Breast-feeding has numerous benefits for maternal and child healthReference Grummer-Strawn and Rollins (1) and society (2) . Exclusive breast-feeding is recommended for 6 months and continued breast-feeding for 1 (3) or 2 years or beyond (4) . However, as recently as 2013, only 22 % of infants born in the USA were exclusively breast-fed for 6 months and 31 % were still breast-fed at 12 months (5) . In 2015, nearly 55 % of all mothers with a child under 1 year of age were working in the USA (6) . The timing of most women’s return to work after birth overlaps with the recommended time frame for breast-feeding; nearly half of working mothers returned to work within 8 weeks of taking parental leave and 22 % returned within 2 weeksReference Klerman, Daley and Pozniak (7) . Employed mothers have lower initiation rates and shorter durations of breast-feeding than those who are unemployed (2) .
One way for women to continue breast-milk feeding (BMF; including feeding at breast and feeding expressed breast milk) while working is to pump breast milk when separated from their infants (2) . The prevalence of breast-milk pumping is increasingReference Johns, Forster and Amir (8) , but its effect on duration among mothers returning to work in the early postpartum period is unknown. Pumping may enable women to continue BMF longer than if they had not pumped( Reference Rasmussen and Geraghty 9 , Reference Meehan, Harrison and Afifi 10 ), and current policies encourage pumping as a way to extend BMF duration (11) , but there is mixed evidence for an association of pumping with BMF durationReference Johns, Forster and Amir (8) . For example, in one observational study, low-income mothers who were given a breast pump requested formula 4 months after mothers who did not receive a pumpReference Meehan, Harrison and Afifi (10) . In another observational study, however, mothers who pumped for non-elective reasons (including employment) had shorter BMF durations than those who pumped electively (e.g. to donate to another infant)Reference Felice, Cassano and Rasmussen (12) .
The purpose of the present study was to estimate the effect of early (defined as infant age less than 9 weeks), regular breast-milk pumping (participant defined) on time to BMF and exclusive BMF cessation, for working and non-working women in the USA. Better understanding of the relationship between early, regular pumping and BMF durations is critical to ascertain if workplace policies that support breast pumping actually have the intended consequence of extending the duration of BMF.
Methods
The Infant Feeding Practices Survey II (IFPS II) was conducted by the US Centers for Disease Control and Prevention, the US Food and Drug Administration and other partners from 2005 to 2007. Its methods are reported in detail elsewhereReference Fein, Labiner-Wolfe and Shealy (13) and briefly summarized here.
Study population and data collection
The original study cohort comprised 3033 women who were aged 18 years or older in their third trimester and who delivered a live, singleton infant weighing 5 lb (~2268 g) or more at 35 weeks or more of gestation, spent 3 d or fewer in the neonatal intensive care unit and completed the neonatal survey (14) . Those women were members of, or living in the household of a member of, a consumer opinion panel. Using that panel was deemed the most efficient way to identify a nationally distributed group that was likely to complete multiple questionnairesReference Fein, Labiner-Wolfe and Shealy (13) . The women completed a prenatal questionnaire at the time of enrolment, reporting information pertaining to prenatal care, maternal diet and postnatal plans for infant care and feeding, and then a telephone survey to report birth-related data, after which investigators confirmed eligibility. Women completed subsequent questionnaires monthly during months 2 to 7 and then every 7 weeks until month 12, providing information about childcare, employment, infant feeding practices, sleep, maternal depression and infant health.
From the original study cohort (n 3033), we selected women who reported BMF on the month 2 questionnaire (n 1624), when the exposure (regular pumping) was measured (first analysis). For the second analysis, we selected women exclusively BMF at the time they completed the month 2 questionnaire (n 971) from the original study cohort (Fig. 1). Both BMF and exclusive BMF were determined by responses to questions about food consumed by the infant in the past 7 d. If her infant consumed only breast milk, then a woman was considered to be exclusively BMF (14) .
