The rising prevalence rates of overweight and obesity have been regarded as a global pandemic( Reference Stevens, Singh and Lu 1 – Reference Swinburn, Sacks and Hall 5 ). A study in the USA showed that the high obesity prevalence could lead to a fall in life expectancy in the future( Reference Olshansky, Passaro and Hershow 6 ). Considering the increased risk of obesity-related diseases, a voluntary target with the purpose of stopping the rise of obesity by 2025 was introduced in WHO member states( 7 ). The WHO provides advocacy to help lower the prevalence of overweight in all populations( Reference Ng, Fleming and Robinson 8 , Reference Gortmaker, Swinburn and Levy 9 ). According to the nutrition and chronic disease status reports of Chinese residents in 2015, the prevalences of overweight and obesity among adults were 7·1 and 4·5 % in 2002, respectively. However, in a short span of 10 years, the prevalence rates had almost doubled in 2012 (overweight: 11·9 %; obesity: 9·6 %). The overweight and obesity prevalences in Chinese children increased rapidly from 22·8 % in 2002 to 30·1 % in 2012 and from 2·1 % in 2002 to 6·4 % in 2012, respectively( 10 ). It was reported that the overall obesity prevalence was 3·3 % in China in 1992. A rapid growth in the prevalences of overweight and obesity was perceived. The prevalence rates of overweight and obesity will continue to increase if no attention is paid to them and no effective intervention measures is taken( Reference Ma, Li and Wu 11 ).
The increased overweight and obesity prevalences and the marked shift in lifestyle-related non-communicable disease patterns in China over the past few decades may be due to rapid economic growth and urbanization as well as overnutrition characterized by increased intakes of high-fat/high-energy foods( Reference Popkin, Adair and Ng 4 , Reference Zhai, Du and Wang 12 – Reference Wu, Wang and Jiang 15 ).
Evidence indicates that the prevalences of overweight and obesity in children and adolescents worldwide have reached worrying levels( Reference Bacopoulou, Efthymiou and Landis 16 , Reference Kelishadi, Mirmoghtadaee and Najafi 17 ). Obese children are more likely to have psychological health issues due to low self-esteem compared with non-obese peers( Reference Wang, Wild and Kipp 18 ). Similarly, the lifestyle-related transformation has largely contributed to the increased prevalence rates of overweight and obesity among children and youths( Reference Al-Hazzaa 19 ). A meta-analysis conducted on the prevalence of overweight/obesity in Portuguese children showed that during the last decade, 30·3 % of Portuguese children were overweight or obese( Reference Gomes, Katzmarzyk and dos Santos 20 ).
Besides the high prevalences of overweight, obesity and abdominal obesity as well as the threat of obesity-related diseases, body weight misperception is also common among adults. Many studies conducted in different countries and populations have demonstrated that a considerable number of adults do not perceive their body weight correctly( Reference Liu, Fu and Hu 21 – Reference Klos and Sobal 26 ). A study in Sri Lanka showed that 44·7 % of overweight females and almost two-thirds of overweight males reported themselves to be ‘right weight’, and 7·6 % of overweight females and 4·1 % of overweight males considered themselves to be ‘underweight’. Over one-third of obese individuals (both males and females) even thought themselves to be ‘underweight’ or ‘right weight’. Nearly 32 % of abdominally obese individuals perceived that their waist circumference was within the normal range. Only 63·6 % thought of themselves as ‘overweight’ or ‘obese’ and tried to lose weight or take advice from professionals( Reference Jayawardena, Byrne and Soares 27 ).
Our study aimed to determine the prevalence of high weight at different characteristics, understand the perceptions and behaviours towards high body weight, and determine potential influencing factors of body weight misperception among adults in Jilin Province.
Methods
Participants
The present study was part of a large cross-sectional survey of chronic diseases in Jilin Province in 2012. Using the method of multistage stratified cluster sampling (the stratifying process has been reported previously( Reference Wang, Kou and Liu 28 )), the study was conducted among residents aged 18–79 years in nine regions per administrative division (Changchun, Jilin, Siping, Liaoyuan, Tonghua, Baishan, Songyuan, Baicheng and Yanbian). A total of 23050 individuals were recruited and 21435 of them completed the survey (response rate 84·9 %). A total of 20552 individuals (5645 in Changchun, 3160 in Jilin, 2779 in Siping, 1302 in Liaoyuan, 1263 in Tonghua, 957 in Baishan, 2217 in Songyuan, 1483 in Baicheng and 1746 in Yanbian) who had detailed information from the physical examination were chosen for the present study. The percentages of males and females were 47·0 % (n 9651) and 53·0 % (n 10 901), respectively. To make the sample more representative, the data analyses were weighted by post-stratification adjustment according to the factors of age, area and gender, using the 2010 China (Jilin Province) Population Census.
Data collection
We used the method of questionnaire investigation (sociodemographic characteristics and health-related information) and body measurements (such as height, weight and waist circumference). Sociodemographic characteristics included gender, residence (rural/urban), age, area, ethnicity, education level, marital status, occupation and income class, and health-related information included perceptions and behaviours towards high weight. All investigators had received uniform training. We calibrated the measurement instruments with a common standard before use( Reference Wang, Zhang and Gao 29 ).
