Adequate Ca consumption throughout childhood and adolescence is essential to achieve peak bone mass and reduce the risk of bone deformities and osteoporosis in later life(Reference Huth, DiRienzo and Miller1,Reference Pettifor2) . However, approximately 40 % of Canadian children aged 4–8 years fail to meet the recommended dietary allowance (RDA) of Ca (1000 mg/d). Furthermore, the percentage of individuals meeting the RDA decreases as children reach adolescence(Reference Vatanparast, Islam and Patil3). Dairy products are key to achieving the RDA of Ca(Reference Gao, Wilde and Lichtenstein4) due to a high concentration of absorbable dietary Ca(Reference Heaney5) while also providing children with essential macro- and micronutrients(Reference Dror and Allen6). Yet, 37 % of Canadian children aged 4–9 years do not consume the recommended two daily servings of milk and milk alternatives(Reference Garriguet7), with similar patterns reported in the USA(Reference Quann, Fulgoni and Auestad8), Australia(Reference Baird, Syrette and Hendrie9) and Europe(Reference Dror and Allen6). With the recent change to Canada’s food guide(10), and the move away from specifying the amount of each food group that should be consumed, it is predicted that further decline in Ca intake will be seen in Canadian children(Reference Barr11). As such, there is a need for effective interventions that ensure that Canadian children meet the RDA of Ca.
Parents represent one medium through which to promote Ca intake in children as they play a crucial role in the development of children’s eating behaviour and food preferences(Reference Patrick and Nicklas12). Wansink(Reference Wansink13) estimated that 72 % of the food consumed by children is controlled by parents, therefore coining them the ‘nutritional gatekeepers’ who control what food is purchased for the home, the meals prepared in the home and the food that is packed for consumption outside the home. Availability of Ca-rich food in the home significantly influences children’s Ca intakes(Reference Banna, O’Driscoll and Boushey14,Reference Larson, Story and Wall15) . In addition, children learn through observation and emulation of parental behaviour, including eating habits. Specifically, when mothers drank and served milk frequently in front of their daughters (aged 5–9 years), the girls were more likely to meet the RDA of Ca(Reference Fisher, Mitchell and Smiciklas-Wright16). Similar results were reported in children aged 10–18 years(Reference Banna, O’Driscoll and Boushey14,Reference Neumark-Sztainer, Hannan and Story17) .
In a review of interventions aimed at increasing dairy food and/or Ca intake in children aged 5–12 years, Hendrie and colleagues(Reference Hendrie, Brindal and Baird18) identified three studies that incorporated parents in the intervention design. Two of these studies were delivered in the context of reducing children’s BMI through a healthy diet, including increasing intake of low-fat dairy products(Reference Van Horn, Obarzanek and Friedman19,Reference Epstein, Paluch and Beecher20) . Although both interventions reported an increase in the servings of low-fat dairy consumed, children failed to consume enough dairy to meet the RDA guidelines. None of the interventions directly targeted parents’ attitudes and behaviours towards dairy and Ca products.
Given the significant associations between parental consumption behaviour, consumption of meals as a family and children’s eating patterns(Reference Haire-Joshu, Elliott and Caito21,Reference Arcan, Neumark-Sztainer and Hannan22) , directly targeting parents may represent an effective medium through which to increase children’s dietary Ca consumption. Unpublished data from a randomised controlled trial aimed at increasing Ca consumption in Canadian adults aged 30–50 years demonstrated that the more milk and milk products the parent consumed, the more servings of dairy they packed into their children’s lunch box (unpublished data, Jung and colleagues). To our knowledge, no interventions have specifically targeted parents as a means of increasing dietary Ca consumption in children of school age.
To maximise the effectiveness of an intervention, while ensuring a large population reach, the intervention content should be targeted to the population of interest(Reference Keller and Lehmann23). Targeted messages focus on outcomes salient to the population of interest. Social Cognitive Theory provides a framework through which to develop targeted messages(Reference Bandura24). Social Cognitive Theory postulates that an individual’s decision to engage in a behaviour is influenced by the individual’s confidence to perform the behaviour in certain situations (self-regulatory efficacy) and beliefs about the outcomes expected to occur as a result of performing the behaviour (outcome expectations). Social Cognitive Theory has been used to develop targeted interventions which effectively increased volitional dairy consumption in young women(Reference Jung, Martin Ginis and Phillips25) and adults aged 30–50 years(Reference Jung, Latimer-Cheung and Bourne26).
Among Canadians aged 30–50 years, attitudes towards milk and milk products and consumption strategies have been shown to differ in parents compared with non-parents(Reference Jung, Mistry and Bourne27). Building on this, Jung and colleagues(Reference Jung, Bourne and Buchholz28) examined the social cognitions related to dairy product consumption in parents and their children to develop intervention messages, specifically targeted towards parents, that could be used to increase children’s Ca consumption. Parents perceived both positive (e.g. increase overall energy) and negative (e.g. eczema and diarrhoea) physical outcomes associated with consuming dairy products for themselves and their child. Significant barriers to the consumption of dairy included distrust of information and the perceived cost of dairy products. Based on this research, a series of intervention materials were created for use in a population-wide health promotion campaign designed to increase dietary Ca consumption from both dairy and non-dairy sources in children through directly targeting parents(Reference Jung, Bourne and Buchholz28). The aim of the current study was to examine the effectiveness of these targeted intervention messages on the dietary Ca intake of children aged 4–10 years, along with their parents’ dietary Ca intake, purchasing behaviour and psychosocial factors that could impact Ca consumption.
