Childhood overweight and obesity is an increasing public health problem(Reference Jackson-Leach and Lobstein1–3). Often persisting into adulthood, childhood obesity increases the risk of suffering from a range of diseases, including diabetes mellitus and CVD, which can lead to poor quality of life and a shortened lifespan(3–Reference Peeters, Barendregt and Willekens5). Overweight among children is related to many factors at the individual, family and environmental levels.
Cross-sectional and longitudinal studies have shown a positive association between time spent watching television (TV) and an increase in the prevalence of childhood overweight and obesity(Reference Wiecha, Peterson and Ludwig6–Reference Robinson9); whereas the results of published studies indicate a positive relationship between TV viewing and overweight(Reference Chou, Rashad and Grossman10–Reference Epstein, Roemmich and Robinson12), mechanisms driving this are not clear. Two primary mechanisms by which TV viewing contributes to weight gain in children have been suggested: reduced physical activity or increased energy intake or a combination of both. Weak-to-modest inverse associations between TV viewing and physical activity have been found(Reference Robinson9, Reference Crespo, Smit and Troiano13). There is also evidence that at least part of the relationship between TV viewing and overweight in children can be linked to energy intake; that is, TV watching is associated with an increase in consumption of fast food and energy-dense snacks(Reference Wiecha, Peterson and Ludwig6, Reference Snoek, Van Strien and Janssens7, Reference Epstein, Roemmich and Robinson12). The present study focuses on the latter mechanism and will explore the potential effect of TV food advertising on childhood obesity.
There is substantial evidence that exposure to TV food advertising significantly influences children’s food preferences, choices, purchase requests and food intake, but the strength of the evidence decreases with the length of the putative causal chain from advertising to obesity(Reference Utter, Scragg and Schaaf8, Reference Crespo, Smit and Troiano13–Reference Chamberlain, Wang and Robinson17). The effects appear to be independent of other factors and operate at both brand and category level(Reference Hastings, Stead and McDermott18). Studies of TV food promotion show that the commercial marketing of food to children is dominated by unhealthy products, promoting the intake of energy-dense nutrient-poor foods. These products pose a risk of weight gain and obesity in children(3, Reference Chou, Rashad and Grossman10, 16, 19, Reference Dietz and Gortmaker20). However, research that quantifies the potential relationship between childhood overweight and TV food advertising while controlling for TV viewing time, physical activity, parental influences, non-TV-related sedentary time and other contextual factors is scarce. It is also unknown how much of the overweight and obesity in children is attributable to TV food advertising exposure at the population level.
Lobstein and Dibb(Reference Lobstein and Dibb11) found a significant association between the proportion of children with overweight and the number of food advertisements per hour on TV in several countries. The authors estimate that TV food advertising could explain up to half of the variation between the different countries’ overweight prevalence figures. However, the Lobstein and Dibb's study made use of data from 1996 on TV advertising to children in thirteen countries, based on an average of only 20 h of recording on commercial channels(Reference Lobstein and Dibb11, 21).
The contribution of TV food advertising to childhood obesity is difficult to examine directly. There is little empirical evidence that has been able to quantify the effect of TV food advertising on obesity because of its interrelatedness with sedentary behaviour, consuming snacks while watching and the influence of alternative types of marketing(Reference Powell, Szczypka and Chaloupka22). Trials in real-life situations are virtually impossible; it would require the ability to vary exposure to TV food advertising while leaving all other influences constant. We are not aware of any existing study that accomplished this.
However, the existing evidence can be used to construct a logical framework and estimate the impact of TV food advertising using mathematical models. Such models do not remove the need for studies that directly examine the effect of advertising on childhood obesity, but can usefully inform policy decisions by exploring the likely range of the effects of measures to limit children’s exposure to food advertising.
