Weight bias is widespread and poses a significant threat to both physical and psychological health, yet is under recognised as a public health issue(Reference Alimoradi, Golbonia and Griffiths1–Reference Hunger, Major and Blodorn4). Experiencing weight stigma is physiologically stressful, undermines the self-regulation resources needed to engage in health-promoting behaviours and contributes to poor mental health outcomes such as depression, anxiety, substance abuse and eating disorders(Reference Alimoradi, Golbonia and Griffiths1–Reference Hunger, Major and Blodorn4). Despite research highlighting the complexity of the biological, genetic and sociocultural factors influencing weight, as well as the physiological adaptions following weight loss that promote weight regain, public health messages often focus on personal responsibility and frame weight as highly controllable(Reference Puhl and Heuer3). Such messaging perpetuates negative weight-based stereotypes and, thereby, threatens core ethical and humanistic public health values(Reference Puhl and Heuer3,Reference O’Hara and Gregg5) and ultimately harms the intended recipients of the public health message.
The presence of weight bias among healthcare trainees and professionals across a range of disciplines has been well described(Reference Phelan, Burgess and Yeazel6). To our knowledge, however, no research to date has examined weight bias among the public health workforce. Understanding beliefs about the controllability of weight among public health trainees could inform workforce development initiatives that aim to reduce weight bias in public health practice. Furthermore, characterising the extent to which public health trainees internalise weight-biased beliefs could provide insight into how exposure to weight-biased content during training may negatively impact the trainees themselves. Accordingly, the aim of this study was to explore explicit beliefs about the controllability of obesity and the internalisation of negative weight-related stereotypes among public health trainees.
Methods
Participants were students of all levels at a Council on Education for Public Health-accredited School of Public Health at a large, Midwestern University. In October 2019, students were invited to complete a Qualtrics survey examining ‘beliefs and experiences of public health students on nutrition-related topics such as weight bias and food insecurity’ via emails from school-wide listservs. Students who completed the survey were entered to win one of fifty $25 gift cards. Only students who indicated they were 18 years of age or older and those who agreed their data could be reported were included in the analysis.
Participants completed the Beliefs About Obese Persons Scale (BAOP)(Reference Allison, Basile and Yuker7), an eight-item measure designed to assess explicit beliefs about causes and controllability of obesity. The BAOP uses a six-point scale (–3 to 3, not including 0), with a possible score range of 0–48 (items summed plus 24) and higher scores indicating a stronger belief that obesity is not within the control of the individual. To examine how beliefs about negative weight-related societal stereotypes apply to oneself, participants completed a modified version of the eleven-item Weight Bias Internalization Scale (WBIS-M)(Reference Pearl and Puhl8), which is applicable to individuals across different body weight statuses. The WBIS-M uses a seven-point scale (1–7) that is averaged (possible score range of 1–7) with higher scores representing greater internalisation of weight bias. Students also provided responses to demographic questions assessing self-identified gender, race/ethnicity, perceived weight status, risk of food insecurity using two-items adapted from the USDA Core Food Security Module(Reference Gundersen, Engelhard and Crumbaugh9), degree programme and academic department. Bivariate associations between BAOP and WBIS-M scores and demographic characteristics were examined using t tests or ANOVA with post hoc Tukey’s tests.
Results
Among the 322 students in our analytic sample, the mean (sd; range) BAOP and WBIS-M scores were 22·89 (7·79; 6·0–42·0) and 3·12 (1·39; 1·0–7·0), respectively. Internal consistency of the BAOP in this sample was acceptable (α = 0·72), and the internal consistency of the WBIS-M was excellent (α = 0·93).
Descriptive characteristics of the sample and results of bivariate analyses are shown in Table 1. We observed significant differences in BAOP and WBIS-M scores according to gender. Relative to students who identified as male, those who identified as female had a stronger belief that obesity is not within the control of the individual (BAOP: 23·25 v. 20·68, P = 0·03), yet had more internalisation of weight bias (WBIS-M: 3·19 v. 2·63, P < 0·01). Greater internalisation of weight bias was also seen among students who perceived themselves to be of a higher weight status (4·12 v. 2·74, P < 0·001) and those who were at risk for food insecurity (3·53 v. 3·02, P < 0·01). No significant differences in BAOP or WBIS-M scores were seen according to race/ethnicity.
