Osteoporosis is characterized by increased skeletal fragility and susceptibility to fractures, leading to a significant increase in morbidity and mortality(Reference Gallagher, Fowler, Detter and Sherman1). Because of the ageing of the European population, a preventive strategy for osteoporosis has become a public health priority.
Ca is an essential nutrient that plays a vital role in neuromuscular function, many enzyme-mediated processes, blood clotting, and provides rigidity to the skeleton by virtue of its phosphate salts(2). Ca consumption also influences the maintenance of bone mass(Reference Heaney3). Nearly all (i.e. 99 %) of total body Ca is located in the skeleton and the remaining 1 % is equally distributed between the teeth and soft tissues, with only 0·1 % in the extracellular compartment(2, Reference Robertson and Marshall4).
The Ca needs for adults are generally recognized as the intake required to maintain Ca balance and, therefore, skeletal integrity(2, Reference Ilich, Brownbill and Tamborini5). The Recommended Dietary Allowance (RDA) for European adults is 800 mg/d(Reference Hautvast, Baya and Amorim Cruz6). After menopause, Ca requirements increase to at least 1000 mg/d(Reference Heaney, Recker and Saville7, 8). The WHO recommendation for European postmenopausal women is 1300 mg/d(2, Reference Heaney3).
The objective of the present study was to assess the daily dietary Ca intake in European postmenopausal osteoporotic women.
Methods
Postmenopausal women aged over 50 years were included in the study. These women were part of a run-in study aimed at normalizing the Ca and vitamin D status of osteoporotic patients prior to their inclusion in a trial investigating the anti-fracture efficacy of a new anti-osteoporotic drug. Patients were considered osteoporotic if their lumbar spine or femoral neck bone mineral density was at least 2·5 standard deviations below the median T-score.
The present study involved 8524 patients from nine European countries: Belgium (n 1193), Denmark (n 327), France (n 1290), Germany (n 373), Hungary (n 353), Italy (n 1233), Poland (n 1544), Spain (n 590) and the UK (n 1621).
Assessment of Ca intake was performed with a previously validated self-questionnaire(Reference Fardellone, Sebert, Bouraya, Bonidan, Leclercq, Doutrellot, Bellony and Dubreuil9). This questionnaire enables evaluation of the Ca content of the diet of an individual on the basis of twenty different types of food (items) rich in Ca and/or frequently eaten. Obviously, tablets of Ca taken as supplements were also considered. Our study population was divided into three categories of Ca consumption: <800 mg/d, 800–1300 mg/d and >1300 mg/d. These thresholds were fixed according to the RDA for European adults (800 mg/d)(Reference Hautvast, Baya and Amorim Cruz6) and the WHO recommendation for European postmenopausal women (1300 mg/d)(2).
Results
The mean age of the 8524 women included in the present study was 74·2 (sd 7·1) years, mean BMI was 25·7 (sd 4·2) kg/m2. Table 1 shows the characteristics of the patients according to category of dietary Ca intake (i.e. <800 mg/d, 800–1300 mg/d, >1300 mg/d).
Table 1 Baseline characteristics of women according to category of dietary calcium intake: European postmenopausal osteoporotic women
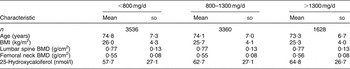
BMD, bone mineral density.
In the whole study population, 37·2 % of the women took Ca supplements (34·9 % of women aged over 75 years and 38·9 % of women aged less than 75 years). Mean daily food intake was significantly lower (P < 0.001) in subjects who did not take a Ca supplement.
The mean dietary Ca intake (food plus supplements) was 930·7 (sd 422·9) mg/d. Only 19·1 % of women (n 1628) had daily dietary Ca consumption >1300 mg. Moreover, 39·4 % (n 3360) of the study population had daily Ca dietary intake of 800–1300 mg and 41·5 % (n 3536) had an intake of <800 mg daily (Fig. 1).

Fig. 1 Proportion of women in the global population, women aged less than 75 years and women more than 75 years of age meeting different thresholds (░, <800 mg/d; □, 800–1300 mg/d; ▒, >1300 mg/d) of dietary calcium intake: European postmenopausal osteoporotic women
Daily Ca intake from food and supplements, stratified by country, is shown in Table 2. The highest level of daily Ca intake from food was found in Denmark (1145·6 mg/d) and the smallest in Hungary (586·7 mg/d). Figure 2 shows the proportions of women in the different countries according to intake category (i.e. <800 mg/d, 800–1300 mg/d, >1300 mg/d).
Table 2 Dietary calcium intake and the percentage of women taking calcium supplements in different countries: European postmenopausal osteoporotic women


Fig. 2 Proportion of women in different European countries meeting different thresholds (░, <800 mg/d; □, 800–1300 mg/d; ▒, >1300 mg/d) of dietary calcium intake: European postmenopausal osteoporotic women
We found the lowest dietary Ca inadequacy in women aged over 75 years compared with women aged less than 75 years (P < 0·0001). Only 17·1 % of women aged over 75 years achieved 1300 mg/d compared with 20·5 % of women aged less than 75 years (P = 0·0001 for the difference between the two groups) (Fig. 1).
Discussion
We have shown that the mean dietary Ca intake of European postmenopausal osteoporotic women was below the WHO recommendation. The majority of these women (41·5 %) took less Ca than that recommended for adults before menopause (800 mg/d) and only 19·1 % of them achieved the WHO recommendation (1300 mg/d) for this population. The level of daily Ca intake from food varied across different European countries but always remained below the WHO-recommended intake.