Methods
Study design
The intervention was a parallel two-arm randomised controlled trial comparing Ca-specific messages targeted at parents of children aged 4–10 years to a control condition, who received generic public health messages on children’s Ca consumption. The trial was registered at ClinicalTrials.gov (ID: NCT02591329). Reporting of this trial will follow the Consolidated Standards of Reporting Trials statement(Reference Schulz, Altman and Moher29).
Participants
Parents from across Canada were recruited using study advertisements placed on social media, online forums and discussion groups. Interested parents clicked on a link directing them to a website which provided detailed study information and an online consent form. Upon provision of consent, eligibility was assessed through parents reporting of their child’s age, any restrictions on dairy or Ca intake for themselves or their child and their child’s Ca consumption the previous day using the self-reported ‘Calcium Calculator™’(30). To complete the Ca calculator, parents indicated the number of portions consumed of thirty common dairy and non-dairy foods by their child on the previous day. A portion size was explained for each product. The Ca calculator has been found to provide a valid assessment of dietary Ca intake(Reference Hung, Hamidi and Riazantseva31). This tool was used to determine total mg of Ca consumed by children on the previous day. Eligibility for the study included having a child between 4 and 10 years of age consuming less than the RDA of Ca, and no dietary or religious restrictions on dairy consumption. Recruitment was open for 8 weeks between November and December 2015.
Procedure
All eligible parents, and their children, were randomly assigned in a 1:1 allocation ratio, using a computer-generated randomisation numbers table produced by an external statistician, to either the experimental condition or control condition upon completion of the eligibility survey. The researchers enrolled participants and were aware of group allocation. After randomisation, baseline measure packages were mailed to parents (all measures were completed by the parent; see Fig. 1 for flow of participants through the study). Subsequent measures (weeks 8, 34 and 52) were sent by mail and returned to the researchers using pre-stamped addressed envelopes provided. Participants received a $5 gift certificate for every measures package that was returned to the researcher, up to $20. The intervention was conducted between January and December 2016.
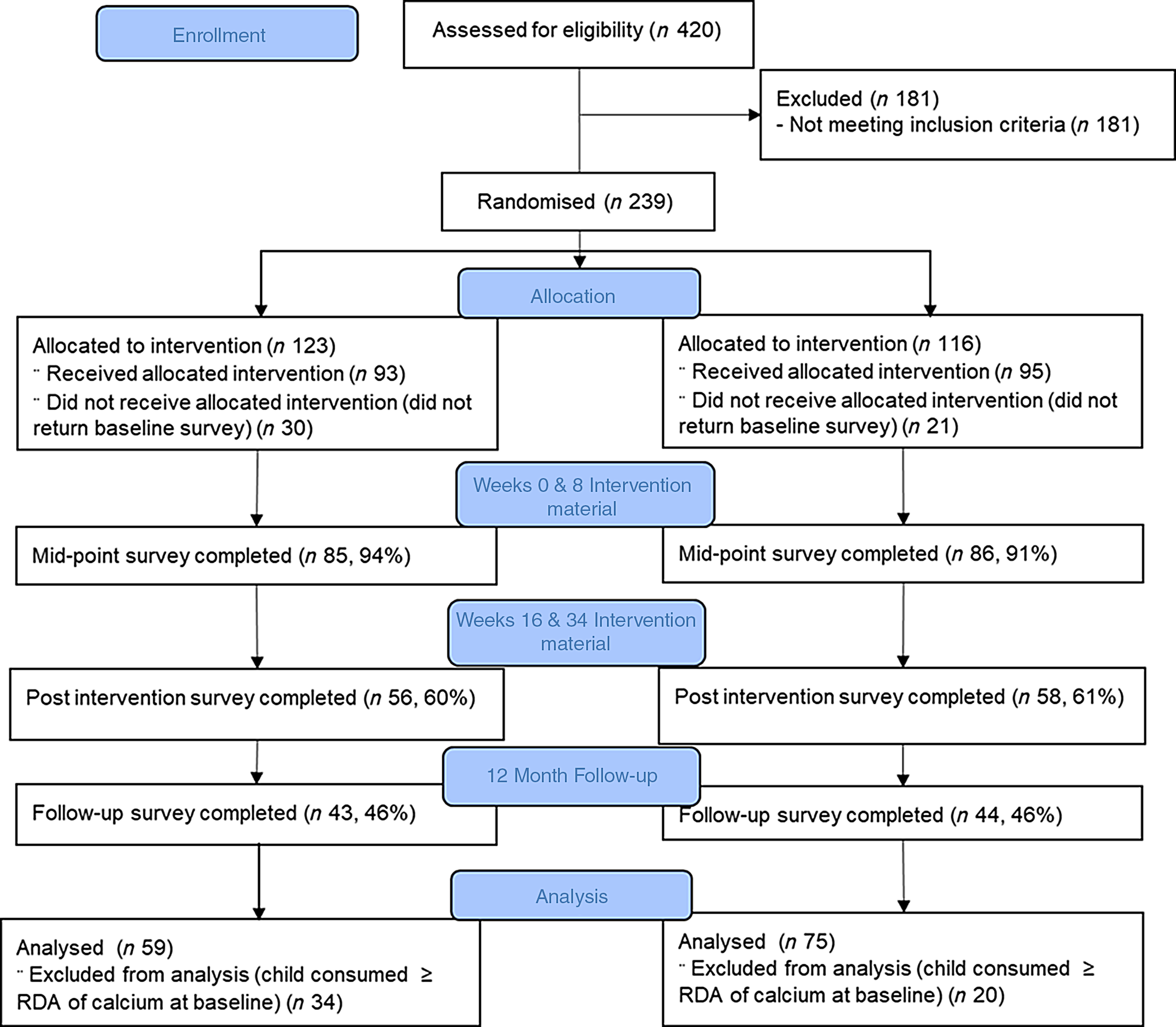
Fig. 1 Consort flow diagram
Strong start together development and content (experimental condition)
The design of the targeted messages is described in detail elsewhere(Reference Jung, Bourne and Buchholz28). To summarise, group interviews were conducted with eleven mothers and seven fathers of children who consumed above and below the RDA of Ca to identify salient benefits and barriers to the purchase and consumption of Ca-rich products. In addition, these discussions aimed to identify purchase and consumption strategies used by parents to promote the consumption of Ca-rich products and a healthy diet in general for themselves and their children. Appropriate channels through which to disseminate information were ascertained. The interviews guided the development of intervention messages. Messages were tested in a second round of interviews with ten mothers and two fathers of children who did not consume the RDA of Ca. Parents were asked whether they found the message content useful and if they would pay attention to the message. Final message content was determined following these interviews.
