National dietary guidelines provide information about the kinds of foods the population should choose each day to promote good health( Reference Smith, Kellet and Schmerlaib 1 ). Efforts to improve nutritional status and prevent diet-related disease involve promoting food habits which are consistent with dietary guidelines. To monitor population compliance with guidelines we need to be able to measure dietary intake accurately and reliably via methods that are feasible in large research studies and population surveys.
Diet indices have been developed to allow comparisons of overall dietary intake against dietary guidelines. One Australian example is the Dietary Guideline Index for Children and Adolescents (DGI-CA)( Reference Golley, Hendrie and McNaughton 2 ). This index comprises eleven components including the five core food groups (vegetables, fruit, bread and cereals, meat and alternatives, dairy), healthy fats, water and energy-dense, nutrient-poor ‘extra foods’, as well as food choices such as choosing reduced-fat milk and wholegrain bread, and dietary variety. Importantly, the composition of the index represents all aspects of the Australian dietary guidelines( 3 ), allowing simultaneous assessment of compliance with the dietary guidelines. The development and validation of the DGI-CA score were based on food intake data averaged from two 24 h recalls( Reference Golley, Hendrie and McNaughton 2 ). In this format the DGI-CA is not appropriate for use in larger research studies or population surveys for assessing children's compliance with the guidelines.
Assessment of dietary intake is complex, and the appropriate method will depend on the measurement objectives and the dietary outcomes of interest( Reference Roberts and Flagherty 4 ). Methods such as 24 h recalls and weighed food records require trained administrators, can be time consuming and inconvenient for participants and time consuming and costly to deploy and analyse. For large research studies and population monitoring, such intensive methods of dietary assessment are not always feasible. The FFQ is a common alternative for dietary assessment as it is relatively easy to administer and less expensive than other methods, yet still can provide estimates of both food and nutrient intakes.
Foods included in FFQ may be chosen for a specific purpose (e.g. to estimate Ca intake) and may not adequately assess total diet. The number of questions included in FFQ can vary widely, up to 350 in the most comprehensive versions, but there are generally about eighty questions( Reference Cade, Thompson and Burely 5 ). A questionnaire of this length takes a considerable amount of time to complete, which has led to the emergence of shorter dietary assessment tools to measure intake. Short tools also vary in their purpose and composition. Some tools measure discrete food groups such as fruit and vegetables, while others assess total diet and cover up to fifty different foods and beverages. Few short dietary assessment tools have been validated( Reference Roberts and Flagherty 4 ). A recent review identifying tools appropriate for use in large populations found eleven tools with validation studies, six measuring children's intake( Reference Roberts and Flagherty 4 ).
Two short dietary assessment tools have been developed and validated in Australian children. The Child Nutrition Questionnaire measures food intake, attitudes, environment and knowledge of children aged 10–12 years( Reference Wilson, Magarey and Mastersson 6 ). This fourteen-item questionnaire is child-reported and covers intake of extra foods, sweetened beverages, water, fruits and vegetables. The second Australian tool is the Children's Dietary Questionnaire( Reference Magarey, Golley and Spurrier 7 ). This twenty-eight-item tool was developed to measure children's compliance with selected dietary guidelines with a focus on obesity-related food habits. The tool measures four aspects of diet: fruit and vegetables, fat from dairy foods, sweetened beverages and extra foods. The limitation with both of these examples is that only selected food groups are measured and therefore simultaneous compliance with all dietary guidelines cannot be evaluated.
Therefore, the aim of the present study was to explore the reliability and relative validity of the DGI-CA score for young children, derived using parent-reported food intake data from a newly developed Short Food Survey (SFS).
Methods
Parents of children aged 4–11 years were recruited via public advertising and word of mouth. Inclusion criteria were: parents of healthy children, living in Adelaide, Australia and willing to be involved in five assessments, with adequate written and spoken English. Parents of children with pre-existing medical conditions affecting their intake such as food allergies or intolerances were excluded. Each parent could only have one child participate. Parents provided informed written consent. The study was approved by the Commonwealth Scientific and Industrial Research Organisation's (CSIRO) Human Research Ethics Committee (11/06).
