Childhood cancer survivors (CCS) are a growing population, with paediatric survival rates currently over 80 %( Reference Siegel, Naishadham and Jemal 1 ). This success emphasizes the importance of promoting long-term wellness in CCS as they age. CCS often fail to adhere to national diet and physical activity recommendations, despite their increased risk for associated chronic conditions including obesity and CVD( Reference Stolley, Restrepo and Sharp 2 – Reference Oeffinger, Mertens and Sklar 6 ). Studies suggest that children with cancer may benefit from nutrition interventions regardless of nutrition status prior to diagnosis( Reference Jaime‐Pérez, González‐Llano and Herrera‐Garza 7 ).
A survey study of CCS noted that over 80 % of respondents were interested in healthy eating and ‘getting in shape’ interventions, with a preference for computer- or camp-based programmes( Reference Badr, Chandra and Paxton 3 ). Paediatric cancer summer camps are tailored to patients and survivors for recreation; however, there are potential benefits of incorporating healthy lifestyle interventions into camp settings( Reference Li, Chung and Ho 8 ). While computer-delivered nutrition interventions may be desirable, evidence suggests that hands-on cooking classes may be more effective than nutrition education alone in changing dietary behaviour( Reference Curtis, Adamson and Mathers 9 ). A recent review of cooking programmes for school-aged children noted participation in cooking classes had positive impacts on child food preferences, attitudes and behaviours( Reference Hersch, Perdue and Ambroz 10 ).
Camp programmes for paediatric oncology patients are now available in many regions and there is evidence that they may help children with cancer enhance their coping skills, quality of life, self-esteem, psychosocial well-being and physical activity( Reference Curtis, Adamson and Mathers 9 , Reference Martiniuk, Silva and Amylon 11 , Reference Wu, McPhail and Mooney 12 ). Nutrition promotion programmes at paediatric oncology camps have not yet been studied in depth, but research from regular summer camps notes that healthy eating is an important target for camp administrators, suggesting cooking programmes could be a welcome addition to programming( Reference Ventura and Garst 13 ). Further, summer camp represents an important developmental experience for many children, making it a potentially effective time to try new foods and develop good cooking habits( Reference Thurber, Scanlin and Scheuler 14 ).
Little research has been done exploring the feasibility of integrating healthy cooking classes into paediatric cancer survivor/patient camps. Cooking classes offer a potential mechanism for delivering healthy eating information while fitting in well with camp activities and hospital-based child life programmes. Current cooking programmes vary widely in content( Reference Hersch, Perdue and Ambroz 10 , Reference Reicks, Trofholz and Stang 15 ), therefore an evidence-based conceptual framework of healthy cooking was used to guide our cooking programme development( Reference Raber, Chandra and Upadhyaya 16 ). The aim of the present communication is to address the development and implementation of healthy cooking classes offered to CCS at paediatric summer camps and a children’s cancer hospital based on a conceptual framework of healthy cooking.
Methods
Conceptual framework development
An evidence-based conceptual framework of healthy cooking was previously developed by the authors and used to guide the cooking classes( Reference Raber, Chandra and Upadhyaya 16 ). A literature search for experimental and observational studies exploring cooking behaviours identified fifty-nine studies used to inform the building of the model. Seventeen specific behaviours were organized into broad categories that formed the main constructs of the framework. These constructs included cooking frequency, techniques/methods, additions/replacements, ingredient minimization and flavouring (Table 1). The resulting framework was then reviewed by a panel of experts in relevant fields for face validation and updated accordingly. The constructs and sub-constructs of the framework were designed to be flexible enough to remain relevant across different types of dishes and cuisines.
Table 1 Healthy cooking framework constructs and defining behaviours
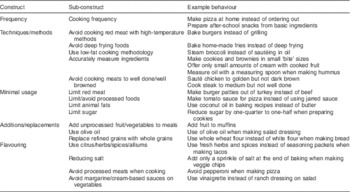
Table depicts the main constructs and sub-constructs from the framework of healthy cooking( Reference Raber, Chandra and Upadhyaya 16 ). The right-hand column shows example behaviours of the sub-constructs.
