Recent studies have linked increased soft drink consumption with the prevalence of asthma. A 2012 Australian study found an association between soft drink consumption and asthma and chronic obstructive pulmonary disease among adults( Reference Shi, Dal Grande and Taylor 1 ). In a 2013 report, the US Centers for Disease Control and Prevention linked soft drink intake by US high-school children with asthma, possibly (but inconclusively) due to preservatives( Reference Park, Blanck and Sherry 2 ). While much is known about what triggers asthma in some people, the exact cause remains unknown for millions of sufferers. In fact, the aetiology behind the epidemic rise in US asthma rates since 1980 remains poorly understood( 3 ). A review prior to the millennium showed that asthma rates began to climb steadily around 1980. According to the Asthma and Allergy Foundation of America, asthma (inexplicably) increased among schoolchildren by 80 % and among pre-school children by 160 % between 1980 and 1994( Reference Akinbami 4 ). In 2009, about 25 million or 8 % of the overall US population had asthma, compared with 7 % of the population in 2001. In 2005, 8·9 % of children in the USA had asthma. A more in-depth review revealed that US asthma rates are highest among Hispanic and African-American children and among those living in poor socio-economic conditions( 5 ). According to a 2011 report by the US Department of Health and Human Services’ Office of Minority Health, African-Americans are 20 % more likely to have asthma, and 3·6 times more likely to visit the emergency room for asthma, than non-Hispanic whites( 6 ). Puerto Rican children are 3·2 times more likely to have asthma( 6 ) than non-Hispanic white children. In 2011, the prevalence of asthma among Puerto Rican children under 18 years of age was 25 %( 7 ). These unprecedented levels are costly not only in terms of human health, but also in economic terms. It is estimated that the annual economic cost of asthma in the USA is over $US 56 billion( 5 ).
Anecdotal evidence links intake of high fructose-sweetened foods and beverages with childhood asthma( Reference DeChristopher 8 ). In situ intestinal formation of advanced glycation end products (enFruAGE) arising from high intake of excess free fructose (EFF) has been suggested as a possible mechanism for EFF-associated childhood asthma( Reference DeChristopher 8 ). Recently, an important role for the receptor of advanced glycation end products (RAGE) in mediating asthma has been suggested( Reference Milutinovic, Alcorn and Englert 9 ). This supports the possibility that advanced glycation end products (AGE) – known ligands of RAGE – might contribute to asthma pathogenesis. While dietary AGE (dAGE) are known to contribute to increased oxidant stress and inflammation, and have been linked to the recent epidemics of diabetes and CVD( Reference Uribarri, Woodruff and Goodman 10 ), and while metabolic syndrome has been linked to increased risk of incident asthma( Reference Brumpton, Camargo and Romundstad 11 ), no study to date has directly linked dAGE to asthma. Further, no study that we are aware of has evaluated the possibility that intestinally formed AGE (enFruAGE) due to EFF intake may contribute to asthma pathogenesis.
Intake of EFF, as contained in apple juice and in the popular sweetener high-fructose corn syrup (HFCS), but not in sucrose, has been shown to result in fructose malabsorption (FM) in a significant percentage of the adult population( Reference Riby, Fujisawa and Kretchmer 12 – Reference Jones, Burt and Dowling 21 ). One study( Reference Riby, Fujisawa and Kretchmer 12 ) showed that 30 % of adults tested positive for FM when challenged with 25 g of EFF (50 g fructose and 25 g glucose) and about 50 % tested positive when challenged with 25 g of fructose alone. While FM in normal paediatric populations is under-studied( Reference Riby, Fujisawa and Kretchmer 12 – Reference Jones, Burt and Dowling 21 ), available data suggest that FM is significantly more common in younger than in older children( Reference Gomara, Halata and Newman 16 , Reference Gibson, Newnham and Barrett 17 , Reference Jones, Burt and Dowling 21 ). Although conventional wisdom suggests that HFCS is 55 % fructose and 45 % glucose, independent laboratory results have shown that concentrations in popular soft drinks may be as high as 65 % fructose to 35 % glucose( Reference Ventura, Davis and Goran 22 ). This suggests that the ratio of fructose to glucose in leading soft drinks and possibly other foods ranges from 1·4:1 to 1·8:1( Reference Ventura, Davis and Goran 22 ), which may predispose to FM( Reference Riby, Fujisawa and Kretchmer 12 – Reference Jones, Burt and Dowling 21 ). It is also noteworthy that increases in asthma appear to parallel US HFCS intake trends( 23 – Reference Haley, Toasa and Jerardo 26 ).
