Human milk provides optimal nutritional benefits for infants’ growth and development( Reference Duijts, Ramadhani and Moll 1 – Reference Ip, Chung and Raman 3 ). The majority of breast-milk feeding studies have focused on the initiation, duration or exclusivity of breast-milk feeding( Reference Thulier and Mercer 4 , Reference Dennis 5 ). Notably, the delivery mode of breast milk (direct feeding at the breast, expressed breast-milk feeding, or a combination) has been substantially less investigated. The WHO recommends that new mothers are taught the skill of hand expression during the postpartum hospital stay( 6 ), especially in cases of preterm delivery, low-birth-weight infants or infants who are unable to feed at the breast( Reference Meier 7 , Reference Furman, Minich and Hack 8 ). In addition to hand expression, breast pumps provide an alternative way for mothers to express breast milk, with exclusive expression more feasible because of substantial developments in breast pump technology after the mid-20th century( Reference Walker 9 ). When compared with direct feeding at the breast, expressed breast-milk feeding provides an alternative method to provide breast milk during periods of maternal–infant separation( Reference Labiner-Wolfe, Fein and Shealy 10 ), when there is a need to store extra milk( Reference Clemons and Amir 11 ), to manage breast-milk feeding difficulties( Reference Binns, Win and Zhao 12 ) and to facilitate maternal independence( Reference Johnson, Williamson and Lyttle 13 , Reference Johnson, Leeming and Williamson 14 ). Conversely, potential contamination of expressed breast milk( Reference Boo, Nordiah and Alfizah 15 ), loss or depletion of nutritional components( Reference Boo, Nordiah and Alfizah 15 , Reference García-Lara, Escuder-Vieco and García-Algar 16 ), the additional handling required in the process of expression( Reference Geraghty 17 ), breast pain or nipple trauma( Reference Ohyama, Watabe and Hayasaka 18 – Reference Flaherman, Gay and Scott 20 ) and lack of mother–infant skin-to-skin contact and bonding( Reference Thorley 21 ) have been identified as disadvantages of feeding with expressed breast milk or the expression process.
Researchers in high-income countries have documented a growing trend in expressed breast-milk feeding among healthy term babies( Reference Johns, Forster and Amir 22 ). Findings from the Infant Feeding Practices Study II in the USA showed that 85 % of mothers had expressed breast milk at some point, 68 % expressed within the first 2 weeks after birth, and 25 % did so on a regular basis( Reference Labiner-Wolfe, Fein and Shealy 10 ). An Australian study found that 98 % of mothers had expressed breast milk at least once( Reference Clemons and Amir 11 ). Only two studies, however, have measured expressed breast-milk feeding rates over time. One study in Australia reported that over a 10-year period from 1992–1993 to 2002–2003, the rate of any expressed breast-milk feeding within the first 6 weeks increased from 38 to 69 %( Reference Binns, Win and Zhao 12 ). Another study in Singapore reported an increase in exclusive expressed breast-milk feeding from 9 % in 2000–2001 to 18 % in 2006–2008( Reference Hornbeak, Dirani and Sham 23 ).
Studies examining the relationship between expressed breast-milk feeding and total duration of breast-milk feeding are also limited, and their conclusions are conflicting. Although some researchers have reported no significant associations between expressed breast-milk feeding and the total duration of breast-milk feeding( Reference Chapman, Young and Ferris 24 ), others have shown both negative( Reference Geraghty, Khoury and Kalkwarf 25 – Reference Jiang, Hua and Wang 28 ) and positive relationships( Reference Meehan, Harrison and Afifi 29 , Reference Win, Binns and Zhao 30 ). Schwartz et al.( Reference Schwartz, D Arcy and Gillespie 31 ) found that expressed breast-milk feeding within the first 3 weeks postpartum was associated with early breast-milk feeding cessation, whereas expressed breast-milk feeding between 4 and 12 weeks postpartum predicted a lower risk of stopping breast-milk feeding. Given the limited research on the practices and consequences of expressed breast-milk feeding in healthy term infants, the aims of the present study were to: (i) describe and compare the prevalence of expressed breast-milk feeding in healthy full-term infants at two time points (2006–2007 and 2011–2012); (ii) identify the factors associated with expressed breast-milk feeding; and (iii) examine the association between expressed breast-milk feeding at different time points and subsequent duration of any and exclusive breast-milk feeding.