Description of cooking classes and participants
Camp classes
Table 2 shows class location, duration and number of participants. The hospital offers several camp programmes including two sleep-away camps for younger children (6–12 years) or teenagers (13–18 years) and a mixed-aged day camp on the hospital campus. Registration for camp is open to patients, survivors and siblings with the goal of offering a camp experience to children who may not have the chance to go to a traditional summer camp. Sleep-away camps for younger children and teens offer an opportunity to experience the outdoors with similarly aged peers and last approximately one week. Campers are divided by age and gender into a series of cabins and assigned two or more adult counsellors. The counsellors travel to activities with their cabin. Other counsellors and camp staff act as activity instructors. The camp staff is comprised of volunteers from the hospital, employees from the hospital’s Child Life department and camp site employees. Organized activities run from approximately 09.00 to 18.00 hours; campers also have group meals and evening events during the week.
Table 2 Description of healthy cooking classes delivered to childhood cancer survivors (n 189) and their parents (n 13) at one paediatric cancer hospital inpatient unit, one paediatric cancer in-hospital camp programme and two off-site paediatric cancer summer camp programmes, April 2015–April 2016
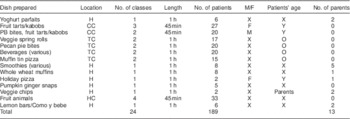
Scheme showing details of classes taught using the conceptual framework including dishes prepared, location (H, in hospital; CC, children’s camp; TC, teen camp, HC, hospital camp), number of classes, length of classes, participant gender (M, male; F, female; X, mixed), patients’ age (O, older (13–18 years); Y, younger (6–12 years); X, mixed) and number of parents present.
Younger children were offered 45 min cooking classes throughout the day in groups of ten, separated by age and gender. The classes were taught in an indoor kitchen equipped with two sinks, as well as an oven, stovetop, microwave and large counters. Cooking classes for teenagers were co-educational with approximately ten CCS per class. Two, one-hour classes per day were offered at teen camp. The cooking classes took place at an indoor recreation space that included a sink, counter, oven, microwave and stovetop. The classes began with short nutrition quizzes (testing basic knowledge of food groups and daily requirements) with small prizes and interactive nutrition activities such as weighing sugar in various foods.
‘In-hospital camp’ refers to a day camp offered on the hospital campus for children who could not or preferred not to travel to the sleep-away camps. The in-hospital camp was mixed ages and mixed gender. Children were broken up into ‘cabins’ by age and they rotated through various activities set up around the hospital. In-hospital camp cooking classes were approximately 45 min in length and held in a recreation room. This room contained a sink but no oven or burners. These classes were distinct from the hospital classes described below, which were offered all year and not associated with a special camp event.
Hospital classes
One-hour cooking classes were offered monthly on the inpatient floor of the children’s cancer hospital in collaboration with the hospital school programme. Classes were held in a kitchen with counter space, cooking supplies, a microwave and an oven. The kitchen was convenient to patients (less than 30 m (100 ft) walk from patient rooms) and classes were open to family members who wished to attend, including siblings and parents. Announcements for the classes were posted in clinic waiting room areas and on the monthly events calendar distributed to patients.
Content of cooking classes
Cooking classes were offered between April 2015 and April 2016. Classes at all sites aimed to teach specific behaviours of healthy cooking adopted from an evidence-based conceptual framework developed by the authors (Table 1)( Reference Raber, Chandra and Upadhyaya 16 ). Conversations with camp leadership and in-hospital participants helped inform the recipes chosen for each class, while the framework guided recipe changes and class talking points. The recipes represented healthier versions of popular foods (e.g. healthy pizza) and alternatives to unhealthy processed foods (e.g. fresh fruit-sweetened drinks). Recipes used in classes were altered based on the conceptual framework (e.g. using whole grains, adding vegetables and reducing cheese). These changes to traditional recipes were highlighted during the cooking demonstrations to encourage understanding of healthy cooking strategies.