In the ‘intestinal enFruAGE fructositis’ hypothesis, high amounts of malabsorbed fructose precipitated by high intake of EFF may lead to the in situ formation of AGE (enFruAGE) within the intestine( Reference DeChristopher 8 ). These enFruAGE may then be absorbed into the systemic circulation, travel to the lungs – a tissue with high RAGE concentration( Reference Buckley and Ehrhardt 27 ) – and activate asthma-associated pro-inflammatory signalling( Reference DeChristopher 8 ). We, therefore, examined a potential role for enFruAGE in asthma pathogenesis by studying the correlation between asthma prevalence and intake frequency of high EFF beverages, including apple juice (AJ)( 23 ), HFCS-sweetened (non-diet) soft drinks (ndSD)( 23 ) and fruit drinks (FD), in a large database containing information about beverage/juice intake and prevalence of asthma at different ages (National Health and Nutrition Examination Survey (NHANES) 2003–2006). Analyses were repeated using intake frequency of orange juice (OJ) as a comparison beverage – i.e. use of a beverage that contains sucrose and a relatively equal ratio of fructose to glucose monomers( 23 ).
Methods
Sample and survey administration
The present cross-sectional study is based on data from the 2003–2006 US NHANES( 28 ). The Centers for Disease Control and Prevention and National Institutes of Health utilize NHANES to assess the health and nutritional status of adults and children in the USA. These surveys are unique in that they combine interviews and physical examinations, as well as dietary intake. In 2003–2006, a food intake frequency questionnaire was added to assess usual intakes of specific foods and food groups. These data are used in the present analysis, as we were interested in long-term patterns of intake rather than detail on specific days. Strong and consistent relationships have been reported between FFQ frequency of food and food-group consumption and probability of consumption on 24 h recalls( Reference Subar, Dodd, Guenther and Kipnis 29 ). Food intake frequencies are commonly used as reliable sources of food intake and dietary pattern information in epidemiological research( Reference Park, Blanck and Sherry 2 , Reference Kerver, Yang and Bianchi 30 – Reference Sofianou, Fung and Tucker 33 ).
The NHANES uses a complex sampling design and constructs sample weights to produce nationally representative data. These sample weights were used to perform statistical analysis for the present study. In the 2003–2006 survey periods, the sampling fractions and screener rates were set to oversample certain groups (low-income persons, adolescents, the elderly, non-Hispanic blacks and Mexican-Americans) to increase the ability to obtain more precise estimates for these groups( 34 ). The weights used were those provided in the food frequency file. Therefore, all statistics and summary tables are appropriately weighted to account for oversampling. The number of observations, detailed within each summary table, reflects the weighted number of respondents within each age group by beverage type being analysed.
Overall, 11 505 individuals aged 2–85 years responded to the FFQ beverage intake questions as well as participated in the medical examinations component of the survey, of whom 11 490 provided information regarding asthma history. For the present analysis, we focused on the youngest children, aged 2–9 years (n 1961), based on evidence from prior research that they are likely to be the most affected by FM( Reference Gomara, Halata and Newman 16 , Reference Gibson, Newnham and Barrett 17 , Reference Jones, Burt and Dowling 21 ) and, therefore, the most likely to form enFruAGE. For comparison, we repeated some of the analyses in children aged 10–16 years. There were 1961 study respondents aged 2–9 years and 2300 aged 10–16 years.
