The food packages received by beneficiaries of the Special Supplemental Nutrition Program for Women, Infants and Children (WIC) – which includes pregnant and postpartum women, infants and children up to the age of 5 years who live in low-income households – were updated in 2009 to better align them with the Dietary Guidelines for Americans(Reference Taylor1). This food package change included the addition of fruits, vegetables and whole grains; a reduction in the amount of juice and dairy, as well as in the amount of fat allowed in milk; and a reduction in infant formula based on a recalibration of amounts to match infants’ age and needs(Reference Taylor1). Further, post-2009 mothers of fully breastfed infants do not receive formula and are given the most generous food package in terms of food quantity and variety for 1 year postpartum, plus additional complementary foods for their fully breastfed infants from 6 to 12 months, including infant-food fruits, vegetables and meats.(Reference Taylor1) Previous research has found the WIC food package change to be associated with healthier growth trajectories(Reference Chaparro, Crespi and Anderson2) and lower obesity risk(Reference Chaparro, Crespi and Anderson2,Reference Daepp, Gortmaker and Wang3) among WIC-participating children. Among children participating in WIC in Los Angeles County between 2003 and 2016, for example, receiving the new food package continuously from 0 to 4 years, compared with the old, was associated with a 10–12 % lower obesity risk at age 4 years(Reference Chaparro, Crespi and Anderson2). Additional reported benefits related to the food package change include better diet quality for women and children, improved breast-feeding outcomes, and healthier neighbourhood food environments with increased availability of fruits, vegetables and whole grains(Reference Schultz, Byker Shanks and Houghtaling4).
WIC serves only households with family incomes ≤ 185 % of the federal poverty level (FPL). Although not always discussed, variations in nutritional outcomes across income levels have been observed among WIC families(Reference Nobari, Whaley and Prelip5,Reference Freedman, Sharma and Hamner6) . Namely, Nobari et al. (Reference Nobari, Whaley and Prelip5) found that 2–4-year-old WIC-participating children in Los Angeles County living in the lowest income households (< 50 % FPL) had higher obesity prevalence than children living in households with incomes ≥ 50 % FPL, and this trend was consistent across the years of study (2003–2014). Similar findings were observed for neighbourhood income, with WIC-participating children living in the poorest neighbourhoods having the highest obesity prevalence across time(Reference Nobari, Whaley and Prelip5). Freedman et al. (Reference Freedman, Sharma and Hamner6) found similar trends by family income in weight-for-length among 3–23-month-old WIC-participating children in several US states. Yet, it remains unclear if the 2009 WIC food package differentially impacted children’s obesity outcomes, across family income and neighbourhood poverty levels. Identifying if the WIC food package change equitably impacted WIC-participating children is an important policy question, particularly to inform future food package revisions.
The goal of the current study was to investigate if the previously identified association between the new WIC food package and reduced obesity risk among WIC-participating children in Los Angeles County(Reference Chaparro, Crespi and Anderson2) was observed among all participating households, irrespective of their family income or the poverty level of the neighbourhood in which they live. Since children with the lowest income and living in the highest poverty neighbourhoods had the highest obesity prevalence and, therefore, stood to gain the most from improved diets, we hypothesised that the effect of the WIC food package change on obesity would be stronger among children living in very-low-income households (< 50 %FPL), particularly among those living in the poorest neighbourhoods.
Methods
Sample
Administrative data on WIC-participating children in Los Angeles County, California, between 2003 and 2016 from the Data Mining Project (https://apps.phfewic.org/Projects/DataMining.aspx) were used and analysed in 2019. These data include weight and height (or length) measures taken on the same children during WIC (re) certification visits, as well as socio-demographic information on children and their families. In addition, children’s residential addresses were geocoded to 2010-census tract boundaries and linked to data from the American Community Survey to obtain neighbourhood-level variables.
The current study was part of a larger study investigating the impact of the 2009 WIC food package change on children’s growth trajectories from 0 to 4 years and obesity at age 4 years(Reference Chaparro, Crespi and Anderson2); as such, children’s inclusion criteria were to be continuously enrolled in WIC from birth (defined as within 42 d of birth) until age 4 years (inclusive), with at least one weight and height (or length) measurement for each year, either before or after the implementation of the WIC food package change (1 October 2009). Additional inclusion criteria for the current study were for children to live in a census tract with at least five WIC-participating children to protect the identity of WIC participants. Children who met eligibility were grouped based on the dates they participated in WIC: if their enrollment in WIC ended before 1 October 2009, they belonged to the old food package group, whereas those whose enrollment began after 1 October 2009 belonged to the new food package group. Children whose enrollment in WIC overlapped with the implementation of the food package change were excluded. A total of 155 991 children were eligible for inclusion, with a final analytical sample of 79 502 children attained after sample matching (explained below in the ‘Statistical Analysis’ section; Fig. 1).