Intervention messages included information on the benefits of Ca consumption. Barriers to dairy consumption were addressed via a series of phrases designed to contradict these beliefs in the form of a ‘myth busters’ sheet. Information included in the messages was verified by a registered dietitian. Messages contained strategies to assist with planning purchases, reading nutrition labels and reducing costs, suggestions on how to make food more attractive to children and advice on involving children in planning and cooking meals. Recipes containing Ca-rich products were provided. Recommended food servings for each food group for adults and children, including dairy, were provided. Table 1 outlines the timeline of message delivery, the methods through which messages were delivered, the focus of the content incorporated into these delivery methods and an example of message content. Intervention material was provided in four postal deliveries at weeks 0, 8, 16 and 34 (see Table 1). Intervention material included a calendar, cartoon food stickers to engage children, food guidelines fridge magnet, kids’ cookbook, a grocery pad and two newsletters. The use of hard copy materials, as opposed to emailed material, was preferred by parents due to a feeling that parents could review the material repeatedly and in their own time(Reference Jung, Bourne and Buchholz28). Parents felt that emailed material would be deleted after a single view.
Table 1 Outline of intervention messages and method of message delivery

Standard care message content (control condition)
Parents in the control condition were provided with messages of a similar length and in the same format as the experimental group messages. These messages pertained to general food guidelines including how to safely cook and store food and tips for increasing consumption of healthy foods. Specific daily intake requirements for all food groups were provided. Messages were delivered via mail at weeks 0, 8, 16 and 34 in formats that included a calendar, stickers of different food characters for children, fridge magnet of Canada’s food guidelines, a physical activity book and two newsletters.
Measures
Demographics
Participants reported their self-identified gender and age, ethnicity, education, employment, marital status, household income and number of individuals living in the house, and their child’s gender and age.
Manipulation check
At each assessment time point, parents were asked to identify the minimum Ca intake requirements for their child, the main theme of the two newsletters and the extent to which they used the material provided.
Primary outcome
Child calcium consumption
Parents’ reports of children’s Ca consumption were assessed using a 3-d food record(Reference Yang, Kim and Hwang32) at baseline, weeks 8, 34 and 52. Food record data were manually entered into ESHA’s Food Processor® Nutrition Analysis software (ESHA Research). The research team developed a protocol for entering dietary information to ensure consistency across different coders. Total Ca consumption over the 3 d was calculated in mg. Average Ca intake across the 3 d was calculated to provide an estimate of mg of Ca consumed per day. In addition, the amount of Ca consumed specifically from dairy products was calculated. At least one full day of diary completion was required for inclusion of a participant’s data in the analysis.
Secondary outcomes
Adult calcium consumption
Parents’ Ca consumption was assessed using a 3-d food record(Reference Yang, Kim and Hwang32) at baseline, weeks 8, 34 and 52. The same procedure was conducted as with child Ca intake to calculate parents’ average mg of Ca consumed each day and the average mg of Ca consumed each day from dairy.
