Physical activity (PA) is well documented to provide important benefits to child and adolescent health and well-being including reducing the risk for overweight and obesity, cardiometabolic risk factors and mental health as well as improved quality of life(Reference Janssen and LeBlanc1). Guidelines established in 2010 by the WHO recommend that children aged 5–17 years old should perform at least 60 min of moderate to vigorous intensity PA daily(2). However, globally, in 2016, four out of five school children between the ages 11 and 17 were estimated to engage in insufficient PA(Reference Guthold, Stevens and Riley3). Between 2007 and 2013, only about 15 % of adolescents met PA recommendations in Latin American and Caribbean countries(Reference Aguilar-Farias, Martino-Fuentealba and Carcamo-Oyarzun4).
Emerging evidence suggests PA levels in children may be associated with food insecurity. Household food insecurity (HFI) is defined as the limited or uncertain availability of nutritionally adequate and safe foods and the limited or uncertain ability to acquire acceptable foods in socially acceptable ways(Reference Bickel, Mark, Cristofer, William and John5). Four studies carried out in the USA and other high-income countries identified an inverse relationship between food insecurity and PA(Reference To, Frongillo and Gallegos6–Reference Fram, Ritchie and Rosen9), while another in the same setting reported null findings(Reference Navarro, Tsai and Ritchie10). A study in Brazil, an upper middle-income country, reported a lack of association between food insecurity and PA in adolescents(Reference Lopes, Sichieri and Salles-Costa11). More recently, two studies used pooled cross-sectional data from low-, middle- and high-income countries to assess the relationship between food insecurity and PA in children aged 11 years and older(Reference Araujo, Werneck and Barboza12,Reference Fram, Nguyen and Frongillo13) . In one, the authors used data from ninety-five countries and found that food-insecure children had lower levels of PA compared with their food-secure counterparts(Reference Fram, Nguyen and Frongillo13). The other study that used national survey data from eleven South American countries found that food-insecure adolescents were more likely to actively commute to school, participate in physical education classes and engage in less time sitting than food-secure adolescents, but did not find an association with total PA(Reference Araujo, Werneck and Barboza12). Therefore, existing literature is inconsistent with studies reporting positive, negative and null associations between HFI and PA.
Ecuador, like many other low- and middle-income countries (LMIC), is in the process of nutritional and epidemiologic transition, a population phase characterised by changes from traditional to western diets high in energy-dense foods, reductions in PA and a shift towards a more sedentary lifestyle, obesity and chronic degenerative diseases(Reference Freire, Silva-Jaramillo and Ramírez-Luzuriaga14). Several studies have reported low PA levels in Ecuadorian children(Reference Guthold, Stevens and Riley3,Reference Aguilar-Farias, Martino-Fuentealba and Carcamo-Oyarzun4,Reference Abril, Manuel-y-keenoy and Solà15) . Similar to the WHO recommendations, the Ecuadorian Ministries of Health and Education recommends at least 60 min of daily PA for children aged 5–17 years(16). However, the 2018 Ecuador Report Card for PA found only about one in three children in this age group were physically active for at least 60 min per day(Reference Andrade, Ochoa-Avilés and Freire17). Recent studies have also identified a high prevalence of overweight and obesity(Reference Abril, Manuel-y-keenoy and Solà15), stunting(Reference Freire, Silva-Jaramillo and Ramírez-Luzuriaga14) and a double burden of malnutrition(Reference Thompson, Nicholas and Watson18), characterised by concomitant obesity and stunting in the same Ecuadorian households. Moreover, a high burden of Zn deficiencies and anaemia has been reported among children and adolescents in Ecuador(Reference Freire, Silva-Jaramillo and Ramírez-Luzuriaga14). In Ecuadorian school age children and reproductive age women, high rates of overweight/obesity co-exist with Zn deficiency or with anaemia(Reference Freire, Silva-Jaramillo and Ramírez-Luzuriaga14). This triple burden of micronutrient deficiencies, overweight/obesity and stunting could lead to fatigue, weakness and raise the risk of infectious illnesses, further disrupting child PA levels.
Ecuadorian households with children have a high prevalence of moderate-severe HFI(19). HFI has been previously linked to poorer health outcomes in Ecuadorian children such as psychosocial dysfunction(Reference Weigel and Armijos20), poor oral health(Reference Weigel and Armijos21) and a dual burden of over- and under-nutrition(Reference Thompson, Nicholas and Watson18). Other studies have reported null associations between HFI and stunting(Reference Walrod, Seccareccia and Sarmiento22), overweight and obesity(Reference Walrod, Seccareccia and Sarmiento22–Reference Velez Pinos and Buenano Rodriguez24). However, due to a lack of published studies, it remains uncertain whether HFI is associated with PA in children and adolescents in Ecuador. Considering the high prevalence of HFI and sub-optimal PA levels, Ecuadorian children may be at risk for overweight, obesity and cardiometabolic risk factors that can develop into comorbidities over the long term. Globally, prior studies have investigated these associations using different metrics and samples, which limits our ability to draw conclusions across studies. Thus, a better understanding of the relationship of HFI with PA in Ecuadorian children is crucial in identifying the most vulnerable groups that could potentially benefit from targeted interventions to alleviate HFI and prevent onset of chronic diseases.
