As societies develop, the spectrum of diseases and number of deaths in urban residents undergo dramatic changes, and chronic diseases have become an important public health issue threatening residents’ health(Reference Liu and Sun1). Chronic non-communicable diseases (NCD), including heart disease, stroke, cancer, diabetes and chronic lung disease, are collectively responsible for almost 70 % of all deaths worldwide(2). Furthermore, NCD are more severe in low-and-middle-income countries, accounting for almost three quarters of all NCD’ deaths and 82 % of the 16 million people who die prematurely or before reaching age 70 years in low-and-middle-income countries(3). In China, due to the increased prevalence, the total number of deaths from NCD have increased, with 17 % of people dying prematurely from any of cardiovascular diseases, cancers, diabetes or chronic respiratory diseases(4). The high morbidity, disability and mortality from NCD bring about huge sufferings to the patients and their families, with very heavy medical cost. Therefore, the prevention and control of NCD have become an important public health issue(5).
Previous studies in low-and-middle-income countries revealed the impact of demographical and sociological characteristics and lifestyle and environmental exposure on chronic diseases(Reference Lu, Su and Zhang6–Reference Bi, Wang and Ma8). A study from rural India showed age, gender, socioeconomic status and geographical location of residence as predictors of chronic disease prevalence(Reference Kinra, Bowen and Lyngdoh9). A study of six low-and-middle-income countries and upper-middle income countries, including South Africa, Mexico, India, Ghana, Russia and China, revealed that daily smoking, frequent alcohol abuse, low levels of physical activity, insufficient intake of vegetables and fruits, high risk waist-to-hip ratio, obesity and high blood pressure are the main risk factors for chronic diseases(Reference Wu, Guo and Chatterji10). Consistent findings reported in Chinese studies revealed that in Ningxia, a remote province in northern China, gender, age, ethnicity, education, marital status, occupation and source of drinking water are the main influencing factors of chronic diseases among residents(Reference Sun, Wang and Liu11). In another northeastern city—Changchun—survey, age, occupation, physical activity and income are the top five risk factors for chronic diseases(Reference Li, Zhang and Jiang12). With increasing urbanisation and aging, changes in the socio-economic levels and lifestyles of residents have caused great changes in the spectrum, morbidity and mortality of chronic diseases(Reference Luo, Zheng and Lu13,Reference Li, Luo and Zhang14) . However, few of these previous studies have examined the comprehensive impact mechanisms of medical insurance, modern lifestyle, diet quality and other factors on chronic diseases.
Therefore, this study was aimed to determine the prevalence of chronic diseases among the population in the surveyed area, explore their influencing factors and identify the underlying mechanisms among Shanghai, a highly urbanised city with well-developed social services. The results of this study are expected to provide updated and innovative evidence for the prevention and control of chronic diseases, especially in urban cities in developing countries.
Methods
Data sources
The data we used were from the survey of chronic diseases by Shanghai Center for Disease Control and Prevention in 2016. This survey included 1005 residents from 240 households in all 12 community streets in Yangpu District, Shanghai, and 20 households were randomly selected from each street. The survey was conducted at the household level, and personal questionnaires were used to obtain data from family members. The respondents were community residents who had lived in the targeted district for at least 6 months preceding the survey. The questionnaire was completed by professional investigators, and the information obtained was recorded in the information system.
The survey included four sections: (1) basic family information, including the number of family members, financial status, family diet and fuel usage; (2) basic personal information, including age, sex, education level, marital status, occupation, medical insurance participation and registered permanent residence; (3) personal dietary habits and lifestyles, including food intake, smoking, second-hand smoking, alcohol drinking, salt intake (self-assessment), tea drinking and amount of exercise and (4) personal health status, including weight status (self-assessment), height (actual measurement), weight (actual measurement), blood pressure and presence of chronic diseases. The questionnaire also included related information such as family history of chronic diseases. A total of 1005 completed questionnaires were collected, including 22 questionnaires with inconsistent or illogical responses. Ultimately, 983 valid questionnaires were retained, and the effective rate was 97·81 %.
