Worldwide, there have been increasing concerns about hypovitaminosis D with high rates of deficiency reported in both developing and developed countries(Reference Holick and Chen1). Infantile rickets and osteomalacia are re-emerging throughout the United Kingdom, Northern Europe, USA, Saudi Arabia(Reference Allgrove2–Reference Plotnikoff and Quigley4), and even in temperate and sub-tropical countries like New Zealand and Australia(Reference Blok, Grant, McNeil and Reid5–Reference Robinson, Hogler, Craig, Verge, Walker, Piper, Woodhead, Cowell and Ambler7).
New Zealand lies in the South Pacific between the latitudes of 34oS and 47oS(Reference Bradley8), and has very high levels of solar radiation during summer(9). However, there is increasing evidence of widespread hypovitaminosis D, with some ethnic groups appearing to be at higher risk(Reference Rockell, Green and Skeaff10–Reference Rockell, Skeaff, Williams and Green12).
Over the last decade, immigration to New Zealand from the Indian sub-continent and Sri Lanka, generally referred to as South Asia, has more than doubled. According to the 2006 census, the number of people of South Asian origin now living in New Zealand is over 113 000 and the majority (70 %) are resident in Auckland(13). There have been similar patterns of migration from India into Australia(14). To date there has been no assessment of the vitamin D status of South Asians living in New Zealand.
The potential consequences of inadequate vitamin D are now known to extend beyond poor bone health. Vitamin D deficiency has been implicated in age-related muscle loss and the development of sarcopenia(Reference Visser, Deeg and Lips15), cancer(Reference Grant16), CVD(Reference Wang, Pencina and Booth17), auto-immune conditions(Reference Munger, Zhang, O’Reilly, Hernán, Olek, Willett and Ascherio18, Reference Hyppönen, Läärä, Reunanen, Järvelin and Virtanen19) and type 2 diabetes(Reference Borissova, Tankova, Kirilov, Dakovska and Kovacheva20). In New Zealand, the prevalence of some of these diseases in South Asians is considerably higher than that of the general population. The 2006 Asian Health Chart Book(21), the first comprehensive survey of the health of Asian people living in New Zealand, documents self-reported incidence of type 2 diabetes in the South Asian population as being three times the national average, and hospitalisation and mortality due to CVD or IHD as approximately double.
Aim
The aim of the present study was to determine the vitamin D status of women of South Asian origin living in Auckland, New Zealand, and to investigate their attitudes and behaviours with regard to sun exposure.
Method
The methodology is reported in greater detail elsewhere(Reference Von Hurst, Stonehouse, Matthys, Conlon, Kruger and Coad22). In brief, the study was promoted in media intended for an Indian and South Asian audience, as well as through community groups, temples and local medical centres. Exclusion criteria included taking a prescription dose of cholecalciferol (>1000 IU/d) or any supplementation with 1,25(OH)2D3, major systemic illness, chronic kidney disease, diabetes, <20 years of age. Ethnicity was confirmed with a questionnaire which established country of birth for subject, her parents and all grandparents. Demographic information, medical history, nutritional supplement and medication use were obtained by interviewer-based questionnaires.
Screening commenced in February 2007 (NZ summer) and continued through the winter into early spring. To test the effect of seasonal variation on vitamin D status, the screening period was divided into seasons: February and March were deemed to be summer; April and May, autumn; June to August, winter; and September to November, spring. Serum 25(OH)D was measured using a DiaSorin double antibody radio-immunoassay. Participants were asked to complete a web-based questionnaire about attitudes and behaviours relating to sun exposure and health motivation. The six health motivation questions were a sub-set of a larger questionnaire, the Osteoporosis Health Belief Survey, which is subject to copyright and was used with permission of the developers(Reference Kim, Horan, Gendler and Patel23). The sun exposure questions were developed for the present study, and consisted of seven statements with pre-set response options plus a section for free comments. These questions were tested in a focus group of South Asian women to ensure that all options were covered, that the questions were understood, and none caused offence. Subjects were also asked to complete a 4 d food diary. These were analysed using Foodworks 2007 (Xyris Software, Queensland, Australia), New Zealand Foods Data Base.