Several potential pathways exist that might explain how HFI can influence child PA, sedentary behaviour (SB), stunting and overweight/obesity (Fig. 1). For example, food-insecure households may be forced to switch to cheaper, energy-dense, pro-inflammatory foods instead of more expensive but nutritious fruits, vegetables dairy and animal protein food(Reference Weigel and Armijos23,Reference Bergmans, Palta and Robert25) . This can not only affect the linear growth and weight gain patterns of children in those households but also adversely impact their micronutrient and protein status and immunocompetence. This situation can increase child risk for anaemia(Reference Eicher-Miller, Mason and Weaver26), fatigue and infectious illnesses, which in turn can make them physiologically less able to engage in PA. In addition, the consumption of a pro-inflammatory diet has been linked to poorer cardiometabolic health and higher odds of metabolic syndrome in Ecuadorian school-age children(Reference Wang, Armijos and Weigel27). Both undernutrition and overnutrition can potentially impact child PA levels. For instance, children who are stunted or underweight have a smaller body size, reduced muscle mass and expend lower total energy in PA(Reference Malina and Katzmarzyk28). However, children who are overweight/obese also may have lower PA levels compared with their normal weight counterparts, particularly in the case of activities involving runs and jumps(Reference Malina and Katzmarzyk28).
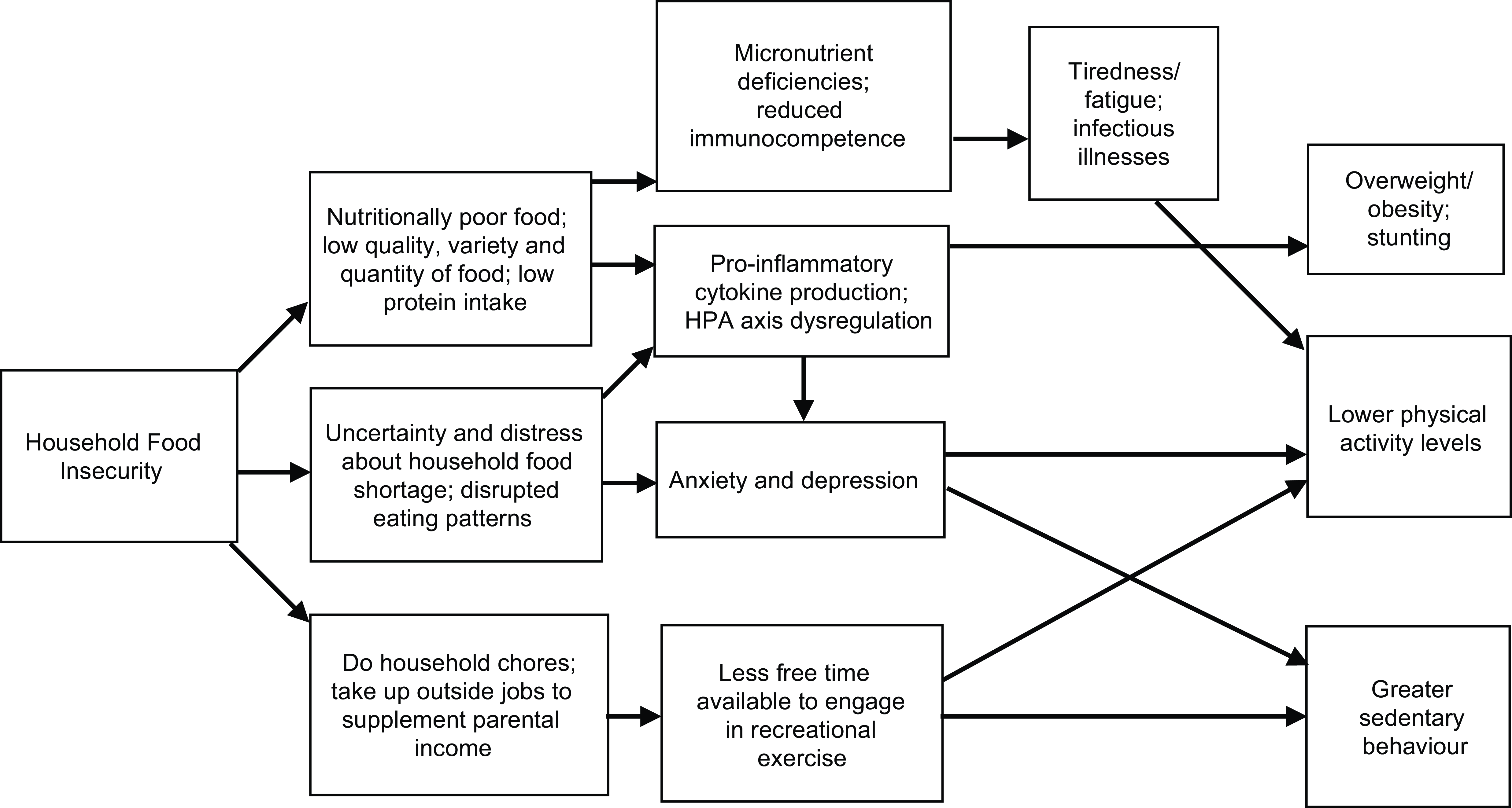
Fig. 1 Potential pathways underlying the relationship between household food insecurity and physical activity, sedentary behaviour, overweight/obesity and stunting in Ecuadorian children and adolescents
Furthermore, children from food-insecure households are often aware of their household’s food situation(Reference Fram, Frongillo and Jones29) and because of this may experience worry, sadness and anger(Reference Fram, Frongillo and Jones29). Chronic stress due to worry or anxiety over the household food situation may also increase the production of pro-inflammatory cytokines and disrupt hypothalamic–pituitary–adrenal axis regulation(Reference Laraia30). Hypothalamic–pituitary–adrenal axis dysregulation promotes the desire to consume high sugar, energy-dense ‘comfort food’, that can lead to overweight/obesity(Reference Laraia30). Such disruption has also been associated with poorer mental health and well-being(Reference Lycett, Wijayawickrama and Liu31). Stress and depression symptoms may further restrict child ability to participate in daily PA and may promote more SB(Reference Fram, Ritchie and Rosen9). Yet another potential pathway is that children from food-insecure households may be required to work outside the home to economically support their families or otherwise help out by performing domestic activities (e.g. household chores, sibling care)(Reference Bernal, Frongillo and Herrera32). These may occupy time that they would have otherwise spent performing recreational PA.
