Major public health organisations recommend exclusive breast-feeding for the first 6 months, followed by continued breast-feeding and solid food introduction(1,2) . Despite efforts to increase breast-feeding in the first 6 months of life, few women in the USA meet the recommended duration with only 25 % breast-feeding exclusively at 6 months and 35 % receiving any breast milk at 1 year(3). Additionally, there are stark differences in breast-feeding initiation by income, with 90 % of high-income infants receiving any amount of breast milk compared with 70 % of low-income infants, and as a result, almost twice as many high-income infants meet the recommendation for 6 months of exclusive breast-feeding compared with low-income infants(Reference Anstey, Chen and Elam-Evans4). African American infants are less likely to receive any breast milk (64 %) compared with White and Latinx infants (81 %)(Reference Anstey, Chen and Elam-Evans4). These disparities can be attributed to experiences of discrimination, systemic barriers, unequal access to lactation support, and decreased employer support in service and transportation jobs, among other reasons(Reference Smith5,Reference Snyder, Hansen and Brown6) .
The US Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) aims to support low-income women and children at nutritional risk by promoting breast-feeding and providing formula and food packages(Reference Whaley, Koleilat and Whaley7). In 2022, the WIC programme served approximately 1·4 million pregnant and postpartum women and 4·8 million infants and children(8) and is an important component of the public health infrastructure for the improvement of maternal and infant health. WIC has supported breast-feeding by instituting many policies to incentivise breast-feeding, for example, the 1997 ‘Loving Support Makes Breastfeeding Work’ campaign was instituted based on social marketing principles to increase breast-feeding initiation rates and breast-feeding duration(Reference Bartholomew, Adedze and Soto9,Reference Pérez-Escamilla10) . WIC participants have lower breast-feeding rates than the general US population (71 % compared with 84 %)(3,Reference Zhang, Lamichhane and Wright11) . Compared with those who are eligible but not participating, WIC participants are less likely to breastfeed(Reference Zhang, Lamichhane and Wright11,Reference Thoma, De Silva and Kim12) , although this gap has decreased with the 2009 WIC food package change that supported and incentivised breast-feeding(Reference Whaley, Koleilat and Whaley7). WIC Infant and Toddler Feeding Practices Study-2 (ITFPS-2) is the most recent longitudinal study of the WIC population to assess feeding practices and nutritional status from 2013 to 2020, as ITFPS-1 was conducted over 20 years prior(Reference May, Borger and Weinfield13).
Social support for breast-feeding is associated with exclusive breast-feeding at 6 months and increased duration(Reference Lyons, Kay and Duke14–Reference Isiguzo, Mendez and Demirci16). Women who have increased support have higher self-efficacy, which has been linked to longer duration(Reference Maleki-Saghooni, Amel Barez and Karimi17). Social support can help minimise breast-feeding barriers and decrease perceived stress(Reference Isiguzo, Mendez and Demirci16,Reference Schindler-Ruwisch, Roess and Robert18) . Mothers are most likely to feed their children the way that their social network fed theirs, be it breast-feeding, formula feeding or mixed(Reference Schafer, Williams and Digney19). Women are also more likely to breastfeed when the baby’s father’s opinion is important to them(Reference Wallenborn, Wheeler and Lu20). This suggests that the social context in which women exist is important to feeding decisions and rates, but the literature in this area is limited. The social context is particularly important to determine in groups that are less likely to breastfeed, such as low-income and minoritised women. To further the research in this area, this study explores how familial sources of encouragement are associated with breast-feeding initiation and duration among WIC participants.
Key messages
-
Familial encouragement, particularly from partners, has the potential to help mothers begin breast-feeding and breastfeed for longer among WIC populations in the USA.
-
Understanding the influence of social networks can help practitioners better support mothers who want to breastfeed.
-
Future breast-feeding interventions should include additional family members. For example, WIC could encourage partners and family members to participate in educational programming.
