A preeminent health concern in the USA is poor cardiovascular health, which serves as a precursor to leading causes of death including heart attack, heart failure and stroke(Reference Benjamin, Muntner and Alonso1). CVD in the USA also carries a large economic burden, estimated to cost over $1 trillion annually by 2030(Reference Heidenreich, Trogdon and Khavjou2). Community-level factors such as disorderly physical conditions, area socioeconomic status and lack of community resources may be linked to cardiovascular health risk(Reference Boylan and Robert3,Reference Browning, Cagney and Iveniuk4) . Nonetheless, there has been a paucity of research assessing whether local food retail environments are associated with cardiovascular health(Reference Kelli, Hammadah and Ahmed5,Reference Kelli, Kim and Tahhan6) .
In recent years, accessibility to food retailers has been increasingly identified as an important feature of communities for health and well-being(Reference Lytle and Sokol7). Healthy People 2020 considers availability of local food markets that provide healthy foods to be a key social determinant of health(8). Of particular interest are the health consequences of living in a food desert (i.e. geographical areas that lack access to retailers which provide nutritious food items)(Reference Beaulac, Kristjansson and Cummins9,Reference Walker, Keane and Burke10) . According to recent estimates, approximately 23·5 million Americans reside in food deserts(Reference Ver Ploeg, Breneman and Farrigan11).
There are several reasons to expect living in a food desert will influence cardiovascular health. First, because individuals often make dietary decisions based on which food retailers are locally available, residents of food deserts tend to have poorer quality diets marked by a greater intake of high energy, nutrient-deficient foods(Reference Walker, Keane and Burke10,Reference Gray, Lakkur and Howard12) . Second, residents who seek to maintain a nutritious diet while living in a food desert must travel further distances to obtain healthy food options, thereby spending greater amounts of time acquiring food, and in turn reducing overall time for physical exercise or leisure activity(Reference Dubowitz, Ghosh-Dastidar and Eibner13,Reference Dubowitz, Zenk and Ghosh-Dastidar14) . A third possibility suggests that any relationship may be spurious given that those who live in food deserts are often more economically deprived than those who do not(Reference Walker, Keane and Burke10). Therefore, any adverse association may result from larger socioeconomic challenges rather than issues related to food accessibility. Finally, socioeconomic status may moderate the association between food deserts and cardiovascular health as economic resources can buffer against the challenges of living in a food desert(Reference Kelli, Hammadah and Ahmed5).
Past work finds that reduced accessibility to grocery stores is associated with select cardiovascular health outcomes such as hypertension(Reference Dubowitz, Zenk and Ghosh-Dastidar14), higher systolic blood pressure(Reference Suarez, Isakova and Anderson15), as well as all-cause mortality and heart-failure hospitalisation(Reference Morris, McAllister and Grant16). While informative, these prior studies use single measures of cardiovascular health conditions, which provide limited insight into the complexities of cardiovascular health risk. Indeed, the American Heart Association (AHA) has outlined a series of metrics that encompass a broader definition of cardiovascular health risk that includes both markers of physical health such as, BMI, total cholesterol, blood pressure and fasting plasma glucose, as well as health behaviours including smoking, physical activity and dietary patterns(Reference Lloyd-Jones, Hong and Labarthe17).
More recently, a series of studies conducted in Atlanta demonstrated that persons living in a food desert had a higher prevalence of hypertension, smoking, BMI, fasting glucose(Reference Kelli, Hammadah and Ahmed5) and 10-year risk for CVD(Reference Kelli, Kim and Tahhan6) relative to those who did not live in a food desert. However, further analyses demonstrated that the association between food desert residence and adverse cardiovascular health outcomes was rendered statistically non-significant after accounting for area income and individual income(Reference Kelli, Hammadah and Ahmed5,Reference Kelli, Kim and Tahhan6) . This raises the possibility that any association between food deserts and cardiovascular health may result from economic deprivation rather than food access. As Kelli and colleagues’ surmise ‘whether neighborhood access to healthy foods is driving these disparities above and beyond income levels at the personal or neighborhood level remains poorly studied.(Reference Kelli, Hammadah and Ahmed5)’
The objective of the current study is to extend the extant literature by (1) assessing the association between living in a food desert and an index of cardiovascular health risk using a nationally representative sample of young adults living in urban census tracts in the USA and (2) evaluating the degree to which personal and area socioeconomic status conditions this relationship.