Methods
Participants and setting
The current multicentre prospective cohort study examined the association between sociodemographic factors and breast-milk feeding. Study methods have been reported in more detail elsewhere( Reference Tarrant, Fong and Wu 32 , Reference Tarrant, Lok and Fong 33 ). In brief, two cohorts of mother–infant pairs were recruited during their postpartum hospitalization from the obstetric units of four geographically distributed public hospitals in Hong Kong. Hong Kong has eight public and ten private hospitals that deliver obstetric care, with public hospitals accounting for 67·8 % of all births to Hong Kong mothers( 34 ). In Hong Kong, about 75 % of women of childbearing age are employed full-time( 35 ). The maximum maternity leave in Hong Kong is 10 weeks and at least 2 weeks must be taken before the expected date of delivery( 36 ). Over 80 % of employed mothers return to work within 10 weeks postpartum, and more than one-half work 45 h or more per week( Reference Bai, Fong and Tarrant 37 ). Child care is generally provided in the home by family members or foreign domestic helpers employed by the family( Reference Bai, Fong and Tarrant 37 ) and workplace-based child care is very rare. Cohort 1 included 1417 mother–infant pairs recruited in 2006–2007 and cohort 2 included 1287 mother–infant pairs recruited in 2011–2012. Participants were Cantonese-speaking, Hong Kong Chinese mothers who had just given birth to healthy, full-term infants with no serious obstetric or birth complications and who were intending to breast-feed their infants.
Data collection
Sociodemographic characteristics were collected by maternal self-report during postpartum hospitalization. Pregnancy and birth data were collected from participants by two trained research nurses for each study cohort. Breast-milk feeding status was assessed by maternal self-report through telephone follow-up at 1, 2, 3, 6, 9 and 12 months postpartum or until breast-milk feeding had stopped, whichever occurred first. Breast-milk feeding patterns were classified as exclusive, predominant or partial, according to widely accepted definitions( Reference Labbok and Krasovec 38 , 39 ). Infants who were still receiving breast milk at 1, 2, 3 and 6 months were also asked about the number of direct feedings at the breast and the number of expressed breast-milk feedings during the previous 24 h( 39 ). We did not collect data on the source of the expressed breast milk (i.e. infant’s mother, wet nurse or breast-milk bank). However, wet nursing is not commonly practised in Hong Kong and there are no established milk banks. Thus, we have assumed that the expressed breast milk was the participant’s milk. For infants who had stopped receiving breast milk during the follow-up, weaning data – including the duration of breast-milk feeding in weeks – were reported by participants in the interview after their infants had stopped receiving breast milk. No further data were collected after this point. Both cohorts were recruited from the same hospitals using the same study protocols, inclusion criteria, questionnaires and data collection procedures.
Variable descriptions
The term ‘breast-feeding’ has been used to describe the feeding of breast milk to infants by any and all means( Reference Labbok and Krasovec 38 , 39 ). Thus, confusion may arise when we try to distinguish between different modes of breast milk delivery. Herein, we use the term ‘breast-milk feeding’ to describe all breast-milk feedings received by the infant or the generic act of feeding breast milk, irrespective of the delivery mode of breast milk. ‘Exclusive breast-milk feeding’ is defined as the infant receiving only breast milk with no other liquids or breast-milk substitutes (other than vitamins or medications). Additionally, we use the term ‘expressed breast-milk feeding’ to denote breast milk received by infants as a result of expression using either manual expression or a breast pump and the term ‘direct feeding at the breast’ to describe the feedings that were given directly from the breast.
At 1, 2, 3 and 6 months postpartum, we computed the proportion of expressed breast-milk feedings among all breast-milk feedings received by the infant in the preceding 24 h. Expressed breast-milk feedings were recoded as four levels: 0 %, >0─50 %, >50–99 % and 100 %. Exclusive expressed breast-milk feeding was defined as the infant receiving expressed milk for all breast-milk feeds (100 %). Breast-milk feeding duration was defined as the total number of weeks the infant received any breast milk. Sociodemographic variables were measured to assess their association with expressed breast-milk feeding and also served as confounding variables in the adjusted regression models. These variables included: the study cohort, proportion of total milk diet that was infant formula (0 %, >0─50 %, >50–99 %), maternal age, maternal education level, monthly family income, length of residence in Hong Kong, intention to exclusively breast-feed, participant breast-fed as a child, previous breast-milk feeding experience, husband’s infant feeding preference, delivery type and mother returning to work. Length of residence in Hong Kong was assessed as many Hong Kong mothers have migrated from Mainland China where breast-milk feeding rates in most regions are higher than in Hong Kong( Reference Xu, Qiu and Binns 40 ). Previous research has shown differences in breast-milk feeding duration between Hong Kong-born and Mainland Chinese-born mothers( Reference Tarrant, Fong and Wu 32 ).