Statistical analysis was performed using SPSS statistical software package version 15 (SPSS Inc., Chicago, IL, USA). 25(OH)D was not normally distributed, so non-parametric tests were used where applicable. The data are reported as frequencies, median (25th, 75th percentile) or mean and sd. Mann–Whitney U and Kruskal–Wallis H tests were used to compare groups, and Spearmans for correlations.
Results
The majority of participants (91 %) were from India, with 6 % from Sri Lanka and 3 % from Pakistan. These proportions reflect those reported in the 2006 census for the South Asian population(13). In all, 79 % were recent migrants, having been in New Zealand for ≤10 years. The mean age was 40·6 (sd 10·3) years. There was a high level of education reported, with 75 % having ≥15 years of education from the age of 5 years, as expected from a newly migrant population, given New Zealand’s immigration requirements for high educational standards. Of the 250 women screened for entry into the study, five were excluded for use of the 50 000 IU supplement, which is only available on doctor’s prescription; three due to illness or use of other medication; and seven due to haemolysed blood sample.
Over a period of 9 months, serum 25(OH)D samples were obtained from 235 women. Serum 25(OH)D concentrations in seven women were over 72 nmol/l and, upon further investigation, it was discovered that all these women had been taking the 50 000 IU supplement, 1–2 months prior to recruitment. The exclusion criteria precluded anyone currently taking supplements >1000 IU/d, but due to the long half-life (∼90 d) of 25(OH)D(Reference Wu, Staykova and Horne24), the 50 000 IU supplements have a longer-lasting effect than anticipated. Consequently, these seven women have not been included in the analysis below. An additional thirty-three women reported either very recent or current use of some form of vitamin D supplementation, including cod liver oil and multivitamins. The median 25(OH)D concentrations of these women was 38 (24, 59) nmol/l, significantly higher than those taking no supplements 27 (17, 40) nmol/l (P < 0·001). The dose available in the dietary supplements reported ranged from 1·2 μg (48 IU) in cod-liver oil capsules, to 10 μg (400 IU) in multivitamins.
The median serum 25(OH)D concentration of the study group (n 228) was 27·5 (18·0, 41·0) nmol/l. Only 16 % of the participants were vitamin D sufficient according to the current reference concentration of ≥50 nmol/l. In all, 43 % of the participants had concentrations less than 25 nmol/l, which are associated with reduced bone mineral density and increased risk of fracture(25). Vitamin D stores were at their peak in summer and reached the nadir by spring (Fig. 1). Median levels by season were: summer, 33·5 (25·7, 46·2) nmol/l; autumn, 27·0 (18·0, 41·0) nmol/l; winter, 18·0 (11·0, 37·0) nmol/l; and spring, 13·0 (8·5, 30·0) nmol/l. Significant differences were observed in median 25(OH)D concentration between summer and winter, and autumn and winter (Mann–Whitney test, Bonferroni adjusted; P value for multiple comparisons, significance = P < 0·01). There was a significant inverse correlation between parathyroid hormone (PTH) and serum 25(OH)D3 concentration (r = −0·372, P < 0·001), mean PTH 5·0 (2·2) pmol/l.
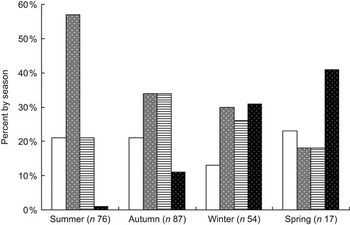
Fig. 1 Levels of deficiency or adequacy by season. Bars indicate percentage of subjects tested in that season (␣, adequate; ![]() , mild;
, mild; ![]() , moderate; █, severe). Classification of serum 25(OH)D3 levels of deficiency/sufficiency as per cut-offs from the Working Group of the Australian and New Zealand Bone and Mineral Society et al.(25): severe deficiency <12·5 nmol/l, moderate deficiency 12·5–24·9 nmol/l, mild deficiency 25·0–50 nmol/l, adequate >50 nmol/l
, moderate; █, severe). Classification of serum 25(OH)D3 levels of deficiency/sufficiency as per cut-offs from the Working Group of the Australian and New Zealand Bone and Mineral Society et al.(25): severe deficiency <12·5 nmol/l, moderate deficiency 12·5–24·9 nmol/l, mild deficiency 25·0–50 nmol/l, adequate >50 nmol/l
Despite very determined follow-up, we were able to retrieve completed food diaries from only 139 subjects. These were analysed for the dietary contribution of vitamin D. Median dietary intake of vitamin D was 0·84 (0·31, 1·89) μg/d or 33·6 (12·4, 75·6) IU/d. When dietary supplements were reported they were included in the assessment of dietary intake of vitamin D, and the maximum mean daily intake (including supplements) was 8·41 μg.