Data
Data for this study come from National Longitudinal Study of Adolescent to Adult Health (Add Health), an ongoing, nationally representative study of adolescents enrolled in either middle or high school during the 1994–1995 academic year(Reference Harris18). The initial sample was obtained from a stratified random sample of 132 schools. Approximately 20 000 students were selected to participate in the Wave I in-home interviews. Following the initial interview, a subset of respondents participated in follow-up interviews at Wave II (1996), Wave III (2001–2002) and most recently Wave IV (2008). At Wave IV, respondents were between the ages 24 and 34 years and 15 701 respondents participated in interviews.
The current study draws on data from Wave I and Wave IV. Wave I data are selected to account for pre-existing socio-demographic characteristics, and Wave IV data are used to measure the key dependent, independent and mediator variables. The final analytic sample was obtained through several stages. First, we began with the 15 626 respondents who participated in Wave IV and had a valid response on the food desert measure. Because the measure of food deserts in the Add Health data are valid only for urban census tracts(Reference Santorelli and Okeke19,Reference Testa20) , we restrict the sample to respondents who reported living in urban areas based using Rural-Urban Commuting Area codes (n 11 493). Further, as pregnancy may impact the measurement of physical health markers and health behaviours, we limit the sample to those reporting that they are currently not pregnant or not ‘probably pregnant’ (n 11 110)(Reference Testa and Jackson21). Finally, the sample is restricted to those with valid response on key variables of interest. After these restrictions, the final analytic sample was composed of 8896 respondents. The procedure for selecting the final analytic sample for the current study is detailed visually in Fig. 1. This study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving research study participants were approved by the University of Texas at San Antonio Institutional Review Board.

Fig. 1 Sample selection flowchart for the National Longitudinal Study of Adolescent to Adult Health Waves 1 and IV
Dependent variable
The measurement of cardiovascular health is based on the American Heart Association definition of cardiovascular health and past research using Add Health data(Reference Lawrence, Hummer and Harris22,Reference Lawrence, Hummer and Domingue23) . Specifically, the American Heart Association has comprised cardiovascular health as a broad concept that entails at least seven factors capturing characteristics of both biological physical health markers and health behaviours: BMI, smoking, physical activity, diet, blood pressure, blood glucose and cholesterol(Reference Lloyd-Jones, Hong and Labarthe17). At Wave IV of the Add Health Study trained and certified interviewers obtained key anthropometric data on weight and height, as well as cardiovascular measures including blood pressure, and biomarker measures of blood glucose and cholesterol obtained from dried blood spots(Reference Harris18). Respondents also self-reported health behaviours including cigarette consumption, physical activity and sugar consumption. Consistent with the coding of prior research using Add Health data, we operationalised each of the seven constructs as ideal, intermediate, or poor(Reference Lawrence, Hummer and Harris22,Reference Lawrence, Hummer and Domingue23) . Each indicator is coded as a mutually exclusive category on a 0–2 scale (0 = ideal, 1 = intermediate, 2 = poor). Values were summed to generate a 14-point scale, where higher values indicate poorer cardiovascular health. Information on the definitions and coding of each measure is detailed in online Supplemental Appendix A.
Independent variables
Food desert measures whether a respondent lives in a census tract that has no access to healthy food retailers at Wave IV. Data on food retailers come from the Centers for Disease Control and Prevention (CDC) Modified Retail Food Environment Index (mRFEI)(24). The mRFEI measures the ratio of healthy to unhealthy food retailers in a census tract and the half mile buffer around that census tract. The mRFEI compiled information on over 1 million food retailers during 2008–2009. The mRFEI score is calculated as follows:
 $${\eqalign{ {\rm{mRFEI}} = {{100 \times}} \cr {{{\rm{\# Healthy\ food\ retailers}}} \over {{\rm{\# Healthy\ food\ retailers}} + {\rm{\# Unhealthy\ food\ retailers}}}}$$
$${\eqalign{ {\rm{mRFEI}} = {{100 \times}} \cr {{{\rm{\# Healthy\ food\ retailers}}} \over {{\rm{\# Healthy\ food\ retailers}} + {\rm{\# Unhealthy\ food\ retailers}}}}$$
Based on the recommendation of the CDC, food deserts are classified as areas that have an mRFEI score of 0 (i.e. areas have no healthy food retailers). Prior research suggests that the geographic boundary used by the CDC is valid to measure the presence of food deserts in urban areas(Reference Santorelli and Okeke19). The mRFEI data were linked with Add Health data through the ancillary studies program(Reference Testa20).