Parents were required to report their child's food intake on five different occasions (as summarised in Fig. 1). Young children have limited ability to conceptualise and recall food consumed over a period greater than one day, so parents were used as proxy reporters( Reference Livingstone and Robson 8 , Reference Livingstone, Robson and Wallace 9 ). The test method for this study was the SFS; therefore it was administered before the comparison method (24 h recall) to minimise any potential influence participation in a dietary recall would have on completing the short survey( Reference Cade, Thompson and Burely 5 ).
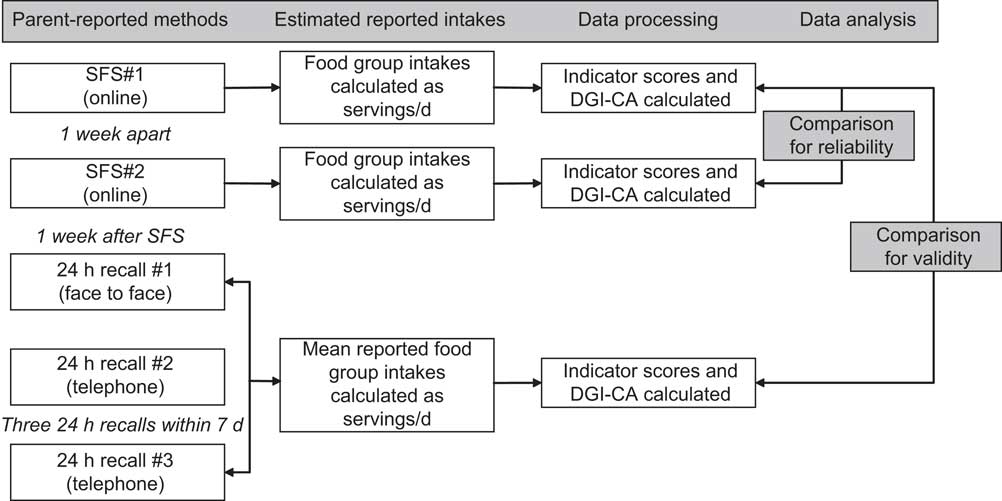
Fig. 1 Summary of the study methodology (DGI-CA, Dietary Guideline Index for Children and Adolescents; SFS, Short Food Survey)
The SFS was administered online via Survey Monkey (http://www.surveymonkey.com/). It was administered twice, approximately one week apart (mean 7 (sd 2·1) d, range 2–13 d). Following the completion of the second SFS questionnaire parents were required to attend a central city clinic on one occasion. At this visit parents completed a three-pass 24 h recall with a dietitian, as well as responding to a demographic questionnaire regarding their family circumstances (relationship, employment and education status, annual income) and child characteristics including height and weight. Parent-reported height and weight measurements are considered not to be as accurate as those that are independently measured( Reference O'Connor and Gugenheim 10 ), but measurement error for boys and girls is considered acceptable and self-report reduces the burden of participation for families. Following the clinic visit, parents completed another two 24 h recalls via telephone.