Responses from the 141 women who answered the sun exposure questions are shown in Table 1. With the exception of question 3, there was no correlation between the responses to these questions and vitamin D status. The serum vitamin D concentrations were significantly higher (P = 0·013) in the respondents who said that they ‘enjoyed spending time in the sun’ (35 (22·0, 53·7) nmol/l) compared to those who said they rarely (26·5 (18·0, 35·7) nmol/l) or never (19·5 (16·5, 27·7) nmol/l) ‘enjoyed spending time in the sun’.
Table 1 Responses to the questionnaire on attitudes and behaviour regarding sun exposure (n 140)
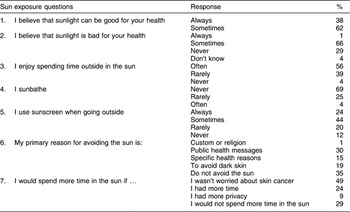
Of the sixty-nine women who chose to make further comments, 42 % remarked on the strength of the sun in New Zealand, the ozone hole and cancer risk. Five women said that they found New Zealand to be too cold, and were always covered by clothing when they went outside.
Responses to the Health Motivation section are shown in Table 2. Only statement 5, regarding having regular health check-ups, attracted a high level of disagreement (41·9 %). Internal reliability of this subsection was acceptable with a Cronbach’s α value of 0·7.
Table 2 Responses to the Health Motivation statements (n 140)

Discussion
Due to the method of participant recruitment, this is not a randomised sample. However, that 84 % were found to have less than the currently recommended level of vitamin D, suggests a problem in this particular ethnic group. There is an increased risk, not only of bone disease later in life, but also a range of other disease conditions now being linked to vitamin D deficiency. It is already acknowledged that this population group is particularly vulnerable to at least two of these diseases – type 2 diabetes and CVD(21).
As there is no fortification of the food supply with vitamin D in New Zealand, and dietary contribution of vitamin D is minimal, endogenous synthesis or supplemental vitamin D are the only realistic sources for this population. The participants who reported taking dietary supplements, either cod-liver oil, multivitamins or vitamin D packaged with calcium, were not achieving recommended serum levels. It has been shown that a supplemental dose of at least 25 μg (1000 IU)/d is required to increase serum 25(OH)D3 from levels of moderate or severe deficiency to 50 nmol/l(Reference Vieth, Chan and MacFarlane26).
It would seem that South Asian women living in New Zealand are not getting sufficient sun exposure to synthesise adequate levels of vitamin D. Concerns about the strength of the New Zealand sun and the risk of skin cancer were the most prevalent reasons for avoiding sun. Although 29 % of respondents said that they would not spend more time in the sun, 49 % indicated they would spend more time in sun if they were not afraid of skin cancer.
In a small, qualitative study in a group of South Asian women (n 23) living in Auckland, Pettit (2007)(Reference Pettit27) also found a high awareness of the risks of sun exposure in New Zealand, and of the sun safety messages which flood the media throughout spring and summer. She argues that this high level of awareness has resulted in a heightened perception of personal risk. The responses to the Health Motivation questionnaire suggest that considerable importance is placed on being healthy and obtaining information about health risks, with 82·4 % saying that they look for new information related to health, and over 70 % following recommendations to keep healthy. Few of these women, however, indulge in pre-emptive health checks and are therefore unlikely to have their vitamin D status checked.
There is reality behind the perceptions of the stronger New Zealand sun. The global solar ultraviolet index (UVI) has been designed as a simple measure of ultraviolet radiation (UVR) at the earth’s surface(9). The UVI is a scale which predicts the maximum daily level of UVR with values of 8–10 regarded as very high, and ≥11 as extreme. Peak UVI values in the New Zealand summer can reach 14, up to 40 % higher than those at corresponding latitudes in North America. This is due, in part, to the elliptical orbit of the earth which brings it closer to the sun during the southern hemisphere summer(Reference McKenzie, Bodeker, Scott, Slusserb and Lantzc28). Lower levels of air pollution also contribute, as does the thinning of the ozone layer over New Zealand in spring(Reference Liley and McKenzie29). Although no direct comparison can be made with India, all these factors would potentiate a lower UVI in many Indian locations, especially urban areas where high levels of pollution have been shown to impact on vitamin D status in children(Reference Agarwal, Mughal, Upadhyay, Berry, Mawer and Puliyel30).