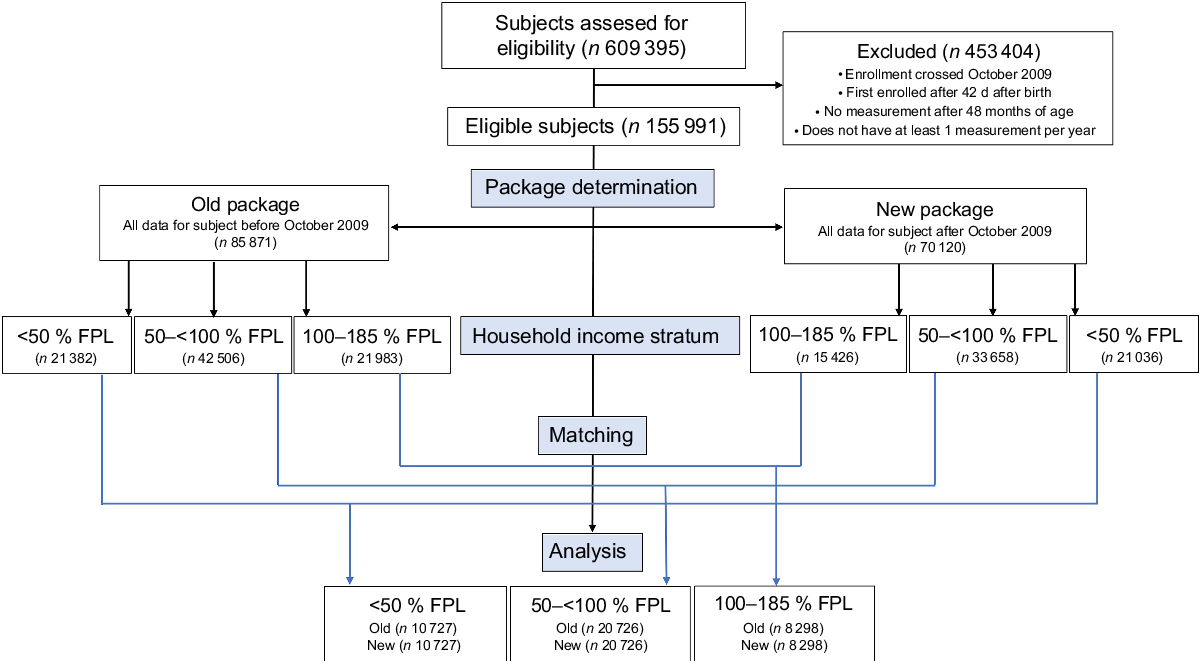
Fig. 1 Flow chart of WIC-participating children included in the study
Outcome
Obesity at age 4 years, defined as a BMI-for-age ≥ 95th percentile in sex-specific growth curves from the Centers for Disease Control and Prevention (CDC), served as the outcome for Poisson regression analyses. Weight and height (or length) used to estimate obesity at age 4 years, as well as initial weight-for-length z-score used as a covariate in multivariable analyses, were measured by WIC staff during WIC eligibility certification and recertification; measurements by WIC staff in Los Angeles County have been found to have high validity(Reference Crespi, Alfonso and Whaley7).
Covariates
Available individual-level socio-demographic data included child’s age, sex and race/ethnicity as reported by the child’s mother (Asian, Black, Hispanic, White and Other); maternal education (less than a high school degree, high school degree or equivalent, and higher than high school) and language preference (English, Spanish and Other); and family size (continuous) and income (<50, 50–100 and >100–185 % FPL). In addition, census tract-level variables from American Community Survey (2005–2009 for children in the old food package group and 2010–2014 for children in the new food package group) included percentage of individuals in the census tract of residence (1) with a high school degree or greater, (2) who are non-White and (3) who live below the FPL (i.e., in poverty).
Statistical analysis
To account for changes in the demographic characteristics of WIC participants in Los Angeles over time,(Reference Chaparro, Crespi and Anderson2) children receiving the new food package were matched one-to-one to children receiving the old food package. Exact matching was used for child’s sex and race/ethnicity; maternal education and language preference; and family income category. Optimal matching was used for age weight-for-length z-score at first measurement(Reference Bergstralh, Kosanke and Jacobsen8,Reference Ming and Rosenbaum9) .