Data analysis
Descriptive statistics were used to describe the characteristics of study participants and practices of expressed breast-milk feeding at 1, 2, 3 and 6 months postpartum. Unadjusted and adjusted logistic regression models were performed to identify factors associated with exclusive expressed breast-milk feeding across the first 6 months postpartum. The Hosmer–Lemeshow goodness-of-fit test( Reference Hosmer, Hosmer and Le Cessie 41 ) was used to assess the adequacy of the logistic models and the variance inflation factor( Reference Hair, Black and Babin 42 ) was used to assess for multicollinearity. We also employed interaction terms between the predictor variables and the study cohort in all adjusted regression models. Kaplan–Meier survival curves and log-rank tests (trend) were performed to explore the association between the different levels of expressed breast-milk feeding at the selected time points and the total duration of breast-milk feeding( Reference Cleves, Gould and Gutierrez 43 ). We used unadjusted and adjusted Cox proportional hazards models to evaluate the extent to which expressed breast-milk feeding influenced subsequent duration of any and exclusive breast-milk feeding( Reference Cox and Oakes 44 ). Breast-milk feeding duration in participants with partial follow-up (n 72) was censored at the last contact. To assess whether the association between expressed breast-milk feeding and cessation of breast-milk feeding varied between infants who were exclusively breast-fed and those who were not, interaction terms between the predictor variables and supplementation with infant formula (0 %, >0─50 %, >50–99 %) were tested in the adjusted regression models. All data analysis was conducted using the statistical software package Stata version 13.1 (2013) and a nominal significance level of 0·05 was used throughout the statistical analysis.
Results
In total, 2704 (cohort 1, n 1417; cohort 2, n 1287) mother–infant pairs were eligible for analysis. We excluded eighteen participants (cohort 1, n 8; cohort 2, n 10) who subsequently did not meet the study eligibility criteria, two participants (cohort 1) without demographic data, 124 participants (cohort 1, n 87; cohort 2, n 37) with whom there was no contact after hospitalization and 110 participants (cohort 1, n 66; cohort 2, n 44) with missing values related the primary variables. A total of 2450 mother–infant pairs (cohort 1, n 1254; cohort 2, n 1196) were included in the final analysis. Of the 2450 participants, 2·9 % (n 72) had partial follow-up, with 0·9 % (n 22) lost to follow-up after 1 month, 0·6 % (n 14) lost to follow-up after 2 months, 0·5 % (n 13) lost to follow-up after 3 months, 0·5 % (n 12) lost to follow-up after 6 months and 0·4 % (n 11) lost to follow-up after 9 months. Characteristics of participants are presented in Table 1. Among all of the participants, about 40 % had obtained a university degree and almost 70 % returned to work postpartum. Approximately one-half of the participants’ husbands supported exclusive breast-milk feeding and over one-third had no specific infant feeding preference.
Table 1 Characteristics of participants: mothers (n 2450) from in-patient postnatal units of four public hospitals in Hong Kong, 2006–2007 and 2011–2012
* HKD, Hong Kong dollars; 1 USD=7·78 HKD.
Of the 2450 participants, 64·7 % (n 1584) fed their infants with breast milk for at least 1 month, 51·0 % (n 1249) for at least 2 months, 41·9 % (n 1027) for at least 3 months and 29·0 % (n 710) for at least 6 months or longer. Figure 1 shows the levels of expressed breast-milk feeding over the first 6 months by study cohort. The proportion of exclusive expressed breast-milk feeding ranged from 5·1 to 8·0 % across the first 6 months in cohort 1, whereas the rate ranged from 18·0 to 19·8 % in cohort 2. The rate of exclusive direct feeding at the breast ranged from 62·2 to 71·4 % in cohort 1 and from 52·4 to 58·1 % in cohort 2. In cohort 1, across the first 6 months, 28·6–37·8 % of participants still breast-milk feeding were giving some amount of expressed milk. In cohort 2, the proportion ranged from 41·9 to 47·6 %.
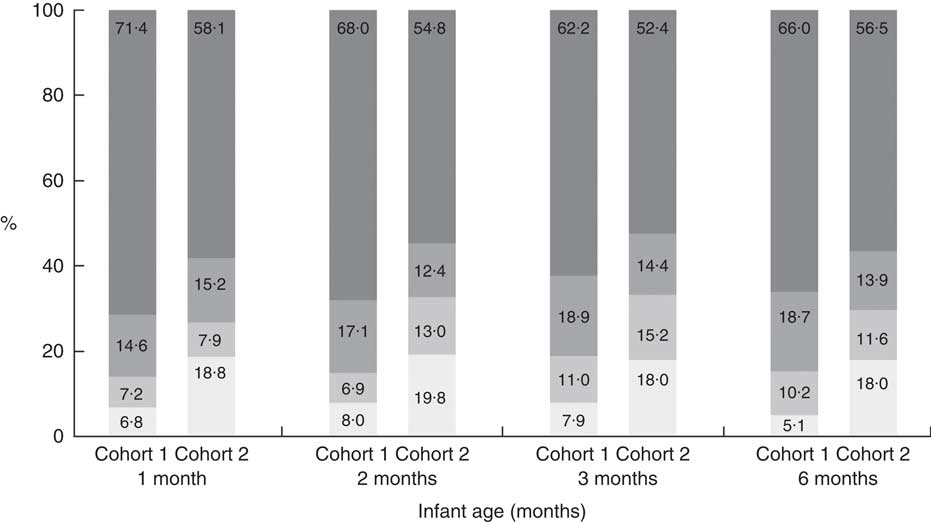
Fig. 1 Different levels of expressed breast-milk feeding (![]() , 100 %;
, 100 %; ![]() , >50–99 %;
, >50–99 %; ![]() , >0–50 %;
, >0–50 %; ![]() , 0 %) over the first 6 months of life, by study cohort (cohort 1, recruited 2006–2007; cohort 2, recruited 2011–2012), in mother–infant pairs from in-patient postnatal units of four public hospitals in Hong Kong. Sample sizes were as follows: 1 month, n 1584; 2 months, n 1249; 3 months, n 1027; 6 months, n 710