Variables
The outcome variable was self-reported current or prior asthma. On the NHANES questionnaire, this was asked as: ‘Has a doctor or other health professional ever told you that you have asthma?’ The exposure to beverage intake variables was obtained from the FFQ questions: ‘How often did you drink: (i) Apple juice? (ii) Orange or grapefruit juice? (iii) Other fruit drinks (such as cranberry cocktail, lemonade, etc.)? (iv) Soft drinks, soda, or pop in the summer? (v) Soft drinks, soda, or pop the rest of the year?’ Additional questions clarified how often fruit drinks or soft drinks were diet or sugar-free, or caffeine-free.
The average daily frequency of ndSD over the past year was calculated by summing individual values for caffeinated and caffeine-free non-diet soda in the summer and rest of the year. The NHANES utilized specialized software (Diet-Calc) to assign frequencies to responses from the FFQ using algorithms as follows: ‘never’=0; ‘1 time per month or less’=0·03; ‘2–3 times per month’=0·08; ‘1–2 times per week’=0·21; ‘3–4 times per week’=0·5; ‘5–6 times per week’=0·79; ‘1 time per day’=1; and ‘2–3 times per day’=2·5. Intake data were combined to establish new intervals for analysis purposes as follows: ≤1 time/month (includes zero) as the reference group; 2–3 times/month; 1–4 times/week; and ≥5 times/week.
To analyse the combined effects of EFF, the following algorithm was used. Intake frequencies for AJ, FD and ndSD were assigned 0 for ≤1 time/month; 0·117 for 2–3 times/month; 0·357 for 1–4 times/week; and 1 for ≥5 times/week. These values were summed to calculate average daily intake of total EFF beverages. Analyses were repeated using frequency of OJ intake as a comparison beverage that does not contain EFF( 23 ). Adjustment variables included sex, race/ethnicity, age, BMI and total energy intake. They were selected for use in the present study based upon existing research( Reference Park, Blanck and Sherry 2 , Reference Eaton, Kann and Kinchen 35 – Reference Park, Sherry and Foti 37 ). Total energy intake was the only variable obtained from the 24 h dietary recall.
BMI (kg/m2) was calculated by NHANES from measured height and weight. Weight status was classified based on BMI percentiles as defined by NHANES as follows: underweight/normal weight, <85th percentile; overweight, ≥85th and <95 percentile; and obese, ≥95th percentile.
Socio-economic status was included as a potential confounding variable using data obtained for family income and head of household education level. NHANES used the Family Interview Income Questionnaire to obtain combined family income for thirteen income ranges. For analysis purposes, these were reduced to: 0–$US 19 999; $US 20 000–34 999; $US 35 000–54·999; and ≥$US 55 000. Head of household education level was obtained by asking: ‘What is the highest grade or school level you have received?’ Categories were: <9th grade; 9th–11th grade; high school/GED; some college; and college graduate (GED=General Educational Development).
Statistical analysis
Analyses were performed utilizing the STATA statistical software package revision 18. As previously described, strata, cluster (primary sampling unit) and weight variables were used to account for non-response and for the complex sampling design.
Rao–Scott χ 2 analysis was used to test for significance of differences in asthma prevalence by intake frequency. A P value of ≤0·05 was considered significant, with values <0·10 considered as approaching significance. Bivariate logistic regression was used to assess the crude odds between exposure variables and asthma across age groups. Analysis was performed individually for AJ, FD, ndSD and total EFF (tEFF). In addition to bivariate analysis, two multivariable models were utilized to analyse adjusted odds ratios. The first model adjusted for age, sex, race/ethnicity, BMI and total energy intake. The second model also adjusted for other EFF beverages. For example, during analysis of AJ as the main exposure variable of interest, the model also adjusted for FD and ndSD. This approach was used to assess the association between (for example) AJ and asthma, independent of FD and ndSD. In logistic regression analysis, confidence intervals that did not include 1·0 and P values ≤0·05 were considered statistically significant.