Descriptive statistics were produced to characterise the sample. Further, using this matched sample and accommodating clustering within matched pairs, sex-stratified Poisson regression with robust se estimation(Reference Zou10) was used to determine whether the association between the WIC food package change and obesity risk at age 4 years varied by family income; this was accomplished by including an interaction term between family income strata and WIC package, adjusting by family size and neighbourhood characteristics. Poisson regression overcomes convergence issues in risk ratio estimation common in binomial regression and has lower sensitivity to model misspecifi-cation(Reference Zou10–Reference McNutt, Chuntao and Xue12). Moreover, Poisson regression can provide an unbiased estimate of the risk ratio when there is equal follow-up time and the event of interest is not rare(Reference McNutt, Chuntao and Xue12), and variance overestimation from applying Poisson regression to binary data can be corrected by using a sandwich estimator for robust error variance estimation(Reference Zou10). Sex stratification of our analysis was deemed necessary since the association between the WIC food package change and obesity has been found to be different for boys and girls(Reference Chaparro, Anderson and Crespi13). To assess whether the strength of the association between WIC food package and obesity was further dependent on neighbourhood poverty within each family income category, additional models were run that included interaction terms between percentage neighbourhood poverty (continuous) and (1) WIC food package, (2) family income and (3) the interaction of WIC food package with family income. All analyses were conducted using SAS 9·4 (SAS Institute Inc.). A P-value < 0·05 was deemed statistically significant.
Results
Summary characteristics of the sample by child sex, family income and WIC food package type are displayed in Table 1. Overall, children whose family income was above poverty (>100 % to <185 % FPL) had a lower initial weight-for-length z-score. Regardless of family income, boys and girls receiving the new food package had a lower obesity prevalence at age 4 years than boys and girls receiving the old food package. Even though the sample was predominantly Hispanic overall, Black children were over-represented in the very low-income group (<50 % FPL), while Asian children were over-represented in the above poverty group (>100 % to <185 % FPL). There was minimal variation in average family size (~ four people) across family income groups. As for neighbourhood characteristics, the overwhelming majority of children lived in neighbourhoods where more than 40 % of residents had higher than a high school education and were non-White, regardless of family income. As for neighbourhood poverty, boys and girls with family incomes <50 % FPL were more likely to live in neighbourhoods where more than 40 % of residents lived in poverty. In addition, the proportion of children living in neighbourhoods where more than 40 % of residents lived in poverty was higher for those receiving the new food package, compared with the old, and this was true across all levels of family income.
Table 1 Characteristics of the sample of WIC-participating children in Los Angeles County (2003–2016) by family income strata, sex and food package type (old v. new)

WIC, Special Supplemental Nutrition Program for Women, Infants and Children; FPL, federal poverty level; WLZ, weight-for-length z-score.
* Measured.
† Self-reported.
‡ Obtained from the American Community Survey.
The new WIC food package was associated with a lower obesity risk at age 4 years for both boys and girls across all family income groups (Table 2). For boys, the new package was associated with reductions in obesity risk ranging from 13 to 18 %; for girls, reductions ranged from 7 to 12 %. The association between the new WIC food package and obesity was not modified by family income (interaction P-values > 0·05).
Table 2 Risk ratios (RR) for the association between the 2009 WIC food package change and obesity at age 4 years by family income among a matched sample of WIC-participating children in Los Angeles County, 2003–2016 (n 79 502)
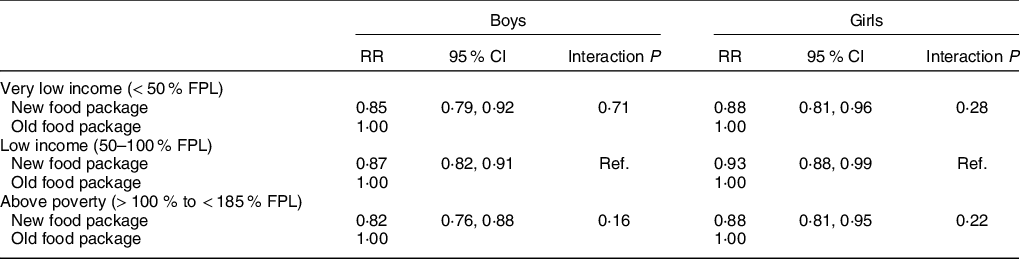
WIC, Special Supplemental Nutrition Program for Women, Infants and Children; FPL, federal poverty level.