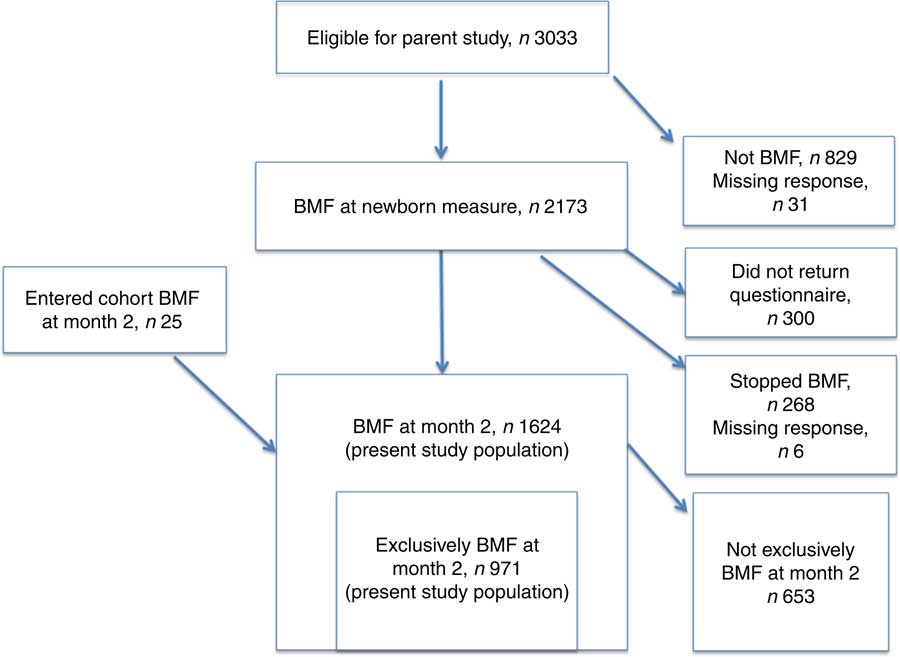
Fig. 1 Participation flowchart for study populations (BMF, breast-milk feeding)
Exposure assessment
The exposure for the present study is ‘regular pumping’ (including expressing breast milk in any way but not further defined on the questionnaire) that began when the infant was less than 9 weeks of age. Mothers responded to: ‘Are you now pumping milk on a regular schedule?’ (answer: yes or no), followed by ‘How old was your baby when you first began pumping on a regular schedule?’ (answer: number of days or weeks) on the 2-month questionnaire (15) . ‘Regular schedule’ was not defined on the questionnaire. Less than 10 % of questionnaires intended to be completed at month 2 (~8·6 weeks) were completed at 13 weeks or more after birth. All mothers who were not regularly pumping or not pumping at all were considered unexposed.
Outcome assessment
Although there is a growing body of research that distinguishes between feeding at breast and expressing breast milk for feedingReference Felice, Cassano and Rasmussen (12) , the IFPS II did not collect those data. Therefore, ‘BMF’ in the present study encompasses both practices. The main outcomes of interest were time to cessation of BMF (including exclusive and partial) and exclusive BMF. Women who continued BMF for at least the recommended duration were censored at the time of reaching the recommended duration (6 months for exclusive BMF and 12 months for BMF) (3) . Each monthly questionnaire contained a module for mothers to complete when they had stopped all breast-feeding and pumping. Respondents indicated infant age when the mother stopped breast-feeding and pumping milk (not necessarily when the infant stopped receiving breast milk). Thus, BMF duration for the current analysis is a measure of the mother’s practice. The Centers for Disease Control and Prevention imputed missing values for BMF duration (approximately 6 % of original study population) (14) , which we used in our analysis. If a mother dropped out of the study, then she was censored and her BMF duration was recorded as her infant’s age at the time of the last completed survey.
Exclusive BMF was measured on each monthly questionnaire through a series of questions about food consumption (14) . We used the IFPS II data set variable for exclusive BMF duration that estimates the mid-point of infant age on the last questionnaire on which the mother indicated exclusive BMF and on the first questionnaire that indicated she was not exclusively BMF. If a mother dropped out of the study, then she was censored and her exclusive BMF duration was recorded as her infant’s age at the time of the last completed survey.
Analysis
To identify appropriate confounders, we created a directed acyclic graph (DAG)Reference Greenland, Pearl and Robins (16) , informed by literature, expert consultation and the Theory of Planned BehaviourReference Bai, Wunderlich and Fly (17) (Dagitty version 2.3). The variables we identified are described in detail in the online supplementary material, Table S1, and include: household income, maternal education, maternal race/ethnicity, previous breast-feeding experience, prenatal intention to breast-feed, childcare plans, planning to return to work, breast-feeding initiation and early practices (index of equally weighted practices in the hospital or birth centre that could affect breast-feeding: pacifier use, breast-feeding within the first hour, feeding other substances to infant, rooming in, breast-feeding support, referral for postpartum support, formula gift bag), professional breast-feeding support if needed, work, childcare arrangement, infant age when mother returned to work, work environment (index of equally weighted unfavourable experiences: negative comments from co-worker; negative comments from supervisor; difficulty arranging break time, place to pump or place to store milk; difficulty carrying pumping equipment; worry about keeping job because of breast-feeding; worry about continuing to breast-feed because of job; embarrassed among co-workers or supervisor) and workplace support. We also tested for effect measure modification by obesity, income, work environment and workplace support. About 20 % of respondents were missing values for more than one covariate.