, 0 %) over the first 6 months of life, by study cohort (cohort 1, recruited 2006–2007; cohort 2, recruited 2011–2012), in mother–infant pairs from in-patient postnatal units of four public hospitals in Hong Kong. Sample sizes were as follows: 1 month, n 1584; 2 months, n 1249; 3 months, n 1027; 6 months, n 710
In the unadjusted analysis (Table 2), exclusive expressed breast-milk feeding was associated with a number of variables including: study cohort, infant formula supplementation, maternal age, maternal education, family income, length of residence in Hong Kong, participant breast-fed as a child, previous breast-milk feeding experience, husband’s infant feeding preference, delivery type and returning to work postpartum. The fully adjusted odds ratios of exclusive expressed breast-milk feeding are presented in Table 3. When compared with infants in cohort 1, infants in cohort 2 were approximately three times more likely to be fed only with expressed breast milk at all time points. Proportion of infant formula supplementation, having a planned caesarean section delivery and returning to work postpartum were all significantly associated with exclusive expressed breast-milk feeding. Conversely, participants with previous breast-milk feeding experience were less likely to feed exclusively with expressed breast milk. Results of the Hosmer–Lemeshow goodness-of-fit tests for the adjusted logistic models ranged from 0·21 to 0·92, indicating that the models were good fits for the data. Variance inflation factor values also indicated a low degree of multicollinearity. There were no significant interactions between the study cohort and the independent variables in all adjusted logistic regression models (P>0·05).
Table 2 Unadjusted odds ratios of exclusive expressed breast-milk feeding at 1, 2, 3 and 6 months postpartum by participants’ characteristics; mother–infant pairs from in-patient postnatal units of four public hospitals in Hong Kong (cohort 1, recruited 2006–2007; cohort 2, recruited 2011–2012)
Ref., reference category.
* Sample size for mothers who still breast-fed at each time point was as follows: 1 month, n 1584; 2 months, n 1249; 3 months, n 1027; 6 months, n 710.
† Supplementation with infant formula was measured at 1, 2, 3 and 6 months for each model.
‡ HKD, Hong Kong dollars; 1 USD=7·78 HKD.
Table 3 Adjusted odds ratios (aOR) of exclusive expressed breast-milk feeding at 1, 2, 3 and 6 months postpartum by participants’ characteristics; mother–infant pairs from in-patient postnatal units of four public hospitals in Hong Kong (cohort 1, recruited 2006–2007; cohort 2, recruited 2011–2012)
Ref., reference category.
* Sample size for infants who received breast milk at each time point was as follows: 1 month, n 1584; 2 months, n 1249; 3 months, n 1027; 6 months, n 710.
† Adjusted for all the variables shown in the table.
‡ Supplementation with infant formula was measured at 1, 2, 3 and 6 months for each model.
§ HKD, Hong Kong dollars; 1 USD=7·78 HKD.
Results from Kaplan–Meier survival analysis and log-rank tests (trend) showed the effect of different levels of expressed breast-milk feeding on the duration of breast-milk feeding (Fig. 2). Across the first 6 months, when compared with exclusive direct feeding at the breast, exclusive expressed breast-milk feeding was consistently associated with the highest risk of early breast-milk feeding cessation. The results of the unadjusted and fully adjusted Cox proportional hazards models showed that exclusive expressed breast-milk feeding was associated with an increased risk of early breast-milk feeding cessation when compared with direct feeding at the breast (Table 4). The hazards ratio ranged from 1·25 (95 % CI 1·04, 1·51) to 1·91 (95 % CI 1·34, 2·73) across the first 6 months. The unadjusted Cox proportional hazards analysis on exclusive breast-milk feeding showed that exclusive expressed breast-milk feeding was associated with a higher risk of stopping exclusive breast-milk feeding, with the hazards ratio ranging from 1·32 (95 % CI 1·05, 1·66) to 1·79 (95 % CI 1·54, 2·09; results not shown). However, these associations were no longer statistically significant after adjustment for confounding variables. There were no significant interactions between infant formula supplementation and different levels of expressed breast-milk feeding in all adjusted Cox proportional hazards models (P>0·05).