Measurement
Dietary quality
Most of the existing researches mainly included single nutrients or food composition indicators to measure the dietary structure or quality of residents; these can only reflect a certain aspect of the diet and hardly explain the complexity of the diet(Reference Ren, Li and Cui15). To evaluate the overall dietary quality and diet structure, this study comprehensively considered the problem of insufficient and excessive dietary intake and quantified the degree based on Chinese Diet Balance index(Reference He, Zhai and Ge16), which can better evaluate the dietary quality of Chinese adults.
Diet Balance Index_16 (DBI_16) is composed of eight food group level indicators, including cereal, fruits and vegetables, dairy, soybean, animal food (red meat and products, poultry and game, aquatic products, eggs), pure heat food (cooking oil and alcoholic beverage), condiments (added sugar and salt), diet variety and water. If the water quantity data is missing, such was excluded from the analysis(Reference He, Zhai and Ge16). The individual indicator in each group were set according to eleven energy levels, and the specific values were based on the revised standards of China’s Dietary index(Reference He, Fang and Xia17). The DBI score is used to calculate the high bound score, low bound score, total score (TS) and diet quality distance from the eight indicators. High bound score was calculated by adding the positive scores of all indicators to indicate the degree of dietary overconsumption; low bound score, the absolute value of the sum of the negative points of all indicators, reflects the degree of insufficient dietary intake; TS, the sum of the scores of all indicators, reflects the average level of the overall dietary quality; while diet quality distance, the sum of the absolute values of each indicator, comprehensively reflects the problems with a particular diet.
Using the DBI_16 evaluation method, the average daily food intake of each group was first calculated, and the energy intake was calculated according to the food composition table 17. The DBI_16 index score of each person was then calculated according to the DBI_16 scoring method to derive the DBI_TS, Diet Balance Index high bound score and Diet Balance Index low bound score. To better reflect the average level of the dietary quality, DBI_TS was selected as the proxy variable of dietary quality in this study. Negative DBI_TS implied undereating by the people on the average; positive DBI_TS implied overeating on the average; while zero DBI_TS does not necessarily imply a balanced diet, but may mean that the degree of overeating and undereating of different kinds of food is equal; hence, they cancel out. DBI_TS ranges from –72 to 44. According to the quartile, the Dietary quality was classified into four categories: dietary under intake (DBI_TS ≤ –14), mild dietary under intake (–14 < DBI_TS ≤ 0), mild overeating (0 < DBI_TS ≤ 8) and overeating (DBI_TS > 8).
Amount of exercise
Individual physiological load of exercise was measured according to the international general Physical Activity Index (PAI)(18). Housework, working activities (reading, writing, reporting, etc.), outdoor activities (running, swimming, ball games, etc.) and other different types of exercise were assigned 0·85–9 points per hour and multiplied by the corresponding time to calculate the PAI. According to the quartile, the PAI was classified into four categories: appropriate amount of physical activity (PAI < 12·8), mild overexercise (12·8 < PAI ≤ 17·1), moderate overexercise (17·1 < PAI ≤ 22·5) and severe overexercise (PAI > 22·5).
Assessment of chronic disease status
Participants were asked to report only NCD that were once diagnosed by medical staff. Hypertension, diabetes, dyslipidemia or hyperlipidemia, chronic kidney disease, cardiovascular and cerebrovascular events were provided as examples. No chronic disease was recorded as ‘0’ and having one or more chronic diseases were recorded as ‘1’.
Statistical analysis
The data collected were recorded in Information Collection Management Platform by investigators, analysed using IBM SPSS version 23.0; Stata version 13.0 and R version 2.8.1, and reported in frequency distribution tables. Chi-square test, logistic regression analysis and mediating effect test were performed. Chi-square tests and non-conditional logistic regression analysis were used to identify factors associated with chronic disease. Addition and multiplication interaction models were used to analyse the interaction of different risk factors on chronic disease. The synergy index (S), relative excess risk due to interaction and attributable proportion due to interaction were calculated with reference to the interaction calculation table compiled by Andersson et al., and determined whether there is additive interaction(Reference Andersson, Alfredsson and Kullberg19,Reference Westreich and Greenland20) . All tests were bilateral, and P < 0·05 was considered statistically significant.