Short food survey
The SFS consisted of thirty-eight items capturing information on children's food group intakes and food choices (see Appendix). Questions were chosen to enable a DGI-CA score to be calculated from the SFS. Twenty-seven items estimated usual consumption of the five core food groups, extra foods and beverages. Core food groups were based on the national dietary guidelines( 3 ) and included fruit (two items), vegetables (three items), breads and cereals (three items), meat and alternatives (including legumes/lentils, five items) and dairy foods (three items). Extra foods included (non-core) food items such as salty savoury snacks, confectionery, soft drinks, and biscuits and cakes (eight items). Beverages included all fluids (three items) except dairy fluids (these were included in dairy) and 100 % fruit juice (included in fruit). Parents were asked to report children's usual intake, in servings, per day, week or month. The reference period was specified as over the last week in order to capture ‘usual’ short term intake, similar to the intended period captured in the multiple 24 h recalls. Four food choices questions asked about the type of milk and spread usually consumed, as well as the frequency of wholemeal/wholegrain breads and trimmed meats eaten. Seven items were related to food variety. These focused on the variety within core food groups over a defined period; for example, the number of different types of fruit eaten in the past 48 h (response options of 0 to 5+; see Appendix). The SFS was piloted with a small sample of parents (n 4) for feedback about readability, clarity and comprehension.
Twenty-four-hour recalls
In children of this age, multiple-pass, 24 h recalls (which cover at least three days, including weekdays and weekends) are considered to be a feasible and acceptable dietary assessment method of known performance against doubly labelled water( Reference Burrows, Martin and Collins 11 ). In the present study a dietitian conducted one face-to-face recall at the clinic visit, followed by two telephone recalls, scheduled within seven days and including one weekend day. Briefly, a multiple-pass recall involves developing a quick list of foods and beverages consumed on the previous day, the second pass collects detailed information on the amount, type, brand and cooking methods and the third pass allows for additional information to be recalled. Parents were provided with a food model booklet, which was adapted from the US Department of Agriculture's Food Model Booklet( 12 ) and used in the Australian National Children's Nutrition and Physical Activity Survey( 13 ). This was used during all three recalls to assist with portion size estimates. Data were entered by the research dietitian into FoodWorks Professional software version 7. Food groups were created using the hierarchy of food codes in the 2007 AUSNUT Australian food composition database( 14 ) and grams consumed was converted to reference servings based on information contained in the national food selection guide( Reference Smith, Kellet and Schmerlaib 1 ).
Calculating diet index scores
Food intake data from the SFS and the average of three 24 h recalls were converted to servings and usual food group intakes per day were calculated (Fig. 1). Daily intake was used to calculate diet quality (DGI-CA) from both the SFS and the 24 h recalls. The DGI-CA scoring criteria are described in detail elsewhere( Reference Golley, Hendrie and McNaughton 2 ). In summary, the DGI-CA comprises eleven components: five core food groups, wholegrain bread, reduced-fat dairy foods, extra foods (nutrient-poor, energy-rich foods), healthy fats/oils, water and diet variety. Usual daily intake was compared with recommendations set out in the national food selection guide( Reference Smith, Kellet and Schmerlaib 1 ) and indicator scores calculated based on the scoring criteria of the DGI-CA scoring matrix (see Appendix). Indicator scoring is such that one dietary recommendation or food group is allocated 10 points. Achievement of a maximum score indicates that an individual's intake met the recommendation or he/she had an optimal intake. Minimum scores were generally assigned to zero intakes, and in between scores were allocated as a proportion of the recommendation. The total DGI-CA score was calculated by summing the eleven indicator scores, with a total possible score of 100, and a higher score representing greater compliance with dietary guidelines.
Statistical analysis
Descriptive statistics (mean and standard deviation) are presented for food group intakes and DGI-CA indicator and total scores for the two SFS administrations and the mean of three 24 h recalls. The significance of the difference in mean estimates of intake was assessed using a paired-samples t test. Pearson correlation coefficients were calculated between the two administrations of the SFS (SFS#1 and SFS#2) and between SFS#1 and 24 h recalls. While it has been suggested that correlation coefficients can be a misleading indicator of agreement, they are useful to compare results with other studies that have not used alternative methods to assess agreement( Reference Ambrosini, De Klerk and O'Sullivan 15 ).
