Research has consistently documented associations between economic hardship (EH) in early childhood and subsequent adverse child outcomes(Reference Shankardass, McConnell and Jerrett1,Reference Shonkoff, Boyce and McEwen2) , including poorer child diet quality(Reference Jansen, Kasper and Lumeng3–Reference Webb, Zimmer-Gembeck and Scuffham11) and risk of childhood obesity(Reference Lee, Andrew and Gebremariam12). The experience of EH may be an isolated stressful event or a source of chronic stress if families experience prolonged exposure to multiple EH(Reference Alaimo13,Reference Conger, Wallace and Sun14) . Fluctuations in EH over the course of early child development may have differential effects on child outcomes such that those experiencing unexpected or extreme hardships (e.g., loss of home) may experience poorer outcomes than those with no EH, mild or temporary EH, or those that experience an underlying lower level of EH over time. The first known study to examine longitudinal trends between poverty and obesity across childhood (aged 2–12 years) demonstrated robust associations between early life poverty (before age 2 years) and adolescent-onset obesity(Reference Lee, Andrew and Gebremariam12). However, the research is limited and inconsistent, and little is known about whether this association is due to having limited access to needed resources or to effects on family processes. Existing research commonly uses federal poverty guidelines as a measure of economic strain(Reference Pabayo, Spence and Cutumisu7,Reference Min, Xue and Wang15,Reference Morris, Northstone and Howe16) . However, income-based measures are inadequate and outdated(Reference Chaudry and Wimer17) and do not account for the complexity of EH that families are likely to experience(Reference Chaudry and Wimer17) both above and below the federal poverty line(Reference Neckerman, Garfinkel and Teitler18). Because we know that experiences with different forms of EH are likely to co-occur or fluctuate, households that experience more risk factors are more likely to experience more adverse outcomes(Reference Hernandez19,Reference Dong, Anda and Felitti20) , including obesity risk(Reference Suglia, Duarte and Chambers21). Accounting for the aggregation of risk factors over time may be a better predictor than focusing on the sole contribution of a single risk factor(Reference Dong, Anda and Felitti20,Reference Sameroff, Seifer and Baldwin22) . Exposure to EH can contribute to feelings of family stress, and specifically parenting stress. Longitudinal assessments of links between prolonged EH, parenting stress and child diet outcomes are limited. Given the disproportionate risk of adverse health consequences across the life span among low-income and racial and ethnic minorities(Reference Skinner, Perrin and Skelton23,Reference Schuler24) , it is essential for prevention efforts to identify ways in which extended exposure to EH across childhood may increase risk of poorer child diet quality among high-risk groups, which may eventually lead to excess weight and chronic health complications. In the present study, we fill these gaps in the literature by examining longitudinal changes in EH from early to mid-childhood to determine whether changes in EH over time associate with child diet quality and whether parenting stress mediates this association.
Economic hardship and child diet
Foods high in saturated fats and added sugars (SFAS), such as sweet and salty snacks and sugar-sweetened beverages are typically comprised of empty energy content and few nutrients that contribute to dietary imbalances(Reference Maillot and Drewnowski25,Reference Cappelli, Pike and Riggs26) and are commonly consumed by children(Reference Reedy and Krebs-Smith27). Energy consumed from SFAS has increased in frequency in the past few decades and encompasses approximately 27 % of total daily energy intake among children(Reference Piernas and Popkin28,Reference Blaine, Fisher and Taveras29) . Preschool-aged children who consume snacks larger in size and higher in energy density tend to have poorer overall diet quality and higher daily intake of SFAS(Reference Kachurak, Bailey and Davey30). Children and adolescents with overweight or obesity are more likely to consume more of their total daily energy from snacks(Reference Kachurak, Davey and Bailey31), consume more SFAS from snacks and consume more energy during each snacking occasion compared with those that are normal weight(Reference Tripicchio, Kachurak and Davey32). These studies indicate that increased intake of foods often consumed by children and typically high in SFAS may increase daily energy intake and risk of overweight and obesity in childhood, even for those consuming two or more snacks per day(Reference Fisher, Davey and Kachurak33). Mid-childhood is a crucial stage for understanding contributors to SFAS consumption. When children transition into childhood and adolescence, they become more autonomous in their eating behaviours and are more likely to increase consumption of SFAS and foods eaten away from home(Reference Lytle, Seifert and Greenstein34,Reference Nielsen, Siega-Riz and Popkin35) . Because children become more independent during adolescence, it is important to understand contributors to eating habits in the preadolescent stage as dietary patterns established in childhood are typically carried into adulthood(Reference Berkey, Rockett and Field36–Reference Miller, Kolonel and Bernstein38) and can have long-term effects on health.