We conducted all statistical analyses with the statistical software package SAS version 9.4. We used multiple imputation with 100 replications to address the missing exposure and covariate values, using confounders, potential effect measure modifiers and selection factors (described below) as predictors. That imputation enabled us to retain the entire cohort in the analyses until they experienced the outcome or were censored. To control confounding from the large number of identified covariates, we created inverse probability (IP) of exposure weights, using methods recommended by Cole and HernánReference Cole and Hernán (18) .
To address potential selection bias, we used two kinds of additional weights. The present study began at month 2 because that was when the exposure (regular pumping) was reported and, therefore, excludes women who stopped BMF before then. To address potential bias caused by that exclusion, we created and applied IP of selection weights using methods similar to those reported by Bengtson et al. Reference Bengtson, Pence and Gaynes (19) . To create those weights, we considered covariates associated with BMF and exclusive BMF at month 2 and then estimated the selection weights as the IP of BMF (and exclusive BMF, separately), with these predictors in the weights equation for BMF: maternal age, college degree, experience of breast-feeding-related pain in the first 2 weeks, marital status and plans to return to work within the first 9 weeks. Selection weights for exclusive BMF included all the predictors for BMF except maternal age because it was not statistically significant at α=0·05. We stabilized the weights by the marginal probability of BMF or exclusive BMF at month 2, which reduced the weights at the extremes, i.e. for exposed women with a low probability of exposure, and the converseReference Xu, Ross and Raebel (20) . In addition, about 20 % of observations were lost to follow-up. We created and applied time-varying IP dropout weights to address possible selection bias due to loss to follow-upReference Buchanan, Hudgens and Cole (21) . All weights were created in the imputed data set.
We used Cox proportional hazards regression models for the outcome assessed at months 2–12 (BMF) and months 2–6 (exclusive BMF) to estimate the hazard ratio (HR) for BMF cessation according to pumping status in the imputed data set. We then stratified the analyses by work status. Women were considered to be working if they answered: ‘Did you work for pay any time during the past 4 weeks?’ on the month 2 survey (15) affirmatively. Finally, we computed crude Kaplan–Meier curves with the unimputed data set to illustrate the probability of BMF for the exposure groups over time.
Results
Most regular pumpers who were BMF at month 2 were married, white, not working (i.e. did not work for pay any time in the past 4 weeks), and had previous breast-feeding experience and a college degree (Table 1). In addition, most were working at the time of study enrolment (third trimester), had childcare plans for when they would be separated from their infants for feeding, and reported pumping so that someone else could feed their infants. Most non-regular/non-pumpers who were BMF had profiles similar to those of regular pumpers, except that most of the former were not working at the time of study enrolment and had childcare plans in which mother and infant were not separated for feeding. Sixty per cent of non-regular/non-pumpers occasionally pumped, and most of them pumped so that someone else could feed their infants. Regular and non-regular/non-pumpers who were exclusively BMF had similar profiles to women in the BMF groups (Table 1).
Table 1 Maternal and infant descriptive characteristics for 1624 women who reported breast-milk feeding (BMF) when they completed the month 2 questionnaire for the US Infant Feeding Practices Survey II (IFPS II), 2005–2007
* Missing, n 6.
† Missing, n 13; exclusive breast-feeding is a subset of any breast-feeding.
‡ Missing, n 42.
§ Women enrolled during the third trimester.
║ Measured in months for any BMF (median reported) and by month range for exclusive BMF.
¶ Variable composition described in the online supplementary material, Table S1.
** Referral for depression treatment is recommended for score of 13 or higher on the Edinburgh Postpartum Depression Screening tool.
†† Worked sometime in the past 4 weeks, from time completed month 2 questionnaire.
‡‡ This is the denominator (those who had pumped) for the list of reasons pumped. Respondents could choose more than one reason.
The crude Kaplan–Meier curve for BMF diverged by pumping status at about 13 weeks, showing a lower probability of BMF for women who pumped regularly compared with women who did not (Fig. 2). The crude curves stratified by work status also diverged at about 13 weeks, showing that women who neither worked nor pumped regularly had the highest probability of BMF, followed by women who worked but did not pump regularly, women who both worked and pumped regularly, and women who did not work but pumped regularly (Fig. 2). The crude Kaplan–Meier curves for exclusive BMF showed a divergence at about 9 weeks, with regular pumpers having a lower probability of exclusively BMF at every subsequent time point compared with non-regular/non-pumpers (Fig. 3). The crude curves stratified by work status also diverged at about 9 weeks, with regular pumpers who were not working having the lowest probability of exclusively BMF, while the other groups had cessation rates similar to one another.