Reliability refers to whether a tool will give the same measurement when measuring the same thing, administered under the same conditions on two separate occasions( Reference Gleason, Harris and Sheean 16 ). Indicator and total DGI-CA scores were calculated and test–retest reliability assessed using intra-class correlations (ICC) using two-way random models. ICC were preferred over correlation coefficients which are commonly reported in other validation studies( Reference Wilson, Magarey and Mastersson 6 , Reference Magarey, Golley and Spurrier 7 ) because ICC provide an indication of the level of agreement between two measures whereas correlations show associations but do not provide information about agreement( Reference Muller and Buttner 17 ). Level of significance for ICC was P < 0·01.
Validity refers to how accurately a tool measures the actual quantity it is intended to measure. For diet it is difficult to measure usual intake and no method of assessment is free from error. Therefore in this context, validity refers to a tool's ability to perform relative to another method of dietary assessment of known performance that uses conceptually different methodology( Reference Willett 18 ). In the present study, relative validity is the comparison between the first SFS and the three 24 h recalls – a previously validated comparison method considered an accurate measure of intake at the group level with known bias (i.e. 7–11 % over-reporting compared with doubly labelled water in children)( Reference Gleason, Harris and Sheean 16 , Reference Collins, Watson and Burrows 19 ). Relative validity was assessed by comparing indicator scores from SFS#1 and mean of three 24 h recalls using a number of approaches.
ICC using two-way mixed models were used to establish the association between the methods( Reference Nelson 20 ). Bland–Altman plots were used to determine the agreement between absolute values from each method( Reference Bland and Altmann 21 ). Bland–Altman plots were generated for all food group indicators, but only the overall DGI-CA plot is presented. Mean differences and limits of agreement (±2 sd) were calculated( Reference Bland and Altmann 21 ), with positive values suggesting the SFS overestimated the indicator score relative to the 24 h recalls. Mean differences indicate how well the SFS and 24 h recall agree at the study sample level. For each indicator, whether agreement between the methods was constant across the range of intakes was examined. Linear regression analysis was performed for each indicator (the regression of the average of the two methods v. their difference) to test if the slope of the mean bias was significantly different from zero( Reference Bland and Altmann 21 ). A result different from zero suggests the bias is proportional, or varying across the range of indicator scores.
The ability of the SFS to rank individuals into tertiles of diet index scores was examined using the percentage of exact agreement (within the same tertile) and Cohen's κ coefficient. To quantify the level of error associated with the SFS, mean DGI-CA scores from the 24 recalls were calculated for tertiles created according to SFS#1. One-way ANOVA was used to determine whether differences in mean index scores between tertiles were statistically significant( Reference Willett 18 ).
All statistical analyses were conducted using IBM SPSS Statistics Version 20.
Results
Sixty-six parents were recruited, with sixty-three completing all dietary assessments. Parents were almost entirely female (97 %), married or living as married (95 %), had a tertiary degree (70 %) and were employed part-time (57 %); and their children were aged between 4 and 11 years with a mean age of 7·1 (sd 2·1) years. There were slightly more male than female children in this sample (56 % male) and almost 70 % of children were classified as normal weight (Table 1).
Table 1 Summary characteristics of child–parent dyads, Adelaide, Australia

†These data are presented as mean and standard deviation.
‡BMI Z-score was classified using the International Obesity Taskforce definition( Reference Cole, Bellizzi and Flegal 26 ).
Table 2 shows the mean food group intakes reported from each dietary assessment method. There were no significant differences between SFS#1 and SFS#2 for the number of servings reported for any food group. While the number of servings reported in SFS#1 was greater in every case, the difference in estimated mean intakes between administrations of the SFS was always less than 0·2 servings. The correlation between mean intakes on the two occasions of the SFS administrations was significant for all food groups (r = 0·43–0·94, P < 0·01). Mean food group intakes estimated from the dietary recalls were lower than from the SFS administrations for all core foods, but higher for extra foods. The difference between estimated intakes using the SFS#1 and the dietary recalls was not significant for breads and cereals (difference = 0·28 servings, P = 0·166) and beverages (difference = 0·34 servings, P = 0·084); however, it was significant for all other foods (differences ranged from 0·33 to 1·46 servings for core foods and was −0·44 servings for extra foods, all P < 0·05). The correlation between SFS#1 and the 24 h recalls was significant only for fruit, beverages and extra foods (r = 0·43–0·44, P < 0·01).