Markers of EH, such as housing insecurity and food insecurity, may link to poorer quality diet in childhood(Reference Liu, Shelton and Eldred-Skemp39). However, studies have not uniformly found significant associations between EH and children’s consumption of high SFAS foods. A systematic review examining correlates of fruit and vegetable consumption among children found that a majority of studies did not find significant associations between family level socioeconomic status, indicators of EH and fruit/vegetable intake(Reference Pearson, Biddle and Gorely40). On the other hand, food insecurity has been linked to higher BMI and lower overall diet quality in early(Reference Jansen, Kasper and Lumeng3) and middle childhood(Reference Fram, Ritchie and Rosen4) and to increased consumption of sugar-sweetened beverages in early childhood(Reference King5). Higher poverty levels have been negatively associated with child consumption of fruit but not vegetables(Reference Lorson, Melgar-Quinonez and Taylor6). Lower socioeconomic status measured as a composite of education, income and employment has been associated with higher intake of sugar-sweetened beverages among Canadian youth(Reference Pabayo, Spence and Cutumisu7). Lower primary caregiver education has been associated with larger serving sizes provided by mothers to children(Reference Rigal, Champel and Hébel8) and higher intake of sugar-sweetened beverages and energy-dense, nutrient-poor snacks among Australian(Reference Grimes, Riddell and Campbell9) and American youth(Reference Larson, Story and Eisenberg10). The inconsistent findings regarding EH and child diet may be due also to limitations in measuring hardship as a single indicator (i.e., poverty level, food insecurity) at a single point in time. Low-income families often face a multitude of economic stressors that may affect dietary outcomes. Given these discrepant findings, it is important to better understand how exposure to multiple elements of EH may increase child intake of high SFAS foods. Risk of adverse health consequences increases with aggregated stress exposure(Reference Hernandez19,Reference Dong, Anda and Felitti20,Reference Suglia, Duarte and Chambers41) . Those living in resource-constrained environments often experience multiple economic stressors simultaneously. Targeting only individual risk factors such as food insecurity or housing insecurity may miss the cumulative effect of other co-occurring economic stressors that may continue to impact parenting stress and child consumption of high SFAS foods. Assessing the aggregate of EH experienced over time allows us to have a better understanding of the cumulative effect on parents, and more holistically address parenting needs.
Multiple forms of EH including unmet material needs, job instability, housing instability and unequal access to services such as medical care are all forms of economic strain(Reference Peters and Massey42–Reference Neppl, Jeon and Schofield45) that can vary from family to family and increase family stress. However, such hardships are not captured by education, income levels or poverty thresholds. Families living above the federal poverty line often experience limitations in access to these essential material items(Reference Boushey, Brocht and Gundersen46,Reference Gershoff, Aber and Raver47) . Furthermore, most studies on child diet measure EH at one point in time(Reference Mazarello Paes, Hesketh and O’Malley48), rather than accounting for fluctuations in the effects of multiple EH over time. One study found an association between greater family stress, inclusive of EH, when children were 3 years old and lower fruit and vegetable consumption at age 5 years, but associations with sugary snacks were not significant(Reference Webb, Zimmer-Gembeck and Scuffham11), and EH was measured at a single point in time. Such research suggests that there may be a longitudinal effect of early economic stress on subsequent child dietary patterns(Reference Duncan, Yeung and Brooks-Gunn49,Reference Wells, Evans and Beavis50) . Focusing solely on family income at only one point in time may limit our understanding of how EH may affect SFAS consumption. This research yielding mixed results on the associations between markers of single-item indicators of EH (e.g., poverty, food insecurity and parent education) and child dietary patterns suggests the need for a more comprehensive understanding of the role of EH(Reference Boushey, Brocht and Gundersen46,Reference Gershoff, Aber and Raver47) . The present study first hypothesises that EH across early to middle childhood (aged 1–9 years) – operationalised as experiencing economic deprivation in relation to food security, housing stability, access to medical care and ability to pay bills and utilities – will associate with more frequent intake of high SFAS foods.