Results
Descriptive characteristics of the sample are presented in Table 1. Overall, 11·7 % of 1961 children aged 2–9 years were reported to have asthma (or history of asthma). There was a statistically significant correlation between increasing intake of EFF beverages and increased prevalence of asthma in children aged 2–9 years (P≤0·05). Unadjusted Rao–Scott χ 2 comparisons with asthma prevalence showed that AJ was significantly associated with asthma and that FD and tEFF approached significance (Table 2).
Table 1 Characteristics of children aged 2–9 years, National Health and Nutrition Examination Survey 2003–2006

Table 2 Crude associations between excess free fructose (EFF) beverage intakes and asthma prevalence in children aged 2–9 years, National Health and Nutrition Examination Survey (NHANES) 2003–2006
Significant associations are shown in bold font.
* AJ (apple juice) is one of very few foods known to contain fructose in high relative proportion to glucose (approximately 2:1)( 23 ).
† FD (non-diet fruit drinks) corresponds to sweetened fruit beverages, other than juices, known to contain high-fructose corn syrup (HFCS) as the main sweetener.
‡ ndSD (non-diet soft drinks) corresponds to caffeinated and caffeine-free, non-diet soda; in 2003–2006 (the NHANES study period) HFCS was the main sweetener in soda( Reference Vartanian, Schwartz and Brownell 47 ).
§ tEFF (total excess free fructose) combines average intake frequency for AJ+FD+ndSD.
|| OJ (orange juice) is not an EFF beverage and is included for comparison. The ratio of fructose to glucose is approximately 1:1( 23 ).
In logistic regression models adjusted for age, sex, race/ethnicity, BMI and total energy intake, the cumulative effects of AJ+FD+ndSD (tEFF) were highly significant. Children in this age group reporting tEFF intake ≥5 times/week had more than five times higher odds of asthma than ≤1 time/month consumers, after adjusting for potentially confounding variables (OR=5·29; 95 % CI 1·49, 18·72; P=0·012). Adjusting for socio-economic status did not materially change the results (Fig. 1). Increased intake of AJ was also strongly correlated with asthma in this age group, after adjusting for other beverages (ndSD and FD). In fully adjusted models, the odds of asthma in children drinking AJ ≥5 times/week or 1–4 times/week was more than double that in children consuming AJ ≤1 time/month (respectively: OR=2·43; 95 % CI 1·07, 5·54; P=0·035 and OR=2·76; 95 % CI 1·39, 5·51; P=0·005; Table 3).
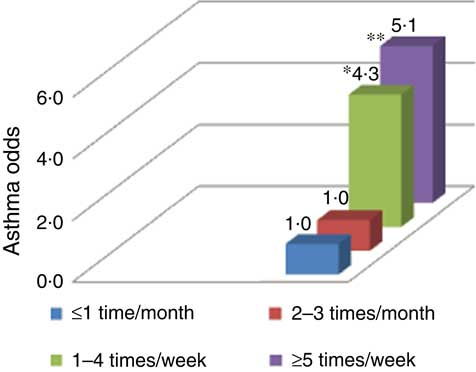
Fig. 1 (colour online) Odds of asthma by tEFF beverages consumption among children aged 2–9 years, adjusted for age, sex, BMI, total energy intake, race/ethnicity and socio-economic status (family income and head of household education level); National Health and Nutrition Examination Survey (NHANES) 2003–2006. tEFF (total excess free fructose) combines average intake frequency for apple juice (AJ)+non-diet fruit drinks (FD)+non-diet soft drinks (ndSD). AJ is one of very few foods known to contain fructose in high relative proportion to glucose (approximately 2:1)( 23 ). FD corresponds to sweetened fruit beverages, other than juices, known to contain high-fructose corn syrup (HFCS) as the main sweetener. ndSD corresponds to caffeinated and caffeine-free, non-diet soda; in 2003–2006 (the NHANES study period) HFCS was the main sweetener in soda( Reference Vartanian, Schwartz and Brownell 47 ). Odds were significantly higher compared with ≤1 time/month consumption: *P=0·024; **P=0·011.