All cooking classes included participatory elements, where children were taught age-appropriate cooking skills. Children were encouraged to help measure, mix, prepare foods for baking and plate final dishes. Most classes included some element of personalization, wherein each child was given the opportunity to individualize his/her dish by adding or subtracting ingredients or amounts. Recipes used in classes for teens were generally more complex than those used for younger children, with more steps and participation required including knife skills and cutting practice.
An online recipe website developed by researchers (https://atthetable.mdanderson.org) was used for sourcing appropriate recipes and as a mechanism for sharing new recipes developed for cooking classes. The online cookbook was created by our group through collaboration with patient families and physicians and consists of over 500 dietitian-approved recipes searchable by type, texture, colour, preparation time and appropriateness for common symptoms( Reference Li, Raber and Chandra 17 ). Although many classes allowed participants to personalize dishes, recipes provided on the website served as core recipes for classes.
Field notes were collected for each cooking class offered in hospital and camp settings. These field notes documented information relevant to the implementation of the cooking classes including total numbers of classes, students, perceived participant enjoyment and key behaviours from the conceptual framework emphasized during each class. Field notes also documented participants including age range, gender (male, female or mixed), number of parents, general attitude of the class, and reactions to recipes and cooking behaviours taught. The constructs from the conceptual framework of healthy cooking and their individual interpretations used during the classes were documented to assess the utility in using a framework for healthy cooking class development. No identifying information was collected. Notes were audio-recorded or typed after class. Audio field notes were transcribed and resulting information compiled for review. The study was reviewed by The University of Texas MD Anderson Cancer Center Institutional Review Board and deemed exempt (PA16-0318).
Results and discussion
A total of twenty-four classes were offered to 189 participants of varying ages. Seventeen classes were taught at camps and seven classes in the hospital. The majority of classes were mixed ages and mixed gender. Parents attended some of the hospital classes but were not present at camp activities. In-hospital classes varied widely in participant numbers, as patients were continually discharged and others admitted. A total of twenty-four children and thirteen parents, with or without their children, joined the hospital cooking classes over the course of the year. Camp classes were generally filled to capacity, with an average of ten students per class (Table 2).
While the classes varied in location, equipment, size and recipe, a similar four-step process was used to develop the lesson for each cooking class: (i) recipes were selected with input from participants; (ii) recipes were altered using the conceptual framework of healthy cooking; (iii) alterations to the recipes were used as talking points during class; and (iv) recipes were added to the ‘At The Table’ online cookbook (https://atthetable.mdanderson.org). Dessert and snack recipes were the most common types of recipes used during classes as they were the foods most often requested by participants at the hospital, as well as camp leadership. Further, these more individual-sized dishes allowed for easier personalization by participants and made a portable snack after class the children could eat immediately or take with them. The flexibility of the conceptual framework allowed for the snack and dessert recipes to be adapted using the constructs and sub-constructs (Table 1).
Across all classes, twelve different behaviours from the conceptual framework were used in various capacities (Fig. 1). Certain behaviours were used more often than others, with reducing sweeteners and animal fats being the most common. The behaviours of avoiding processed foods and avoiding processed meats were used less often. Some behaviours were not used at all as accommodations needed to be made with regard to the environment, kitchen equipment available and time allotted. For example, we chose to limit recipes that required heating especially on hot camp days, so behaviours relating to heat cooking methods were used less often. Also, recipes that did not require ovens or stoves were chosen when those facilities were not available. Classes were further tailored to the age and ability of participants. For example, a teen class may include a demonstration of how to make pizza dough, while pre-made dough would be provided for younger children.