Other epidemiological studies have described low dietary Ca intake. In 131 healthy postmenopausal women aged 64·7 (sd 7·6) years, Andon et al. found mean Ca consumption of 606 (sd 302) mg/d(Reference Andon, Smith, Bracker, Sartoris, Saltman and Strause10). In late (≥5 years) postmenopausal women, Jensen et al.(Reference Jensen, Holloway, Block, Spiller, Gildengorin, Gunderson, Butterfield and Marcus11) described mean Ca consumption of 793 (sd 280) mg/d in women aged 65 years and older. In 184 elderly women aged over 65 years, Pfister et al.(Reference Pfister, Wul and Saville12) found a mean dietary Ca intake of 563.4 mg/d. The combined dietary Ca intake and supplement Ca intake in elderly women (>60 years old) participating in NHANES III (Third National Health and Nutrition Examination Survey) was 864 (sd 16) mg/d(Reference Ervin and Kennedy-Stephenson13). In a recent study, the mean dietary Ca intake reported by 167 postmenopausal women aged 40–65 years was 924 (sd 347) mg/d(Reference Cussler, Going, Houtkooper, Stanford, Blew, Flint-Wagner, Metcalfe, Choi and Lohman14).
Subjects included in the present study were women being screened for taking part in a study assessing the anti-fracture efficacy of a new anti-osteoporotic drug in postmenopausal osteoporosis. Other studies performed in such populations (i.e. screening for randomized controlled trials of anti-osteoporotic drugs) also described low Ca intake in postmenopausal osteoporotic women(Reference Liberman, Weiss, Broll, Minne, Quan, Bell, Rodriguez-Portales, Downs, Dequeker and Favus15–Reference Reid, Ames, Evans, Gamble and Sharpe20). For example, in 1637 postmenopausal women with prior vertebral fractures, mean daily intake of Ca from food ranged from 675 mg to 786 mg in the different randomized groups(Reference Neer, Arnaud and Zanchetta19). In the baseline characterization of the Fracture Intervention Trial(Reference Black, Cummings and Karpf16), the mean Ca intake was 619 mg/d for the placebo group (n 1005) and 652 mg/d for the treatment group (n 1022).
In the present study, we have shown that the daily intake of Ca from food was low and that only 37·2 % of the women took Ca supplements. Foods provide the best way to meet the Ca requirement because they constitute good sources of other essential nutrients(Reference Heaney3). However, dietary Ca intake has been found to be dependent on socio-economic status(Reference Winzenberg, Riley, Frendin, Oldenburg and Jones21) and personal attitudes towards food (i.e. milk)(Reference Pfister, Wul and Saville12). Moreover, it is difficult to achieve vitamin and mineral requirements when daily energy intake is below 6·28 MJ (1500 kcal)(Reference Schlienger, Pradignac and Grunenberger22–Reference Walker and Ball24). Thus different expert groups have recommended use of Ca supplements by postmenopausal osteoporotic women(Reference Boonen, Rizzoli, Meunier, Stone, Nuki, Syversen, Lehtonen-Veromaa, Lips, Johnell and Reginster25–Reference Compston27). In the present study, it appeared that women who took Ca supplements had higher mean daily Ca intake from food (P < 0.001) compared with women who did not take supplements, probably because of a greater awareness of their osteoporosis disease.
Osteoporotic fractures occur predominantly in populations aged over 65 years(Reference Dhesi, Allain, Mangoni and Jackson28). Elderly populations have lower daily intakes of vitamins and minerals compared with younger populations(Reference Mowe and Bohmer29), partly because of a lower food intake. In the present study, we found the highest dietary Ca inadequacy in women aged less than 75 years compared with women aged over 75 years. Only 17·1 % of women aged over 75 years achieved 1300 mg Ca/d compared with 20·5 % of women aged less than 75 years. We used the WHO recommendation for postmenopausal women to set up a threshold of 1300 mg/d, but the National Institutes of Health consensus group recommends a Ca consumption of at least 1500 mg/d after 65 years(8, Reference Lowenstein30). Our results confirm the difficulty in achieving correct daily Ca intake by food consumption alone in old postmenopausal women. Unfortunately, it should be pointed out that only 36·8 % of these women used Ca supplements.
In the present study we assessed dietary Ca intake of a population screened prior to inclusion in a trial investigating the anti-fracture efficacy of an anti-osteoporotic drug. Because of the patient inclusion/exclusion criteria in this particular study, our population cannot be representative of the general population but more of an osteoporotic population starting a treatment.
Another limitation of the study relates to the Ca intake assessment, which was performed with a validated self-questionnaire(Reference Fardellone, Sebert, Bouraya, Bonidan, Leclercq, Doutrellot, Bellony and Dubreuil9). However, it should be pointed that some studies have found that some dietary recalls and records could have an underestimation of 25–30 %. However, even if our data are underestimated, our conclusion that dietary Ca intake is very low in European postmenopausal women is still true and could even be more serious.
Osteoporosis and its consequences are a serious public health problem in the ageing population(Reference Gallagher, Fowler, Detter and Sherman1, Reference Boonen, Bischoff-Ferrari, Cooper, Lips, Ljunggren, Meunier and Reginster31). Our study shows insufficient dietary Ca intakes in postmenopausal osteoporotic women (whatever the age) in nine European countries. A substantial part of our study population does not achieve the general recommendation for Ca intake in such a population. We believe that greater awareness of this public health problem could help the fight against osteoporosis.
Acknowledgements
Declaration of interest: The authors declare that they have no competing interest. No industry funding was received for the study. The authors thank Servier for providing access to their database.
Author contributions: design of the study – O.B. and J.-Y.R.; analysis of the results – O.B., C.D.C., C.M., A.N. and O.M.; interpretation of the results – O.B., C.D.C., C.M. and J.-Y.R.; draft of the manuscript – O.B. and C.D.C.; final approval of the manuscript – all authors.