Parenting stress and child diet
As noted earlier, the link between EH and child intake of high SFAS foods may also not be direct but may instead become established through parenting behaviours or practices, such as parenting stress. Parenting stress refers to challenges and feelings of burden related to the demands of parenthood(Reference Deater-Deckard51,Reference Abidin52) . Experiences with multiple forms of EH (e.g., unmet material needs, housing instability) can increase parenting stress(Reference Neppl, Senia and Donnellan53,Reference Knowles, Rabinowich and De Cuba54) , negatively affect parent emotional and behavioural health(Reference Knowles, Rabinowich and De Cuba54) and increase tendencies for harsh parenting(Reference Neppl, Senia and Donnellan53), particularly when parents have limited personal and social resources(Reference Conger, Wallace and Sun14). In early and mid-childhood, a range of parenting practices can impact diet and child weight development, including food selection, feeding practices and the modelling of eating behaviours(Reference Lampard, Franckle and Davison55,Reference Birch, Savage and Ventura56) . Stress from EH can lead to maladaptive coping behaviours and reduce a parent’s ability to meet the emotional and physical needs of children(Reference Murry, Butler-Barnes and Mayo-Gamble44) during critical stages of development in early and mid-childhood. This may extend to food parenting. Parents experiencing high levels of stress may lack the emotional energy and sense of mastery(Reference Murry, Butler-Barnes and Mayo-Gamble44) to plan and prepare healthy meals. Parenting stress may also influence a parent’s approach to feeding children. For example, the inability to afford adequate food for one’s family is a stressful experience, may affect parent emotional states and compromise parenting practices and decision-making around feeding practices(Reference Bronte-Tinkew, Zaslow and Capps57). Further, the effects of parenting stress on children may lead to impairments in the development of self-regulation and executive functioning(Reference Deater-Deckard and Panneton58,Reference Zajicek-Farber, Mayer and Daughtery59) that have been linked to eating behaviours. However little is known about how the timing and duration of EH during early and mid-childhood can subsequently affect parenting stress, and how these stressors may shape parenting practices that affect child diet. Therefore, prevention efforts should begin in the preadolescent stage. It is necessary to expand the current literature on parenting stress to account for how EH may increase risk for parenting stress and whether these effects persist over time to affect diet when children are 9 years old, before they reach adolescence.
Associations between parenting stress and child consumption of fruits and vegetables have been equivocal(Reference Webb, Zimmer-Gembeck and Scuffham11,Reference Baskind, Taveras and Gerber60,Reference O’Connor, Maher and Belcher61) . Some studies have found a positive association between parenting stress and consumption of sugary foods and beverages(Reference Suglia, Duarte and Chambers21,Reference Nanjappa, Hector and Marcenes62) while others have not(Reference Shonkoff, Boyce and McEwen2,Reference Webb, Zimmer-Gembeck and Scuffham11,Reference Baskind, Taveras and Gerber60,Reference O’Connor, Maher and Belcher61) . Qualitative work indicates that feelings of stress among parents affect the eating environment in low-income households. Feeling stressed and overwhelmed led parents to feel more difficulty in setting and keeping limits on their child’s intake of sweets(Reference Norman, Berlin and Sundblom63) and to increase purchasing and consumption of high-energy foods like ice cream and fast food even if a meal was already prepared at home(Reference Parks, Kumanyika and Moore64). Parenting stress has been associated with higher child consumption of fast food(Reference Baskind, Taveras and Gerber60), higher BMI(Reference Shankardass, McConnell and Jerrett1,Reference Baskind, Taveras and Gerber60,Reference Tate, Wood and Liao65) , greater decline in overall dietary quality over 1 year(Reference O’Connor, Huh and Schembre66), more parental pressure to eat, having fewer homemade foods(Reference Berge, Tate and Trofholz67), higher levels of child emotional overeating(Reference Mandelbaum, Moore and Silveira68) and poorer overall child health(Reference Larkin and Otis69). Although EH may directly affect child diet quality(Reference Reedy and Krebs-Smith27), there are likely other processes by which EH can affect child diet, such as parenting stress. No studies were identified that examine EH as an antecedent in the association between higher parenting stress and poorer child diet quality. It is important to understand how levels of EH across childhood may have sustained effects on later parenting stress and subsequent child consumption of SFAS. As such, this study hypothesises that the links between EH and child consumption of high SFAS foods may not be direct, rather, that increases in EH across early to middle childhood will be associated with higher levels of parenting stress, which will in turn associate with more frequent consumption of SFAS foods when children are 9 years old.