Purchasing of dairy products
The purchase of dairy products was assessed through photographs of grocery receipts and restaurant bills over a 7-d period at baseline, weeks 8, 34 and 52. Participants were asked to send copies of all receipts electronically or in the mail directly to the researchers. The amount of money spent on dairy products was calculated by researchers.
Psychosocial outcomes
All psychosocial outcomes were assessed at baseline, weeks 8, 34 and 52.
Outcome expectations for consumption of dairy for parents
The perceived likelihood of a range of outcomes occurring because of consuming adequate Ca was assessed using a fifteen-item measure. Parents were asked, ‘how LIKELY is it that each outcome in the list below will occur in the next week as a result of consuming adequate calcium?’ Parents were provided a list of outcomes including ‘weight control’, ‘feeling energized’, ‘bloating’ and ‘weight gain’. The items were developed by drawing from previous research(Reference Jung, Latimer-Cheung and Bourne26) and qualitative work examining perceived outcome expectations regarding dairy consumption in parents(Reference Jung, Bourne and Buchholz28). All outcomes were previously highlighted as being of high value to adults(Reference Jung, Bourne and Buchholz28). Responses were scored on a nine-point scale from 1 (very likely) to 9 (very unlikely). The items demonstrated good internal consistency in the current study (α ≥ 0·92).
Outcome expectations for consumption of dairy for child
Parents’ expected likelihood of a range of outcomes occurring in their child because of consuming adequate Ca was assessed using a nine-item measure. Parents were asked, ‘how LIKELY is it that each outcome might occur next week as a result of my child consuming adequate calcium?’. The list of outcomes included ‘improve bone health’ and ‘have more energy’. The items were developed through qualitative interviews with parents examining perceptions of outcome expectations of dairy consumption for their child(Reference Jung, Bourne and Buchholz28). All outcomes were perceived as being of high value to parents(Reference Jung, Bourne and Buchholz28). Responses were scored on a nine-point scale from 1 (very likely) to 9 (very unlikely). The items demonstrated good internal consistency in the current study (α ≥ 0·91).
Self-regulatory efficacy
Parents’ confidence in their ability to plan, monitor and overcome barriers to ensure the purchase and consumption of Ca-rich products was assessed using an eleven-item measure. Each question included the stem, ‘How confident are you that you can…’. Example items include ‘plan ahead so that your child consumes the minimum RDA of calcium’ and ‘remember to purchase enough calcium products at the supermarket even when you are in a rush?’ Responses were scored on a scale of 0 % (not at all) to 100 % (extremely confident) with response options in 10 % increments. Summary scores were created by taking the average for self-regulatory efficacy for purchasing Ca-rich products (four items) and self-regulatory efficacy for ensuring their child’s consumption of Ca-rich products (seven items). The specificity of the time frame (i.e. next week) and action queries in the eleven items aligns with recommendations made by Bandura(Reference Bandura33) and McAuley and Mihalko(Reference McAuley and Mihalko34) for measuring self-efficacy. This measure demonstrated good internal consistency in the current study (α ≥ 0·85).
Social support
The degree to which parents perceived themselves as offering support to their child regarding the consumption of Ca-rich products was assessed using an eight-item measure. This measure was adapted from the Social Support for Diet Survey(Reference Sallis, Grossman and Pinski35). Questions were adapted to pertain to the child’s specific consumption of Ca-rich products. Each question included the instruction: ‘Please rate how often you provided the following to your child last week’. Example items include ‘discussed the importance of consuming calcium products with your child’ and ‘packed calcium-rich foods in your child’s lunch bags’. Responses were scored on a scale from 1 (none) to 5 (very often). Items were summed to provide a score out of 40. This measure demonstrated good internal consistency in the current study (α ≥ 0·71)
Role modelling
Perceived parental role modelling for the consumption of Ca-rich products was assessed using an adapted version of Cullen and colleagues family and peer influences on fruit, juice and vegetable consumption(Reference Cullen, Baranowski and Rittenberry36). This measure was adapted in a similar way to the current study by Draxten and colleagues(Reference Draxten, Fulkerson and Friend37). The current six-item measure asked parents to record ‘Over the past week, how often have you done/said the following when your child is present?’ Example items include: ‘eat calcium rich foods at lunch’ and ‘make positive comments regarding your calcium consumption’. Responses were scored on a scale from 0 (never) to 3 (usually/always). These items were summed to give a total score out of 18. The internal consistency of this measure for the current study was acceptable (α ≥ 0·64).
Sample size
A total of 142 participants were estimated to be needed in each condition to detect a significant within-participant, between-conditions interaction in the primary outcome, consumption of Ca in children(Reference Cohen38). This estimation was based on a two-tailed alpha of 0·05 and 80 % power and expectation of a medium-sized effect (Cohen’s d = 0·50) based on results of a previous Social Cognitive Theory-based intervention aimed at increasing Ca intake in young women(Reference Jung, Martin Ginis and Phillips25). With an anticipated dropout rate of about 30 %, based on a previous intervention aimed at increased Ca consumption in Canadian adults(Reference Jung, Latimer-Cheung and Bourne26), it was estimated that recruitment of 200 parents and their under-consuming children in each condition would provide enough statistical power to detect changes in Ca consumption and dairy product purchasing.