Table 1 Sample characteristics and bivariate associations with controllability of obesity and weight bias internalisation (n 322)
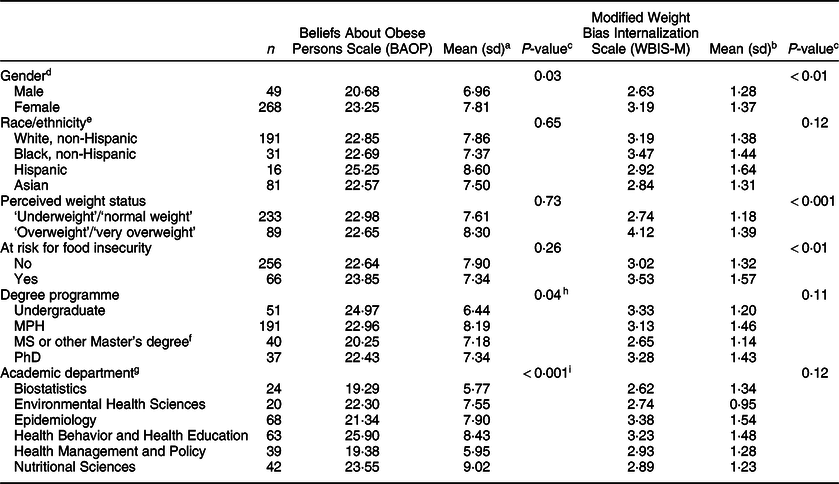
a Higher BAOP scores represent the belief that obesity is not within the control of the individual.
b Higher WBIS scores represent greater internalisation of weight bias.
c Bivariate associations between BAOP and WBIS-M scores and demographic characteristics were examined using t tests or ANOVA.
d To protect the anonymity of the small number of students who identified as a gender other than male or female (n 5), mean BAOP and WBIS-M scores for this group are not reported and are excluded from the bivariate analyses for gender.
e Students who wrote in their race/ethnicity as Middle-Eastern were classified as White, non-Hispanic; students who indicated they were both White/Caucasian and Hispanic were classified as Hispanic; students who indicated they were both White/Caucasian and Asian were classified as Asian.
f Other Master’s degrees included students in the Master of Health Services Administration and Master of Health Informatics degree programmes.
g Students from ‘other’ academic departments, including those in multiple departments and in the online MPH program, and those in the undergraduate programme were excluded from the bivariate analyses for academic department.
h Post hoc Tukey’s tests show a significant difference in BAOP scores among students in the undergraduate public health programme relative to those pursuing an MS or ‘other’ Master’s degree; no other significant differences between groups were observed.
i Post hoc Tukey’s tests show significant differences in BAOP scores among students studying Epidemiology, Health Management and Policy, and Biostatistics relative to those studying Health Behavior and Health Education; no other significant differences between groups were observed.
We observed significant differences in beliefs about the controllability of obesity according to degree programme (P = 0·04) and across academic departments (P < 0·001), with post hoc tests revealing a stronger belief that obesity is not within the control of the individual among students in the undergraduate public health programme (relative to those pursuing a MS or ‘other’ Master’s degree) and students studying Health Behavior and Health Education (relative to those studying Epidemiology, Health Management and Policy and Biostatistics). There were no significant differences in weight bias internalisation across programme or department.
Discussion
Among public health trainees, we observed differences in beliefs about the controllability of obesity according to gender, degree programme and academic department. Higher weight bias internalisation was seen among students who identified as female, those who perceived themselves to have a high weight status and those who were food insecure.