The primary objective of this study was to investigate the association of HFI and PA and SB in 5–17-year-old children and adolescents from Ecuador, an upper-middle income country setting. We also assessed the relationship between HFI and anthropometric indicators of nutritional status, specifically stunting, underweight, overweight and obesity in these children. We hypothesised that children from food-insecure households would be more likely to have (a) lower PA levels, (b) greater SB and (c) present with stunting and overweight/obesity through one or more of the pathways described above.
Methods
Study Design and Sampling
We analysed cross-sectional data from the Ecuador 2018 National Health and Nutrition Survey (ENSANUT-2018).(33) The study design, sampling strategy, data collection procedures and other methodological considerations used by the survey have been published in detail(33). Briefly, the survey used a probabilistic two-stage sampling strategy to collect data from a nationally representative sample of 46 638 households of non-institutionalised individuals between 0 and 99 years of age. The the Ecuador 2018 National Health and Nutrition Survey collected data at the national, provincial, urban and rural levels during November 2018–January 2019 and June–July 2019. The underlying sampling frame for this survey was drawn from the 2010 Ecuadorian Population Census as well as the 2010–17 census updates(33). We used data from two survey modules, the Household (‘Hogar’) and the Risk Factors (‘Factores de Riesgo’) for children 5–17 years old. These modules collected information on household socio-demographic characteristics, food security status, anthropometric measurements, PA and SB of children and adolescents, among other items. For the present study, our analytic sample was composed of all 23 621 children and adolescents included in the risk factors module who were aged 5–17 years.
Study measures
Household food insecurity status
Food security status during the past 12 months was assessed using the eight-question Food Insecurity Experience Scale (FIES), Spanish language version, developed by the UN FAO(34). The FIES was administered to adult caregivers, primarily mothers. The questions ranged from difficulties in accessing food due to lack of money or other resources to going without eating for a whole day. Affirmative responses were coded as ‘one’, while negative responses were coded as ‘zero’. The responses were summed to give a raw score ranging from zero to eight. Statistical validation of the FIES in this sample was conducted in a prior study(Reference Weigel and Armijos35). Briefly, the eight-item FIES had infit values ranging from 0·86 and 1·17, residual correlations < 4 for all item pairs and a Rasch reliability of 0·75(Reference Weigel and Armijos35). Therefore, this scale had adequate model fit and reliability(Reference Weigel and Armijos35). In this study analysis, households with a raw score of zero were categorised as ‘food secure’, those with raw scores of 1–3 as ‘marginal HFI’ and scores of 4–8 as ‘moderate-severe HFI’.