Analytic approach
Data were analysed using SPSS version 24 (IBM Corp.). Descriptive statistics were calculated using means and standard deviations for continuous variables and frequencies and percentages for categorical variables. Differences in the demographic characteristics associated with dropouts at 12-month follow-up (IV = study adherence) were examined using independent t tests and χ 2 tests. Assumption testing was conducted, and log transformations were performed if necessary.
Changes in the primary outcome (child Ca intake) and secondary outcomes were assessed using intention-to-treat linear mixed models using maximum likelihood estimation. These models analyse the longitudinal changes in the outcome variables as a result of the intervention allowing for an unequal number of observations across individuals which is an advantage over general linear models. Linear mixed models also account for the nested data inherent to repeated measurements from the same individual. Fixed effects included treatment group, time and the interaction of group and time. Participants were entered as a random effect. Demographic variables were entered as covariates into the models. The results report regression coefficients, 95 % CI and P-values.
Results
Participant demographics and randomisation effects
Baseline participant demographics are reported in Table 2. There were no significant differences in demographic characteristics, adult and child Ca or dairy consumption or purchasing outcomes at baseline between those who completed 12-month follow-up and those who did not (P > 0·05). Table 3 provides descriptive statistics for behavioural outcomes. Specifically, at baseline, children’s total Ca consumption per day was 743·05 mg (sd = 211·54) and 743·63 mg (213·76) for the experimental and control groups, respectively. Supplementary file 1 provides descriptive statistics for all psychosocial outcomes.
Table 2 Demographic characteristics of the sample at baseline excluding those whose baseline survey indicated their children were consuming adequate calcium
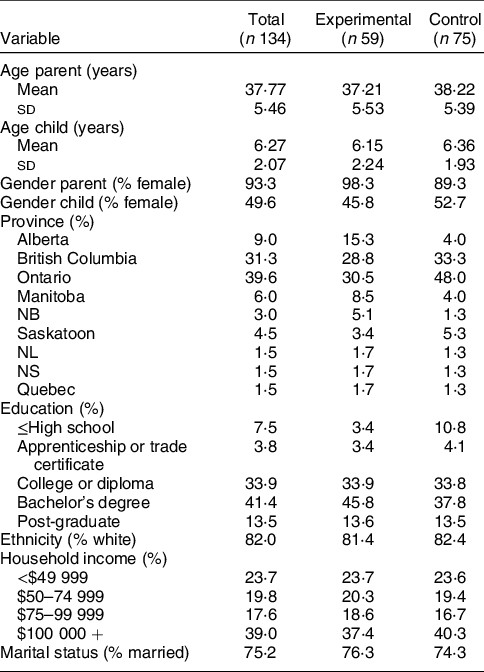
Table 3 Descriptive statistics for milligrams of calcium consumed per day between groups and amount spent of dairy per week
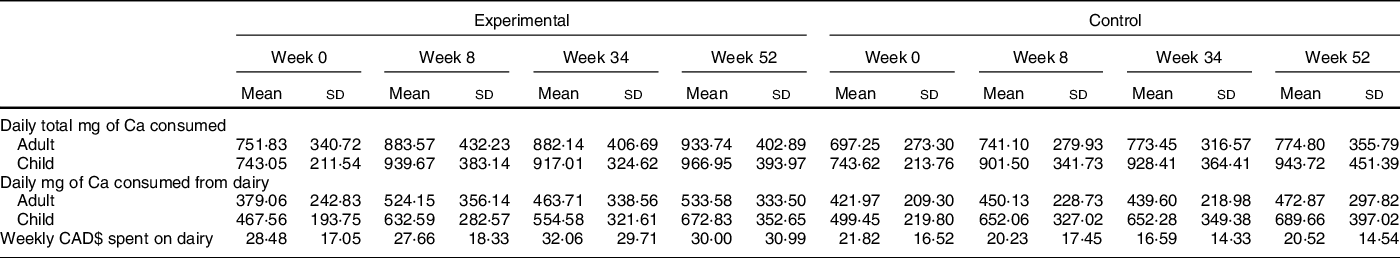
CAD$ = Canadian dollar.
Study attrition
Over the course of 8 weeks, 420 interested parents completed the eligibility survey of which 239 reported that their children were not meeting the RDA of Ca and were therefore deemed eligible to participate in the study. Due to funding and timeline restrictions, it was not possible to extend recruitment further. Two hundred thirty-nine parents were randomised to the experimental or control condition and were sent a baseline survey (Nexp = 123; Ncon = 116). Of these, 188 participants completed and returned the baseline survey (Nexp = 93; Ncon = 95). Eighty-seven (46 %) participants completed follow-up at 12 months (Nexp = 43; Ncon = 44). Reasons for not completing mid, post and 12-month follow-up surveys were not provided. The 3-d food record completed at baseline revealed that several children were already consuming the RDA of Ca. These individuals were excluded from analyses leaving 134 parent and child dyads at baseline (Nexp = 59; Ncon = 75; see Fig. 1 for flow of participants through the study).