Materials and methods
Target population and study sample
This study was a secondary analysis of the WIC ITFPS-2, a longitudinal study of US-based mothers participating in WIC and their children. WIC ITFPS-2 used a nationally representative sample of WIC participants with a random selection of WIC sites followed by a stratified sampling of the participants enrolled at each(Reference May, Borger and Weinfield13). Eligible participants were at least 16 years of age at enrolment and spoke either Spanish or English(Reference May, Borger and Weinfield13). Participants were enrolled prenatally, or before the infant turned 2·5 months old and were assessed via phone interview at months 1, 3, 5, 7, 9, 11, 13, 15, 18, 24, 30, 36, 42, 48, 54, 60 and 72(Reference May, Borger and Weinfield13). Data from both the core and supplemental samples were included in the analysis. The core sample was interviewed at all interviews across the first 24 months; however, the supplementary sample was only interviewed at months 1, 7, and 13 and was designed to focus on subpopulations with specific characteristics. A description of sample selection for WIC ITFPS-2 is provided in May et al.(Reference May, Borger and Weinfield13) Data collection for the first 13 months occurred from 2013 to 2015(Reference May, Borger and Weinfield13). Overall, 3777 participants were enrolled in the study, and by month 13, 74·3 % were retained (n 2807)(Reference May, Borger and Weinfield13). Although the original study applied a longitudinal approach, the current study uses the data from the first 13 months of the child’s life and applied a cross-sectional analysis.
Measures
The breast-feeding encouragement variables were based on the three questions asked during the 1-month interview about who provided support: ‘Has your husband or boyfriend encouraged you to breastfeed?’, ‘Has your mother encouraged you to breastfeed?’ and ‘Have other relatives encouraged you to breastfeed?’. The answer choices were ‘Encourage’, ‘Discourage’, ‘Mixed advice’ and ‘No advice’. The additional answers of ‘don’t know’ or ‘not applicable’ were not included. Each source of encouragement was explored separately as was a sum score. The possible range of scores for each individual source was –1 to 1, and the possible range for the sum score was –3 to 3.
Breast-feeding initiation was determined when mothers self-reported whether they initiated breast-feeding at the first interview. Breast-feeding duration was determined by mothers’ reports of if they stopped breasting and the infant’s age in days at each interview. If mothers were still breast-feeding at the time of the 13-month interview, they were assigned a value of 1 d longer than the maximum value reported for those who had stopped breast-feeding.
The control variables selected included maternal age at birth, race (Black or African American, White, and other), ethnicity (Hispanic or Latino, not Hispanic or Latino), maternal education (high school or less, more than high school), poverty status (<75 % of the 2013 Federal Poverty Limits, 75–130 %, > 130 %) and nativity (foreign-born, US born)(Reference May, Borger and Weinfield13). Control variables were selected based on their associations with breast-feeding outcomes in the current literature(Reference Anstey, Chen and Elam-Evans4).