Table 3 Associations between excess free fructose (EFF) beverages and asthma in children aged 2–9 years, National Health and Nutrition Examination Survey (NHANES) 2003–2006
Significant associations are shown in bold font.
* tEFF (total excess free fructose) combines average intake frequency for AJ+FD+ndSD.
† AJ (apple juice) is one of very few foods known to contain fructose in high relative proportion to glucose (approximately 2:1)( 23 ).
‡ FD (non-diet fruit drinks) corresponds to sweetened fruit beverages, other than juices, known to contain high-fructose corn syrup (HFCS) as the main sweetener.
§ ndSD (non-diet soft drinks) corresponds to caffeinated and caffeine-free, non-diet soda; in 2003–2006 (the NHANES study period) HFCS was the main sweetener in soda( Reference Vartanian, Schwartz and Brownell 47 ).
|| OJ (orange juice) is not an EFF beverage and is included for comparison. The ratio of fructose to glucose is approximately 1:1( 23 ).
While increasing tEFF and AJ intakes were significantly correlated with asthma, the opposite tendency was observed with OJ. In fully adjusted models, including remaining EFF beverages, the odds for asthma in children aged 2–9 years consuming OJ ≥5 times/week approached significance and appeared to be half that of ≤1 time/month consumers (OR=0·50; 95 % CI 0·24, 1·05; P=0·065; Table 3). Adjusted odds of asthma in FD drinkers aged 2–9 years followed a similar pattern, albeit less significant, to that seen with AJ. The adjusted odds of asthma in FD drinkers was higher in 2–3 times/month, 1–4 times/week or ≥5 times/week consumers v. ≤1 time/month consumers (respectively: OR=2·56; 95 % CI 1·03, 6·36; P=0·043; OR=2·00; 95 % CI 0·85, 4·73; P=0·110 and OR=1·61; 95 % CI 0·64, 4·05; P=0·299; Table 3). Consumption of ndSD was associated with asthma only in conjunction with AJ and FD, as part of tEFF. There were no significant associations between any of the EFF beverages analysed and asthma in 10–16-year-olds (data not shown).
Discussion
Recent studies have linked intake of non-diet soda with asthma in high-school children( Reference Park, Blanck and Sherry 2 ) and adults( Reference Shi, Dal Grande and Taylor 1 ). The present study is the first one we know of to link intake of HFCS-sweetened beverages and AJ – beverages with relatively high levels of EFF – with asthma in young children. Results are consistent with anecdotal evidence linking HFCS with asthma( Reference DeChristopher 8 ) and with research indicating that RAGE is a central mediator of asthma( Reference Milutinovic, Alcorn and Englert 9 ). Although other interpretations are possible, these analyses support the mechanistic hypothesis that enFruAGE – ligands of RAGE that are generated locally within the intestinal lumen following excessive intake of EFF beverages – may play a role in the pathogenesis of asthma in young children. Further, these results are consistent with parallel trends between US HFCS intake( 23 – Reference Haley, Toasa and Jerardo 26 ) and the inexplicable rise in childhood asthma beginning around 1980( Reference Akinbami 4 ).
The present analyses showed that after adjusting for FD and ndSD, the odds of asthma among children aged 2–9 years reporting AJ consumption ≥1–4 times/week was nearly three times that of low or non-AJ consumers. Odds of asthma remained more than two times higher among ≥5 times/week AJ consumers v. low or non-AJ consumers. Further analysis indicated the odds of asthma among children aged 2–9 years reporting consumption of all EFF beverages (AJ, FD and ndDS) ≥5 times/week was more than five times that of low or non-EFF beverage consumers.