Manipulation check
In the experimental condition, at the midpoint of the intervention, 73·5 % and 54·5 % of parents with children aged 4–8 years and >8 years, respectively, correctly identified the minimum Ca intake requirements for their child. Similar results were seen in the control condition with 70·3 % and 55·6 % of parents of children aged 4–8 years and >8 years, respectively, correctly identifying the minimum Ca requirements for their child at midpoint of the intervention. In the experimental condition, 72·5 % of parents reported using the calendar provided and 46 % used the accompanying stickers. In addition, 62·5 % of participants correctly identified the main theme of the third newsletter which focused on providing recipes. In the control condition, 57 % of parents reported using the calendar and 34 % used the stickers. In total, 52·1 % correctly identified the main content of the third newsletter which focused on physical activity.
Effects of intervention on child calcium consumption
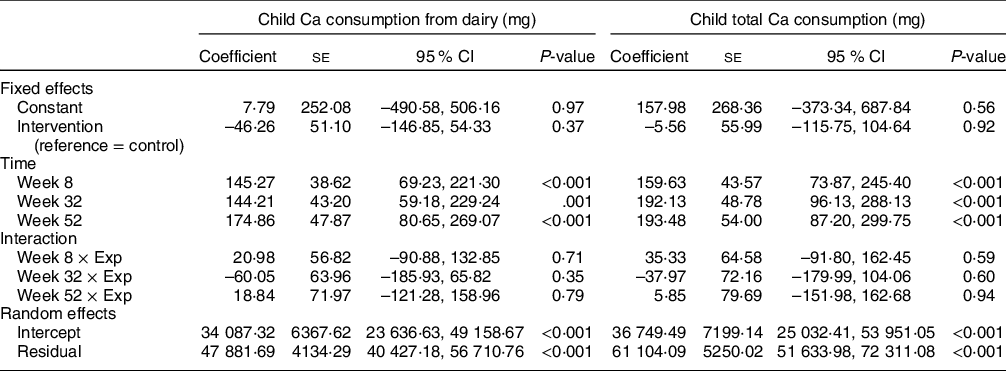
Table 4 shows the estimated effects from the mixed effects linear models for the child total Ca consumption and Ca consumption from dairy. Compared with baseline, there was a significant increase in total Ca consumed and Ca consumed from dairy for children at mid, post and 12-month follow-up (P ≤ 0·01). This increase was similar in the experimental and control conditions (see online Supplemental file 3).
Table 4 Estimated parameters from linear mixed models for child calcium consumption
Effects of intervention on parent calcium consumption and dairy purchasing
Table 5 shows the estimated effects from the mixed effects linear models for parent’s total Ca consumption, Ca consumption from dairy and amount spent on dairy. There was no change in parents’ total Ca consumption or Ca consumption specifically from dairy (P > 0·05). Furthermore, there were no significant differences between conditions. Adjusting for multiple comparisons, post hoc analyses revealed a significant increase in adult total Ca consumption and dairy consumption from baseline to mid-intervention in the experimental condition (P < 0·04). This increase was not maintained over time. There was no change within or between groups in the amount of money spent on dairy specific products (P > 0·05). Across all behavioural outcome models, there were significant variances in outcomes across participants (P ≤ 0·001).
Table 5 Estimated parameters from linear mixed models of adult consumption and purchasing outcomes
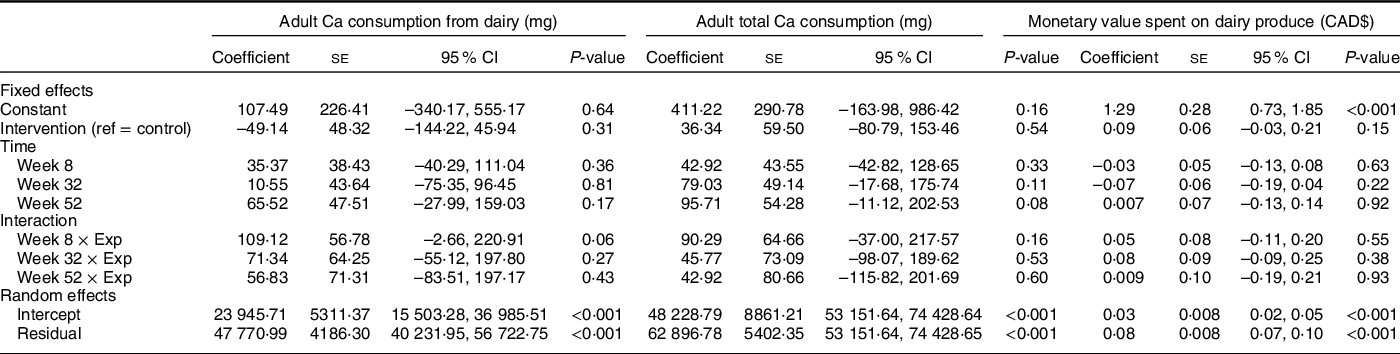
CAD$ = Canadian dollar.