The present study builds upon earlier research in which a mathematical simulation model was used to predict the effects of reducing TV food advertising on childhood obesity in the United States, applying CDC-2000 definitions for overweight and obesity. The results suggested that one in every three to seven obese children in the United States might not have been obese in the absence of advertising for unhealthy food on TV(Reference Veerman, Van Beek and Barendregt23). However, with its high prevalence of childhood obesity and high amount of TV food advertising, the results from the United States are not directly applicable to other countries. The present study uses the same methods (except that the International Obesity Task Force (IOTF) cut-off values for overweight and obesity(Reference Cole, Bellizzi and Flegal24) are used) and applies these to a range of Western countries. The aim of the present study is therefore to quantify and compare the effect of TV food advertising on the prevalence of overweight and obesity in 6–11-year-old children in Australia, Great Britain (England and Scotland only), Italy, The Netherlands, Sweden and the United States.
Methods
On the basis of available published literature and other reviews(Reference Lobstein and Dibb11, 19, 21, Reference Halford, Boyland and Hughes25–Reference Spagnoli, Bioletti and Bo27), three countries were selected with expected higher exposure rates of TV food advertising – Australia, United States and Great Britain (England and Scotland only) – and three countries where we expected lower exposure rates – Sweden, The Netherlands and Italy.
Overweight and obesity
A literature search was carried out using the PubMed database to identify studies in the six different countries that estimate the prevalence of overweight and obesity among 6–11-year-old children. Search terms used were ‘child’, ‘childhood’, ‘overweight’, ‘obesity’, ‘prevalence’, ‘epidemiology’ in combination with country names, and the ‘related links’ feature in PubMed. Also the IOTF archive(28) was searched. We included studies if they were published between January 2000 and January 2008, and defined overweight and obesity by BMI (kg/m2) values calculated on the basis of the measured anthropometrics. In a second phase, authors of identified studies were contacted and asked for detailed data on overweight and obesity prevalence rates as well as mean weight and height by age and sex.
In every country, boys and girls were modelled separately in 1-year age categories by fitting the measured prevalence of BMI in the current situation to a log-normal distribution with intercept, using the least squares method. In Fig. 1, the continuous lines illustrate the results for 11-year-old boys. The international reference values of Cole et al.(Reference Cole, Bellizzi and Flegal24) were applied to determine the prevalence of overweight and obesity.

Fig. 1 (a)–(f) Modelled BMI distributions of 11-year-old boys. Illustrations of modelled BMI distributions of 11-year-old boys in all countries are shown. The continuous line denotes the current situation, the dotted line represents the hypothetical distribution in the absence of television food advertising as modelled in the Delphi scenario. The vertical lines indicate the age- and sex-specific cut-off points for overweight and obesity
Television food advertising exposure
Studies on TV food advertising exposure in the six countries were identified through searches of the PubMed database. Search terms used were ‘child’, ‘marketing’, ‘TV’, ‘food’, ‘advertising’ in combination with country names, and the ‘related links’ feature in PubMed. We included studies on TV food advertising if they were published between January 2000 and March 2008. No nationally representative studies that used a standard methodology of data collection were found. Where possible, direct estimates of TV food advertising were used and when not available an average exposure of children to TV food advertising was estimated by combining studies that provided data on the number of TV food and drink-related advertisements per hour during children’s viewing time and data on viewing patterns from national media and broadcasting organisations. In case exposure time was not available but studies did report the number of advertisements, we assumed that the average duration of a TV food commercial is 30 s. This was verified with the authors of each study as a reasonable estimate.
Analysis
The effect of TV food advertising on the prevalence of overweight and obesity was estimated using the mathematical simulation model that was developed for the study that focused on the United States mentioned above(Reference Veerman, Van Beek and Barendregt23). Two counterfactual scenarios – the ‘Bolton’ and the ‘Delphi’ – for overweight and obesity after removing all exposure to TV food advertising are modelled. The prevalence of overweight and obesity in each of these scenarios was compared to the prevalence as calculated above (‘current situation’ scenario). For each country, the data on BMI distribution and mean weight and height for age by sex, combined with data on TV food advertising exposure, were entered into the model.