Table 2 Comparison of food intakes estimated from the two administrations of the SFS and the 24 h recalls: parent-reported food intake data of 4–11-year-old children (n 63), Adelaide, Australia

SFS, Short Food Survey.
*P < 0·05, **P < 0·01.
†Difference between methods assessed using the paired-samples t test.
‡The two administrations of the SFS were on average 7 d apart (range 2–13 d).
§Mean of three 24 h dietary recalls.
∥Pearson correlation coefficients.
Reliability of the diet index score derived using the short food survey
Table 3 shows the ICC for the DGI-CA indicator scores calculated from the two administrations of the SFS. The ICC for food groups ranged from 0·43 for dairy foods to 0·94 for beverages, and for the food choice indicators ranged from 0·77 for variety to 0·96 for reduced-fat dairy foods. The ICC for the total DQI-CA score was 0·92. All ICC were significant (P < 0·01).
Table 3 Reliability and validity of DGI-CA total and indicator scores calculated using the SFS and 24 h recalls: parent-reported food intake data of 4–11-year-old children (n 63), Adelaide, Australia
DGI-CA, Dietary Guideline Index for Children and Adolescents; SFS, Short Food Survey; ICC, intra-class correlation; LOA, limits of agreement.
*P < 0·05, **P < 0·01.
†Mean of three 24 h dietary recalls.
‡ICC calculated using a two-way random model, type: consistency.
§ICC calculated using a two-way mixed model, type: consistency.
∥All P < 0·001.
¶Positive value for difference means that SFS is higher than 24 h recall (SFS overestimates); negative value means that SFS is lower than 24 h recall (SFS underestimates).
††95 % LOA = ± 2 sd, slope of bias is regression.
Relative validity of the diet index score derived using the short food survey
The ICC for the validity of the DGI-CA indicator scores was lowest for meat and alternatives (ICC = 0·04, P = 0·393) and breads and cereals (ICC = 0·08, P = 0·279) and highest for fruit, beverages and extra foods (ICC = 0·41–0·44, P < 0·01, Table 3). The ICC for food choice indicator scores were generally higher than for the food group indicators. The ICC for wholegrain breads and cereals was lowest (ICC = 0·21), but all ICC for food choice indicators were significant (ICC = 0·21–0·47, P < 0·05 or better). The ICC for the total DQI-CA score was 0·44 (P < 0·01).
The total DQI-CA score derived from the SFS tended to overestimate the total DQI-CA score calculated from the 24 h recalls by an average of 16 points (out of 100), and the Bland–Altman plot shows that the total DGI-CA score derived using the SFS ranged from 39 % above to 7 % below the total DGI-CA score derived from the 24 h recall data (Fig. 2). The slope of this bias was not significantly different from zero (that is, the bias was consistent across the range of diet index scores). The greatest bias, within the food groups, was observed for extra foods and vegetables where the SFS overestimated the indicator score by 2·12–2·40 points (out of 10), but the slopes of these biases were not significant. The biases for dairy foods and meat and alternatives were also relatively high in the context of the overall indicator score (1·49–1·71 points out of 10) but these food groups demonstrated proportional bias (that is, the bias decreased as the indicator score increased).