The mediating effect model was used to further test whether medical insurance influenced chronic diseases through dietary quality, exercise and tea drinking variables. Taking dietary quality (DBI_TS) as an example to explore the influence mechanism of residents’ participation in medical insurance on chronic disease. DBI_TS was the mediation variable (reported as a continuous variable), the independent variable was types of health insurance that residents participate in (reported as a categorical variable), while the dependent variable, having or not having chronic disease, was a dichotomous variable. The specific models are as follows:
In the mediation analysis, where the mediating variable or dependent variable was a categorical variable, the usual linear regression analysis was replaced by the logistic regression analysis(Reference Liu, Luo and Zhang21–Reference Perignon23). Since the dependent variable was a categorical variable, equations (2) and (3) for logistic regression analysis were adopted. Since the mediating variable was a continuous variable, the linear regression analysis in equation (1) was used(Reference MacKinnon24–Reference MacKinnon, Lockwood and Brown26). The same was true for the analysis that medical insurance affected the risk of chronic disease by influencing the amount of exercise or tea consumption of residents.
The RMediation software package in R was used to calculate the CI for the mediation variable statistics. The significance level was set at P < 0·05 for all the tests. Since the family history of chronic diseases was a perfect predictor of chronic diseases, it was automatically omitted from the multiple logistic regression model. Considering that members from the same family are more similar in diet and other living habits, individuals with a family history of chronic diseases are more likely to experience chronic diseases. Therefore, family history of chronic diseases was not discussed in the follow-up analysis.
Data quality
Myer’s blended index is a method used to estimate the quality of survey data based on the age distribution of the participants. The index score ranges from 0 to 99 and cannot be greater than 60, otherwise, that indicates a serious quality problem with the survey demographic data. In general, errors while completing the question on age may occur due to ‘number preference’ and ‘age heaping’, and several participants tend to report the last digit of their ages as 0 or 5(Reference Susuman, Hamisi and Lougue27). In this study, the Myer’s blended index of the survey data was 4·49, indicating that there was no data heaping; thus, confirming the overall validity of the data collected.
Results
Socio-economic and demographic characteristics
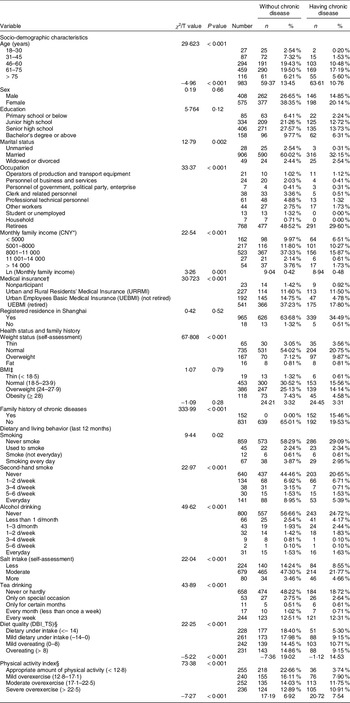
As shown in Table 1, most respondents were aged 61–75 years (46·69 %), women (58·49 %), graduated from senior high school (41·30 %), married (92·17 %), retired (78·13 %), enjoyed Urban Employees Basic Medical Insurance and retired (55·04 %), and were registered Shanghai residents (98·17 %). In terms of the health status, 74·77 % of the respondents evaluated themselves as having normal weight, while the BMI showed that 46·41 % of the respondents actually had normal BMI level, and 51·64 % of the respondents were above normal BMI level. Of the 983 respondents, 34·99 % had chronic diseases and 84·54 % had a family history of chronic diseases.
Table 1 Socio-demographic characteristics of the respondents (n 983)

* CNY: Chinese Yuan (currency unit). The average exchange rate between USD and the CNY in 2016 was 6·6423.
† Since 2016, China has started the merger of New Rural Cooperative Medical Insurance System and Urban Residents Basic Medical Insurance, collectively referred to as URRMI. Due to the availability of data and the convenience of interpretation, the two were combined in this study. In addition, since the reimbursement ratio of urban employees after retirement is significantly higher than that before retirement, the UEBMI can be divided into two groups (not retire v. retired) according to China’s statutory retirement age (males retire at the age of 60 and females retire at the age of 50).