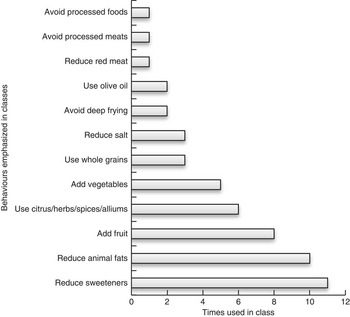
Fig. 1 Frequency of behaviours from the conceptual framework of healthy cooking emphasized during twenty-four healthy cooking classes for childhood cancer survivors (n 189) and their parents (n 13) at one paediatric cancer hospital inpatient unit, one paediatric cancer in-hospital camp programme and two off-site paediatric cancer summer camp programmes, April 2015–April 2016
The behaviour of ‘adding fruits and vegetables to dishes’ was also an opportunity for children to personalize their individual dish by choosing the types of produce to include. This exercise revealed information about participants’ favourite fruits and vegetables. Some fruits, such as berries, mangoes and grapes, were more popular with children than fruits such as cantaloupe. When other ingredient additions such as chocolate chips and nuts were offered along with fruit, fruit was mostly ignored in place of the alternatives.
Encouraging participants to add vegetables to dishes was more difficult. When offered a choice, many children opted to not add vegetables at all and leave dishes plain (e.g. plain cheese pizza, lettuce-only spring rolls). Children noted enjoying preparing dishes with vegetables in class; however, they did not always consume the entire dish. Data on receptivity to new foods suggest it takes repeated exposure before children are able to form an opinion on a new food( Reference Lakkakula, Geaghan and Zanovec 18 ). Cooking classes that encourage hands-on preparation of vegetables and freedom for individual choice may help children engage with new types of produce.
The behaviour of ‘using citrus, herbs, spices and alliums’ offered another opportunity for participants to make individual or group decisions when flavouring recipes. Spices and herbs were presented as optional and participants were given the opportunity to taste, smell and discuss different flavour possibilities. Vanilla, cinnamon and ginger were among the most popular flavourings for sweet foods. Strong flavours such as chillies, oregano and garlic were popular for savoury dishes. Many CCS experience changes in taste as a result of certain treatments( Reference Bodánszky 19 ). Stronger flavours may be preferred by those with reduced taste sensitivity, while those with mouth sores may require blander foods. The impact of treatment on taste should be kept in mind when creating cooking classes for paediatric cancer patients; offering a variety of herbs and spices can allow class participants to alter flavours to their preference.
In general, classes were well received both by children and teenagers as gauged by attendance and interaction with instructors and other participants. Camp classes were better attended than hospital classes, but parents showed appreciation for the hospital classes and took the opportunity to ask food and nutrition questions. The difference in participation between camp and in-hospital classes may be due to the fact that the children attending camp were healthier and more active than those in the hospital, and therefore more willing to participate.
Camp classes were full nearly to capacity in both teen and children’s camps. The camp director noted that although campers were not always willing to eat all of the foods made during classes, they enjoyed the sessions and the opportunity to learn cooking skills. Camp counsellors and teenage participants also asked nutrition and cooking questions to instructors during the cooking classes. Younger CCS focused on participation during the cooking classes (identifying, mixing and measuring ingredients) as opposed to nutrition inquiries.
After teen camp classes, the instructors held a group discussion about the students’ favourite and least favourite cooking classes during camp, what they may be interested in learning to prepare in the future, if they felt the information we provided was helpful and any general suggestions. Teenage campers mentioned pizza and beverages (smoothies, juices, etc.) were their favourite two classes, and the date-energy bites and veggie spring rolls their least favourite. Teen campers also mentioned wanting to learn more egg-based recipes. After hospital classes, instructors answered any questions from parents and took requests for subsequent class themes or recipes. This was done to keep participants engaged in the class process and for planning future classes.
Paediatric cancer patients may experience symptoms during treatment that can impact diet and eating habits( Reference Bodánszky 19 ). During one class on the hospital inpatient floor, a teenage participant with a throat injury noted all fruit she ate needed to be cut up into small pieces. Class instructors made accommodations by offering some fruit options in finely cut form. In another class, one participant was following a neutropenic diet and would not eat raw fruits or vegetables. Neutropenic diets aim to reduce exposure to bacteria in foods and patients with weakened immune systems sometimes choose to follow these diets( Reference Sonbol, Firwana and Diab 20 ). This class included two recipes: a cooked fruit dish and raw fruit salad, allowing the child to participate fully in at least half of the class and have something to sample with the group. Considerations should be made when working with childhood cancer patients to promote fruit and vegetable intake within the bounds of a patient’s preferences and abilities( Reference Zhang and Parsons 21 ).