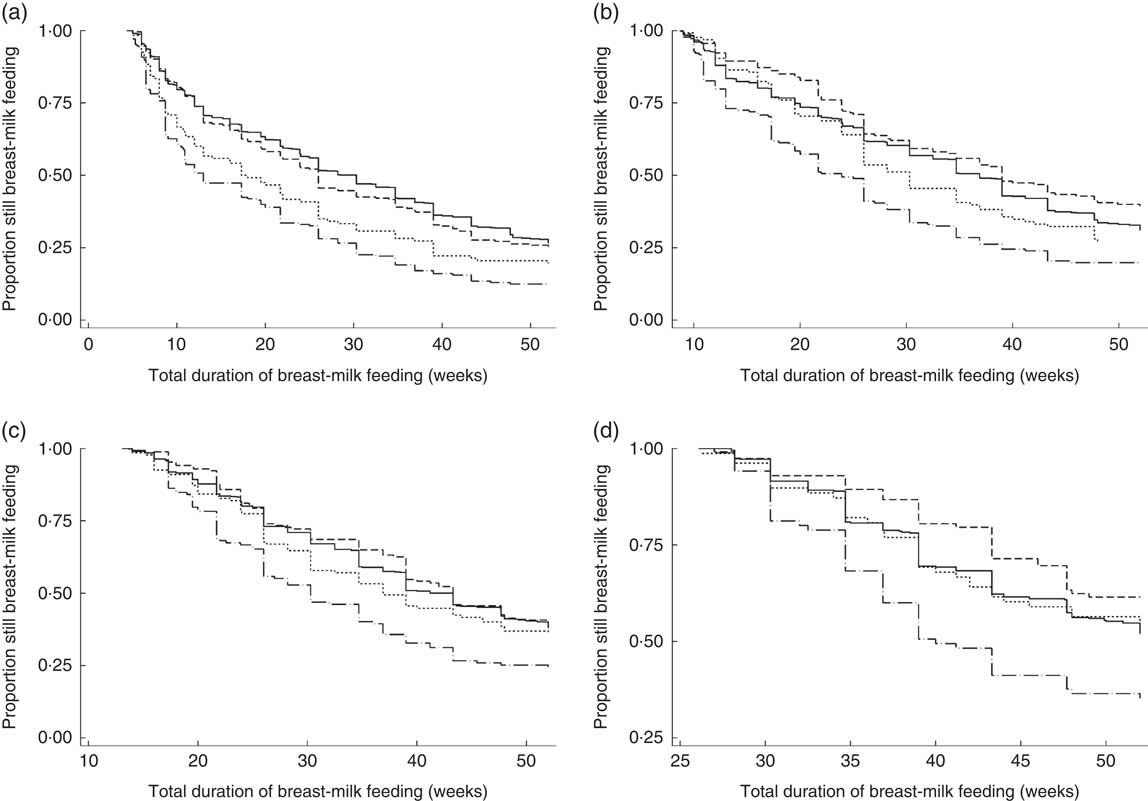
Fig. 2 Kaplan–Meier survival estimates of breast-milk feeding duration by different levels of expressed breast-milk feeding (———, 0 %; – – – – –, >0–50 %; - - - - -, >50–99 %; — · — · —, 100 %) at (a) 1 month (P trend < 0·001), (b) 2 months (P trend < 0·001), (c) 3 months (P trend < 0·001) and (d) 6 months (P trend=0·01) in mother–infant pairs from in-patient postnatal units of four public hospitals in Hong Kong. Sample sizes were as follows: 1 month, n 1584; 2 months, n 1249; 3 months, n 1027; 6 months, n 710
Table 4 Unadjusted (HR) and adjusted hazards ratios (aHR) of breast-milk feeding cessation by different levels of expressed breast-milk feeding at 1, 2, 3 and 6 months postpartum; mother–infant pairs from in-patient postnatal units of four public hospitals in Hong Kong (cohort 1, recruited 2006–2007; cohort 2, recruited 2011–2012)
Ref., reference category.
* Adjusted for study cohort, supplementation with infant formula, maternal age, maternal education level, monthly household income, length of residence in Hong Kong, participant breast-fed as a child, previous breast-milk feeding experience, husband’s infant feeding preference, delivery type and mother returning to work postpartum.
† Sample size for infants who received breast milk at each time point was as follows: 1 month, n 1584; 2 months, n 1249; 3 months, n 1027; 6 months, n 710.
Discussion
The present study is one of only a few that have examined the rate of expressed breast-milk feeding over time( Reference Binns, Win and Zhao 12 , Reference Hornbeak, Dirani and Sham 23 ). We found a substantial increase in the rate of exclusive expressed breast-milk feeding among healthy full-term infants between 2006–2007 and 2011–2012. At 1 month postpartum, the rate of exclusive expressed breast-milk feeding increased from 6·8 % in cohort 1 to 18·8 % in cohort 2. At 2 months postpartum, one-fifth of infants in cohort 2 who were still breast-milk feeding were fed exclusively with expressed breast milk. We identified risk factors associated with exclusive expressed breast-milk feeding, including supplementation with infant formula, lack of previous breast-milk feeding experience, having a planned caesarean section and returning to work postpartum. Our findings suggest that when compared with feeding solely at the breast, exclusive expressed breast-milk feeding was associated with a shorter duration of breast-milk feeding across the first 6 months.