Measurements
The physical examination included the measurement of height, weight, waist and hip circumferences. The participants were asked to take off their shoes and wear light clothes, and the indices were recorded to the nearest 0·1 cm or 0·1 kg.
Definitions
We calculated BMI as weight/height2 (kg/m2). All participants were categorized as normal weight (BMI=18·5 to 25 kg/m2), underweight (BMI<18·5 kg/m2), overweight (BMI=25·0 to 30·0 kg/m2) or obese (BMI>30·0 kg/m2)( 30 ). Waist circumference >94 cm in males and >80 cm in females was defined as abdominal obesity( Reference Alberti, Eckel and Grundy 31 ).
Data analysis
In addition to the complex sampling design, post-stratification adjustment according to the distribution of gender and age groups was also used for our study( 32 ). EpiData 3.1 software was used for establishment of the database and the statistical analyses were carried out using the IBM SPSS Complex Samples add-on module with IBM SPSS Statistics Version 21.0. We used χ 2 tests to compare the distribution of high weight at different characteristics and multiple logistic regression analyses were used to explore the association between sociodemographic factors and body weight misperception. P<0·05 was considered to be statistically significant.
Results
The prevalence of high weight at different characteristics by gender is shown in Table 1.
Table 1 The prevalence of high weight at different characteristicsFootnote * by gender among adults (n 20 552) aged 18–79 years from Jilin Province, Northeast China, 2012

* The numbers are unweighted, but the percentages are weighted. Complex weighted computation was used in the statistical analysis.
Among males, the prevalence of overweight, obesity and abdominal obesity in urban residents was higher than that in rural residents; however, it is interesting to note that the results in females were precisely the opposite. Among females, those of Han ethnicity were more likely to develop high body weight compared with other ethnicities. Males with a higher level of education (undergraduate and above) had a higher prevalence of high weight than those with a lower level of education, but the prevalence overall in females showed a downward tendency along with increasing education levels. Retired people had a higher chance of having high body weight than those who were not retired. In addition, the differences according to age, area, marital status and income class were of statistical significance.
Body weight perception, management and changes in the past 12 months, as well as the related lifestyles and behaviours of weight-control practices among adults in Jilin Province, are shown in Table 2.
Table 2 Perceptions and behaviours towards overweight, obesity and abdominal obesityFootnote * among adults (n 20 552) aged 18–79 years from Jilin Province, Northeast China, 2012
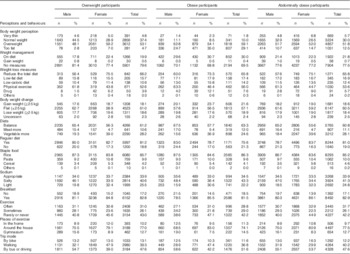
* The numbers are unweighted, but the percentages are weighted. Complex weighted computation was used in the statistical analysis.
Body weight misperception was common among adults in Jilin Province. Among those who were overweight, 44·5 % of males and 28·9 % of females considered themselves of ‘normal weight’. Moreover, 4·6 % of overweight men and 5·0 % of overweight women reported themselves being ‘very thin’. Only 48·1 % of overweight men and 59·2 % of overweight women were aware of their weight being ‘overweight, and 4·7 % of overweight participants considered themselves ‘too fat’.
About 1·8 % of both male and female obese participants perceived themselves as ‘very thin’. Only 24·7 % of obese men and 35·0 % of obese women were aware of themselves being ‘too fat’, and 10·0 % obese participants thought that they had ‘normal weight’.
Nearly 30·0 % of centrally obese men and women perceived that their waist circumference was about right and they were of normal weight, and 5·7 % of centrally obese men and women even perceived themselves to be ‘very thin’. Only 51·8 and 12·5 % of centrally obese participants reported themselves as ‘overweight’ and ‘too fat’, respectively.
Only 19·9 % of overweight, 30·0 % of obese and 21·8 % of abdominally obese participants tried to lose weight, and nearly two-thirds of them (79·6, 69·5 and 77·5 %, respectively) did not take any measures to manage their weight. Participants were more likely to choose the methods of ‘Reduce the total diet’ and ‘Physical exercise’ to lose weight (overweight participants: 66·2 % reduced their total diet and 52·6 % did physical exercise; obese participants: 65·8 % reduced their total diet and 56·0 % did physical exercise; abdominally obese participants: 65·8 % reduced their total diet and 53·6 % did physical exercise). More than half of participants had no body weight changes (±2·5 kg) in the past 12 months (overweight: 61·0 %; obese: 57·1 %; abdominally obese: 60·5 %). The related lifestyles in these three groups were observed as follows: more than half of participants had a balanced diet (i.e. meat and vegetables in fine match); two-thirds had regular diet; more than 85 % of participants were more likely to eat rice as staple food; and less than half of participants had a high salt intake. More than 80 % of participants had breakfast every day. About 40 % of the participants rarely or never did exercise; more than 70 % of them chose to exercise around the house; and nearly 50 % of participants chose to drive or go out by bus.