Control variables
We control for several socio-demographic characteristics including respondent age at Wave IV, race/ethnicity (White, Black, Hispanic or other race), sex (1 = male; 0 = female), high school graduate (1 = yes; 0 = no) and whether a respondent reported being married at wave IV (1 = yes, 0 = no). Because the impact of the food environment may differ if a young adult lives on their own or with parents who can provide resources to buffer against adversities, we include a binary measure of whether a respondent reported living in their parent’s home at Wave IV (1 = yes; 0 = no). In addition, to capture previous health and health behaviours, a binary measure of the use of any illegal drugs aside from marijuana during adolescence (1 = yes; 0 = no) and self-rated health in adolescence (excellent, very good, good, fair and poor) are included. To measure early life socio-economic status, we include a variable for Wave I census tract socioeconomic status, which is a standardised ten-point scale based on the proportion of persons in a respondent’s Wave I census tract who are on welfare, living at or below the poverty line, are unemployed and female-headed households (Cronbach’s Alpha = 0·984). Finally, we include a control variable for population density, which measures the density of persons per kilometre within a census tract at Wave IV. The natural logarithm of population density is used to reduce positive skew.
Conditioning variables
Consistent with prior research(Reference Kelli, Hammadah and Ahmed5), this study examines whether any association between food deserts and cardiovascular health is conditioned by area and personal socioeconomic status. Similar to the measure detailed above, we include a measure of census tract socioeconomic status at a respondents Wave IV census tract using a standardised ten-point scale based on the prevalence of welfare, poverty, unemployment and female-headed households (Cronbach’s Alpha = 0·821). Household income is measured using a self-reported survey item asking respondents what their household income was before taxes and deductions. Income levels were reported in intervals ranging from less than $5000 to $150 000 or more. The mid-point of each response category was used to generate a continuous income measure(Reference Gooding, Walls and Richmond25). Next, household income was adjusted for the number of persons living in a household using the equivalence of scale method: adjusted household income = household income/(household size) × 0·5. Income was log transformed to reduce positive skew.
Statistical procedures
The relationship between living in a food desert and cardiovascular health is assessed using ordinary least squares regression. The results are presented with a progressive modelling approach: (1) The direct bivariate association is assessed, (2) control variables are included in the model and (3) mediator variables are added. Potential mediation effects are assessed using the Karlson–Holm–Breen method to examine the degree to which each mediator variable reduces the association between living in a food desert and cardiovascular health(Reference Karlson, Holm and Breen26). While the KHB approach was originally created for mediation in non-linear models, the procedure is valid for calculating mediation in ordinary least squares regression models and offers the benefit of allowing multiple mediators and decomposing the indirect effect attributed to each mediator variable(Reference Kohler, Karlson and Holm27). Finally, we conduct a moderation analysis to determine whether the influence of living in a food desert on cardiovascular health differs conditional on personal or area socioeconomic status. To do so, respondents are separated into tertiles based on socioeconomic status (low, moderate and high), then food desert residence is regressed on cardiovascular health conditional on level of socioeconomic status. Variance inflation factors were below two across all models, indicating no issues with multicollinearity(Reference Allison28).