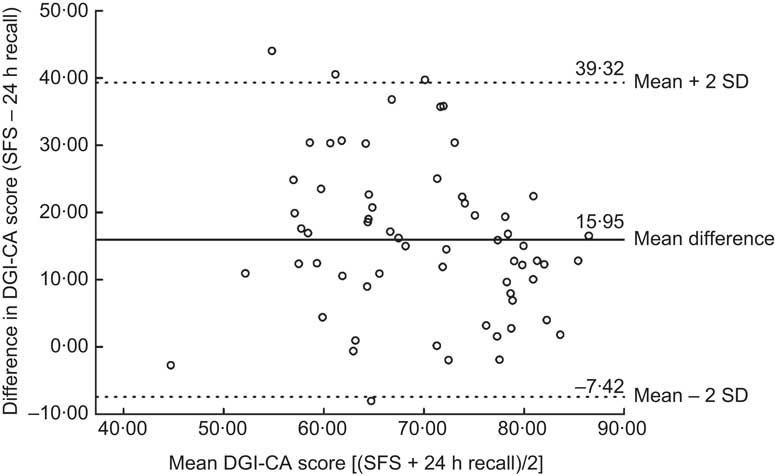
Fig. 2 Bland–Altman plot showing agreement between total DGI-CA scores calculated by the SFS and 24 h recalls. —— represents the mean difference between the two methods; – – – – represent the 95 % confidence interval (DGI-CA, Dietary Guideline Index for Children and Adolescents; SFS, Short Food Survey)
Percentage agreement between methods
In 84 % of cases the DGI-CA score derived from the two administrations of the SFS placed an individual in the same tertile for the diet index score (Table 4). The Cohen's κ value suggests substantial agreement between the two administrations of the SFS (κ = 0·76, P < 0·0 0 1). The level of agreement between SFS#1 and the 24 h dietary recalls would be considered less acceptable (κ = 0·14, P = 0·109), with only 43 % of individuals being placed in the same tertile of the index score using the different methods (Table 4).
Table 4 Agreement between methods by allocation to tertiles: parent-reported food intake data of 4–11-year-old children (n 63), Adelaide, Australia
DGI-CA, Dietary Guideline Index for Children and Adolescents; SFS, Short Food Survey.
†Exact percentage agreement for tertile allocation.
To assess the measurement error of the SFS, DGI-CA scores from the 24 h recalls were calculated for tertiles of DGI-CA score created according to SFS#1. There was a progressive increase in DGI-CA score with SFS tertile (P < 0·001, Table 5).
Table 5 Mean diet index score from the 24 h recalls for tertiles from the SFS: parent-reported food intake data of 4–11-year-old children (n 63), Adelaide, Australia
DGI-CA, Dietary Guideline Index for Children and Adolescents; SFS, Short Food Survey.
†Comparison between groups using ANOVA, significant difference and significant linear trend P < 0·01.
Discussion
The present paper describes the performance of a diet index, the DGI-CA, when index scores are derived using dietary intake data assessed using the SFS. Overall, the thirty-eight-item SFS demonstrated good reliability for all eleven indicators of the diet index. The level of agreement analysis showed that the SFS tended to overestimate intake of core food groups and underestimate the intake of extra foods compared with multiple 24 h recalls. The SFS was able to produce a reliable estimate of overall compliance with dietary guidelines, but overestimated the diet index score (DGI-CA) by 16 % relative to recalls. Its ability to correctly classify children into tertiles of compliance was less than 50 %, but comparable to another Australian study validating an FFQ against 3 d food diaries( Reference Ambrosini, De Klerk and O'Sullivan 15 ).
The performance of the SFS compared with multiple 24 h recalls was below an acceptable level for several aspects of guideline compliance (e.g. vegetables, breads and cereals, dairy and meat), but not unlike other short dietary assessment tools validated in Australian populations. The Children's Dietary Questionnaire is most similar to the current study in its attempt to measure compliance with dietary guidelines, but only includes four aspects of children's diet. The relative validity using a 7 d food checklist as the reference method, based on Spearman correlations, ranged from 0·31 for extra foods to 0·60 for fat from dairy products( Reference Magarey, Golley and Spurrier 7 ). A second questionnaire, the Child Nutrition Questionnaire, differed from the SFS in that children reported their own intake and estimated intake was compared with 7 d diet diaries, but correlation coefficients were similar (ranging from 0·36 for non-core foods and vegetables to 0·48 for fruit)( Reference Wilson, Magarey and Mastersson 6 ). So while the SFS builds on previous studies as a comprehensive measure of diet in children from which compliance with dietary guidelines can be estimated, its performance relative to a more established method of dietary assessment needs to be improved.
