladesh, Vietnam and Ethiopia†; baseline data from Alive & Thrive

CMD, common mental disorders; ref., referent category; ARI, acute respiratory infections; SES, socio-economic status.
(*) P < 0·10, *P < 0·05, **P < 0·01, ***P < 0·001.
† Results presented are odds ratios. Models were also adjusted for age squared and cluster effects.
Associations between maternal common mental disorders and maternal and household characteristics, child feeding practices, hygiene and health-seeking behaviours
In an effort to characterize mothers with CMD, we examined the association between CMD and maternal and household characteristics (Table 4). The results showed that maternal CMD was more prevalent among older women, women with lower education level and those suffering from undernutrition (BMI <18·5 kg/m2). Not surprisingly, women living in a food-insecure household or a household of lower SES were much more likely to have high CMD than women from more food-secure or wealthier households. These findings were consistent across all three countries.
Table 4 Bivariate association of maternal CMD with maternal and household characteristics in Bangladesh, Vietnam and Ethiopia; baseline data from Alive & Thrive
CMD, common mental disorders; SES, socio-economic status.
**P < 0·01, ***P < 0·001.
When looking at the potential pathways by which maternal CMD might be associated with child health and nutrition, we found that maternal CMD was significantly associated with poorer hygiene practices (proxied by child's cleanliness or mother's cleanliness) and a lower likelihood of having attended prenatal care services (Table 5). These findings were true for all three countries. There was also a pattern of poorer IYCF practices among mothers with high CMD, but differences were statistically significant only for early initiation of breast-feeding in Vietnam and Ethiopia, and for minimum acceptable diet (a composite indicator of appropriate child feeding practices) in Vietnam.
Table 5 Bivariate association of maternal CMD with child feeding practices, hygiene and health-seeking behaviours in Bangladesh, Vietnam and Ethiopia; baseline data from Alive & Thrive
CMD, common mental disorders.
*P < 0·05, **P < 0·01, ***P < 0·001.
†Minimum meal frequency is defined as 2 times/d for breast-fed infants aged 6–8 months; 3 times/d for breast-fed children aged 9–23·9 months; 4 times/d for non-breast-fed children aged 6–23·9 months. ‘Meals’ include both meals and snacks and frequency is based on mother's report.
‡Acceptable diet is defined as at least the minimum dietary diversity and the minimum meal frequency during the previous day.
§Fe-rich or Fe-fortified foods include flesh foods, commercially fortified foods especially designed for infants and young children that contain Fe, or foods fortified in the home with a micronutrient powder containing Fe.
Discussion and conclusions
The present paper indicates that maternal CMD is a considerable public health problem in Bangladesh, Vietnam and Ethiopia. It also corroborates that maternal CMD is associated with both child undernutrition and common illnesses. After adjusting for potential confounding factors, maternal CMD was associated with 1·21 higher odds of being stunted in Bangladesh and 1·27 higher odds of being underweight in Vietnam. For child illnesses, the associations were even higher and more consistent across countries: children whose mothers had high CMD were more than twice more likely to have upper ARI in Vietnam and Ethiopia (and 1·4 times more likely in Bangladesh); and for diarrhoea, the odds ranged from 1·67 times in Bangladesh to 2·11 times in Vietnam.
To our knowledge, only a few studies, conducted in Chile( Reference Humphreys, Araya and Cruchet 39 ), Nigeria( Reference Adewuya, Ola and Aloba 21 ), Ethiopia( Reference Ross, Hanlon and Medhin 22 ) and Pakistan( Reference Rahman, Bunn and Lovel 20 ), have examined the association between maternal mental health and child illness. Our results showed a strong association between maternal CMD and both diarrhoea and upper ARI in three different countries. These findings suggest that a potential pathway for the relationship between maternal CMD and child undernutrition could be through child illness – as high levels of maternal CMD may hinder a mother's ability to take adequate care of her child, prevent illnesses and seek health care when the child is ill, hence leading to higher illness rates. The illness measurement was based on two-week recall and was similar to the method used in the Demographic and Health Survey. However, the duration and number of episodes of the illnesses were not captured and therefore were not included in the analysis. Other possible mechanisms linking maternal CMD to child growth and child illness include compromised parenting behaviour and non-responsive care-giving practices( Reference Rahman, Harrington and Bunn 40 ). Our data also showed evidence of poorer hygiene practices, lower use of prenatal care services, and some trends towards poorer IYCF practices among mothers with high CMD. There was also evidence in our data that children's illness symptoms (upper ARI and diarrhoea) were associated with undernutrition, although the associations were statistically significant only in Bangladesh.
The lack of an association between maternal CMD and child undernutrition in Ethiopia is consistent with recent findings from a prospective cohort study in Ethiopia. The latter study showed that maternal CMD was associated with child underweight at 12 months in a bivariate analysis, but the association did not remain after adjusting for maternal characteristics or household characteristics( Reference Medhin, Hanlon and Dewey 17 ).