Despite the growing trend of breast-milk expression, antenatal breast-milk feeding education has not sufficiently addressed this issue( Reference Lumbiganon, Martis and Laopaiboon 45 ). Therefore, new mothers may believe there is no difference between expressed breast-milk feeding and direct feeding at the breast and thus may express more liberally than necessary( Reference Sheehan and Bowcher 46 ). While some amount of expressed breast-milk feeding may be necessary for healthy full-term infants to remedy short-term breast-milk feeding problems, providing only expressed breast-milk feedings may negatively impact the establishment of direct feeding at the breast( Reference Win, Binns and Zhao 30 ).
Returning to work has been identified as a common reason for healthy term infants to receive expressed breast milk( Reference Labiner-Wolfe, Fein and Shealy 10 , Reference Clemons and Amir 11 , Reference Fein, Mandal and Roe 47 , Reference Geraghty, Davidson and Tabangin 48 ). Globally, an increasing number of women have become involved in the labour market over the past several decades( 35 , 49 , Reference Walling 50 ). With the short maternity leave in Hong Kong and the long working hours, mothers may find it challenging to continue breast-milk feeding when they are separated from their infants because of work( Reference Bai, Fong and Tarrant 37 ). Advances in breast pump technology have enabled mothers to effectively express breast milk at work so that they can continue breast-milk feeding while employed( Reference Walker 9 , Reference Clemons and Amir 11 ). However, maternal employment is also identified as the main reason mothers provide only expressed breast milk( Reference Fein, Mandal and Roe 47 ). In the present study, when compared with participants not returning to work, mothers returning to employment postpartum were twice as likely to feed their infants only expressed breast milk. While exclusive expressed breast-milk feeding was negatively associated with breast-milk feeding duration, at 2 months postpartum, when most Hong Kong mothers return to work( 36 , Reference Bai, Fong and Tarrant 37 ), >0─50 % expressed breast-milk feeding was associated with a lower, but not statistically significant, risk of breast-milk feeding cessation. Fein et al.( Reference Fein, Mandal and Roe 47 ) found that an infant feeding strategy that combined expressed breast-milk feeding and direct feeding at the breast was more effective in prolonging breast-milk feeding duration when compared with expressed breast-milk feeding only. In most workplaces in Hong Kong, it is currently not an option for women to bring their infants for direct breast-milk feeding, and child care is often provided by a family member or domestic helper in the home while mothers are at work( Reference Bai, Fong and Tarrant 37 ). Employers should be encouraged, or even mandated, to provide a friendly work environment that allows mothers to express breast milk during their work hours( Reference Fein, Mandal and Roe 47 ). Furthermore, reduced working hours, especially in the early postpartum period, would allow mothers more time to maintain direct breast-milk feeding( Reference Bai, Fong and Tarrant 37 ).
We also found that lower household income was associated with a lower likelihood of exclusive expressed breast-milk feeding. This may be because lower-income women are less likely to be employed full-time and therefore do not need to exclusively express breast milk. Another possible reason may be that mothers with lower income are less likely to own an electric breast pump, which is commonly used in exclusive expressed breast-milk feeding( Reference Labiner-Wolfe, Fein and Shealy 10 ). In Hong Kong there are no subsidies provided by the government or employers for purchasing breast pumps and although high-quality pumps are available to rent from commercial companies, they are highly sought after and must be booked well in advance.
Our study also found that participants with previous breast-milk feeding experience were less likely to feed exclusively with expressed breast milk, which is consistent with a previous study( Reference Labiner-Wolfe, Fein and Shealy 10 ). Mothers without breast-milk feeding experience often lack confidence in their ability to breast-feed( Reference Bandura 51 , Reference Dennis 52 ) and may be more concerned about an over- or under-supply of breast milk, a frequently cited reason for expression( Reference Labiner-Wolfe, Fein and Shealy 10 , Reference Clemons and Amir 11 , Reference Johnson, Williamson and Lyttle 13 , Reference Dykes and Williams 53 ). Other researchers have also reported that caesarean section was associated with higher rates of expressed breast-milk feeding, likely because of the delayed onset of lactation when compared with vaginal delivery( Reference Labiner-Wolfe, Fein and Shealy 10 , Reference Binns, Win and Zhao 12 ). However, we found that participants who had a planned caesarean section were more likely to feed their infants with only expressed breast milk, whereas participants who had an emergency (unplanned) caesarean section were not more likely to do so. Another study in this population found that women undergoing a planned caesarean section were less likely to initiate breast-milk feeding when compared with mothers who had an emergency caesarean or who delivered vaginally( Reference Lok, Bai and Tarrant 54 ). In Hong Kong public hospitals, elective caesarean sections are not permitted and all planned operative births are medically indicated. Therefore, it is unlikely that participants with a planned caesarean birth were substantially different from those who experienced an emergency caesarean section, except that they knew in advance they would have an operative delivery. Thus, these women may prepare in advance to feed their infant with expressed breast milk after birth and may not even attempt direct breast-milk feeding. Existing research, however, had rarely distinguished between these two types of caesarean birth when assessing the relationship between delivery type and expressed breast-milk feeding( Reference Labiner-Wolfe, Fein and Shealy 10 , Reference Binns, Win and Zhao 12 ).