A study from Belgium describes a similar process to validate a diet quality index score for children, but using data derived from an FFQ( Reference Huybrechts, Vereecken and De Bacquer 22 ). This index also compares children's intake with food-based dietary guidelines. The reported reliability was slightly lower than ours (Pearson correlation r = 0·88), and validity relative to a 3 d record ranged from 0·39 to 0·74 for the different components of the index and was 0·82 overall. The mean difference between diet index scores derived from their test and reference methods was 5 %, compared with 16 % reported for the SFS. The agreement of classification into tertiles for repeat administrations was higher for our study (84 % v. 69 %), but lower between test and reference methods (43 % v. 60 %)( Reference Huybrechts, Vereecken and De Bacquer 22 ). Both studies showed progressive increases in diet index score with tertiles created using the test method. The Belgium FFQ is also parent-reported but is longer (forty-seven items) and includes frequency of meals and dietary moderation, which may be more habitual behaviours than food intake and partially explain the better relative validity results. Also, their validation was conducted in younger children for whom parents have more control over intake. Evidence suggests that parents are reliable reporters of their children's intake within the home, but not as good at reporting foods consumed outside the home( Reference Livingstone and Robson 8 ).
The ability of the SFS to estimate breads and cereals, meat and alternatives, and dairy indicator scores, compared with the mean of three 24 h recalls, was poorer than for other indicators. This may reflect the questions within the SFS, parents’ accuracy in reporting intake of these food groups or real day-to-day variation in children's eating habits. If daily variation in children's intake is high, parents may find it more difficult to estimate usual intake over the past week. In addition, pasta, rice and meat, for example, are often consumed within composite dishes, making estimating amounts consumed more difficult. Consumption of meat was asked as a frequency (where one serving was assumed to be consumed per eating occasion). The use of frequencies as an indication of portions has been validated in Australian adults( Reference Riley, Rutishauser and Webb 23 ), but results from the present study suggest that for some food groups this may not be the best way to ask parents to report their children's usual intake.
Also, the number of questions included is important. Fruit intake was estimated in one question, whereas for vegetables parents were asked to think about cooked, salad and starchy vegetables in separate questions. The level of agreement between the two methods for fruit was much higher than the level of agreement for vegetables. Fruit consumption might be more habitual and usually eaten as one piece (e.g. banana for breakfast), whereas vegetables are eaten in a range of ways and may be more difficult for parents to estimate. The questions associated with these poor-performing indicators need to be refined to better capture children's intake within the defined time period. Previous studies have not measured children's intakes of meat and bread and cereals, possibly because it has proved too difficult.
Mean bias indicates that compared with 24 h recalls, the SFS overestimates indicator scores for all food groups but underestimates extra foods, healthy fats, reduced-fat dairy and diet variety scores. Overestimation of intake of ‘desirable’ or healthy aspects of diet is commonly reported( Reference Huybrechts, Vereecken and De Bacquer 22 ). The type and the size of the bias in the context of the possible score need to be considered. Extra foods and vegetables were the two food groups with the greatest degree of bias, but in both cases the regression analysis revealed no significant difference between the slope of the bias line and zero; therefore this bias is considered to be consistent across the range of intakes and can be adjusted for more easily. In contrast for meat and dairy the bias was proportional, meaning it varied over the range of intakes, and therefore is more difficult to adjust for. The SFS overestimated the DGI-CA score derived from 24 h recalls by about 16 %, but the bias was similar regardless of the level of compliance. Ideally a questionnaire would have no bias, but all dietary assessment methods have some bias or error associated with them, so it is useful to know the magnitude of bias associated with the SFS and that, for the diet index score at least, the amount of bias is consistent across the study population.