Effect of intervention on psychosocial outcomes
Supplementary file 2 shows the estimated effects from mixed effects linear models for the psychosocial outcomes as dependent variables in the models. The psychosocial outcomes varied significantly across participants (P ≤ 0·001). There were no significant effects of the study condition on any of the psychosocial outcomes (P > 0·05). There were significant increases in all psychosocial outcomes from baseline to immediately post-intervention (week 32), except self-regulatory efficacy for purchasing Ca-rich products (P = 0·70). Furthermore, there was a significant change from baseline to 12-month follow-up (week 52) on all psychosocial outcomes (P < 0·02).
Discussion
The purpose of this randomised controlled trial was to test the effectiveness of a Ca intervention, targeting parents, at increasing Ca consumption in children consuming less than the RDA for Ca. To our knowledge, this is the first study to specifically target parents as a mechanism through which to increase Ca consumption in children. Children’s total Ca consumption increased from baseline to 52 weeks in both the experimental (Δ223·9 mg) and control (Δ200·1 mg) conditions. The level of change equates to approximately one additional serving of dairy per day.
Are targeted messages necessary?
With no difference in children’s Ca consumption between the two conditions, is there a need for public health messages that specifically target a discrete nutrient? Messages in the experimental condition focused on strategies to help parents increase their children’s Ca consumption and outlined the benefits of Ca consumption. Messages in the control condition focused on strategies for consuming a healthy diet with general and non-nutrition-related information. Of note, parents in both conditions received Canada’s food guide daily consumption targets for Ca, dairy and other food groups in the form of a fridge magnet that could have served as a daily prompt to consider their child’s dietary Ca intake. Interestingly, the manipulation check demonstrated that 50–74 % of parents in both conditions were aware of how much Ca their child should be consuming each day. Golley and colleagues(Reference Golley, Hendrie and Slater39) reported that specific goal setting and environmental restructuring were key components in effective interventions to change children’s nutrition intake and activity patterns in obesity prevention interventions. Behavioural restructuring has also been associated with intervention effectiveness aimed at increasing dairy and/or Ca consumption in preschool-age children, as was the use of prompts and cues(Reference Srbely, Janjua and Buchholz40). Based on the meaningful significant increase (equating to one more serving of dairy per day) in daily Ca consumption in each condition, providing specific dietary targets, and a daily prompt may have provided parents with enough information and motivation to change their behaviour.
It is also noteworthy that the messages provided in both conditions were branded as coming from the University of British Columbia. Qualitative work with parents suggests that parents are more receptive to messages that they perceive as coming from a trustworthy source(Reference Jung, Bourne and Buchholz28). In previous work, parents communicated a mistrust of supermarkets and the dairy farming industry but communicated trust in universities and information on Health Canada’s website(Reference Jung, Bourne and Buchholz28). As such, the messages provided in both conditions may have been potent due to the perceived trustworthiness of the source. These findings are important for public health messaging as they suggest that minimal targeting may be required when directing child nutritional interventions at parents. Contrary to research aimed at increasing Ca consumption in adults in which tailoring or targeting are key strategies for intervention success(Reference Jung, Latimer-Cheung and Bourne26,Reference Estok, Sedlak and Doheny41,Reference Sedlak, Doheny and Estok42) , a repeated, simple message from a trusted source, in the form of specific daily Ca requirements for children, could be sufficient to evoke change.
Interestingly, parental perceived role modelling behaviour and social support for children’s consumption of Ca significantly increased in both conditions. This observation aligns with findings that parents positively influence their children’s intake of Ca-rich foods(Reference Banna, O’Driscoll and Boushey14,Reference Edlefsen, Reicks and Goldberg43) and suggests that parents were actively encouraging increased Ca consumption. Nevertheless, change in parental Ca intake did not reach statistical significance. Increases of 181·91 mg and 77·55 mg of Ca were reported from baseline to 52 weeks in the experimental and control conditions, respectively. Post hoc analyses revealed a significant increase in parents’ total Ca intake at week 8 in the experimental condition, which was significantly different from the control condition. Although this significant increase was not maintained across the intervention, Ca intake values at weeks 32 and 52 were like those at week 8. As such, it appears that the Ca-specific messaging provided in the intervention condition may have impacted parents’ Ca intake beyond the provision of Ca-specific goals. This result is similar to findings from other research aimed at increasing Ca consumption in adults(Reference Jung, Martin Ginis and Phillips25,Reference Jung, Latimer-Cheung and Bourne26) . Interestingly, parents have been shown to be more motivated to change their home food practices to ensure that their children meet nutritional requirements and are less concerned about their own dietary behaviours(Reference Jung, Bourne and Buchholz28). This could explain why parents perceived social support and role modelling increased significantly but their Ca consumption did not.