Analytic approach
The ITFPS-2 study weights were applied to all analyses to account for unequal sampling and non-response which adjusted for WIC enrolment timing, and maternal race, weight, Hispanic origin, age, food security, language, and poverty status(Reference May, Borger and Weinfield13). Frequencies and descriptive statistics were used for univariate analysis. Bivariate analyses were conducted to assess associations with sociodemographic variables. The multivariate analysis was conducted using logistic (for dichotomous outcomes) and linear regressions (for continuous outcomes) to determine whether breast-feeding support was a predictor of breast-feeding initiation and duration. Linear regression assumptions were tested, and duration was log-transformed to meet the assumption of normality. Two regressions were conducted for each outcome: one with and one without the control variables. Statistical significance was set at a P-value of 0·05. All statistical analyses were conducted in SAS version 9.4.
Results
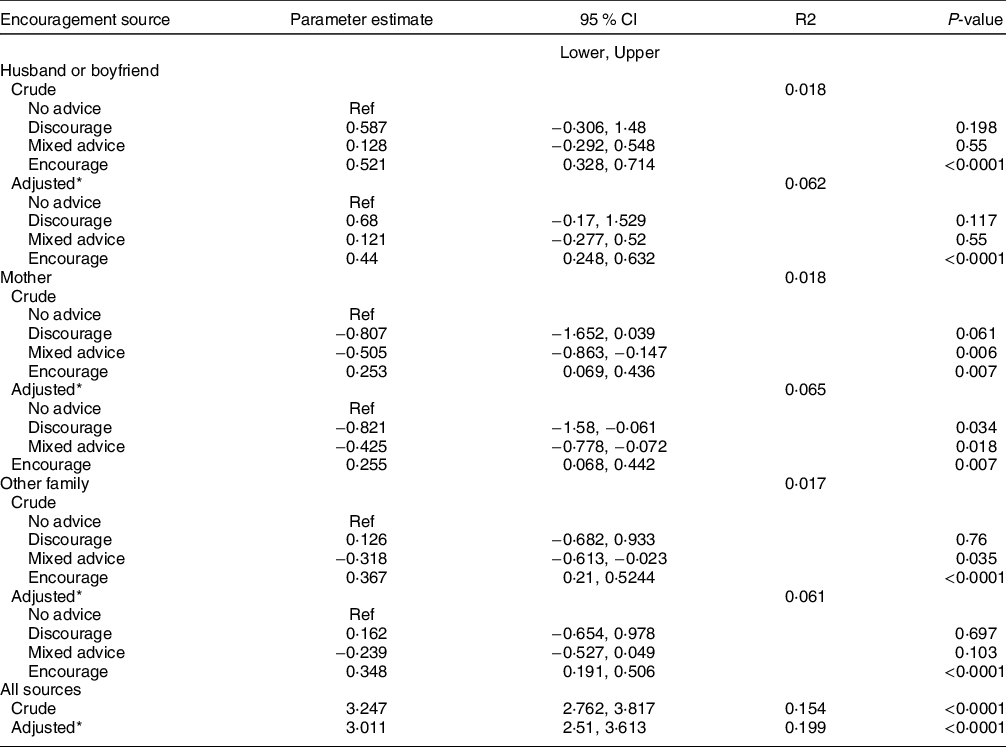
Most mothers had a high school education or less and were born in the USA(Reference May, Borger and Weinfield13). One-quarter of mothers identified as Black or African American, and about 40 % identified as Latinx(Reference May, Borger and Weinfield13). Over 80 % of mothers-initiated breast-feeding and 16 % of mothers were exclusively breast-feeding at 5 months(Reference May, Borger and Weinfield13). The mean duration of breast-feeding was 149 d (sd 157·2). The mean number of encouragement sources was 1·7 (95 % CI 1·6, 1·7). Most mothers (64·5 %) reported that husbands or boyfriends encouraged breast-feeding (presented in Table 1). Two-thirds of their mothers and 37·4 % of other relatives encouraged breast-feeding. Few mothers felt that their family discouraged breast-feeding, and discouragement ranged from 0·9 % (other relatives) to 1·6 % (their mothers).
Table 1 Sources of encouragement
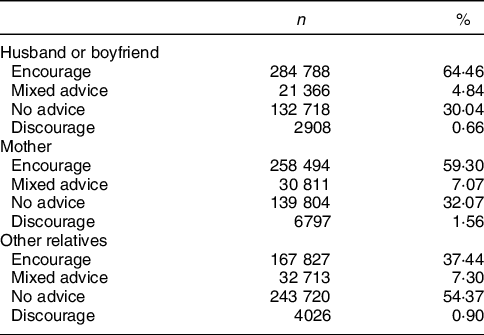
Logistic regression models for breast-feeding initiation are presented in Table 2. Husband or boyfriend, mother, and other family encouragement were all significantly associated with breast-feeding initiation, and husband or boyfriend encouragement was associated with the highest odds of initiation. The sum of all sources of encouragement was a significant predictor of breast-feeding initiation in the crude and adjusted models. In the first, each source of encouragement was associated with a 3·2 (95 % CI 2·8, 3·8) increase in the odds of initiating breast-feeding (<0·0001). After adjustment for covariates, there were 3·0 (95 % CI 2·5, 3·6) times the odds of initiating breast-feeding (<0·0001) for every additional source of encouragement. Education, nativity, ethnicity and poverty status were also significant in the model.
Table 2 Logistic regression results for predictors of breast-feeding initiation by source of encouragement
* Models adjusted for maternal age, race, ethnicity, maternal education, poverty status and nativity.