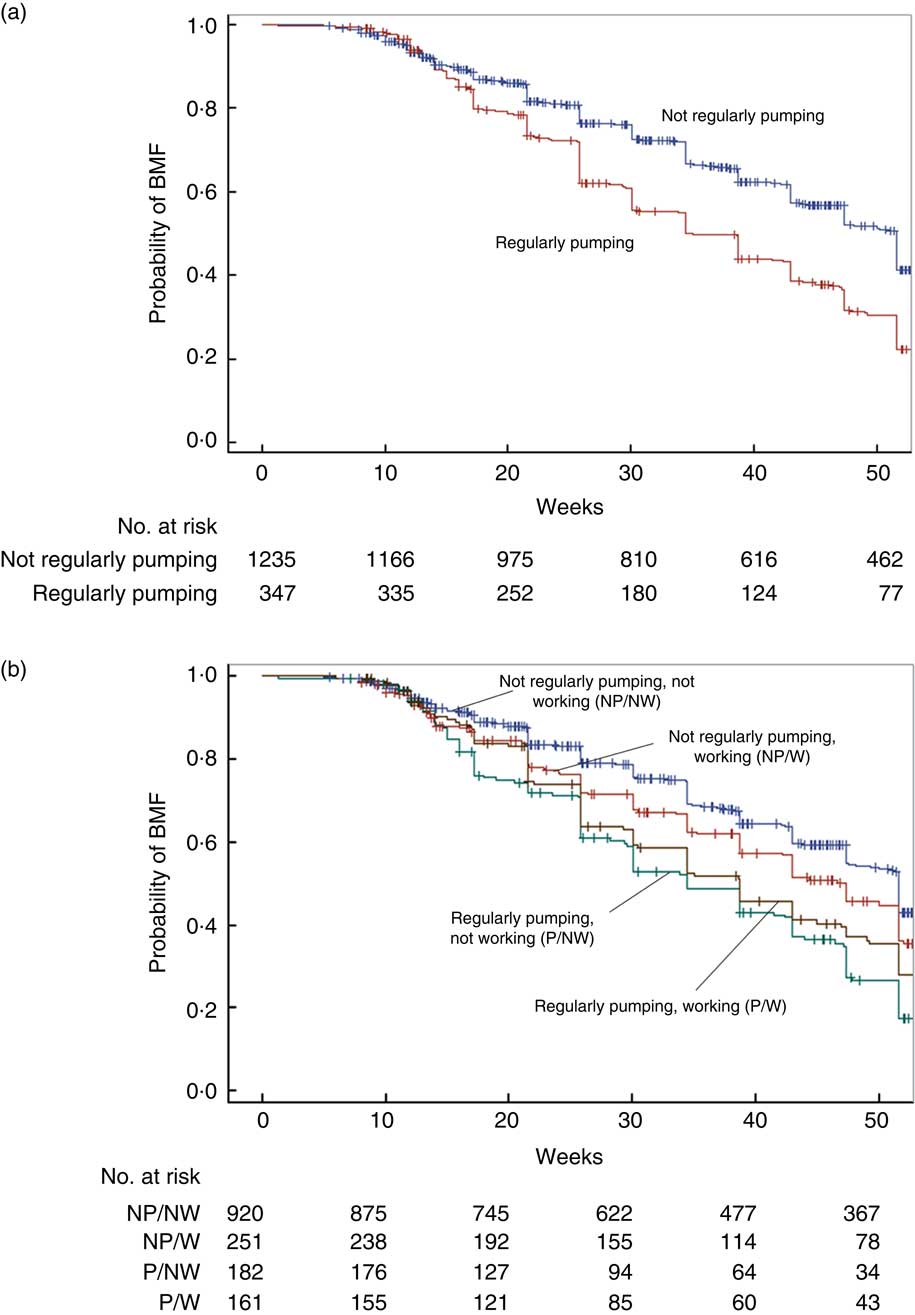
Fig. 2 (colour online) Kaplan–Meier curves (+, censored) for 1624 women in the US Infant Feeding Practices Survey II (IFPS II) feeding breast milk to their infants, by (a) pumping practice and (b) work status, 2005–2007. (a) Crude curves computed from unimputed data set; forty-two observations missing (<3 %); log rank P<0·0001; (b) crude curves computed from unimputed data set; 110 observations missing (<7 %); log rank P<0·0001 (BMF, breast-milk feeding)
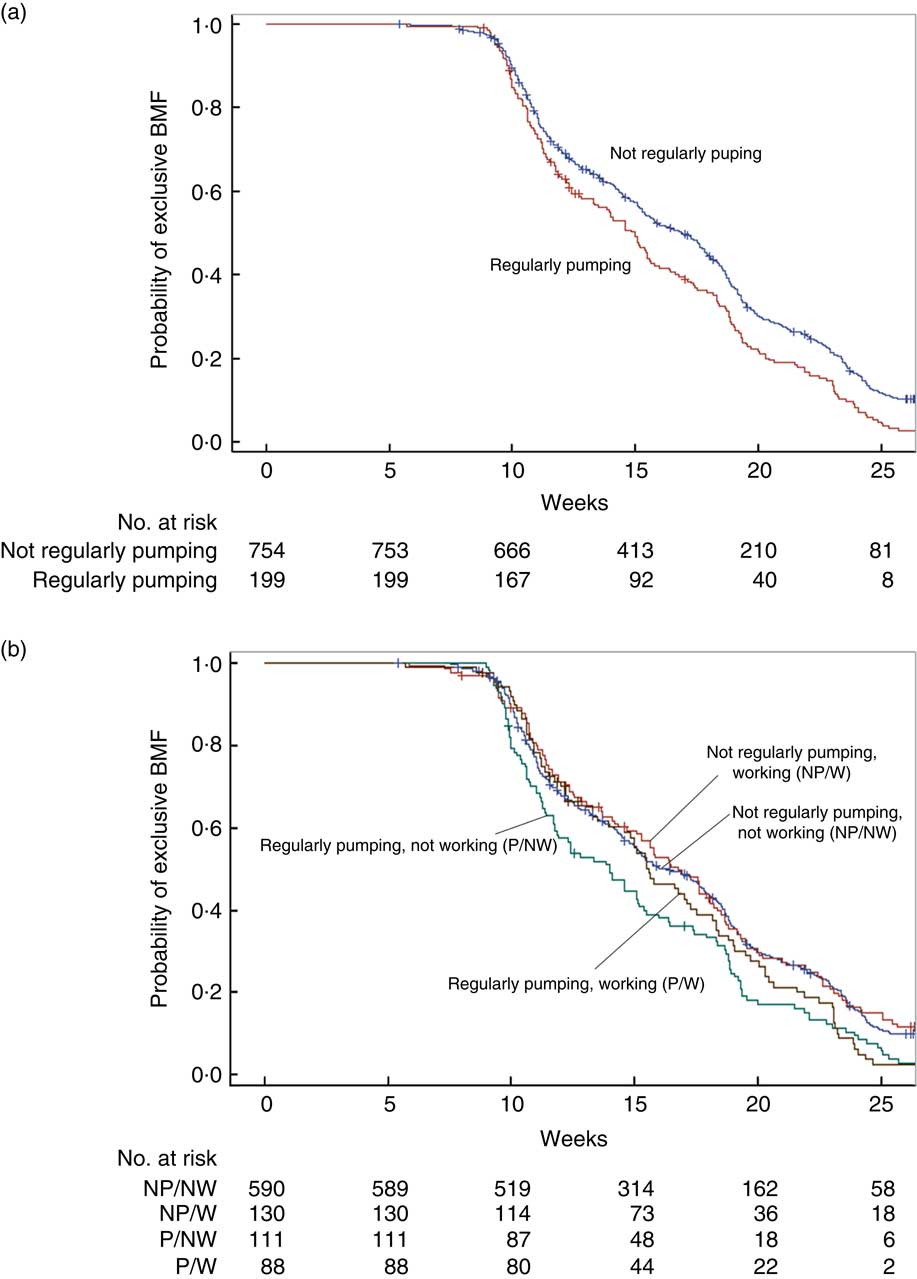
Fig. 3 (colour online) Kaplan–Meier curves (+, censored) for 971 women in the US Infant Feeding Practices Survey II (IFPS II) exclusively feeding breast milk to their infants, by (a) pumping practice and (b) work status, 2005–2007. (a) Crude curves computed from unimputed data set; eighteen observations missing (<2 %); log rank P=0·0004; (b) crude curves computed from unimputed data set; fifty-two observations missing (<6 %); log rank P=0·0062 (BMF, breast-milk feeding)
In the first weighted Cox proportional hazards regression model, regular pumpers had an increased hazard of early BMF cessation (HR=1·62; 95 % CI 1·47, 1·78; Table 2) compared with non-regular/non-pumpers. When stratified by working status, the estimated effect of regular pumping on time to BMF cessation was close to the null among working women (HR=0·90; 95 % CI 0·75, 1·07), but was two times higher among non-working women (HR=2·05; 95 % CI 1·84, 2·28). In the second weighted Cox proportional hazards regression model, regular pumpers had an increased hazard of early exclusive BMF cessation (HR=1·14; 95 % CI 1·03, 1·25; Table 2) compared with non-regular/non-pumpers. When stratified by working status, the estimated effect of regular pumping on time to exclusive BMF cessation was higher than in non-regular/non-pumping among working women (HR=1·14; 95 % CI 0·96, 1·36), but the CI includes the null value. There was a similar result among non-working women (HR=1·10; 95 % CI 0·98, 1·22). Thus, while the overall estimated effect of early pumping on time to exclusive BMF cessation was significant, stratification by work indicated a null estimated effect for both groups.