Calcium-rich products already present in the home
Parent and children’s increase in Ca consumption came primarily from increases in dairy product consumption. However, the total amount of money spent on dairy products did not increase during the study. Parents spent between $27·66–$32·06 and $16·59–$21·82 on dairy products in the experimental and control conditions, respectively, across time points. Parents may have achieved an approximately 200 mg/d increase in children’s Ca intake by reducing dairy waste, or purchasing lower-cost dairy products (e.g. purchasing yoghurt in bulk). The use of food receipts represents a novel method of tracking the consumption and availability of Ca-rich products in the home.
Strengths and limitations
Reliance on parents to report Ca intake for themselves and their children could lead to inaccurate reporting. Furthermore, social desirability could have influenced reporting of Ca intake and psychosocial factors. Children may have perceived their parents’ behaviour differently than how their parents reported it. However, given the young age of the children in the study, parental self-reporting was the most practical method of data collection. The Ca calculator used to determine eligibility for the study was not sensitive enough to capture individuals’ daily Ca intake. As such, several children, who were identified as under-consuming Ca when determining eligibility, were consuming adequate Ca at baseline based on completion of the 3-d FFQ. These parents and children were randomised following completion of the eligibility survey but were later removed from analyses. It is important to note that both the Ca calculator and the food record provide estimates of nutrient intakes and may not be comparable to actual intake. Future research could use other measures such as intake 24(Reference Simpson, Bradley and Poliakov44) or ASA-24(Reference Wallace, Kirkpatrick and Darlington45) and assess parental behaviour through videoing interactions with children.
The study dropout rate of approximately 50 % by 52 weeks may have been due to the use of mail-out surveys and postal returns. These methods may have put greater burden on the participants than online data collection. However, a 50 % dropout for a yearlong mail-out intervention is not uncommon(Reference Bendtsen, McCambridge and Bendtsen46). Mailing out information was identified as the preferred method of communication by parents in our focus groups(Reference Jung, Bourne and Buchholz28). Future research could provide parents with mailed-out material but have measures and interventions delivered online(Reference Haerens, Craeynest and Deforche47).
The dropout rate in the current study reduced the statistical power to detect a true effect and eliminated the opportunity to conduct more advanced statistical analyses to examine the potential mediating effects of the intervention through parental consumption behaviour and psychosocial variables. The present findings should be interpreted with caution as reduced statistical power increases the likelihood of a false positive(Reference Button, Ioannidis and Mokrysz48). To increase certainty in the findings, the trial should be repeated, using data obtained from the current study, specifically study dropout and effect estimates, to calculate an appropriate sample size. A more extensive recruitment strategy should be adopted to ensure that the necessary sample size is reached.
Despite these limitations, a study strength was that parents and children were strategically recruited from across Canada, representing a diverse nationwide sample. Sample heterogeneity enhances generalisability of findings across Canada. In addition, the intention-to-treat analysis allowed for participants to be included who did not complete all study measures. This provides a conservative and pragmatic evaluation of the intervention.
Future research
The current study highlights that the provision of specific nutrient goals directed at parents can increase Ca consumption in children. More research is needed to examine the relationship between potential mediating psychosocial variables to identify which variables impact nutrition behaviour. Components of the experimental and control conditions that lead to change need to be explored. The control condition incorporated general nutrition information including benefits of a healthy diet and strategies to consume a healthy diet. An attention control condition that does not incorporate nutritional information or specific dietary intake goals should be included in future studies to determine whether basic nutritional information is sufficient to evoke change as opposed to nutrient-specific information. This approach would also test the possibility that merely participating in the study elicited behavioural change in the outcome measure, particularly in the control group (i.e. Hawthorne effects).
Conclusion
The results of this study suggest that targeting parents as a means of increasing Ca consumption in children aged 4–10 years is an effective intervention strategy with effects maintained at 12-month follow-up. Given similar increases in child Ca consumption between the experimental and control conditions, this study suggests that simple, repeated reminders of daily Ca intake requirements for children provide sufficient motivation to change parents’ behaviour to provide Ca-rich foods to their children. This strategy represents an extremely low-cost initiative that could be easily implemented across Canada through the provision of materials such as fridge magnets or calendars with stickers to engage children in monitoring their consumption. Future studies should be conducted to confirm the current findings given the high rates of Ca under-consumption in Canadian children. If confirmed, these results could have implications for future public health campaigns.
Acknowledgements
Acknowledgements: None. Financial support: Support by a grant from the Canadian Agri-Science Clusters Initiative, Dairy Research Cluster (Dairy Farmers of Canada, Agriculture and Agri-Food Canada and Canadian Dairy Commission). The Canadian Agri-Science Clusters Initiative had no role in the design, analysis or writing of this article. Conflict of interest: There are no conflicts of interest. Authorship: J.E.B. and M.E.J. were responsible for project conception. J.E.B. and M.E.J. designed the research, developed the overall research plan, conducted the research, analysed the data, determined the content for manuscript and collaborated on the writing. K.M.G. and A.B. contributed to the overall research plan and assisting with manuscript writing. S.S. contributed to the writing of the manuscript. All authors read and approved the final manuscript. Ethics of human subject participation: This study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving human subjects were approved by the University of British Columbia Behavioural Ethics Committee (H14-02762). Written informed consent was obtained from all subjects.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980021001087