Physical activity
The PA levels of the child participants were obtained by asking their caregivers three questions: (1) how many days was the child physically active (recreational PA) for at least 60 min in the past week? (2) how many days did the child walk or bike to and from school in the past week (active commute) and how many minutes per day were spent on this activity? and (3) how many days did the child participate in physical education (PE) classes in school during the past week and what was the duration of each class in minutes? These questions were adapted from Ecuador’s previous ENSANUT 2012 survey(36). The responses to these three questions were aggregated to estimate total minutes of PA per week (recreational PA minutes/week + PE class minutes/week + active commute minutes/week = total PA minutes/week). We also created an indicator for adherence to PA recommendations by dichotomising total PA minutes/week at 420 min to assess whether children met the Ecuador’s PA recommendations (total minutes of PA ≥ 420 min) or not (total minutes of PA < 420 min) in a week(16).
Sedentary behaviour
The daily SB of child participants was obtained by asking the caregiver, in a normal day, how much time (in minutes) the child participant spends seated or resting, watching television, playing video games, talking to friends or other activities that require the child to stay seated including chatting, surfing the internet and sending emails? While WHO currently does not have established thresholds for time spent in SB, spending more than two hours of sedentary time/day has been linked to several negative physical and mental health outcomes in children and youth(Reference Tremblay, LeBlanc and Kho37). Accordingly, we categorissed daily sedentary minutes in two groups, ≤120 min and >120 min.
Anthropometric indicators of nutritional status
Trained survey anthropometrists measured the standing height (cm) and weight (kg) of child participants using a standardised protocol(33). These measurements were made twice and the average recorded in the database. If the first two measurements differed by ± 0·5 cm (height) or ± 0·5 kg (weight), a third measurement was made and the average value from the two closest values was used. The child weight and height measurements were used to calculate BMI defined as weight (kg)/height (m2). The BMI-for-age z (BAZ) scores and height-for-age z (HAZ) scores were compared with the WHO age- and sex-specific growth reference using the WHO macro for R software(38). Child BMI were classified as underweight (BAZ < –2), normal weight (–2 ≤ BAZ ≤ +1), overweight (BAZ > +1) or obese (BAZ > +2)(39). Children were classified as stunted if their HAZ was < –2(39). Since anthropometric data for 822 participants were missing, the analysis of the anthropometric indicators was based on 22 799 child participants.
Covariates
The individual-level characteristics examined for potential inclusion as covariates in the statistical models included child age (5–12 years v. 13–17 years), child sex (female v. male), any child health problems in the past month (yes v. no), mother’s age (years), maternal ethnicity (mestizo ethnic majority group v. ethnic minority group, i.e. indigenous or afro-descendants), employment status (full-time housewife v. other), marital status (legally married v. other) and formal education (primary schooling or less, v. secondary or higher schooling). The household-level attributes included urbanicity (urban v. rural), region of residence (Pacific Coast, Amazon and Galapagos v. Andean Highlands), number of children in the household and household asset index (high v. low). The household asset index was created based on ownership of twenty-seven items including cars, motorcycles, household appliances such as refrigerator, stoves and washing machines.(Reference Weigel and Armijos35) In this study, we categorised households in the lowest quartile of the asset index as having a low asset index.
Data analysis
We used survey-provided sample weights to yield nationally representative estimates. All analyses were conducted in Stata/SE 17·0 (StataCorp LLC) using the svy prefix command for survey data analysis. The summary statistics are presented as frequencies with weighted percentages for categorical variables and weighted mean and se for continuous variables. We specified unadjusted and adjusted linear and log-binomial regression models to examine the association of HFI with total minutes of PA/week and adherence to PA recommendations, respectively. Unadjusted and adjusted log-binomial regression models were used to examine the association of HFI with SB and stunting. We conducted unadjusted and adjusted multinomial logistic regression to assess the association of HFI with BMI-for age categories. Results are reported as beta estimates or prevalence ratios (or OR for multinomial logistic) with 95 % CI.
We adjusted for several covariates in separate regression models. In adjusted model 1, we included child age, sex, maternal ethnicity, maternal education and number of children in the household. In adjusted model 2, we included model 1 covariates and added urbanicity and region. In adjusted model 3, in addition to model 1 and 2 covariates, we included household asset index. Considering household asset index may be collinear with HFI, we tested for multicollinearity using variance inflation factor. We found no evidence of multicollinearity in our models with all independent variables having a variance inflation factor value of < 2. Furthermore, we did not have household asset index data for 4372 participants. We conducted a complete case analysis and present results for adjusted model 3 using 19 249 observations. However, we performed a sensitivity analysis by imputing all the missing asset index values as either low or high to estimate the maximum possible difference in results that could be expected based on the exclusion of this missing data. Our sensitivity analysis results are detailed in the Supplementary Materials. Statistical significance for all hypothesis tests was set at P < 0·05. All statistical tests were two tailed.