The stronger dose–response seen with the total sum of EFF beverages suggests that the association is with the total cumulative exposure of EFF, rather than something else specific to AJ. A previous study linking AJ to asthma suggested that it may be due to a preservative( Reference Steinman and Weinberg 38 ). Our pattern of results, rather, implicates EFF. These results suggest that total EFF load and cumulative effects of EFF may be important considerations in the association with asthma. The magnitude of the association of asthma with intake of beverages containing EFF in children dictates the need for further investigation.
In contrast, relatively high OJ intake appeared to be protective against asthma. No correlation was significant between EFF intake and asthma in 10–16-year-olds, suggesting, perhaps, that tolerance may occur with age.
The lower association between ndSD intake and asthma, compared with the significantly stronger associations seen with AJ and FD, is likely due to the fact that of all age groups (excluding those aged ≥60 years), children aged 2–9 years are the lowest consumers of ndSD( Reference Ogden, Carroll and Park 39 , Reference Han and Powell 40 ), and fewer children in this age range reported ndSD intake ≥5 times/week relative to AJ and FD. Another potential reason is that the ratio of fructose to glucose is higher in AJ than ndSD. In AJ it is 2:1( 23 ), whereas in ndSD it is from 1·35:1( 23 ) to 1·8:1( Reference Ventura, Davis and Goran 22 ). Therefore, limited exposures to ndSD alone may not contribute to enFruAGE formation necessary to reach the Lowest Observed Adverse Effect Level needed for an observable immune response.
Adjusted odds of asthma in FD drinkers aged 2–9 years followed a similar pattern, albeit less significant, to that seen with AJ, with a similar plateau. The higher association between FD and asthma, as compared with ndSD and asthma, may be because many varieties of FD contain AJ as well as HFCS and therefore are likely to contain higher EFF than ndSD. The opposite tendency towards no association with orange or grapefruit juice further supports the hypothesis that EFF may be responsible for the relationship with asthma. As post-pasteurization vitamin C is comparable in OJ and AJ( 23 ), significant differences in antioxidant properties between these beverages are unlikely to explain the observed differences. Importantly, the ratio of fructose to glucose in OJ and grapefruit juice is about 1:1( 23 ). Therefore, from an EFF perspective, AJ, FD and ndSD are more closely comparable than are OJ and AJ. Notably, very few unprocessed foods are known to contain high EFF; exceptions include apples, watermelons, mangos and pears( 23 ).
The question of how much EFF is too much, and how much EFF is in a serving of AJ, FD and ndSD, warrants further investigation. An important concept is the difference between total fructose load and EFF. This distinction is important because FM – which could contribute to enFruAGE-related asthma – is seen only with EFF or plain fructose challenges, but not with sucrose or solutions containing equal parts fructose and glucose, even when the total amount of fructose intake is the same( Reference Riby, Fujisawa and Kretchmer 12 – Reference Jones, Burt and Dowling 21 ).
According to the US Department of Agriculture’s National Nutrient Database for Standard Reference (NDB) Release 26, the total fructose in 100 g of cola is 6·1 g; in AJ it is 6·4 g and in OJ it is 4·5 g( 23 ). However, their EFF contents are quite different. Cola and AJ contain significantly more EFF than OJ. Specifically, the EFF content in a 237 ml (8 fl oz) cup of cola is 3·9 g (NDB No. 14148), in AJ it is 9·3 g (NDB No. 09400) and in OJ it is 0·4 g (NDB No. 09207)( 23 ). Per 237 ml (8 fl oz) cup, cola contains 10·5 times more EFF than OJ and AJ contains twenty-five times more. A similar sugars breakdown was unavailable for FD in the NDB, and it is likely to vary across types. Another important consideration is that the amount of EFF in cola, as reported in the NDB, is based on the assumption that the HFCS used to sweeten cola is 55 % fructose and 45 % glucose. However, independent laboratory tests have challenged this assumption( Reference Ventura, Davis and Goran 22 ), suggesting the need for further testing. To answer the question whether pre-existing AGE in beverages could explain the association between AJ, FD and ndSD with asthma, we compared reported AGE content of beverages( Reference Uribarri, Woodruff and Goodman 10 ) and found that most beverages contain relatively low levels, with no significant AGE measurement differences between beverages that could explain our results.