Results
Table 1 presents the descriptive statistics of the analytic sample. Approximately 16·5 % of respondents live in a food desert. The mean value of the cardiovascular health score is 5·19 and ranges from 0 to 14. Table 2 presents the result of the ordinary least squares regression regression assessing the association between living in a food desert and cardiovascular health risk. The results in Model 1 demonstrate a positive association between residence in a food desert and cardiovascular health risk (β = 0·062, P < 0·001). Thus, in the bivariate model, living in a food desert is associated with a 0·062 sd increase in the cardiovascular health index. After including the control variables in Model 2, the positive association between food deserts and cardiovascular health problems remains (β = 0·048, P < 0·01). Model 3 adds the mediator variables, which reduces the magnitude of the association between food deserts and cardiovascular health risk, though food desert residence retains a positive and statistically significant association with cardiovascular health risk (β = 0·035, P < 0·05). The results of the KHB mediation analysis presented in Table 3 indicate tract socioeconomic status reduces the association between living in a food desert and cardiovascular health by 19·93 % (z-score = 4·15, P < 0·001) and household income reduces the association by 7·79 % (z-score = 2·45, P < 0·05).
Table 1 Weighted summary statistics of analytic sample (n 8896)
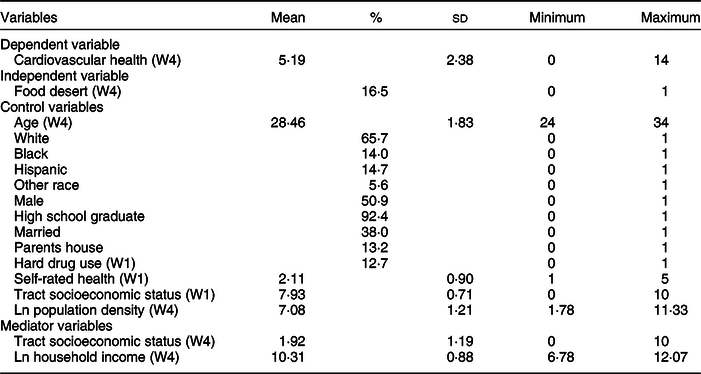
W1, Wave 1; W4, Wave 4.
Table 2 Results of ordinary least squares regression (OLS) regression of cardiovascular health index on food desert and other covariates (n 8896)

b, unstandardised coefficient; β, standardised coefficient; W1, Wave 1; W4, Wave 4: Cardiovascular health index ranges from 0 to 14 (higher scores indicate worse health).
**P < 0·01, ***P < 0·001.
Table 3 Karlson–Holm–Breen (KHB) test of mediators between food desert and cardiovascular health

*P < 0·05, **P < 0·01, ***P < 0·001.
Figure 2 stratifies the sample by tertiles of area and personal socioeconomic status. The results highlight that the positive association between living in a food desert and cardiovascular health problems is concentrated among the lowest socioeconomic status respondents. This is the case for both personal (β = 0·086, P < 0·01) and area (β = 0·090, P < 0·001) socioeconomic status. Summary statistics of the composition of the stratified samples are provided in online Supplemental Appendix B.

Fig. 2 Standardised coefficients from ordinary least squares regression (OLS) of cardiovascular health index regressed on food desert conditional on personal income and area socioeconomic status (SES). Control variables are the same as in Table 1; cardiovascular health index ranges from 0 to 14 (higher scores indicate worse health). Standardised coefficients are reported. **P < 0.01; ***P < 0.001
Online Supplemental Appendix C presents the results from a multinomial logistic regression analysis using the classifications of individual cardiovascular indicators as ideal, intermediate or poor as the dependent variable. In the bivariate analysis, food desert residence is associated with poorer smoking, blood glucose and sugar consumption. However, after the inclusion of the control and mediator variables, several associations are reduced to statistical non-significance. Ultimately, living in a food desert retains an association only with smoking in the fully specified model.
Discussion
Poor cardiovascular health is a serious public health issue in the USA. Indeed, recent research suggests that cardiovascular health problems may underlie current declines to life expectancy in the USA(Reference Mehta, Abrams and Myrskylä29). The CDC’s Division for Heart Disease and Stroke Prevention notes that several modifiable risk factors serve as leading causes for heart disease and stroke, including high blood pressure, high cholesterol, smoking, poor nutrition, lack of physical activity, diabetes and obesity. Accordingly, identifying ways to reduce risk factors and improve cardiovascular health has become a leading objective in the endeavour to advance population health(8). It is particularly important to identify risks for cardiovascular health problems among young adults, given that the prevalence of cardiovascular health problems among young adults are rising, yet research on risk factors for cardiovascular health among this population remains limited(Reference Yang, David and Singh30). Moreover, risk factors for poor cardiovascular health will likely manifest into more severe problems, including premature mortality, as individuals age(Reference Ford, Greenlund and Hong31). Thus, identifying modifiable risk factors for cardiovascular health problems during this time period provides the opportunity to develop meaningful intervention and prevention strategies(Reference Walker-Harding, Christie and Joffe32).