‡ BMI was calculated by the actually measured height and actually measured weight, and was divided into six categories according to guidelines for the prevention and control of overweight and obesity in adults in China.
§ Classified by quartile.
Univariate analysis of chronic disease risk factors
The univariate analysis results showed that age, marital status, occupation, monthly family income, medical insurance, weight status (self-assessment), family history of chronic diseases, smoking, second-hand smoking, alcohol drinking, salt intake(self-assessment), tea drinking, diet quality (DBI_TS) and PAI were associated individually with chronic diseases (all P < 0·05; Table 2).
Table 2 Socio-demographic characteristics, health status, lifestyle and chronic diseases (n 983)

* CNY: Chinese Yuan (currency unit). The average exchange rate between USD and the CNY in 2016 was 6.6423.
† Since 2016, China has started the merger of New Rural Cooperative Medical Insurance System and Urban Residents Basic Medical Insurance, collectively referred to as URRMI. Due to the availability of data and the convenience of interpretation, the two were combined in this study. In addition, since the reimbursement ratio of urban employees after retirement is significantly higher than that before retirement, the UEBMI can be divided into two groups (not retired v. retired) according to China’s statutory retirement age (males retire at the age of 60 and females retire at the age of 50).
‡ BMI was calculated by the actually measured height and actually measured weight, and was divided into six categories according to Guidelines for the prevention and control of overweight and obesity in adults in China.
§ Classified by quartile.
Logistic regression analysis of chronic disease risk factors
The results of the logistic regression analysis, including significant variables in the chi-square test are shown in Table 3. Age, tea drinking, diet quality (DBI_TS) and PAI were significant influencing factors of chronic diseases. Among these factors, a higher prevalence of chronic disease was related to older age, drinking tea more often, more unbalanced diet and more excessive exercise.
Table 3 Logistic regression analysis of chronic disease risk factors (n 962)

* Adjustment variables include gender, education, marital status, occupation, medical insurance, ln (monthly family income) and registered residence in Shanghai or not.
Specifically, logistic regression analysis showed that, in the case of adjusting relevant variables, the risk of chronic disease of residents aged 46–60, 61–75 and > 75 were 6·88 times (95 % CI: 1·47, 32·21), 8·54 times (95 % CI: 1·80, 40·56) and 10·21 times (95 % CI: 2·02, 51·52), compared with residents aged 18–30. Compared with those never or hardly drank tea, the risk of chronic disease was 1·84 times (95 % CI: 1·30, 2·61) for those who drank tea weekly. Compared with the Dietary under intake (DBI_TS ≤ –14), the risk of chronic disease in the population with mild overeating (0 < DBI_TS ≤ 8) or overeating (DBI_TS > 8) were 2·04 times (95 % CI: 1·32, 3·16) and 1·76 times (95 % CI: 1·13, 2·74). Relative to residents with appropriate amount of physical activity (PAI < 12·8), the risk of chronic disease in mild overexercise (12·8 < PAI ≤ 17·1), moderate overexercise (17·1 < PAI ≤ 22·5) and severe overexercise (PAI > 22·5) group were 2·34 times (95 % CI: 1·47, 3·74), 4·13 times (95 % CI: 2·61, 6·53) and 4·42 times (95 % CI: 2·75, 7·11), respectively (Table 3).
Interaction analysis of chronic disease risk factors
As shown in Table 4, there were both multiplicative interactions (P = 0·003) and additive interactions between excessive exercise (PAI > 17·1) and tea drinking on the occurrence of chronic diseases. The risk factor variables were converted into dichotomous variables, and their product items were included in the logistic regression model. After adjusting the relevant variables, the results showed that residents with excessive exercise (PAI > 17·1) and tea drinking had a lower risk of chronic disease than residents with relatively low exercise (PAI < 17·1) and no tea drinking (OR = 0·40, 95 % CI: 0·22, 0·72), and the risk of chronic disease when the two exist together was lower than the sum of the risk caused by the two factors alone (relative excess risk due to interaction = –5·97, attributable proportion due to interaction = –15·06, S = –0·11), that is, there was negative interaction. There was no multiplicative interaction between age > 60 and overeating (DBI_TS > 0) on the occurrence of chronic disease, but there was additive interaction (relative excess risk due to interaction = –2·47, attributable proportion due to interaction = –4·00, S = –0·18). The risk of chronic disease in people with age > 60 and overeating was lower than the sum of the risk caused by the two factors alone, that is, there was negative interaction. In addition, there was no additive or multiplicative interaction between the combination of other risk factors and the risk of chronic disease.