Table 3 displays the results of the Poisson regression models predicting obesity risk by WIC food package, including interactions between family income and neighbourhood poverty. Neighbourhood poverty did not significantly modify the association between the new WIC food package and obesity across family income groups (all interaction P-values > 0·05). However, we observed variations in the strength of the association between the new food package and obesity for some sub-groups. Boys living in census tracts in which half of residents lived in poverty, regardless of family income, experienced the largest obesity risk reduction when receiving the new food package compared with the old (20–23 %). On the other hand, girls living in the same type of neighbourhoods (i.e., with 50 % of residents living in poverty), regardless of family income level, did not experience a significant reduction in obesity risk when receiving the new food package, compared with the old.
Table 3 Effect modification of the association between the 2009 WIC package change and obesity at age 4 years by family income and neighbourhood poverty
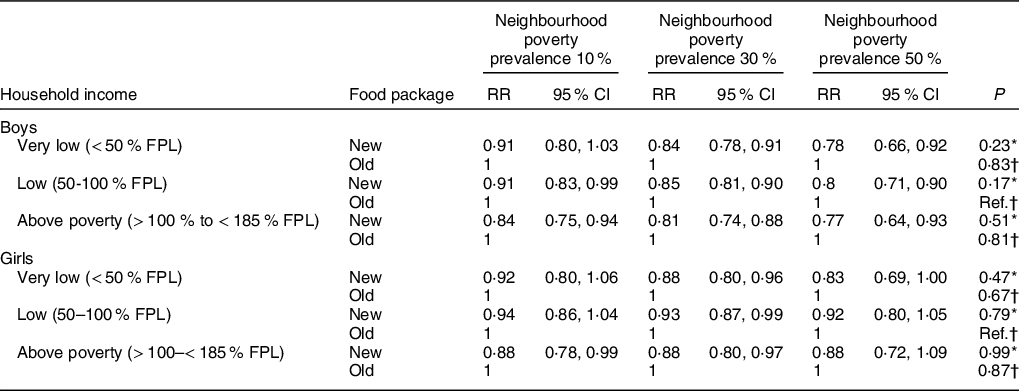
WIC, Special Supplemental Nutrition Program for Women, Infants and Children; FPL, federal poverty level; RR, relative risk.
* P-value for the interaction between WIC package and tract percentage poverty in the specified family income stratum.
† P-value for the comparison of the interactions between WIC package and neighbourhood poverty between family income levels (reference = low income [50–100% FPL]).
Discussion
The goal of the current study was to investigate if a previously identified association between the new WIC food package and reduced obesity risk among WIC-participating children in Los Angeles County applies to all children regardless of their family income and the poverty level of their neighbourhoods of residence. We hypothesised that children living in the poorest households would benefit the most from the WIC food package change in terms of obesity risk, particularly those living in the poorest neighbourhoods. We only found partial support for this hypothesis. Neither family income nor neighbourhood poverty significantly modified the association between the new WIC food package and obesity risk. However, boys living in the poorest households had a modestly larger obesity risk reduction (18 %) compared with boys living in less poor households (13–15 %) when they received the new food package v. the old. For girls, those living in the poorest households (< 50 % FPL) and in households above poverty experienced the same level of obesity risk reduction at 12 % if they received the new food package, compared with the old. In other words, both boys and girls whose families had incomes between 50 and 100 % FPL experienced the smallest obesity risk reductions associated with the new food package receipt compared with the other sub-groups analysed.
While no previous studies have examined the moderating role of family income in the relationship between the WIC food package and child obesity risk, there is evidence that the effects of childhood obesity interventions may vary by family income(Reference Hillier-Brown, Bambra and Cairns14). The Healthy Living Cambridge Kids intervention, for example, used community- and school-wide approaches to encourage healthy eating and physical activity among kindergarten students in Cambridge, MA(Reference Chomitz, McGowan and Wendel15). After a 3-year intervention – which in schools included the introduction of gardens, cooking classes, nutrition education, improved recipes for school lunches and expanded physical education – BMI z-score and obesity prevalence significantly decreased among children in higher income households only(Reference Chomitz, McGowan and Wendel15). On the other hand, an obesity treatment intervention among 2–6-year-olds in ten paediatric clinics in Massachusetts found positive intervention effects (i.e., reduced BMI) only among children living in low-income households(Reference Taveras, Gortmaker and Hohman16). In their systematic review of factors that modify (i.e., moderators or effect modifiers) school-based energy-balance interventions, Yildirim et al. (Reference Yildirim, Van Stralen and Chinapaw17) found that household socio-economic status did not significantly modify the effect of such interventions, though it was not an often-studied moderator. McGill et al. (Reference McGill, Anwar and Orton18) conducted a systematic review focused on determining if interventions promoting healthy eating were equally effective across the socio-economic spectrum. They found that ‘price’ interventions (including food taxation, food subsidies or other economic incentives) were more effective at improving healthy eating outcomes among low-income households, whereas ‘person’ interventions (focused primarily on nutrition education) were more beneficial as household income increased(Reference McGill, Anwar and Orton18). These observations are not surprising given that family income has been shown to play an important role in the causal mechanisms by which social factors influence health(Reference Marmot19).