Our findings suggest that supplementation with infant formula was associated with an increased likelihood of exclusive expressed breast-milk feeding. Infants supplemented with formula, especially if the supplements are given using a bottle, are more likely to experience nipple confusion and problems with direct feeding at the breast( Reference Neifert, Lawrence and Seacat 55 ). Thus, to maintain breast-milk feeding, mothers may be more likely to provide expressed breast milk. Another possible explanation is that both early formula supplementation and exclusive expressed breast-milk feeding are consequences of breast-milk feeding infants who experience difficulty in latching and sucking( Reference Labiner-Wolfe, Fein and Shealy 10 – Reference Binns, Win and Zhao 12 , Reference Parry, Ip and Chau 56 ). Either way, mothers who experience difficulties in establishing breast-milk feeding require adequate support and guidance, especially if they need to transition from a bottle to direct feeding at the breast.
The previous conflicting research findings on the association between expressed breast-milk feeding and breast-milk feeding duration( Reference Chapman, Young and Ferris 24 , Reference Geraghty, Khoury and Kalkwarf 25 , Reference Meehan, Harrison and Afifi 29 – Reference Schwartz, D Arcy and Gillespie 31 ) may have resulted from variations in study designs and sample size or the measurement of expressed breast-milk feeding using a single yes/no variable without distinguishing between different levels of the expressed breast-milk feeding( Reference Chapman, Young and Ferris 24 , Reference Meehan, Harrison and Afifi 29 – Reference Schwartz, D Arcy and Gillespie 31 ). Consistent with another recent study( Reference Jiang, Hua and Wang 28 ), we found that exclusive expressed breast-milk feeding was negatively associated with the total duration of breast-milk feeding whereas other levels of expressed breast-milk feeding were not. Existing evidence suggests that, apart from the extra time and work involved with producing and handling expressed breast milk( Reference Geraghty 17 ) and possible nipple confusion( Reference Neifert, Lawrence and Seacat 55 ), expression can cause breast pain, nipple trauma and mastitis( Reference Clemons and Amir 11 , Reference Kelleher 57 , Reference Flaherman, Hicks and Huynh 58 ), which may contribute to early discontinuation of breast-milk feeding. Also, exclusive expressed breast-milk feeding is associated with a lack of skin-to-skin contact and bonding when compared with direct feeding at the breast( Reference Thorley 21 ). Although expressed breast-milk feeding provides greater nutritional benefits than infant formula, bottle-feeding may diminish the positive effects of direct breast-milk feeding on the infant’s respiratory system. Expressed breast milk is usually fed with a bottle, which can cause a shorter duration of sucking, a higher rate of swallowing, more frequent ventilator interruptions and a lower oxygen saturation( Reference Mizuno and Ueda 59 ). The negative pressure before milk ejection in direct breast-milk feeding is approximately three times higher than the pressure developed during bottle-feeding( Reference Mizuno and Ueda 60 ). As a result, bottle-feeding reduces the lung function (lung volume and flow rate) of infants( Reference Ogbuanu, Karmaus and Arshad 61 ), which is associated with a higher risk of asthma at 10 years of age( Reference Håland, Carlsen and Sandvik 62 ). In addition to the negative effect on the respiratory system, bottle-feeding, irrespective of the type of milk, is also associated with a compromised ability to self-regulate milk intake( Reference Li, Fein and Grummer-Strawn 63 ), rapid weight gain( Reference Li, Magadia and Fein 64 ) and oral diseases( Reference Harris, Nicoll and Adair 65 ).