Table 4 Interaction analysis of chronic disease risk factors (n 962)

* Adjustment variables include gender, education, marital status, occupation, medical insurance, monthly family income and registered residence in Shanghai or not.
Medical insurance and chronic diseases: an analysis of the mediating effects of diet quality
Table 5 presents the results of the mediation effect analysis. Models 1, 3, 5 and 7 were the results of logistic regression, and Models 2, 4 and 6 were the results of linear ordinary least squares (OLS) regression (although the frequency of tea drinking is actually a classification variable, for the sake of simplicity of analysis, when the number of classification levels of the classification variable is greater than or equal to 5, it can be regarded as a continuous variable and put into the OLS regression equation(Reference Fang, Wen and Zhang28)). Taking the mediating effect of DBI_TS on medical insurance and chronic disease as an example, Model 2 showed β
1 = –2·36, se (β
1) = 0·66, and
![]() ${Z_{{\beta _1}}}$
= –3·58. Model 3 showed ϕ2 = 0·02, se (ϕ2) = 0·01, and
${Z_{{\beta _1}}}$
= –3·58. Model 3 showed ϕ2 = 0·02, se (ϕ2) = 0·01, and
![]() ${Z_{{\varphi _2}}}$
= 2. Finally, using the product distribution method of R mediation software package, 95 % CI,
${Z_{{\varphi _2}}}$
= 2. Finally, using the product distribution method of R mediation software package, 95 % CI,
![]() ${Z_{{\beta _1}}}{Z_{{\varphi _2}}}$
was (–0·097, –0·007), excluding 0. Therefore, diet quality had a significant mediating effect on the relationship between medical insurance and chronic diseases. According to Baron and Kenny causal stepwise regression analysis(Reference Baron and Kenny29), γ1, β1, ϕ1 and ϕ2 were significant (all P < 0·05; Table 5). Further confirming that diet quality was an incomplete mediator of the relationship between medical insurance and chronic disease while medical insurance also influenced chronic illnesses from other pathways. As shown in Table 5, the 95 % CI of PAI and tea drinking did not contain 0, and the corresponding γ1, β1, ϕ1 and ϕ2 were both significant. Therefore, PAI and tea drinking were also incomplete mediators of medical insurance for chronic diseases.
${Z_{{\beta _1}}}{Z_{{\varphi _2}}}$
was (–0·097, –0·007), excluding 0. Therefore, diet quality had a significant mediating effect on the relationship between medical insurance and chronic diseases. According to Baron and Kenny causal stepwise regression analysis(Reference Baron and Kenny29), γ1, β1, ϕ1 and ϕ2 were significant (all P < 0·05; Table 5). Further confirming that diet quality was an incomplete mediator of the relationship between medical insurance and chronic disease while medical insurance also influenced chronic illnesses from other pathways. As shown in Table 5, the 95 % CI of PAI and tea drinking did not contain 0, and the corresponding γ1, β1, ϕ1 and ϕ2 were both significant. Therefore, PAI and tea drinking were also incomplete mediators of medical insurance for chronic diseases.
Table 5 The results of the mediation effect of variables on dietary quality (n 962)

P < 0·05, **P < 0·01, ***P < 0·001.
DBI_TS, Diet Balanced Index total score.
Discussion
In the 2011 World Economic Forum, it was again emphasised that the five chronic diseases (cardiovascular diseases, tumor, diabetes, respiratory diseases and mental diseases) would have a profound impact on the national medical and economic systems in the next 20 years(30). Shanghai has been an aging city since 1999, and the disease spectrum of the residents has changed greatly; furthermore, the prevention and treatment of chronic diseases in the elderly is facing severe challenges(Reference Zhao, Wang and Yan31). In this study, the survey showed that 34·99 % of the investigated residents in Yangpu District of Shanghai suffered from chronic diseases. This higher prevalence, compared to that at the national level, could be explained by the relatively complete community-level health service system in Shanghai, which makes it possible to diagnose chronic diseases of community residents more timeously. In addition, Shanghai, being the financial center of China, regular overtime work by the residents and higher work pressure, may have contributed to the high prevalence of chronic diseases, to some extent(Reference Müller, Anita and Marti32–Reference Sheng, Zheng and Fei34).