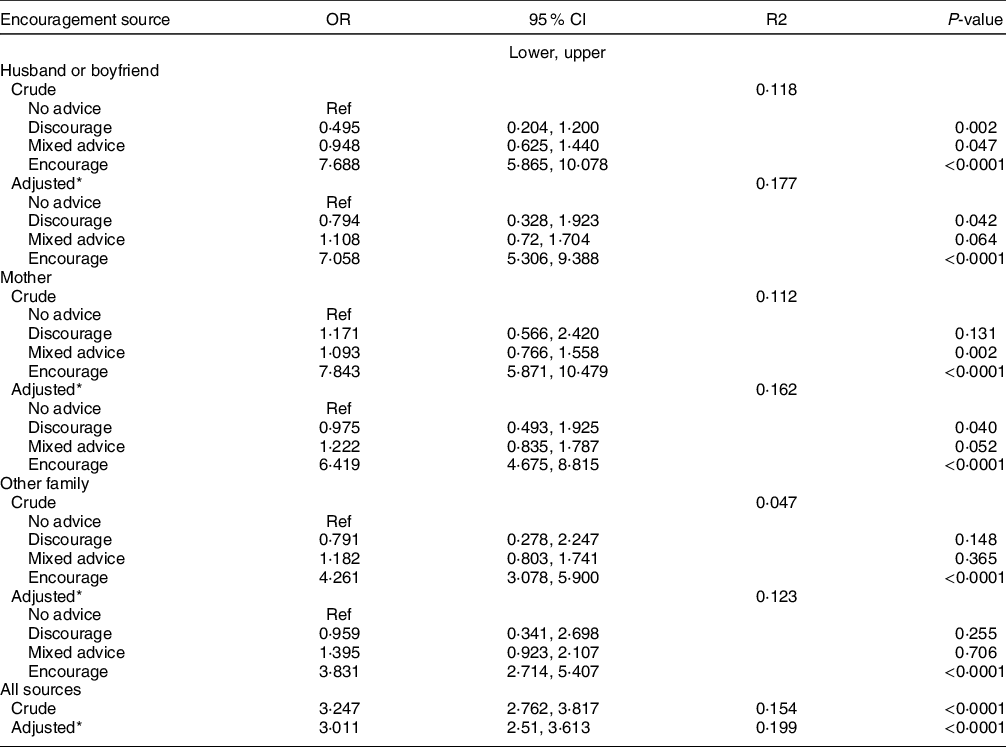
Results of the linear regression are presented in Table 3. Each of the three possible encouragement sources was significantly associated with log of the duration, with encouragement by a mother’s husband or boyfriend having the strongest association. The sum score of all sources of encouragement was a significant predictor of log of breast-feeding duration (P < 0·001); with a 1 percent increase in encouragement, there is an average increase in duration of 0·003 d (95 % CI 0·2, 0·3). Encouragement continued to be a significant predictor (P < 0·001) with an increase of an average of 0·002 d (95 % CI 0·2, 0·3) per 1 percent increase in encouragement source, controlling for age, education, nativity, poverty status, race and ethnicity. Education, nativity, age and poverty status were also significant in the model.
Table 3 Linear regression results for predictors of log of breast-feeding duration by source of encouragement

* Models adjusted for maternal age, race, ethnicity, maternal education, poverty status and nativity.
Discussion
Among a national sample of women participating in WIC, including a large racial-ethnic minoritised population, encouragement from one’s family was a significant predictor of both breast-feeding initiation and duration and encouragement from a husband or boyfriend had the strongest association. Additional sources of encouragement were associated with higher odds of initiation and longer duration in women participating in WIC even after controls were added. These findings suggest that encouragement from social network members has the potential to improve breast-feeding rates. Previously, breast-feeding women have expressed the desire to have family members that serve as breast-feeding advocates for them(Reference Grassley and Eschiti21). In another study, there was a 20 % decrease in odds of early cessation for each additional family member who supported breast-feeding(Reference Bai, Fong and Lok22). In general, women have a high level of trust in the opinions of their family members when it comes to infant feeding(Reference Moon, Mathews and Oden23).
The influence of family members, and mothers’ trust in them, provides an opportunity for intervention with additional members rather than just mothers. Particularly as family member advice is not always based on current recommendations(Reference Grassley and Eschiti21). Family members also express the desire to become more involved. Fathers in one study expressed a desire to be more involved and to learn more about breast-feeding, and programmes that provide such opportunities have the potential to improve fathers’ or other partners’ ability to encourage mothers(Reference Brown and Davies24).
Previous interventions targeting the inclusion of fathers have been associated with improved outcomes. In one study, paternal inclusion in a breast-feeding intervention was associated with longer duration and with mothers feeling they received more help and were more satisfied with the paternal support(Reference Abbass-Dick, Stern and Nelson25). Another study found that paternal involvement in interventions was associated with both early initiation of breast-feeding and exclusivity(Reference Bich, Long and Hoa26).
Potential interventions to involve fathers and other family members in breast-feeding support should include ways to bond with the infant outside of breast-feeding, as fathers can sometimes feel that breast-feeding changes the relationship with their infant(Reference de Montigny, Larivière-Bastien and Gervais27). Mothers whose partners participated in a breast-feeding intervention reported receiving better emotional and practical support, and they appreciated the additional encouragement(Reference Nickerson, Sykes and Fung28).