The estimation of overweight and obesity prevalence in the counterfactual (no food advertising) scenarios consists of three steps. First, the level of exposure to TV food advertising determines the total daily energy intake. We used two alternative methods for this step: one based directly on the literature (‘Bolton scenario’), and the other based on expert opinion (‘Delphi scenario’). Bolton(Reference Bolton29) estimated that a weekly increase of 25 min of TV food advertising exposure would increase the energy intake by approximately 1·4 %. This value was replaced with 3·5 % in a parallel analysis based on expert opinion obtained in a Delphi study. In the Delphi study, eight (out of thirty-three) researchers who had recently published on the topic, or whom we knew to be knowledgeable, provided their estimate of the effect of TV food advertising exposure on energy consumption(Reference Veerman, Van Beek and Barendregt23).
Second, a change in energy intake results in change in the average body weight and (thus) BMI. The model applied Swinburn et al.’s(Reference Swinburn, Jolley and Kremer30) estimate that two populations with a 10 % difference in mean ‘EnFlux’ (balance energy expenditure = energy intake) would have a 4·5 % (95 % CI 3·8 %, 5·1 %) difference in mean weight.
Third, a new log-normal BMI distribution is modelled based on the new (lower) mean BMI. We first derived the mean BMI from the log-normal distributions in the ‘current situation’ scenario. We then derived the average weight for each age and sex group, and changed this by the percentage that resulted from the previous two steps. Next, assuming the height stable, mean weight was converted back to a new mean BMI value. Assuming the ‘sigma’ parameter and the intercept of the log-normal distribution stable and changing only the ‘mu’ variable now allowed deriving the shape of the counterfactual BMI distribution (Figs 1(a) to (f) provide graphical examples). The new BMI distributions had a reduced spread and rightward skew, which means that the section of the population with the highest BMI values are disproportionately affected. The methods have been described in more detail elsewhere(Reference Veerman, Van Beek and Barendregt23, Reference Flegal and Troiano31).
In the Bolton scenario, 95 % uncertainty intervals (UI) around the outcomes were calculated by varying the relationship between the number of kJ consumed and body mass to reflect the 95 % CI of the source study(Reference Swinburn, Jolley and Kremer30). (UI are comparable to CI, but incorporate uncertainty from various – not necessarily statistical – sources.) In the Delphi scenario, simultaneous parametric and non-parametric bootstrapping (5000 iterations) was applied to estimate the combined uncertainty in relationship between the number of kJ consumed and body mass and the relationship between advertising and BMI as estimated by the Delphi panel(Reference Efron and Tibshirani32). Calculations were carried out in MS Excel; bootstrapping with the Ersatz add-in (Ersatz 1·0; EpiGear, Brisbane, Australia).
Reductions in the prevalence of overweight and obesity were calculated by dividing the difference in prevalence rates between the counterfactual Bolton and Delphi scenarios and the observed prevalence rates (‘current situation’ scenario) on the observed prevalence. This results in estimates of the proportion of currently overweight/obese children that would not have been obese in the absence of TV food advertising.
Results
Prevalence of childhood overweight and obesity
Nine cross-sectional studies that examined the prevalence of overweight and obesity in children aged 6–11 years were identified. Two studies were excluded; one because it was a small study including one city only(Reference Vignolo, Pistorio and Torrisi33) and another because the author did not respond to our request for data(Reference O’Dea34). Thus, seven studies were available for analysis. Nationally representative data were available only for the United States and Great Britain (England and Scotland only). For the other participating countries, studies based on regional surveys were used under the assumption that these provide the best approximation of the situation in these countries (Table 1).