To prevent and control chronic diseases effectively, nutrition, diet and exercise are the key factors. Imbalanced diet, including overeating, is a major contributor to chronic diseases. Compared with normal dietary intakes, people who eat excessively are at higher risks of chronic diseases, which is consistent with the findings of previous studies(Reference Patel, Nossel and Alexander35–Reference Mills, Thomas and Larkin37). With changes in diet structure, the consumption of refined cereals increases, and long-term consumption causes insufficient intake of vitamins, minerals, dietary fibre, etc(Reference Su, Yang and Liu38). Excessive intake of high-sodium food also increases the risk of chronic diseases(Reference Tian, Ma and Jia39). Consistent with the conclusion of previous studies, the older the person, the higher the risk of chronic diseases(Reference Xu40). However, in this study, it was found that there was negative additive interaction between age > 60 and overeating (DBI_TS > 0) on chronic disease, which may be due to deviation in the measurement of diet quality by DBI_TS. DBI_16 is generally suitable for the dietary evaluation of adults. The elderly (age > 60) have very different nutritional requirements from normal adults due to their special physiological characteristics(Reference He, Zhai and Ge16). In addition, continuous variable DBI_TS may have a U-shaped relationship with the risk of chronic disease, which needs to be further explored in future studies. However, healthy food habits are always protective factors for chronic diseases. Eating reasonably is the basis of human health, and nutrient deficiency or excess may occur with long-term insufficient or excessive nutrient consumption(Reference Ma, Sha and Tan41–Reference You, Yuan and Li44). Moreover, dietary nutrition has a long-term impact on health, and unreasonable dietary structure and pattern are facilitating factors for the occurrence of chronic diseases(Reference Chia, deSeymour and Colega45–Reference Monneuse, Bellisle and Koppert47).
Considering other aspects of diet habits, the high frequency of tea drinking increases the risks of chronic diseases. A prospective cohort study conducted in Zhejiang Province showed that moderate tea consumption could reduce the risk of stroke(Reference Wang, Du and Hu48). However, an epidemiological investigation on the incidence of diabetes in Changsha City suggested that patients with gout or hyperuricaemia should not drink tea(Reference Tang, Xia and Wu49). Although the caffeine content of different teas varies depending on the production place, type and processing technic, Chinese consumers preferred more traditional tea varieties containing caffeine, such as green tea, black tea and oolong tea(50).Long-term excessive drinking of tea results in the over accumulation of caffeine in the body. This impairs the nervous and digestive system functions, increases the burden on the kidneys, and results in nervousness, fatigue and discomfort, headache and other symptoms in people(Reference Gao and Tao51).
With physical activity, excessive exercise also increases the risk of chronic diseases, as it can lead to cardiovascular events, musculoskeletal injuries, upper respiratory infections, gastrointestinal symptoms or sudden death due to multi-organ system failure(Reference Liu, Wang and Zeng52,Reference Wang, Su and Xie53) . However, there were negative additive and multiplicative interactions between PAI greater than 17·1 and tea drinking on the occurrence of chronic diseases. May be associated with the increase of physical activity intensity, there will be internal organs, muscles and nervous fatigue, the tea polyphenols can promote metabolism, accelerate liver detoxification and the caffeine, tea polysaccharide, amino acid and other nutrients can strengthen physique and eliminate fatigue(Reference Li54,Reference Zhou55) . Thus excessive physical activity combined with tea drinking reduced the risk of chronic diseases. It is likely that there is a U-shaped relationship between physical activity and chronic disease risk, which needs to be further analysed in future studies.