In 2005, the Sunsmart™ Partnership published a position statement on the Risks and Benefits of Sun Exposure in New Zealand. This document acknowledges the health implications of too little sun exposure, but states, ‘There is no evidence that the sun protection messages promoted in New Zealand have affected vitamin D levels’(31). More recently, the Cancer Society of New Zealand (2008) has announced plans to develop a range of healthy sun exposure messages, that take into account season, skin type, time of day and related research findings as they emerge(32). Since late 2007 there has been an information sheet on the Cancer Society web site about sun exposure for people with dark skin(33).
To a lesser degree, lifestyle, cultural and personal appearance reasons also featured as reasons to avoid the sun. A number of women commented on long work hours, working in an office, and driving to and from work. Of the respondents, 24 % said that they would spend more time in the sun if they had more time. Pettit also found that amongst the married women in her study, time and opportunity were important constraints(Reference Pettit27).
Despite the seasonal variation, the majority were still failing to reach concentrations >50 nmol/l, even those tested at the end of summer. An assessment of serum 25(OH)D concentrations in the New Zealand population also showed seasonal variation with a difference (in women) of 31 nmol/l between summer and spring(Reference Rockell, Skeaff, Williams and Green12). Above latitudes of 40o it is not possible to make vitamin D during winter, and 25(OH)D levels in summer can be 20–120 % higher(Reference Porojnicu, Robsahm, Dahlback, Berg, Christiani, Bruland and Moan34).
Low levels of vitamin D have been seen in other migrant South Asian populations in Denmark and Britain(Reference Andersen, Mølgaard, Skovgaard, Brot, Cashman, Jakobsen, Lamberg-Allardt and Ovesen35, Reference Roy, Berry, Pye, Adams, Swarbrick, King, Silman and O’Neill36); however, these populations were subject to much lower UVI than the present study population in Auckland, New Zealand. It is probably more useful to compare the vitamin D levels of these South Asian women to other brown-skinned ethnic groups in New Zealand. Rockell et al. (Reference Rockell, Skeaff, Williams and Green12) found the mean 25(OH)D concentration in New Zealand, European and other women (adjusted for age, ethnicity, season, region and BMI) to be 49 nmol/l, compared to Maori women at 38 nmol/l and Pacific women at 33 nmol/l. Mean serum vitamin D concentration in participants of the present study was 32 (19) nmol/l.
There is currently much debate around the use of 50 nmol/l as the cut-off for sufficiency, and scientists working in vitamin D research have recently called for this minimum to be raised to 80 nmol/l(Reference Vieth, Bischoff-Ferrari and Boucher37). None of the participants in the present study met that criterion for adequacy.
In conclusion, the present study shows that we can no longer afford to assume that vitamin D levels in the population will be concurrent with environmental UVR. Some groups, such as South Asians, are at higher risk of hypovitaminosis D, due, in part, to deliberate avoidance of sun exposure, a lifestyle that allows little or no incidental sun exposure, and lack of fortification of the food supply. Such groups are especially vulnerable during winter and spring.
Acknowledgements
The present study was funded by the NZ Lotteries Board from their Lotteries Health fund. P.R.H. is funded by a Massey University Doctorate Scholarship. The authors declare that there are no conflicts of interest. The authorship responsibilities are as follows: P.R.H. and J.C. conceived the study, acquired funding and ethics approval. P.R.H. coordinated recruitment, participant management and data collection. W.S. designed the laboratory protocol. P.R.H. drafted the manuscript. All authors were involved in revising the manuscript and all read and approved the final manuscript. The authors would like to thank the 239 participating women and Dr R Sood (Mount Roskill Surgical and Medical Centre), Midi Tsai, Laura King and Hymavathy Danthala (Massey University Post Graduate students).