The findings yielded four main conclusions regarding the link between living in a food desert and cardiovascular health. First, living in a food desert is associated with poorer cardiovascular health among a sample of young adults living in urban areas in the USA. Second, we found that the association between food deserts and cardiovascular health was partially mediated by area and personal socioeconomic status. This finding differs from past research on the topic(Reference Kelli, Hammadah and Ahmed5,Reference Kelli, Kim and Tahhan6) , which found the link between living in a food desert and cardiovascular health was rendered null after accounting for socioeconomic status. This finding led us to probe how living in a food desert impacts people at different strata of the socioeconomic spectrum, leading to our third conclusion that the adverse consequences of food desert residence for cardiovascular health are concentrated among respondents in the bottom tertile of either area or personal socioeconomic status. In contrast, we found no association among moderate or higher socioeconomic respondents. These findings highlight that a lack of economic resources can make individuals more susceptible to resource deprivation. As Beaulac and colleagues explain, ‘food deserts in disadvantaged areas are arguably more of concern because a process of “deprivation amplification” may contribute to social disparities, whereby area-level disadvantage compounds individual disadvantage’(Reference Beaulac, Kristjansson and Cummins9). In contrast, individuals of higher socioeconomic status may be able to use economic resources to buffer against the adversities of living in a food desert. The difference in effect across socioeconomic strata suggests that poorer cardiovascular health may not just be a result of a lack of access to healthy foods but also greater exposure to multiple types of deprivation(Reference Chen and Kwan33,Reference Mackett and Thoreau34) .
Finally, our examination of the seven individual cardiovascular health indicators that comprised the overall index suggested that living in a food desert has the strongest association with greater cigarette use. One possibility is that engagement in worse health behaviours via living in a food desert may be a partial function of the composition of the type of retail outlets in the area. For instance, food deserts tend to have a larger composition of unhealthy retailers that sell cigarettes and advertise the sale of tobacco products on store fronts(Reference Gordon, Purciel-Hill and Ghai35,Reference Tolzman, Rooney and Duquette36) (such as convenience stores or neighbourhood bodegas), which may translate into poorer health behaviours(Reference Whelan, Wrigley and Warm37). To be sure, prior research consistently identifies smoking as a key risk factor for poor cardiovascular health among young adults(Reference Carroll, Huffman and Zhao38–Reference Sabogal, Su and Tingen41).
Policy and practical implications
The findings of the current study have implications for improving local food retail environments, which in turn may enhance cardiovascular health. First, in communities that lack access to full-service grocery stores, but contain a number of convenience stores or bodegas, these smaller retailers in distressed communities can stock healthier options, as well as limit unhealthy items such as tobacco products(Reference Gittelsohn, Rowan and Gadhoke42,Reference Ribisl, D’Angelo and Evenson43) . Second, mobile food markets should be more widely expanded to service food deserts. Mobile markets use automobiles, buses, trucks or trailers, as an alternative to brick-and-mortar stores to provide healthy food options directly to communities with low food access(Reference Zepeda, Reznickova and Lohr44). Past research finds that mobile market availability improves dietary behaviour in food deserts(Reference Gary-Webb, Bear and Mendez45). Third, bolstering community gardens and farmers’ markets can improve access to fresher healthier food, as well as increase physical movement and neighbourhood cohesion(Reference Wang, Qiu and Swallow46). Finally, to the extent that living in a food desert and experiencing food distress increases unhealthy behaviours such as smoking(Reference Kelli, Hammadah and Ahmed5,Reference Hosler and Michaels47,Reference Kim-Mozeleski and Pandey48) , alleviating nutritional hardships in food deserts may help improve health behaviour and in turn enhance cardiovascular health.