The WIC programme targets mothers specifically, and although some individual sites include fathers in their programming, there is no national policy(29). Fathers have expressed feeling excluded and ignored in the current WIC programming and a desire to be more involved, although on a voluntary basis(Reference Dychtwald, Kaimal and Kilby30). One potential strategy would involve encouraging mothers to invite sources of support to participate in WIC programming with them. Dychtwald found that WIC parents felt that both names could be included on appointment cards, the waiting room should be welcoming to both men and women, and that providing incentives for fathers or support people could encourage participation without requiring it(Reference Dychtwald, Kaimal and Kilby30). Previous WIC efforts to improve support include the ‘Loving Support Makes Breastfeeding Work’ campaign which was based on the Social Ecological Theory and aimed to increase public support for breast-feeding as well as increase breast-feeding rates among WIC participants(Reference Bartholomew, Adedze and Soto9,Reference Pérez-Escamilla10) . Later iterations of the campaign included a social media campaign and training for peer counselors programmes(Reference Bartholomew, Adedze and Soto9,Reference Pellechia, Soto and Haake31) . The social media campaign, which was updated in 2016 and included messaging about the importance of fathers’ and grandmothers’ support(Reference Pellechia, Soto and Haake31), was launched after the data in this study were collected, and as such, the effects are not reflected in these results.
WIC currently provides breast-feeding peer counselors in some locations to provide support and perhaps a source of encouragement. Women who have access to a peer counselor are more likely to breastfeed and meet their duration goals(Reference McCoy, Geppert and Dech32,Reference Lee, O’Leary and Kirk33) . Additional research that explores how peer counselors align with current network support and how this changes breast-feeding rates is needed.
Although WIC aims to promote breast-feeding, there is a perception among some mothers that it gives mixed-messaging by also providing free formula(Reference Barbosa, Masho and Carlyle34). This perception may impact who enrols in or continues to receive WIC(Reference Weber, Wichelecki and Chavez35). It is important to consider perceptions of WIC in any analysis of breast-feeding practices among participants as they may not be generalisable to non-WIC participants. Additional considerations include differences between local WIC programmes as women who believe that WIC is only promoting breast-feeding are more likely to continue when compared with women who believe they promote formula or both feeding methods(Reference Zhang, Li and Wouk36). Outside of WIC’s programming, there needs to be a coordinated approach to support with other healthcare organisations that serve this population, for example, including lactation care in Federally Qualified Healthcare Centers(Reference Rosen-Carole, Waltermaurer and Goudreault37).
In addition to the potential importance of breast-feeding encouragement, it is necessary to note the need to address structural barriers to breast-feeding. In the USA, there is a need for better access to paid parental leave, medical care including lactation providers and workplace protections(Reference Pérez-Escamilla38). The recently enacted PUMP act, which provides employees protected time for pumping, is an example of the needed broader societal changes(39).
Strengths and limitations
This study is one of few to explore familial sources of encouragement and breast-feeding initiation and duration. Although this study used a cross-sectional analysis with a derived variable, the continual assessment of breast-feeding practices of the first 13 months allows for more accurate duration measurement.
This study has several limitations. Familial encouragement is one factor in a broader construct of social support. The possible number of sources was limited as only husbands/boyfriends, mothers and other relatives were considered. The language of the survey was not inclusive of partners who were not a boyfriend or husband and could be phrased as spouse/partner in the future. As other relatives were only one source, it did not account for multiple family members serving as a source of encouragement. Grandmothers are valuable sources of support from both sides, so a question about the partner’s mother would strengthen the results(Reference Wallenborn, Wheeler and Lu20). The lack of information about non-family members also limits the study results, as the people with whom mothers interact are important influences in how they feed their children(Reference Schafer, Williams and Digney19,Reference Bai, Fong and Lok22) .
Additionally, as mothers self-reported breast-feeding behaviours, social desirability bias is a concern. Finally, the study is limited by the lack of variables that consider the many structural barriers that can limit breast-feeding among WIC participants, and future studies should include both the structural factors and familial encouragement.
Conclusions
This study contributes to the growing evidence that social network influence and support are important in breast-feeding practices. New mothers may be more likely to begin breast-feeding and continue breast-feeding longer when they receive encouragement from family. Future research should explore other sources of encouragement as well as include other breast-feeding populations, such as non-WIC populations. Additionally, interventions may want to consider potential sources of encouragement and include family members in their programmes.
Acknowledgements
Authorship: A.C.D. designed the study, conducted the analysis and drafted the initial manuscript. S.G. provided substantial contributions to the design of the study and interpretation of the data. S.G. and EA reviewed and provided comments on the manuscript. All authors reviewed and approved the final manuscript. Ethics of human subject participation: This study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving research study participants were approved by federally certified institutional review boards of Westat and of the University of California, Los Angeles; in addition, the study has been reviewed and approved by all state health department and local WIC agency review boards that are in the sample and that have review requirements. Written informed consent was obtained from all participants.
Financial support:
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of interest:
The authors have no conflicts of interest to report.
Supplementary material
For supplementary material/s referred to in this article, please visit https://doi.org/10.1017/S1368980023000666