Results
Household food insecurity and socio-demographic characteristics
In this study, about one in four child households (24 %) had marginal HFI, while one in five (20 %) had moderate-severe HFI. Nearly half the child participants were female (49 %) and nearly two-thirds (64 %) were between ages 5 and 12 years (Table 1). The table shows that other socio-demographic characteristics differed by HFI status. For example, a greater proportion of children from food-insecure households had mothers who were slightly younger, belonged in an ethnic minority group, were not legally married, had poorer education and were full-time housewives, compared with food-secure counterparts. More children from food-insecure households resided in rural areas, particularly in the Pacific Coast or Amazonian regions of Ecuador and belonged to households having a low asset index, compared with food-secure groups. A higher proportion of food-insecure households reported that their children had experienced some type of health problem during the past 30-day period, and the number of household children was greater in food-insecure households compared with their food-secure counterparts.
Table 1 Socio-demographic, general health and physical activity characteristics of Ecuadorian children according to their household food insecurity (HFI) status, (n 23 621)*

* Bivariate tests conducted using χ 2 tests for categorical variables and adjusted Wald tests for continuous variables.
† Household asset index N 19 249.
‡ BMI-for-age N 22 545.
§ Stunting N 22 785.
|| Other marital status options include single, separated, divorced, widowed and domestic partnership.
¶ Other maternal employment options include self-employed, employers, salaried workers, domestic employees and unpaid workers.
Physical activity behaviour
The child participants were reported to average 259 min of PA per week. About one in five (19 %) met Ecuador’s PA recommendations for children (Table 1). After adjusting for covariates in models 1–3, HFI was not associated with minutes of PA nor with meeting PA recommendations (Table 2).
Table 2 Household food insecurity (HFI) and its association with physical activity levels and sedentary behaviour in Ecuadorian children (n 23 621)
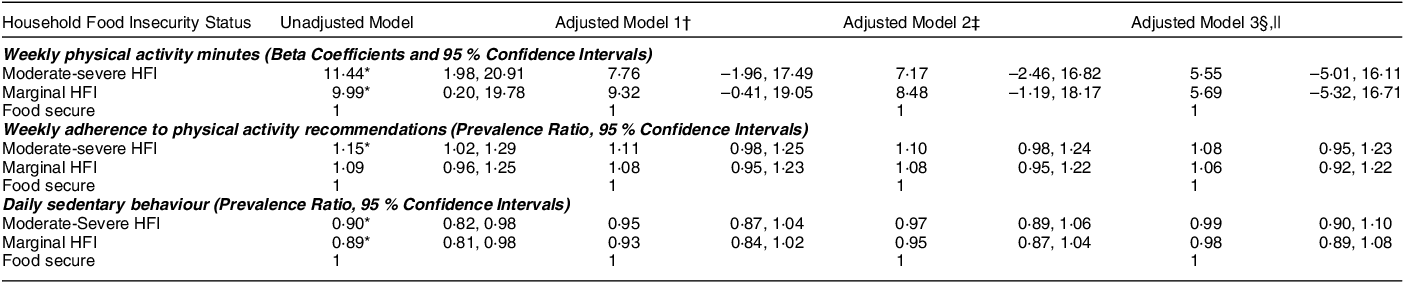
* P < 0·05.
† Adjusted for child age, child sex, maternal ethnicity, maternal education and number of children in the household.
‡ Adjusted for model 1 covariates + urbanicity and region.
§ Adjusted for model 1 and model 2 covariates + household asset index.
|| Adjusted model 3 has N 19 249.
Sedentary behaviour
Approximately one out of every three children (32 %) in the study were reported as being sedentary for 2 hours or more per day (Table 1). After adjustment for covariates, HFI was not associated with SB in the child participants in models 1–3 (Table 2).
BMI-for-age
In this study, three out of five (60 %) children had normal weight, while 24 % were overweight, 14 % were obese and 1·7 % were underweight (Table 1). After adjusting for covariates in models 1 and 2, moderate-severe HFI was associated with lower prevalence of overweight and obesity in the children (Table 3). However, after including the asset index in the adjustment set in model 3, HFI was no longer associated with overweight and obesity. HFI was not associated with underweight in any of the regression models.
Table 3 Household food insecurity (HFI) and its association with anthropometric indicators of nutritional status in Ecuadorian children (n 22 799) †

* P < 0·01.