On the other hand, it is possible that malabsorbed fructose can react with peptides present in the lumen of the intestine. The high pH of the jejunum may favour the local formation of AGE (enFruAGE). At physiological pH, a higher percentage of fructose than glucose is in the open chain form, explaining why fructose is significantly more reactive than glucose( Reference Wrolstad 41 ). Moreover, using animal models, researchers have recently pointed to evidence of up-regulated expression of AGE and RAGE in the small intestine( Reference Chen, Zhao and Gregersen 42 ). Also, morpho-mechanical intestinal remodelling in type 2 diabetic GK rats points to enAGE formation in the jejunum( Reference Zhao, Chen and Gregersen 43 ).
To answer the question whether a nexus exists between high EFF intake and the well-studied associations between eczema and asthma in young children, we examined possible correlations between EFF intake and eczema. No significant associations were found (data not reported).
The popularity of fructose lies in part in its sweetness; fructose is approximately twice as sweet as glucose( Reference Bovard 44 ). In the context of HFCS, less is required to achieve the same sweetness of sucrose – a key factor driving its popularity and status as a preferred sweetener among US food manufacturers. Recent estimates show that US average per capita consumption of HFCS is just under 0·45 kg (1 lb) per week, down from its 1999 peak of over 0·45 kg (1 lb) per week( 45 , Reference Marriott, Cole and Lee 46 ).
Advocates of the use of HFCS as a viable sweetener and alternative to cane/beet sugar argue that fructose metabolism is the same irrespective of how it is consumed – that HFCS should not be singled out in the association between sugar-sweetened beverages and obesity, diabetes and other chronic diseases. After all, empty calories are empty whether they are from added HFCS or sucrose or other sugars. However, the science behind sugars, fructose and EFF is not that simple. The strong association revealed in the present study between increased intake of EFF and increased odds of asthma in young children, independent of age, sex, race/ethnicity, BMI and total energy intake, suggests that the question to be asked – at least in the context of EFF-associated asthma – may not be one of metabolism but of pre-metabolism.
Conclusion
In conclusion, our results support the hypothesis that intake of beverages containing EFF is associated with asthma in children. Results provide epidemiological support for the mechanistic hypothesis that enFruAGE may be an overlooked source of pro-inflammatory AGE, which play a role in asthma pathogenesis in young children. Results are consistent with the hypothesis that unabsorbed EFF and FM may underlie formation of AGE within the digestive tract (enFruAGE). Once absorbed, enFruAGE may enter the systemic circulation and activate RAGE – a central mediator of asthma. Further epidemiology research and longitudinal studies are needed. Biochemical research is also needed to confirm and clarify the mechanisms involved.
Acknowledgements
Acknowledgements: The authors wish to thank Anelia Persad, student of medicine at NY Medical College, Valhalla, NY, for her assistance in data pre-processing and data set construction. Financial support: This analysis received no specific grant from any funding agency in the public, commercial or not-for-profit sectors. Conflict of interest: None. Authorship: L.R.D.C. researched and developed the biochemical hypothesis, designed the epidemiology research, performed the analyses and drafted the manuscript; J.U. reviewed the analyses and helped to write the manuscript; K.L.T. reviewed all statistical analyses in detail and contributed to writing the manuscript. All authors read and approved the final manuscript. Ethics of human subject participation: Ethical approval was not required.