Table 3 shows the associations between sociodemographic factors and body weight misperception by multivariable logistic regression among individuals with overweight, obesity and abdominal obesity in Jilin Province. Rural residents were more likely to have misperception of their high body weight compared with urban residents (OR=1·340; 95 % CI 1·191, 1·509). Middle-aged participants (OR=1·826; 95 % CI 1·605, 2·078) and old participants (OR=3·101; 95 % CI 2·648, 3·632) were more likely to develop body weight misperception than youth. The prevalence of body weight misperception declined with the increase of education level (junior middle school: OR=0·628; 95 % CI 0·545, 0·723; senior middle school: OR=0·498; 95 % CI 0·426, 0·583; undergraduate and above: OR=0·395; 95 % CI 0·320, 0·487).
Table 3 Multivariate analysis of risk factors associated with body weight misperception among high-weight adults (n 11435) aged 18–79 years from Jilin Province, Northeast China, 2012
Ref., reference category.
Discussion
We come to the conclusion that body weight misperception is common among adults from Jilin Province. Nearly half of overweight individuals did not realize that their weight had already reached the warning level. Only 29·1 % of obese participants perceived themselves as being ‘too fat’; instead, 10·0 % of those who were obese thought that they had ‘normal weight’ and 1·8 % even thought that they were ‘very thin’. Nearly 30·0 % of centrally obese men and women perceived that their waist circumference was about right and they were of normal weight, and 5·7 % of centrally obese men and women even perceived themselves as ‘very thin’. A cross-sectional study that recruited 162 Chinese Americans in a community health centre in New York reported that 32 % of individuals did not perceive their body weight correctly. Nearly 20 % of them underestimated their body weight and there were significant differences by gender( Reference Liu, Fu and Hu 21 ). These Chinese Americans had a proper positioning towards their body weight compared with the present study participants. Many studies have shown that body weight misperception is common, but the correct cognition of weight is the premise of weight control( Reference Zainuddin, Manickam and Baharudin 22 , Reference Agrawal, Gupta and Mishra 24 , Reference Klos and Sobal 26 , Reference Lee, Seo and Shim 33 ).
By analysing weight management among our participants, we found that nearly two-thirds of those with high weight did not take any measures to manage their weight. They were more likely to choose the methods of ‘Reduce the total diet’ and ‘Physical exercise’ to lose weight. More than half of high-weight participants had no body weight change (±2·5 kg) in the past 12 months and most of them had a balanced diet (meat and vegetables in fine match). Two-thirds of them had regular diet, less than half of them had a high intake of salt and more than 80 % of the participants had breakfast every day. Studies exploring the association between meal intake habit and abdominal obesity in four Spanish cities reported that having breakfast did not show any association with abdominal obesity, but the individuals who did not eat dinner were more susceptible to abdominal obesity( Reference Keller, Rodriguez Lopez and Carmenate Moreno 34 ). This is consistent with our findings. Among our study participants, about 40 % of those with high weight rarely or never did exercise, more than 70 % of them chose to exercise around the house and nearly 50 % chose to drive or go out by bus. Evidence has suggested that regular self-weighing and weight management by nutrition professionals are more effective to lose weight( Reference Zheng, Klem and Sereika 35 , Reference Bleich, Bandara and Bennett 36 ).
Multivariate logistic regression analysis suggested that several factors were associated with body weight misperception. Compared with the youth, it was difficult for middle-aged and old participants to get a correct cognition of their high body weight. In our culture, symmetrical and slim features are regarded as symbols of health and beauty, but as people get older they do not pay particular attention to their appearance anymore, so they may not be consciously aware that they are gaining weight. Rural participants were more likely to get body weight misperception; possible explanations for this finding include that the education level of rural populations is lower than that of urban populations; also that rural inhabitants may lack information and knowledge about overweight and obesity.
The high prevalence of body weight misperception presents a severe challenge to public health in Jilin Province. Now we may safely arrive at the conclusion that redoubled efforts are needed to improve the situation of high weight and body weight misperception in Jilin Province. Change begins with attitude. Only when high-weight individuals realize their problem can they take effective measures, like physical exercise and regular diet, to reduce the prevalence of high weight.
Acknowledgements
Acknowledgements: The authors thank all participants involved in this study. Financial support: This work was supported by the Scientific Research Foundation of the Health Bureau of Jilin Province, China (grant number 2011Z16). The funder had no role in the design, analysis or writing of this article. Conflict of interest: The authors declare no conflict of interest. Authorship: C.G., B.L., Y. Yu, Y. Yin and X.L. conceived and designed the experiments; C.G., X.L., Y. Yin, Y.S., P.Z., R.W., L.J. and Y.W. performed the experiments; C.G. analysed the data and drafted the manuscript; C.G. and X.L. participated in revising manuscript. Ethics of human subject participation: The Ethics Committee of Jilin University School of Public Health approved this study (reference number 2012-R-011). Written informed consent was obtained from each participant.