When designing validation studies, it is important to note that the most accurate results are reported when the reference method and test tool cover the same period of time( Reference Gleason, Harris and Sheean 16 ). It is likely that estimates of DGI-CA derived from the SFS underestimate the relative validity of the SFS because data from the survey were collected prior to the period that the 24 h recalls were collected. The SFS asked parents to think about their children's usual intake over the past week. In this analysis we assumed that three days of recall within the following week would also reflect usual food group intake and therefore be a comparable point of reference to estimate validity. However, it is possible that three days of recall is not enough to capture children's usual intake, particularly given the choice and diversity in the Australian food supply. Results of this study suggest that the test and reference methods may not have captured the same period of time, contributing to poor agreement between the two methods( Reference Cade, Thompson and Burely 5 ).
The strength of the present study is that the SFS allows whole-of-diet quality and compliance with dietary guidelines to be determined in a relatively short questionnaire. Previous questionnaires have included a selection of food groups or dietary guidelines but here we have attempted to capture the guidelines in their entirety. This ability to feasibly measure compliance with guidelines will be useful for larger population studies. However, to allow monitoring of compliance with guidelines at a population level, the ability of the SFS to detect change in diet quality over time would need to be tested. The sample size was considered sufficient to adequately determine reliability and validity( Reference Cade, Thompson and Burely 5 , Reference Peat, Mellis and Williams 24 ). In terms of weight status distribution, these children were similar to the broader Australian population( 13 ); however, the mean diet index score was higher than the national average( Reference Golley, Hendrie and McNaughton 2 ).
The SFS is not immune to the errors and biases associated with most self-reported dietary assessment methods. The accuracy of the SFS to estimate compliance with guidelines relies on the estimation of food groups using the SFS to be as similar as possible to the reference method. Significant differences were observed between the SFS and 24 h recalls for five of seven food groups, which indicates limited ability of the SFS to estimate absolute intakes. Social desirability is a common phenomenon which may explain the over-reporting of healthy foods and under-reporting of extra foods seen here and in similar studies( Reference Huybrechts, Vereecken and De Bacquer 22 ). Children in the present study were from well-educated, high-income, traditional families( 25 ), so generalisability of the results to the whole population and lower socio-economic groups should be with caution. Finally, it has been suggested that by age 10 years, children have the ability to be the primary source of recall( Reference Livingstone and Robson 8 ). Future research could evaluate the SFS performance for child- v. parent-reported data.
Conclusion
Accurate and consistent measurement of dietary intake is important when evaluating public health efforts to improve diet. The SFS can provide a consistent estimate of overall compliance to dietary guidelines for children aged 4–11 years but the accuracy of the tool at both the individual and group level needs improvement. The SFS consistently overestimated diet quality by 16 % across all levels of compliance, suggesting adjustment would be necessary when estimating diet index scores in future research.
Acknowledgements
Sources of funding: This research was supported by CSIRO and the University of South Australia. R.K.G. was supported by a National Health and Medical Research Council Public Health Postdoctoral Fellowship (478115). Conflicts of interest: The authors declare no conflicts of interest. Authors’ contribution: G.A.H. and R.K.G. designed the study. E.V.S. was primarily responsible for the data collection. All authors contributed to the data analysis and interpretation of results. G.A.H. drafted the manuscript. All authors contributed to the revisions of the manuscript and approved the final manuscript for publication. Acknowledgements: The authors would like to acknowledge the parents who volunteered to participate in this study.
Appendix Details of the Short Food Survey (SFS): questions, responses and Dietary Guideline Index for Children and Adolescents (DGI-CA) scoring criteria