In the present study, we address important gaps in the literature by examining changes in individual family experiences with EH over the course of early to mid-child development, whether changes in EH associate with child consumption of high SFAS foods, and whether this association is mediated by parent stress. Several individual level characteristics may affect child consumption of high SFAS foods in addition to EH and parenting stress. As such, we account for factors known to associate with child consumption of high SFAS foods, including maternal age, race and ethnicity, education level, maternal BMI, and child sex and BMI z-score(Reference Kachurak, Davey and Bailey31,Reference Anderson, Lemeshow and Whitaker70) . Understanding the potential links between the magnitude and duration of exposure to EH on subsequent child consumption of foods high in SFAS through parenting stress may help improve child outcomes by shedding light on whether cumulative EH and parenting stress should be targets of intervention.
Methods
Procedure and sample
Data were drawn from the Fragile Families and Child Wellbeing (FFCW) study, a longitudinal study of approximately 4898 new mothers in twenty randomly selected cities with a population density of 200 000 or more(Reference Reichman, Teitler and Garfinkel71). The FFCW is representative of unmarried births; about three-quarters of the sample were born to unmarried parents(Reference Reichman, Teitler and Garfinkel71). There is a higher proportion of poor and racial/ethnic minority families in unmarried households, and the FFCW sample is referred to as ‘high risk’ because of the multiple risk factors associated with non-marital childbearing(Reference Reichman, Teitler and Garfinkel71). Mothers were recruited from hospitals from 1998 to 2000, where baseline data were collected at the child’s birth, and families participated in follow-up studies when children were 1 (T1), 3 (T3), 5 (T5) and 9 (T9) years old using a combination of phone interviews and in-home assessments. Participants were excluded at the start of the study if parents were planning for adoption, the child or father was deceased prior to the interview, parents did not speak English or Spanish or were too ill to complete the interview. Additional details on the study design and sampling procedures of the original FFCW study can be found elsewhere(Reference Reichman, Teitler and Garfinkel71). For the present study, 1052 cases were excluded, resulting in a sample of 3846 families based on the following criteria: teen mother under 18 at baseline (due to likelihood of different living circumstances and correlations of age with income and parenting stress; n 140), child developmental disability that may impair growth (n 812) and non-singleton birth (n 95). Additional five cases were excluded for being extreme outliers on measures of EH based on box plot results.
Measures
Economic hardship trajectory
EH was assessed at waves T1–T9. Items were derived from the Survey on Income and Program Participation section on basic needs(72). Mothers responded to eight dichotomous items indicating the presence or absence of the following EH in the past 12 months: (1) received free food/meals, (2) unable to pay full amount of rent/mortgage, (3) evicted for not paying rent/mortgage, (4) could not pay full gas/oil/electric bill, (5) borrowed money from family/friends to pay bills, (6) moved in with people because of financial problems, (7) stayed in a place not meant for regular housing and (8) could not afford needed medical care for anyone in house. Based on prior research(Reference Shelleby73–Reference Zilanawala and Pilkauskas75), an index was developed by summing scores across all eight items for each time point (T1, T3, T5 and T9), with a possible range of 0–8; higher scores represent more EH.
Parenting stress
Parenting stress was assessed at T9 using a series of four questions derived from the Parenting Stress Inventory(Reference Abidin52). Mothers were asked to respond to the following items on a 4-point Likert scale from 1 (strongly agree) to 4 (strongly disagree): (1) being a parent is harder than I thought it would be, (2) I feel trapped by my responsibilities as a parent, (3) I find that taking care of my child(ren) is much more work than pleasure and (4) I often feel tired, worn out or exhausted from raising a family. Items were reverse scored and averaged to account for missing responses; higher scores represent more parenting stress (T9 α = 0·70).
Child consumption of foods high in saturated fats and added sugars
Children’s consumption of high SFAS foods was assessed using a FFQ format(Reference Olukotun and Seal76) and includes food items that are the most common sources of added sugar and saturated fat (e.g., desserts, candy, sugar-sweetened beverages and savoury snacks/chips)(Reference Reedy and Krebs-Smith27,Reference Huth, Fulgoni and Keast77–Reference Johnson, Bell and Zarnowiecki80) that have been used in prior studies with similar samples(Reference King5,Reference Suglia, Duarte and Chambers21,Reference Jackson and Vaughn81,Reference Suglia, Solnick and Hemenway82) . Based on study designed measures at T9, mothers were asked the number of servings of each of the following items that their child consumes on a typical day on a scale of 0 (never) to 5 (five or more): candy or sweets, snack foods or chips and soda. In accordance with prior research, the measure of the frequency of high SFAS foods was constructed using a standardised index(Reference Jackson and Vaughn81), in which each dietary item was included in the analysis as a latent construct of child consumption of high SFAS foods, with higher values representing more frequent consumption of high SFAS foods.