† Data for 822 child participants were missing.
‡ n = 22 545 since 254 participant’s BMI-for-age values were flagged as improbable.
§ n = 22 785 since fourteen participant’s height-for-age values were flagged as improbable.
|| For adjusted model 3, n (BMI-for-age) = 19 044 and n (stunting) = 19 236.
¶ Adjusted for child age, child sex, maternal ethnicity, maternal education and number of children in the household.
** Adjusted for model 1 covariates + urbanicity and region.
*† Adjusted for model 1 and model 2 covariates + household asset index.
Stunting
Stunting was present in < 10 % of the child participants (Table 1). In our covariate adjusted models 1–3, moderate-severe HFI was not associated with stunting (Table 3).
Sensitivity analysis
The magnitude and precision of our estimates after imputing missing asset index value as high or low were similar to the adjusted models excluding the missing asset index data (see online supplementary material, Supplementary Analysis Tables 1–4). Children from households with missing asset index data were more likely to present with stunting but had lower total PA minutes per week and were less likely to meet the PA recommendations. HFI, SB and BMI-for-age were not significantly different between those with and without missing asset index data (see online supplementary material, Supplementary Analysis Table 6). Moreover, we found that HFI was not associated with PE class minutes/week nor with recreational PA minutes/week separately (see online supplementary material, Supplementary Analysis Table 5). However, moderate-severe HFI was associated with an average of 7·4 (95 % CI: 3·46, 11·26) more minutes/week spent in active commuting to and from school. In sex-stratified analysis, HFI was not associated with PA, SB, overweight/obesity, nor stunting (see online supplementary material, Supplementary Analysis Tables 7 and 8). However, in males, moderate-severe HFI was associated with 0·51 times the odds of underweight, while marginal HFI was associated with 0·47 times the odds of underweight in females (see online supplementary material, Supplementary Analysis Table 8) after adjusting for asset index.
Discussion
This study identified a high prevalence of HFI in the households of 5–17-year-old child participants. The high HFI prevalence is consistent with that reported by previous surveys and other studies for Ecuadorian households(19,Reference Walrod, Seccareccia and Sarmiento22–Reference Velez Pinos and Buenano Rodriguez24) . The major findings of this study were that HFI was not associated with reported PA, SB, stunting or overweight and obesity in the Ecuadorian child and adolescents surveyed in the 2018 ENSANUT. These findings suggest that while HFI continues to be a burden in Ecuadorian households, it does not appear to contribute towards the physical inactivity and SB reported for this group of Ecuadorian children and adolescents.
The null associations identified in our study between HFI with total minutes of PA and meeting PA recommendations differ from our apriori hypothesis. However, they are consistent with the evidence published on HFI and PA in Brazilian(Reference Lopes, Sichieri and Salles-Costa11), U.S.(Reference Navarro, Tsai and Ritchie10) and Spanish(Reference Ortiz-Marrón, Ortiz-Pinto and Urtasun Lanza40) children and adolescents. They also partially concur with a U.S. study reporting that food-insecure children did not differ from their food-secure counterparts regarding meeting physical activity guidelines although they engaged in fewer minutes of moderate to vigorous physical activity(Reference To, Frongillo and Gallegos6). Another study also found that although HFI was not associated with physical activity, it was associated with attending more PE classes and with higher odds of active commuting to school(Reference Araujo, Werneck and Barboza12).
In our post hoc analyses, we found that children from moderate-severe HFI households had higher active commuting minutes than those from food-secure households. It is plausible that children from resource constrained, food-insecure households might not have had extra money for public transport or access to carpools and other forms of passive transport. Therefore, they accumulated more active commuting minutes by walking or biking to school, which is a low-cost alternative(Reference Araujo, Werneck and Barboza12). However, it is important to note that our findings imply that, on average, children from food-insecure households actively commuted about one extra minute per day compared with children from food-secure households, which may not be a meaningful difference.
Different from our findings, other studies have reported negative associations between HFI and physical activity(Reference To, Frongillo and Gallegos6,Reference Fram, Ritchie and Rosen9,Reference Fram, Nguyen and Frongillo13) . The inconsistent findings they reported for this relationship could be due to the different methods used to define and measure physical activity. For instance, some studies focused on recreational physical activity(Reference Gulliford, Nunes and Rocke8), one included active commute time and time spent in PE classes(Reference Navarro, Tsai and Ritchie10), while another relied on objective measurements obtained from accelerometers(Reference To, Frongillo and Gallegos6). Differing methods were also used by the various studies to measure food insecurity. Some relied on a single question that asked how often adolescents had been hungry during the past 30 d(Reference Araujo, Werneck and Barboza12,Reference Fram, Nguyen and Frongillo13) , while others used either the full version of the US Department of Agriculture’s eighteen-item Household Food Security Survey Module(Reference To, Frongillo and Gallegos6) or an abbreviated(Reference Gulliford, Nunes and Rocke8,Reference Navarro, Tsai and Ritchie10) , or an adapted version(Reference Lopes, Sichieri and Salles-Costa11) of the same. Furthermore, two studies measured individual-level child food insecurity instead of HFI(Reference Shanafelt, Hearst and Wang7,Reference Fram, Ritchie and Rosen9) . In addition, differences in geographical location, environmental and infrastructural factors, attitudes towards physical activity behaviour and access to TV and video games among the study populations between HIC and LMIC may be responsible for the mixed findings for this relationship(Reference Vancampfort, Van Damme and Firth41).