Table 2 Hazard ratios (HR) for the effect of regularly pumping, recorded at 2 months after birth, compared with not regularly pumping, on time to stopping breast-milk feeding (BMF) within 12 months postpartum, for 1624 women BMF at 2 months in the US Infant Feeding Practices Survey II (IFPS II), 2005–2007
* BMF: weighted for selection (mean=0·98; range 0·69–5·72) and loss to follow-up (mean=0·99; range 0·27–3·46) in imputed data set.
† Exclusive BMF: weighted for selection (mean=1·00; range 0·48–7·54) and loss to follow-up (mean=1·00; range 0·10–4·99) in imputed data set.
‡ Weighted to control for confounding by household income, education, white race/ethnicity, prenatal breast-feeding intention, childcare plan, plan to return to work within 9 weeks, early breast-feeding practices, accessing help for breast-feeding problems, infant age when mother returned to work, mother–infant sometimes separated for feeding, work, late preterm status, work environment and workplace support. Also weighted for selection and loss to follow-up in imputed data set: BMF weights (mean=0·98; range 0·24–8·66); exclusive BMF weights (mean=1·00; range 0·21–17·64).
§ Missing, n 42 (<3 %).
║ Reported on month 2 questionnaire; missing, n 68 (<5 %).
¶ Missing, n 18 (<2 %).
** Reported on month 2 questionnaire; missing, n 34 (<4 %).
Of the four variables tested, only work environment was a statistically significant effect measure modifier (P<0·05) and only for exclusive BMF. Regular pumpers who had no unfavourable experiences at work had an increased hazard of exclusive BMF cessation compared with non-regular/non-pumpers (HR=1·31; 95 % CI 1·03, 1·66). For working women who regularly pumped and had unfavourable experiences at work, the estimated effect of regular pumping on time to exclusive BMF cessation was lower than in non-regular/non-pumping among working women (HR=0·82; 95 % CI 0·61, 1·10), but the CI includes the null value.
When we reviewed the characteristics of regular pumpers, we found that 45 % who BMF and did not work at month 2 had planned to return to work in the first year (see online supplementary material, Table S2). While 11 % of non-working regular pumpers had a high depression score, 6 % of working, regular pumpers had a high depression score. The reasons for pumping among working and non-working regular pumpers were generally similar. Among non-working regular pumpers: 76 % pumped for someone else to feed the baby; 56 % pumped to have an emergency supply; 46 % pumped to increase supply; 46 % did not want to breast-feed or infant could not breast-feed; 40 % pumped to relieve engorgement; and 27 % pumped to maintain supply when separated or infant was ill. Among working, regular pumpers: 85 % pumped for someone else to feed the baby; 47 % pumped to maintain supply when separated or infant was ill; 37 % pumped to have an emergency supply; 34 % did not want to breast-feed or infant could not breast-feed; and 32 % pumped to relieve engorgement (Table S2).
For those exclusively BMF, 33 % who did not work at month 2 had planned to return to work in the first year, and nearly half (48 %) had not planned to return to work in the first year. Reasons for regularly pumping at month 2 among women who exclusively BMF were similar by work status. Non-working women reported regularly pumping for someone else to feed the baby (82 %); to have an emergency supply of breast milk (68 %); to increase milk supply (46 %); to relieve engorgement (40 %); because they did not want to breast-feed or infant could not (39 %); and to maintain supply when separated or infant was ill (25 %). Among working, regular pumpers: 90 % pumped for someone else to feed the baby; 48 % pumped to have an emergency supply of breast milk; 43 % pumped to maintain supply when separated or infant was ill; 41 % pumped to increase milk supply; 32 % pumped to relieve engorgement; and 32 % pumped because they did not want to breast-feed or infant could not breast-feed (see online supplementary material, Table S2).
Discussion
The present study estimated the effect of regular breast-milk pumping in the early postpartum period on time to BMF and exclusive BMF cessation, up to the recommended durations (12 months and 6 months, respectively), among working and non-working women in the USA. We found that regular pumpers were more than 60 % more likely to stop BMF, and nearly 15 % more likely to stop exclusive BMF, than non-regular/non-pumpers, within the recommended time frames. Work status modified the association only for women who BMF. Among working women who BMF, regular pumping had a nearly null estimated effect; however, non-working women who regularly pumped were more than twice as likely to stop BMF as non-regular/non-pumpers. Among working women who exclusively BMF, our findings suggested an elevated hazard for regular pumping compared with non-regular/not pumping, although the CI included the null. There was a similar estimation for non-working women who exclusively BMF.