Findings from the present study should be considered relative to the literature documenting weight bias among other healthcare trainees and the general population. Mean BAOP scores in our sample of public health trainees (22·9) indicated a stronger belief that obesity is driven by genetic/environmental causes, as opposed to a lack of personal control, relative to a study of student nurses (17·4) in Turkey(Reference Yılmaz and Yabancı Ayhan10), a Mexican study of psychology (18·6) and medical (16·6) students(Reference Soto, Armendariz-Anguiano and Bacardí-Gascón11) and a study of nursing students (17·2) at a US university(Reference Darling and Atav12). Scores were similar to those seen among social work students (23·9) in the same US-based study(Reference Darling and Atav12). This finding may reflect qualities of students who choose to study public health v. other health-related careers, such as a natural orientation towards population level v. individual approaches to health promotion. Public health students also appear to be more likely to recognise genetic/environmental drivers of obesity than the general population. The original reliability study of the BAOP reported mean scores of 16·7 and 14·8 among undergraduate and graduate students, respectively(Reference Allison, Basile and Yuker7), and a general sample of college-aged students in the United Kingdom reported a mean BAOP score of 14·2(Reference Flint, Hudson and Lavallee13). WBIS-M scores in our sample were similar to those reported in a large study of undergraduate university students from Australia, in which students with higher body weights and female students were particularly vulnerable to weight bias internalisation(Reference O’Brien, Latner and Puhl14). The observed relationship between perceived weight status and internalisation of weight bias is consistent with past literature documenting that weight perception is related to susceptibility to weight bias(Reference Lin, Latner and Fung15,Reference Major, Hunger and Bunyan16) and related outcomes such as disordered eating(Reference Isomaa, Isomaa and Marttunen17–Reference Hazzard, Hahn and Sonneville19). Our observation that students at risk for food insecurity had higher WBIS-M scores aligns with a previous study where food insecurity was associated with greater weight self-stigma among adult food bank clients(Reference Becker, Middlemass and Taylor20). Because only public health trainees were recruited for this study, we were unable to directly compare beliefs of public health trainees with the general population. This limitation should be addressed in future studies.
This study was conducted among public health trainees at a single university and, as participation was voluntary, was susceptible to response bias. While these limitations impact the generalisability of our findings, this study is the first of its kind to examine weight bias among public health trainees and provides a foundation for future work examining approaches to address weight bias within public health training and practice. Findings from this study suggest that public health trainees may be more attuned to the complexities of weight relative to trainees in other health-related fields, but are still susceptible to internalisation of harmful weight-biased beliefs.
Overall, there is limited evidence for effective approaches to reduce weight bias, in part due to the paucity of research efforts in this area(Reference Daníelsdóttir, O’Brien and Ciao21), highlighting the need for the development and rigorous testing of intervention strategies that target public health trainees. Significant improvement in explicit attitudes and beliefs towards people with obesity was seen in a study of trainee healthcare professionals who viewed brief, educational films that used a range of strategies to promote stigma reduction (e.g. attributions of weight controllability, empathy induction and debunking weight-based stereotypes)(Reference Swift, Tischler and Markham22). Another recent study conducted among medical students showed that favourable interactions with higher-weight patients were significantly associated with less negative attitudes towards them(Reference Meadows, Higgs and Burke23). These studies underscore the importance of using a range of strategies to address issues of weight bias among public health trainees. Course offerings or school-wide initiatives that raise awareness of size diversity or weight-inclusive health promotion, particularly those that centre individuals with lived experience, could be leveraged to reduce the internalisation of weight bias among the most vulnerable students (e.g. those with higher body weights). To help prepare the next generation of practitioners and scholars to effectively work with individuals with higher body weights, content on the multi-factorial aetiology of weight and on the harms of weight bias could be incorporated into foundational public health coursework.
Acknowledgements
Acknowledgements: The authors wish to thank the Diversity, Equity, and Inclusion Committee in the Department of Nutritional Sciences for their support and valuable input. Financial support: The authors have no financial relationships relevant to this article to disclose. Conflict of interest: The authors have no conflicts of interest to disclose. Authorship: K.R.S. oversaw the study; K.L.R./N.J.L./C.W.L. contributed to the design of the study; K.L.R. oversaw data collection; H.M.W. led data analyses; K.R.S./K.L.R. led the writing of the manuscript; N.J.L./M.R.B./H.M.W./C.W.L. contributed to the interpretation of the results and provided critical feedback on the manuscript. Ethics of human subject participation: This study was conducted according to the guidelines laid down in the Declaration of Helsinki. The study was deemed exempt by the University of Michigan Institutional Review Board.