Also different from what we hypothesised, HFI was not associated with child SB. Our results are similar to previous findings from Brazil(Reference Lopes, Sichieri and Salles-Costa11) and the USA(Reference To, Frongillo and Gallegos6,Reference Navarro, Tsai and Ritchie10) reporting that children from food-insecure households were not more likely to be sedentary than their food-secure counterparts. One study used school-based data from Global Student Health Surveys conducted in sixty-six LMIC. Their findings indicated that food insecurity in adolescents living in upper-middle income and low-income countries was not associated with SB.(Reference Vancampfort, Van Damme and Firth41) This contrasts with the results from other studies suggesting that HFI was associated with higher(Reference Ortiz-Marrón, Ortiz-Pinto and Urtasun Lanza40) or lower(Reference Araujo, Werneck and Barboza12) SB. Since more than two-thirds (68 %) of our study participants had less than 2 hours of daily SB, it is possible that the Ecuadorian population is at an earlier stage of epidemiologic transition characterised by a lower prevalence of SB among children and adolescents. Furthermore, Ecuadorian adolescents may have to assist with household chores, cooking and particularly in rural areas, help with farming, which reduces the time available for sedentary activities(Reference Van Royen, Verstraeten and Andrade42).
The evidence of an association between HFI and overweight/obesity in this age group is ambiguous. However, studies suggest that adolescent girls from food-insecure households may be at risk of overweight/obesity compared with their food-secure counterparts(Reference Frongillo and Bernal43,Reference Maitra44) . This relationship could be further complicated by the Ecuador’s economic development level(Reference Maitra44). Most studies that have found a positive association of HFI with overweight/obesity were situated in high-income country settings(Reference Ortiz-Marrón, Ortiz-Pinto and Urtasun Lanza40,Reference Maitra44,Reference Dubois, Francis and Burnier45) . Fewer studies from LMIC have found a similar positive relationship,(Reference Schlüssel, Silva and Pérez-Escamilla46) and some have reported negative associations(Reference Maitra44,Reference Dubois, Francis and Burnier45) . This inconsistency could be due to different pathways that link HFI, socio-economic status, the stage of nutritional transition and overweight/obesity in children from HIC v. LMIC. One study investigating this relationship in Quebec, Canada (HIC setting) and Jamaica (LMIC setting) found that HFI raised the risk of overweight/obesity in children in the former, but was negatively associated with overweight/obesity in the latter(Reference Dubois, Francis and Burnier45). The current study findings, while contrary to our hypothesis, tend to align with the published evidence. We found HFI was associated with lower prevalence of overweight and obesity in children and adolescents. However, adjustment for household asset index attenuated the findings, and HFI was no longer associated with overweight/obesity. It is possible that it may have confounded the relationship between HFI and overweight/obesity in the other regression models. However, it is also crucial to consider that the asset index, a proxy for socio-economic status, may explain some of the effect of HFI on overweight/obesity in our study. It seems likely that the food-insecure households of Ecuadorian children may not have the economic resources to purchase more obesogenic processed and ultra-processed food and beverages which can be more expensive than traditional diet in this setting. It has been reported that in Colombia, another upper middle-income Andean country, children from food-insecure households consumed fewer snacks and processed food than children from food-secure households(Reference Isanaka, Mora-Plazas and Lopez-Arana47). This contrasts with evidence from HIC where those from food-insecure households have easier availability and accessibility to fast food, which can promote weight gain(Reference Ma, Liese and Bell48). Furthermore, our child participants may have actively commuted to school due to it being a cheaper or only option than passive modes of transportation which slightly increased their physical activity. This may have contributed to the low prevalence of overweight/obesity observed in Ecuadorian child participants living in from households with marginal and moderate-severe food-insecure households compared with their food-secure counterparts. Interestingly, after adjusting for asset index, both males and females from food-insecure households had lower odds of underweight than those from food-secure households. However, these results should be interpreted with caution due to the low prevalence of underweight reported in this study, which may have biased our results.