Table 1 Selected studies on the prevalence of childhood overweight and obesity
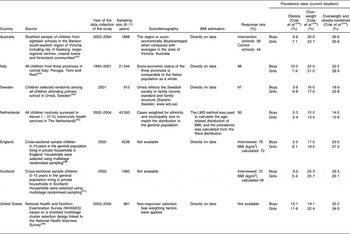
The lowest prevalence rates of childhood overweight/obesity were found in The Netherlands and Sweden; Great Britain had a high prevalence rate of overweight/obesity particularly for boys in Scotland and for girls in England. Italy had a high overweight/obesity prevalence rate for boys and Australia had a high prevalence rate particularly for girls. The highest overweight/obesity prevalence rates for both girls and boys were found in the United States (Table 1).
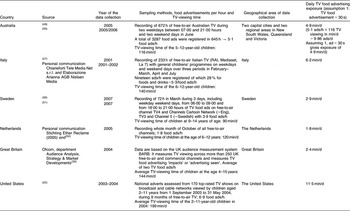
Exposure to television food advertising
For the United States, a comprehensive study by Powell et al.(Reference Powell, Szczypka and Chaloupka22) provided a direct estimate of TV food advertising exposure in 2003–2004 in min/d. The UK Ofcom report(35) provided data on TV food impacts or TV food advertisements actually seen in Great Britain during 2004. For all other countries, we combined studies that provided data on TV food advertisements and TV-viewing patterns monitored between February 2001 and March 2007. TV food advertising exposure was found to be highest in the United States and lowest in The Netherlands, Sweden and Great Britain, while Italy and Australia took intermediate positions (Table 2). TV viewing and food advertising exposure data used in this study were from before the introduction of advertising restrictions to children in most countries. The average daily TV viewing time in 6–11-year-old children was found to be 90 min/d in Sweden, 116 min in Australia, 120 min in The Netherlands, 140 min in Italy, 144 min in Great Britain and 199 min/d in the United States.
Table 2 Selected studies on television food-advertising exposure
Expected changes in overweight and obesity by television food advertising
The estimated changes in overweight and obesity based on the Delphi study are more than twice as high as those based on the Bolton study (Table 3). The contribution of TV food advertising to the prevalence of childhood obesity ranks highest in the United States, where the Delphi scenario estimated that 40 % (95 % UI 23, 58 %) of obese children would not have been obese in the absence of TV food advertising. In Australian and Italian girls and boys, point estimates were 25 %–28 % and 11 %–18 % in Swedish, Dutch, English and Scottish girls and boys. The corresponding point estimates in the Bolton scenario are 16 % for American boys and girls, 10 %–11 % for Australian and Italian boys and girls and 4 %–7 % for Swedish, Dutch, English and Scottish boys and girls.
Table 3 Estimated fractions of childhood overweight and obesity prevalence attributable to television food advertising

The values represent expected relative reductions, with 95 % uncertainty intervals in brackets, in 6–11-year-old children.
Discussion
Our study attempted to quantify the effect of exposure to TV food and drink advertising on the prevalence of overweight and obesity among 6–11-year-old children by making use of a mathematical simulation model and data from published sources. The results presented suggest a noticeable effect of TV food advertising exposure on the prevalence of overweight and obesity in all six countries. The country with the highest overweight and obesity prevalence rates among children 6–11 years (the United States) also had the highest exposure to TV food advertising (Tables 1 and 2). Italy had an intermediate TV food advertising exposure rate, but the highest overweight prevalence rate for boys. Australia also had an intermediate TV food advertising exposure rate but the highest prevalence rate for overweight in girls. The two countries with the lowest TV food advertising rates, The Netherlands and Sweden, also had the lowest prevalence rates childhood overweight and obesity. Great Britain was an exception in having a low exposure to TV food advertising but high prevalence rates of overweight and obesity, particularly for boys in Scotland and for girls in England.