These results suggest that regular pumpers in the early postpartum period may be more likely to stop BMF than their non-regular pumping counterparts and may need specialized support to BMF for the recommended duration. In particular, regular pumpers who are not working may need support. Further, regular pumping, as opposed to non-regular or not pumping, may neither help nor hinder working women’s BMF and exclusive BMF durations, despite policy intentions to support breast-feeding through breast pumping (11) and national goals to increase BMF duration (22) . This finding suggests that workplace protections of BMF that focus mainly on pumping may not be effective in increasing BMF and exclusive BMF durations for working women.
One explanation for the observed association between pumping and early cessation of BMF could be that women who pumped to build a supply of expressed milk planned to use that supply to continue BMF after they returned to work. They may have intended to pump less often than their infants’ feeding patterns, or not at all, at work. Not removing milk at regular intervals during the workday would eventually decrease supplyReference Mannel and Walker (23) , which could lead to BMF cessation. Many regular pumpers who were not working at month 2 had planned to return to work within the first year. Most regular pumpers in the present study cited reasons for pumping that could be related to employmentReference Geraghty, Davidson and Tabangin (24) , although that was not specified. Overall, several categories of ‘reasons for pumping’ overlap and it is difficult to distinguish between them, e.g. ‘pumping for someone else to feed the infant’ and ‘to maintain supply when infant could not nurse due to separation or infant illness’, both of which could be related to working. Thus, the utility of the information pertaining to reasons for pumping is limited.
The fact that regular pumping was not associated with BMF and exclusive BMF cessation among working women in our study was somewhat surprising; we had expected to find either a protective effect on duration, as reported by Meehan et al. Reference Meehan, Harrison and Afifi (10) , or a detrimental effect, as reported by Felice et al. Reference Felice, Cassano and Rasmussen (12) . Our finding may represent the statistical equalizing of two different strategies for BMF at month 2 in this population. The first strategy, mentioned above in the context of women who were not working at month 2, could also apply to women working at month 2, with the same consequence through the aforementioned biological mechanism. The second strategy, pumping at work, could lead to early cessation for some but not others, due to: a biological mechanism through which repeated ineffectiveReference Mannel and Walker (23) or infrequent milk removal could decrease supply( Reference Baker and Lamb 25 ); a reluctance to pump due to the psychological and logistical burdens of carrying pumping supplies and equipment, and of negotiating time and space for pumping during the workday and cleaning pump parts, as well as milk storage; or unknown factors.
Our findings suggested a detrimental effect of regular pumping for women who reported no unfavourable experiences at work, which is consistent with our overall finding: regular pumpers were more likely to stop exclusive BMF compared with non-regular pumpers. We observed no effect of regular pumping compared with non-regular pumping for women with unfavourable experiences at work. There is currently no literature that sheds light on this finding. Perhaps some women became more determined to persist when faced with obstacles while others decided that pumping is not worth risking more unfavourable experiences. Further research on this topic is needed.
Our findings are particularly salient for the USA, which lacks basic maternity protections such as paid leave and affordable, high-quality childcare for all families. However, the USA supports breast-milk pumping as a way for mothers to continue BMF when they are separated from their infants due to work (11) . These data were collected in 2005–2007, before the Affordable Care Act introduced protections for breast-milk pumping in the workplace. Nevertheless, the present study provides some indication of expectations for the effect of regular pumping on BMF duration. Breast-feeding rates in the USA have increased slightly over the past decade (26) and pump ownership has increased under the Affordable Care ActReference Hawkins, Noble and Baum (27) . However, persistent gaps in coverage of breast-feeding support remain( Reference Hawkins, Noble and Baum 27 , Reference Kozhimannil, Jou and Gjerdingen 28 ), underscoring the importance of understanding how breast pumping affects BMF duration.
Our findings align with the results of another study using data from the IFPS IIReference Felice, Cassano and Rasmussen (12) , which reported that a greater frequency of pumping was associated with stopping BMF. A different study with IFPS II data reported that women who pumped at work had longer BMF durations than those who neither pumped nor fed at breast during work time, but shorter BMF durations than women who only fed at breast, or both pumped and fed at breast during work time( Reference Fein, Mandal and Roe 29 ). That study indicated some benefit for pumpers, although neither the regularity nor the frequency of pumping was consideredReference Fein, Mandal and Roe (29) . Neither study used DAG analysis to determine an appropriate set of covariates for adjustment and thus may be biased from uncontrolled confounding, given the number of factors that affect both pumping and BMF duration throughout the perinatal and postpartum periods. Our DAG analysis did not reveal adjustment factors commonly used in breast-feeding studies, such as age and obesity, to be confounders for the effects we studied. In our DAG, age affects regular pumping through its effects on more proximal factors including prenatal intention, which was controlled in our statistical model via IP of exposure weights. Obesity affects regular pumping through its effects on more proximal factors including breast-feeding initiation and early practices, which was controlled in our statistical model via IP of exposure weights. We decided to control for more proximal factors to avoid ‘overcontrol’ and to fit a more parsimonious statistical model.