The findings from some prior studies suggest that HFI appears to be positively associated with stunting in children. However, this direction of association was predominantly reported in LMIC rather than HIC(Reference Maitra44,Reference Moradi, Mirzababaei and Mohammadi49) . Differences in the absolute severity of HFI, different coping strategies and local safety net programs may partially explain these mixed findings(Reference Hadley and Crooks50). Our findings indicate that HFI was not associated with stunting in our child participants. While contrary to our hypothesis, our results are consistent with previous literature from Latin America that have also reported null findings between food insecurity and child stunting(Reference Walrod, Seccareccia and Sarmiento22,Reference Isanaka, Mora-Plazas and Lopez-Arana47) . While stunting continues to be a burden in Ecuador, its aetiology is multifactorial and there may be other determinants such as access to water and safe sanitation that was not assessed in this study. Furthermore, stunting in LMIC settings is often the consequence of chronic undernutrition and repeated infections. Thus, this cross-sectional study may not have been able to capture the association between HFI and stunting.
Strengths and limitations
Our study has several strengths. One of these is that we used data from a nationally representative survey. The ENSANUT-2018 had a low non-response rate (1·2 %), achieved high national coverage (∼92 %) and used standardised data collection procedures and quality control methods to ensure data quality(33). The child risk module used for the analysis had a large sample size (n 23 621), which permitted the adequate testing of our study hypotheses. In addition, physical activity was more broadly defined than some previous studies, including recreational physical activity, PE classes and active commuting, which is more closely aligned to the WHO definition. The survey used the FIES, an experience-based food security survey module to measure HFI. This allowed for us to identify children from households with both marginal and moderate-severe HFI. Also, height and weight were objectively measured by trained survey anthropometrists rather than relying on self-reported measurements which are not as accurate. Finally, this study extends prior work by assessing the relationship of HFI with physical activity and SB, which, to our knowledge, has not yet been studied in Ecuadorian children.
However, our study also has several limitations. One of the study limitations was that caregiver-reported data were used to assess HFI, physical activity and SB. Caregivers could have over- or under-reported their household’s food insecurity as well as over- or under-estimated the physical activity and SB of their children. These types of self-reports could have been affected by social desirability and recall bias. Also, the caregivers reported food insecurity at the household level which might not accurately reflect the individual food security situation of the child and adolescent participants. Another limitation is that the ENSANUT-2018 measured HFI for the previous 12-month period. Therefore, it might not reflect the HFI situation over a longer period which may be a concern since anthropometric indicators of nutritional status such as stunting, overweight and obesity can develop over a long time. Our study did not identify associations between HFI and underweight which may develop over a longer period of time. Considering that < 2 % of our sample were reported as underweight, it is possible that this study was not adequately powered to detect differences in child underweight across HFI groups.
Moreover, unmeasured confounders could have affected the results. Our analyses were restricted to variables contained in the database. Although the ENSANUT-2018 survey collected limited data on the intakes of a few types of foods, it did not collect data on the dietary protein and micronutrient (e.g. Fe, Zn and vitamin A) intakes of the child and adolescent participants. Diet plays a significant role in not only BMI-for-age and stunting but also on physical activity and SB. While in this study, we hypothesise that diet likely mediates some of the pathway between HFI and our study outcomes, future research should incorporate dietary data in their analysis of HFI and physical activity and SB to get a more in-depth understanding of the mechanisms for this relationship. Finally, the cross-sectional nature of this study allows us to infer but not establish causal effects.
Conclusion
Our study findings suggest HFI is not associated with physical activity, SB, stunting nor overweight/obesity in Ecuadorian children and adolescents. However, a notable prevalence of insufficient physical activity was reported among Ecuadorian children and adolescents aged 5–17 years. Thus, it is imperative to enhance the monitoring of physical activity levels and comprehensively examine the underlying factors that impede or facilitate physical activity in this particular age group. Leveraging this evidence can inform the design of interventions and evidence-based policies aimed at fostering physical activity and reducing SB, which can promote the health and well-being of Ecuadorian children and adolescents.
Acknowledgements
We would like to thank Dr. Molly Rosenberg for her advice with data analysis.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflict of interest
There are no conflicts of interest.
Authorship
Conceptualisation: R.C. and M.M.W.; formal analysis: R.C.; writing – original draft: R.C.; writing – review and editing: R.C., M.M.W. and R.X.A.; supervision: M.M.W.
Ethics of human subject participation
This study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving research study participants were approved by the Ecuadorian Instituto Nacional de Estadística y Censos (INEC). Written informed consent was obtained from the head of each participating households by the ENSANUT-2018 survey. This study used data from de-identified public database and was categorised as non-human subjects research by Indiana University Bloomington.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980024000351