Limitations and directions for future research
There are limitations in the current study that can be expanded upon in future research. First, there may be some unobserved variables that confound the association between food desert residence and cardiovascular health such as the food environments that individuals resided in during previous waves, as well as items regarding the modes of transportation available to a respondent. Unfortunately, these variables were not available in the data used for this study. Second, the measure of food deserts is based on geographic access to food retailers. However, future research should consider other important features of food environments, including the cost and quality of food available to local residents. Third, the current study uses a measure of food retailer access created by the CDC, which defines food deserts based on geographic access to healthy and unhealthy food retailers. Ultimately, there are several ways to define food deserts, and it would be useful for future research to use alternative measures of food deserts, such as those by the United States Department of Agriculture, which defines food deserts in terms of both income and geographic food access. Fourth, to the extent that living in a food desert alters dietary patterns, it would be valuable for future research to evaluate how the relationship between living in a food desert and health is explained by dietary behaviour. Fifth, based on the measurement of food deserts available in the mRFEI data, the sample was restricted to residents living in urban census tracts. However, past research suggests that cardiovascular health among young adults differs between those residing in urban and rural areas(Reference Lawrence, Hummer and Harris22). Sixth, this study used the most recent wave of Add Health data (Wave IV measured in 2008). Still, certain features may have changed over the past decade that change the impact of food deserts on health outcomes. For instance, mobile food delivery applications have proliferated in recent years. Accordingly, it would be valuable for future research to assess the relationship between living in a food desert and cardiovascular health using more recent data.
Despite the noted limitations, we find numerous avenues for future research. One possibility for subsequent studies is to link food desert data through the ancillary studies program with Wave V Add Health data, collected in 2016–2018 and scheduled to be released in the near future. In addition, the current study evaluated the degree to which personal and area socioeconomic status both mediated and moderated the relationship between living in a food desert and cardiovascular health. An alternative possibility is that socioeconomic status determines the location of where one lives (i.e. food environment), and in turn, one’s local food environment shapes health behaviours, which then influences cardiovascular health. While data limitations prevented a test of this theoretical pathway in the current study, future research that explores the relationship between socioeconomic status, food environments, nutrition and health over time would be extremely valuable. Finally, food environments may be influenced by features such as attending school or work outside of one’s local neighbourhood, as well as food delivery services. While the current study lacked the data to account for these features, future research that investigates food environments based on the location of one’s home residence, as well as features such as where individuals travel to school and work on a regular basis, would be particularly instructive.
Conclusions
It is well established that food deserts are intertwined with a host of adverse social, economic and health outcomes. The present study revealed that cardiovascular health is closely connected to accessibility to food retailers, particularly for residents who experience economic deprivation, as well as lack of access to healthy food retailers. We advocate for policy efforts to increase the accessibility of affordable, nutritious foods for those currently living in food deserts. We also argue that such policies should be part and parcel of the effort to improve cardiovascular health among young adults in the USA. Future research should continue to examine the relationship between food deserts and health outcomes, as well as assess the efficacy of intervention strategies that might serve to mitigate the deleterious health effects of residing in a food desert.
Acknowledgements
Acknowledgements: This research uses data from Add Health, a program project directed by Kathleen Mullan Harris and designed by J. Richard Udry, Peter S. Bearman and Kathleen Mullan Harris at the University of North Carolina at Chapel Hill and funded by grant P01-HD31921 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, with cooperative funding from twenty three other federal agencies and foundations. Information on how to obtain the Add Health data files is available on the Add Health website (http://www.cpc.unc.edu/addhealth). No direct support was received from grant P01-HD31921 for this analysis. Financial support: This research received no funding or financial support. Conflict of interest: Authors do not have any conflicts of interest including financial interests or relationships or affiliations relevant to the subject of the manuscript. Authorship: A.T. conceptualised the study, conducted the data analysis and contributed to the writing. D.B.J. helped conceptualise the study and contributed to the writing. D.C.S. contributed to the writing of the study. M.G.V. contributed to the writing of the study. All authors reviewed, commented and revised drafts of the manuscript. Ethics of human subject participation: This study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving human subjects/patients were approved by the University of Texas at San Antonio Institutional Review Board. Written informed consent was obtained from all subjects/patients.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980020001536