Researchers have raised awareness about the increasing trend of expressed breast-milk feeding( Reference Geraghty, Sucharew and Rasmussen 66 , Reference Rasmussen and Geraghty 67 ), especially exclusive expressed breast-milk feeding. On one hand, the increase in expressed breast-milk feeding may be because more mothers are choosing expressed breast milk over infant formula. In that context, this is a positive trend as expressed breast milk can provide infants with the superior nutritional benefits when compared with infant formula( Reference Ip, Chung and Raman 3 ). Conversely, the increase in expressed breast-milk feeding may be because new mothers are unaware of the benefits of direct breast-milk feeding and that expressed breast-milk feeding may be correlated with some negative health outcomes( Reference Ip, Chung and Raman 3 , Reference Ogbuanu, Karmaus and Arshad 61 , Reference Li, Magadia and Fein 64 ). Unfortunately, no qualitative data on the reasons for and experiences with expressed breast-milk feeding were collected. Further studies would be helpful to explore the reasons why mothers are increasingly expressing breast milk. It is also necessary to conduct studies to identify the health risks of expressed breast-milk feeding when compared with direct breast-milk feeding. Furthermore, researchers have recommended that in addition to the existing methods of classifying breast-milk feeding status as exclusive or non-exclusive, infant feeding studies should also categorize breast-milk feeding according to the mode of breast-milk delivery( Reference Hector 68 – Reference Felice and Rasmussen 70 ).
To our knowledge, the present study is one of only a few to describe the prevalence of expressed breast-milk feeding over time and to examine its association with breast-milk feeding duration. A large number of participants were followed prospectively for up to 12 months, with low dropout and loss to follow-up (4·6 %). The study also has some limitations. First, it was not population-based. It is also possible that mothers with less positive breast-milk feeding attitudes chose not to participate. We do not have data on those who refused to participate and participants in our sample had higher levels of maternal education and family income when compared with all mothers who initiate breast-feeding( Reference Lok, Bai and Tarrant 54 ). Other population-based surveys suggest, however, that the breast-milk feeding patterns reported in our study are similar to those in the larger population( 71 ). Second, breast-milk feeding duration was self-reported by participants and may be affected by recall bias. Such bias, however, is likely to be minimal as we followed participants on a regular and frequent basis after hospital discharge and studies have reported that mothers accurately report breast-milk feeding duration many years later( Reference Natland, Andersen and Nilsen 72 , Reference Li, Scanlon and Serdula 73 ). Third, we did not measure the method of breast-milk expression (i.e. hand expression, manual pump or electric pump). However, a Cochrane review found no significant difference in breast-milk volume between manual and electric pumps, whereas hand expression did produce less milk than an electric pump( Reference Becker, Cooney and Smith 74 ). Furthermore, mothers who exclusively express their breast milk are more likely to use electric breast pumps( Reference Labiner-Wolfe, Fein and Shealy 10 ). Fourth, at the follow-up intervals, we recorded the proportion of total feedings given – not the total volume of feeding. Thus, some misclassification bias may have been caused among those infants receiving both expressed breast-milk feeding and direct feeding at the breast. However, such misclassification bias would be unlikely to affect the interpretation of the results as infants who were fed with exclusive expressed breast milk, and those who were receiving all breast milk directly at the breast, would not be subject to misclassification. Finally, at the follow-up intervals we assessed infant feeding status by asking the mother to report the feeding patterns on the day before the follow-up( 75 ). Thus, it is possible that the feeding pattern reported did not reflect the usual infant feeding pattern of the infant.
Conclusions
An increasing number of healthy full-term infants are given expressed breast milk. Exclusive expressed breast-milk feeding is associated with a significantly higher risk of early breast-milk feeding cessation when compared with feeding directly at the breast. Thus, in both clinical practice and research, it is necessary to collect data on the mode of breast-milk delivery. Mothers who feed their infants with expressed breast milk should be encouraged to feed directly at the breast as much as possible to prolong the total duration of breast-milk feeding and to maximize the health benefits of breast-milk feeding. Further studies are needed to re-examine the current definitions of ‘breast-milk feeding’ by taking into account both the duration and the exclusivity of breast-milk feeding as well as the method of breast-milk delivery. Further studies are also needed to identify the reasons why more infants are given expressed breast milk and to assess the effect of the breast-milk delivery mechanism on maternal and child health outcomes.
Acknowledgements
Financial support: This study was supported by a grant from the Health and Medical Research Fund of the Food and Health Bureau, Government of Hong Kong Special Administrative Region (grant number #05060721); the University of Hong Kong (grant number #10207306); the University of Hong Kong Strategic Research Theme of Public Health; and the School of Nursing, the University of Hong Kong. All of the funders mentioned above had no role in the design, analysis or writing of this article. Conflict of interest: None. Authorship: D.L.B. participated in the study design, conducted data analysis, wrote the first draft of the manuscript, and approved the final manuscript as submitted. D.Y.T.F. participated in the study design, assisted the data analysis, critically reviewed and revised the manuscript, and approved the final manuscript as submitted. K.Y.W.L. assisted with data analysis, critically reviewed and revised the manuscript, and approved the final manuscript as submitted. J.Y.H.W. assisted with data analysis, critically reviewed and revised the manuscript, and approved the final manuscript as submitted. M.T. conceptualized and designed the study, obtained funding, supervised and assisted with data analysis, critically reviewed and revised the manuscript, and approved the final manuscript as submitted. Ethics of human subject participation: This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects were approved by the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster and by all participating institutions. Written informed consent was obtained from all participants.