In addition, higher reimbursement level of medical insurance reduces the risk of chronic diseases, which is supported by a natural experiment, which showed that switching from Urban Residents Basic Medical Insurance to Urban Employees Basic Medical Insurance significantly improved health(Reference Zhou, Deng and Liu56). In fact, in the current social basic medical insurance system in China, the urban employee compensation rate and maximum compensation amount are higher than those for urban and rural residents. Therefore, it is more likely for people with Urban Employees Basic Medical Insurance to utilise medical services due to the higher reimbursement value, which indirectly affects the residents’ health(Reference Ma, Gu and Sun57). The mediating effect analysis on the impact of medical insurance on chronic disease showed that residents with higher reimbursement level of medical insurance had lower DBI_TS and PAI and less frequent drinking of tea. This is inconsistent with previous research conclusions, which believe that while medical insurance increases the accessibility of medical services, it may also lead the insured to reduce their investment in preventing disease risk before getting ill, thus leading to ‘ex-ante moral hazard’(Reference Peng and Qin58). In this study, residents who participated in high-reimbursement health insurance were likely to be more risk averse and therefore focused more on eating a balanced diet and exercising reasonably, as well as limiting caffeine intake in tea, thereby reducing the probability of chronic disease, which further proved the robustness of the conclusion that participation in high-reimbursement health insurance can reduce the risk of chronic disease.
There are several limitations to this study. First, it was conducted in one district of Shanghai, due to the possible sampling bias, the respondents age showed a large proportion of aging. Therefore, the application of the findings to other areas needs to be done with caution. Second, we were unable to assess for the presence of undiagnosed chronic diseases in the population, and some answers were recalled and reported by participants, which could cause recall bias and response biases. Third, the study design was limited to some extent by the availability of data, and the cross-sectional data made it impossible to demonstrate causality between lifestyle factors and chronic disease. It is also a question need to be further explored. In addition, if data on alcohol consumption and severity of chronic diseases are available, further studies can be conducted in the future.
In conclusion, the proportion of residents suffering from chronic diseases in Yangpu District was relatively high. The age, diet habit, tea drinking habit and the amount of exercise were main risk factors of chronic diseases. Health insurance improved residents’ access to medical services. But contrary to the conclusions of previous studies, this study proved that there was no ex-ante moral hazard of medical insurance among the surveyed residents. To facilitate the prevention and control of chronic diseases, the community residents should be encouraged to develop balanced eating habits and healthy exercise behaviours. In addition, the government should focus on improving the nutritional environment of old people, strengthening access to health education, coordinate different types of medical insurance to promote access to health services by the residents.
Acknowledgments
Acknowledgments: Thanks for the questionnaire and data support provided by Shanghai Yangpu District CDC. Financial support: The design of this study involving some previous investigation was supported by the Natural Science Foundation of China (71603182, 71774116, 72104140 and 82101870). Data extraction was financially funded by the National Key R&D Program of China (2018YFC2000700). The analysis and interpretation of the data guided by the statisticians were funded by the Shanghai Pujiang Program (2019PJC072, 21PJC083 and 2020PJC081), the Shanghai Health System Outstanding Talents Program (2018YQ52) and the Shanghai Public Health Outstanding Young Personnel Training Program (GWV-10·2-XD07). The writing and revision, including the language improvement, were sponsored by Zhejiang Provincial Natural Science Foundation of China (LQ21H100001), Soft Science Project of Shanghai Science and Technology Innovation Action Plan (21692191300) and Connotation Foundation of Shanghai Jiao Tong University School of Medicine (17ZYGW12). Conflict of interest: There are no conflicts of interest. Authorship: Y.Y. interpreted the data and drafted the manuscript. H.J. and P.Z. analysed and interpreted the data. M.C. has made substantial contributions to conception and design. X.L. revised the manuscript. Z.C. and X.G. acquired of data. L.Z., Y.Lv., J.H. and N.C. analysed and interpreted the data. W.Y., Z.W. and J.S. involved in analysis and interpretation of data, revising the manuscript and given final approval of the version to be published. Ethics of human subject participation: This study was approved by the ethics committees of Tongji University (ref: LL-2016-ZRKX-017). Official permission was obtained from selected hospitals and health centres. Confidentiality was kept and informed verbal consent was obtained from each study participants after explaining the purpose of the study. Verbal informed consent was approved by the Tongji University Research and Ethics Committee. This research was carried out in accordance with the principles of the Declaration of Helsinki.