Prospective studies using data collected after the Affordable Care Act was enacted would provide a useful comparison to understand how its pumping protections may have changed the experiences of, as well as the BMF intensity (exclusive v. any) and durations, for working mothers. In particular, further research among women from various income levels and occupations, and who combine working with BMF using different strategies including minimizing maternal–infant separation, as some have recommended( Reference Fein, Mandal and Roe 29 , 30 ), would be particularly useful.
Strengths of the current study included the use of IP weights to control confounding, which improved model parsimony. Under assumptions of positivity (i.e. a positive probability of each level of exposure at each covariate level), consistency, exchangeability and correct specification of the weights model, the parameters produced by a weighted regression model can estimate the average causal effect of early, regular pumping in our study populationReference Cole and Hernán (18) . For example, positivity assumes that each race/ethnicity category in the analysis (white and non-white) could include regular pumpers and non-regular pumpers. The characteristics of this study population (e.g. >80 % white race/ethnicity) led to certain ‘blunt’ categorization of some variables (e.g. race/ethnicity) to address potential problems with positivity. Our exposure is well defined in that there are not multiple versions of ‘regular pumping in the first 8 weeks’, as defined in this data set; however, ‘regular’ was not defined on the questionnaire or in other parent study materials. We believe that the model is correctly specified because we consulted literature and subject matter experts during the creation of the DAG. DAG theory maintains that appropriate analysis yields a minimally sufficient set of covariates to control confounding of the exposure–outcome relationshipReference Greenland, Pearl and Robins (16) . There was no unmeasured confounding, meaning that we have measured all of the confounders in the minimally sufficient adjustment set of covariates identified by the DAG; however, there is likely residual confounding from an unknown source, which is a common limitation to observational studiesReference Buchanan, Hudgens and Cole (21) . These same assumptions apply to non-weighting methodsReference Cole and Hernán (18) .
We also used selection and dropout weights to address selection bias. There is still selection bias related to membership of consumer panels and meeting participation criteria for the parent study, which prevents generalization of these results to the US maternity population. The parent study population has been reported to be better off than the general maternity population in the USA( 14 ). Thus, our results may be a conservative estimate of the effect of regular pumping on time to BMF and exclusive BMF cessation in the general population, if the observed effect could be stronger for those with fewer resources.
There may be confounding by indication (a type of selection bias), meaning that women may not be included in this study because they decided not to BMF because they knew that they would be returning to work early and could not combine BMF with working. In addition, full- or part-time work status was not measured at month 2, nor was the type of job reported. That information could have enabled an in-depth categorization of ‘work’.
Further, some questionnaires were not completed at the intended time, resulting in possible misclassification or recall bias. Approximately 10 % of women completed month 2 questionnaires more than 13 weeks after childbirth. The variation in time of questionnaire completion could have caused limited misclassification of work status. Exclusive BMF measurement assessed behaviour during the past 7 d; it is assumed that this practice was constant for the remaining days of the month. This is a common but imperfect way to measure exclusive BMF practice. Finally, BMF cessation measures when the mother stopped breast-feeding and pumping milk, and not necessarily when the infant stopped receiving breast milk. Some infants probably continued to receive pumped milk, so the outcome is not fully aligned with the actual measurement.
Public health implications
Early, regular breast-milk pumping was associated with early BMF and exclusive BMF cessation, compared with non-regular or no pumping. It is critical to further evaluate the effect of pump provision and workplace policies, along with access to support, on BMF and exclusive BMF durations. Although the present study took place in the USA, its findings may be relevant for all countries with policies that encourage regular breast-milk pumping in the early postpartum period.
Acknowledgements
Acknowledgements: The authors thank the University of North Carolina’s Breastfeeding Umbrella Study Team for advice on study design and variable specifications, Ann Von Holle for SAS coding advice and Rob Carty for assistance with figures. Financial support: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors. Conflict of interest: None. Authorship: J.Y. designed the study, conducted the analyses and drafted the manuscript. All other authors contributed to the study design and interpretation of the results and provided substantive feedback on manuscript drafts. All authors approved this submission. Ethics of human subject participation: This is a secondary analysis of data from the Infant Feeding Practices Study II, a sample of pregnant women throughout the USA, with follow-up during the first year of life. We used the de-identified, publicly available data set, which was exempted from review by the Institutional Review Board of the University of North Carolina, Chapel Hill.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/S1368980017004281