As for neighbourhood poverty, we hypothesised that children living in the poorest neighbourhoods would benefit the most in terms of obesity risk reduction after the WIC food package change. This hypothesis is based on multiple reports that the new WIC food package has improved the neighbourhood food environment, as in response to the WIC food package change, food stores stocked more fresh produce and whole grains(Reference Schultz, Byker Shanks and Houghtaling4). Similarly, there is evidence that stores in the poorest neighbourhoods, which are often convenience stores selling mostly high-fat, high-sugar foods, improved the most to be able to keep their WIC authorisation(Reference Andreyeva, Luedicke and Middleton20). Further, there have been several large initiatives established in Los Angeles County to support changes in the food environment, such as the Healthy Eating and Active Communities initiative funded by the California Endowment(Reference Samuels, Craypo and Boyle21) and the Healthy Eating and Active Living initiative funded by Kaiser Permanente(22). While neighbourhood poverty did not significantly modify the association between the new WIC food package and obesity, we found that boys, but not girls, living in neighbourhoods with 50 % poverty experienced the largest obesity risk reductions (20–23 %) when receiving the new food package compared with the old. This is not the first time we have reported sex patterning of our results(Reference Chaparro, Anderson and Crespi13); reasons for this and previously identified sex differences could not be fully explained with the available data and thus warrant further study. Previous studies do support the notion that neighbourhoods may affect boys and girls differently, with the effects varying based on the neighbourhood characteristics and the outcomes under study(Reference Leventhal and Brooks-Gunn23,Reference Chaparro, Bilfield and Theall24) .
The current study has several strengths and limitations. Strengths include the use of a well-characterised sample, including children who participated in WIC between 2003 and 2016. Sample matching was used to minimise the impact of secular trends and confounding, as the characteristics of WIC-participating families have changed over time and other larger changes (e.g., Great Recession) occurred in the studied time frame. The Great Recession may explain why WIC participants were more likely to live in poorer neighbourhoods after the WIC food package change compared with before; however, we are unable to test this hypothesis given our data. Sample matching reduced our sample size and thus our power to detect associations. Our sample was predominantly Hispanic, given that we restricted our sample to children who participated in WIC from birth until their fifth birthday and Hispanic families are more likely to participate in WIC for longer. Thus, our results may not be generalisable to other WIC populations unless they are also largely composed of Hispanics. Moreover, our study did not involve randomisation or a control group of WIC-eligible, non-participating children, so our results cannot be interpreted as causal. It is important to point out, though, that WIC in Los Angeles County currently reaches over half of all children 1–5 years(25), so finding a control group of children who have never been in WIC is extremely difficult.
Conclusions
The new WIC food package was associated with lower child obesity risk across families in all low-income strata. Neither family income nor neighbourhood poverty significantly modified the association between the new WIC food package and obesity risk among WIC-participating children in Los Angeles County. The current study adds to the mounting evidence of the beneficial impacts of the current WIC food package on dietary behaviours and obesity-related outcomes. Implementation of further changes to the WIC food package as recommended by an expert panel in 2017(26) – including additional cash value for fruits and vegetables; further reductions of juice, milk and peanut butter; and reduction in amounts of jarred infant food – should be prioritised in order to maximise the health benefits of WIC participation.
Acknowledgements
Acknowledgements: The data used in this project are collected with the support of First 5 LA, a child advocacy and grant-making organisation created by California voters to invest Proposition 10 tobacco taxes to improve the lives of children from prenatal to age 5 years in Los Angeles County. Financial support: This research was funded by the American Heart Association’s Scientist Development Grant to M. Pia Chaparro (grant no. 17SDG33660878). Conflict of interest: None. Authorship: M.P.C., S.E.W., M.C.W. and C.M.C. conceptualised the study and secured funding. M.P.C. and C.E.A. conducted the data management and analysis under the supervision of C.M.C. All authors aided in the interpretation of results. M.P.C. wrote the manuscript. S.E.W., C.E.A., M.C.W. and C.M.C. edited the manuscript. All authors approved the manuscript for submission. Ethics of human subject participation: The current study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving research study participants were approved by the UCLA Office of the Human Research Protection Program (OHRPP; IRB# 17–000920). The current study is based on deidentified administrative data; thus, participant consent was not sought.