The variability in findings among the three countries, especially regarding the association between maternal CMD and child undernutrition, may be explained by socio-cultural differences in care and feeding practices, differences in maternal resources such as education, knowledge or time, or in household food insecurity and wealth( Reference Surkan, Kennedy and Hurley 18 ). In our data, the two variables that were most different among the three countries were maternal education (with 65·4 % of women in Ethiopia having no schooling compared with 26·8 % of women in Bangladesh and 15·7 % of women in Vietnam) and household food insecurity (the prevalence of food insecurity was twice as high in Ethiopia as it was in Bangladesh and Vietnam). We examined whether the association between maternal CMD and child nutrition outcomes in Ethiopia differed by maternal education, household SES or food insecurity, but we did not find evidence of such interactions (results not shown). It is possible, therefore, that the variability in the associations across countries could be attributable to broader socio-cultural issues, including potential differences in access to social support mechanisms or social networks within communities for women with high CMD.
The high prevalence of maternal CMD among women in the three countries and the associated risk of high CMD for child undernutrition and child illness suggest that interventions to address maternal mental well-being, and the factors that influence mental well-being, could make important contributions to improving the health and nutrition of children. Several environmental and poverty-related factors were associated with CMD in our analyses (lower education, living in a food-insecure or a lower-SES household), which suggests that attempts to relieve some of these constraints (e.g. through poverty reduction, social protection, women's empowerment programmes) may be necessary to help improve maternal mental well-being. In the context of behaviour change interventions which aim at reducing undernutrition and death in children by improving IYCF practices, CMD might be an important factor that prevents mothers either from participating in the programme or from adopting recommended practices( Reference Rahman, Patel and Maselko 6 , Reference Field 41 ). Further, programme interventions focused on the creation of women's groups and health committees to discuss maternal and child health problems and formulate approaches to deal with them based on methods learned within these group settings have also shown to be successful in improving maternal mental health and breast-feeding practices, indicating that interventions centred around improving maternal CMD can be an important aspect to consider( Reference Tripathy, Nair and Barnett 42 ). It would therefore be important to examine the role of maternal mental well-being in relation to participation in public health programmes and adoption of public health recommendations that require behaviour change.
The strengths of the present study include the large samples of mother–child dyads in the three countries and the use of the same questionnaire and survey methodology, which allowed for a valid comparison across countries. The instrument used to capture maternal CMD was validated for use in developing countries( 30 ) and was locally adapted by taking cultural and social factors into consideration. Finally, the availability of data on a wide range of child, maternal and household factors in the surveys allowed us to control for a range of potentially confounding factors and isolate the association between maternal CMD and child undernutrition and illness.
Two limitations of the study merit further discussion. First, data were collected based on maternal recall of their emotional distress in the last four weeks (for CMD) and of their children's symptoms of illness in the two weeks prior to the interview. Maternal recall has its limitations and can result in either under- or over-reporting of information. We do not have evidence, however, to suggest that maternal CMD could adversely affect recall and assume, therefore, that recall biases for CMD and illness are randomly distributed across the sample. The cut-off point used to categorize the level of high and low maternal CMD was supported by one validation study( Reference Giang, Allebeck and Kullgren 32 ) and it is possible that the cut-off itself is not uniformly applicable across countries. However, analyses with the continuous variables for CMD yielded similar results. Second, the cross-sectional nature of the data used for the present analysis did not allow us to establish the causal relationship of maternal CMD with child undernutrition and illness. The potential of reverse causality cannot be ruled out as children's poor growth or illness may cause maternal stress or mental distress, which in turn may impede the ability of mothers to take adequate care of their children and lead to compromised growth and increased prevalence of infections( Reference Stewart 5 ). Several studies support this hypothesis. Preterm birth and failure to thrive among children have been found to be associated with postnatal depression( Reference Surkan, Kennedy and Hurley 18 , Reference Vigod, Villegas and Dennis 43 , Reference Drewett, Blair and Emmett 44 ). Additionally, there is evidence from intervention trials showing that interventions targeted to the child, through early child stimulation activities, have positive effects on reducing maternal depression( Reference Baker-Henningham, Powell and Walker 45 ). This further suggests reverse causality of the relationship between CMD and child undernutrition.
The results from the present study contribute to the growing evidence of the potential negative effects of maternal mental health on child undernutrition and illness. The findings underscore the importance of identifying ways to prevent, detect and address maternal mental health in the context of programmes aimed at improving child health and nutrition in these countries and in similar settings elsewhere.
Acknowledgements
Sources of funding: The study was supported by the Bill & Melinda Gates Foundation through Alive & Thrive (A&T), managed by FHI360. Conflicts of interest: There is no conflict of interest. Authors’ contributions: P.H.N. participated in the concept and design, coordinated data collection in Vietnam, performed statistical analysis of the data, and drafted and revised the manuscript. K.K.S. coordinated data collection in Bangladesh, provided comments for the analyses, contributed to the introduction and discussion, and edited the paper. D.A. coordinated data collection in Ethiopia, provided comments for the analyses, and contributed to the introduction and discussion. P.M. participated in the overall design of the baseline survey and provided comments/inputs for the analyses and manuscript. S.M. participated in the literature review and provided background for the topics. L.T.M. assisted in the analyses and prepared tables/figures. R.R. participated in the overall design of the baseline survey. M.T.R. participated in the overall design of the baseline survey, provided comments/inputs for the analyses and revised the manuscript. Acknowledgements: The authors are grateful to Ali Subandoro for research assistance and to Edward Frongillo for statistical advice.