Comparison with other studies
Our study results confirm the findings of an ecological study by Lobstein and Dibb(Reference Lobstein and Dibb11) who found a significant association between the proportion of children with overweight and the number of advertisements per hour on children’s TV in different countries. It is also consistent with a recent econometric study that estimated that a ban on TV fast food advertising in the United States would reduce the prevalence of overweight among children 3–11 years old by 18 %(Reference Chou, Rashad and Grossman10). However, the findings for Australia, Italy, Scotland and England are not fully in line with the findings for The Netherlands, Sweden and the United States. An explanation might be that the studies used were not representative of the TV food advertising exposure in those countries or TV food advertising occurred through other types of marketing on TV, such as product placement, a commercial product or brand used as an integral part of a TV programme and famous personalities or cartoon characters.
Policy implications
Our study results suggest that limiting TV food advertising exposure may lead to significant reductions in the prevalence of childhood overweight and obesity.
As a result of public action and lobbying of health bodies, the majority of European countries, the United States and Australia have been trying to persuade the food industry to voluntarily restrict promotion activities of unhealthy foods through responsible self-regulation(19, Reference Caraher, Landon and Dalmeny36). Such measures were introduced by the food industry in Australia in January 2009(37), in the United States in July 2007(38) and in the United Kingdom by media regulator Ofcom in April 2007 and January 2008(3). In Sweden, all broadcast advertising aimed at children under the age of 12 years has been banned since 1991 as a measure to protect the rights of children. However, the effectiveness of this ban is undermined by commercials on cable and satellite TV broadcast from other countries, for example, from the United Kingdom. European legislation prevents Sweden from stopping this advertising(19, 26). Do initiatives to reduce food advertising make an impact? According to the UK Department of Health report 2008(39), the annual spend for child-themed TV food advertisements decreased by 41 %, but spending for food advertising across all media increased by 19 % between 2003 and 2007(39). As has been shown for tobacco advertising, bans may have to cover multiple advertising channels to achieve optimal effects(Reference Saffer40). The effectiveness of efforts to stimulate industry self-regulation is also uncertain. Caraher et al.(Reference Caraher, Landon and Dalmeny36) found large differences in the enforcement and monitoring of self-regulation in twenty countries and a lack of representation of public health and consumer groups on industry self-regulating bodies. Control and regulation can be implemented regionally, as some states in Australia are considering, but preferably need to be addressed at the national or international level. In 2008, the IOTF presented the ‘Sydney Principles’ that call for international statutory actions to reduce marketing to children and the development of an International Code of Marketing Food and Beverages to Children(Reference Swinburn, Sacks and Lobstein41). According to these principles, such statutory regulations should have sufficient authority, be enforced and evaluated for their impact on children’s dietary patterns(Reference Swinburn, Sacks and Lobstein41).
Recommendations for future research
Estimates of the impact of TV food advertising on childhood obesity cannot be better than the data they are based on. There is an urgent need for more nationally representative data on the prevalence of overweight and obesity in children, in the countries studied and beyond. Similarly, there is a need for nationally representative studies on food advertising exposure on TV that use comparable methods.
Strengths and limitations
This study provides the first estimate of the effect of TV food advertising on the prevalence of childhood overweight and obesity in six Western countries on the basis of the best available evidence. The study also provides a comparison of TV-viewing data and advertising exposure in these countries.
However, the present results should be regarded as approximations of the effect of TV food advertising on the prevalence of overweight and obesity. First, the results are mostly based on BMI data from published smaller and/or localised surveys, as apart from the United States and the British studies, there were no recent national surveys available. The limited representativeness of the BMI data may have introduced bias in an unknown direction. We could only include published data, but the risk of publication bias is limited by the fact that we were looking for the largest, most representative studies, which are most likely to be published. The comparability between countries is slightly diminished by the differing dates of data collection, though, except for the Italian sample, all data were collected between 2001 and 2004. Assuming increasing trends in obesity, the more recent data probably have the highest prevalence overweight/obesity. If the prevalence of obesity is underestimated in these data, our study overestimates the proportion of childhood obesity that is attributable to TV food advertising (however a higher absolute number of children would be affected).