The implementation of cooking classes in the context of a paediatric oncology camp and hospital setting revealed several factors for further consideration in future programming. Community engagement played a key role in the development of cooking classes for the various age groups and settings. By engaging the end users (child patients/survivors) in choosing initial recipes, we could ensure the dishes we prepared would be at least somewhat relevant to the audience. Having a flexible framework to guide the recipe modifications was important, as it allowed staff to honour recipe requests while maintaining consistent messaging regarding healthy cooking habits. The demonstrated relevance of the constructs across different types of dishes, such as snacks and desserts, suggests they may also useful when adapting culturally diverse recipes.
The present study had several limitations. As it was an observational study based on ethnographic field notes, the results are not generalizable to the entire population of paediatric cancer survivors. Field notes were kept relatively brief due to limited staff. Ages of participants varied widely and there was no follow-up. More in-depth qualitative research techniques such as interviews and focus groups were not used in the study, which would have given more depth to the results.
Hands-on cooking classes show promise for improving children’s food choices and attitudes about healthy foods( Reference Hersch, Perdue and Ambroz 10 ). Parents and children being engaged during these preliminary classes suggests cooking classes could become a part of standard paediatric camp programming. The current report could be used as a model for a more formal camp cooking programme.
Conclusion
The present communication is the first reporting reactions to camp- and hospital-based healthy cooking classes for CCS. This report of the development and initial implementation of cooking classes suggests promise for using a conceptual framework of healthy cooking to teach relevant skills to paediatric cancer populations. The use of an evidence-based conceptual framework for guiding cooking classes is an important addition to the literature, as current cooking interventions vary widely in content( Reference Engler-Stringer 22 ). By using a flexible, evidence-based framework, practitioners can standardize healthy cooking curricula while remaining accommodating to an individual community’s needs and cultural norms. While findings from the current pilot study suggest cooking classes may be a feasible method for teaching relevant skills, the extent to which classes elicit behaviour change is unknown. One of the major limitations of the existing literature on healthy cooking is the lack of validated metrics for evaluating cooking behaviour( Reference Reicks, Trofholz and Stang 15 , Reference Raber, Chandra and Upadhyaya 16 ). The development of a validated assessment tool to measure cooking practices based on the framework is currently underway and will be used in subsequent trials of healthy cooking interventions for CCS. Studies exploring the impact of cooking programmes on dietary intake, anthropometrics and/or quality of life should be considered for future research.
Acknowledgements
Acknowledgements: The authors would like to acknowledge Rhea Li, MPH, RD, Melvin Covington and Elizabeth Escobedo for assistance on this project. The authors would also like to thank e-Health Technology for e-cookbook development and the Center for Energy Balance in Cancer Prevention and Survivorship at MD Anderson. Financial support: This project was supported by the MD Anderson Children’s Cancer Hospital’s ON to Life Program with funding from the Archer Foundation and Cancer Center Support Grant. Research reported herein was supported by the National Cancer Institute of the National Institutes of Health (NIH) (award number R25CA057730; Principal Investigator: Shine Chang, PhD). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. A portion of this research was supported by the Albert Schweitzer Fellowship. These funding organizations had no role in the design, analysis or writing of this article. Conflict of interest: None. Authorship: M.R. developed the conceptual framework of healthy cooking, organized, scheduled and conducted the cooking classes, as well as took and transcribed field notes and organized this manuscript. K.C. assisted with teaching the cooking classes, gathering data and reviewing the manuscript. J.C. oversaw the development and implementation of all aspects of this project, and supervised analysis and manuscript production. Ethics of human subject participation: This study was reviewed by The University of Texas MD Anderson Cancer Center Institutional Review Board and deemed exempt (PA16-0318).