Second, there is no agreed gold standard method for measures of TV food advertising exposure and we therefore had to make use of the best available information. For some countries direct estimates were available, for other estimates based on national TV-viewing patterns were combined with individual studies. Data collection of these studies was between February 2001 and March 2007; differences in the year of data collection may have reduced comparability.
Third, the real quantity of interest is exposure to TV food advertising for energy-dense and nutrient-poor foods and not for foods and drinks in general. However, such detailed advertising data are rarely available and if they were, they could not have been used in the absence of studies that quantify the effect of advertising for different food product groups on BMI.
A fourth uncertain factor is the exposure–response relationship between TV food advertising and total energy intake. The only estimate we found in the literature was the Bolton study(Reference Bolton29). In addition, an expert panel was asked to estimate the same relationship in a Delphi study(Reference Veerman, Van Beek and Barendregt23). Both methods have their limitations. The Bolton study uses data from the United States in 1977, a context that may not be representative for the populations we applied it to. The effect of TV food advertising may be confounded with eating snacks while watching TV (regardless of advertising), since the time children were exposed to TV food advertising was not adjusted for the time spent watching TV. However, the Bolton study may have underestimated the effect of TV food advertising since it adjusts for parental influence (rules and behaviour) while adults can also be influenced by TV food commercials. In the Delphi study, a response rate of 24 % and self-selection bias may have led to an overestimation of the effect of advertising.
A fifth limitation concerns the timing of the impact of TV food advertising. The data collection of the prevalence overweight and obesity studies and data collection of TV food advertising and TV viewing were approximately from the same period. Exposure takes place over an extended period of time and there may be a time delay between exposure and consequences. Our model did not include this potential delay effect. It is likely that the cumulative effects of TV food advertising to children are larger in the older age groups. However, sufficient data to support more precise analyses that include delayed and cumulative effects of TV food marketing to children over time was not available.
Lastly, our study only examines one marketing channel. The combined effect of all marketing for energy-dense, nutrient-poor foods is likely to be larger than the effect of TV food and drink advertising alone. Inclusion of other marketing channels was not possible due to data limitations.
Conclusion
The present study suggests that the exposure of children to advertising for foods and drinks on TV varies considerably by country, with a sixfold difference between the highest and lowest exposure in the countries studied. Reducing TV food advertising may significantly lower the prevalence of childhood overweight and obesity in some countries.
Acknowledgements
The authors thank the following persons for provision of data and other relevant information. In Australia: Dr Andrea Sanigorski and Mary Malakellis, Deakin University; Kathy Chapman, the Cancer Council NSW; Bridget Kelly, NSW Centre for Overweight and Obesity; in Italy: Dr Vittorio Bini, University of Perugia; Mr Giulio Malgara, Chiarieforti Tele Media Net s.r.l; in Sweden: Louise Ekström, Swedish Consumers’ Organisation; Dr Helena Sandberg, Lund University; in The Netherlands: Prof. Dr Stef van Buuren, TNO Kwaliteit van Leven; Stichting Ether Reclame; in Great Britain: Dr Tim Lobstein, Director Childhood Obesity Programme IASO – IOTF, Kam Atwal and Leila Agyeman, Ofcom and Marleen Kestens, European Heart Network. Sources of funding: The present study is partly funded from a University of Queensland Start-Up grant and a National Health and Medical Research Council Capacity Building Grant. The funders had no influence on the design and conduct of the study; collection, management, analysis and interpretation of the data; and preparation, review, or approval of the manuscript. Conflict of interest: The authors have no conflicts of interest to declare. Author responsibilities: J.M.G. is responsible for data collection, analysis, interpretation and writing of the manuscript; S.P. has provided the childhood overweight and obesity data, Umea study, Sweden, and commented extensively on the structure and content of the manuscript. E.S. has provided childhood overweight and obesity data England and Scotland, and commented on structure and content of the manuscript. J.L.V. developed the mathematical simulation model, supervised the development of the paper and provided advice regarding analysis, interpretation of data and structure and content of the manuscript.