Control variables
Several mother and child characteristics were included as control variables. Maternal characteristics include mother’s age at the time of the child’s birth (baseline), maternal education at T1 (1 = <high school, 2 = high school equivalent, 3 = some college and 4 = college degree) and maternal BMI at T9 based on self-report of height and weight. Maternal race/ethnicity (baseline interview report) was included to compare those that are Hispanic and non-Hispanic Black to those that are non-Hispanic White or of an ‘other’ (Asian/Pacific Islander, American Indian/Eskimo/Aleut and other not specified) race/ethnicity. Child sex was collected via baseline interview report. Child height and weight were measured by trained researchers at T9, and BMI z-scores were calculated based on Centers for Disease Control and Prevention growth charts for age and sex(Reference Kuczmarski, Ogden and Guo83).
Data analysis
Missing data analysis
Missing data were present in fewer than 5 % of cases for all variables except for EH (7 % missing) and child diet items (26 % missing). Bivariate analyses were conducted to determine the extent to which missing data on child diet variables were missing at random. Most missing data occurred because parents did not participate in the 9-year wave of data collection. Missing data on diet items did not vary by child sex (P = 0·09) or maternal BMI (P = 0·28). Missing data on child diet was significantly more likely among mothers that were slightly older on average (M = 26·07, sd = 6·00) compared with parents who were not missing data (M = 25·32, sd = 5·86; t = –3·62, P < 0·001), among those with less than a high school education (34·4 %), compared with college graduates (11·7 %; χ 2 = 14·04, P = 0·003), and among those who were African American (40·9 %) or Hispanic (33·8 %) compared with those who were White (19·9 %) or of an ‘other’ race/ethnicity (5·4 %; χ 2 = 33·44, P < 0·001). Missing data analysis suggests that data are missing at random but not missing completely at random. Mplus uses maximum likelihood estimation as default to handle data that are missing at random by using all available data(Reference Little and Rubin84).
Main analysis
To test whether change in EH from T1 to T9 was associated with the frequency of child consumption of high SFAS foods (hypothesis 1), MPLUS V.8 was used to conduct a latent growth curve modelling analysis, a framework of structural equation modelling(Reference Byrne85) to assess the longitudinal trajectory of change in EH from T1 through T9 (T1, T3, T5 and T9) using maximum likelihood estimation. Latent growth curve modelling intercept values reflect the mean starting level of EH, and slope values represent the change in each child’s exposure to EH from ages 1 through 9. Given the study aim to assess the association of change in EH over the early life course, slope values were centred at T1, T3 and T5 in separate models to assess hardship averages and trends at different stages of child development. To determine the best fitting model, we assessed whether trajectories of EH scores followed a linear or nonlinear/curvilinear pattern by testing linear and quadratic slopes. Next, structural equation modelling was used to test hypothesis 1 (direct association between EH and SFAS food consumption) and hypothesis 2 (parenting stress as a mediator of the EH-child high SFAS food consumption association). Observed factors for parent stress and a latent factor for frequency of child SFAS food consumption were included in models with EH growth curves to investigate trends over time for EH with random intercepts and random slopes for subjects.
Indirect effects can be present in the absence of total or direct effects(Reference Rucker, Preacher and Tormala86). Given the temporally distal nature of EH, particularly the average starting level (i.e., intercept) at T1–T5, and child SFAS food consumption outcomes at T9, a direct association between EH and SFAS consumption was not a requirement to proceed with mediation models(Reference Shrout and Bolger87). To estimate the significance of mediation effects, bootstrapping with 1000 samples and bias-corrected estimates were applied(Reference Shrout and Bolger87,Reference Preacher and Hayes88) . Model fit was assessed based on χ 2 goodness-of-fit indices, a comparative fit index (CFI) and Tucker-Lewis index (TLI) > 0·95, and root mean square error of approximation (RMSEA) < 0·08(Reference Hu and Bentler89). Models were adjusted for the following potential covariates: maternal age, maternal BMI, education, and race/ethnicity, child sex and child BMI z-score; only maternal education and race/ethnicity were retained as significant predictors of SFAS intake at T9.
Results
Sample characteristics and descriptive statistics
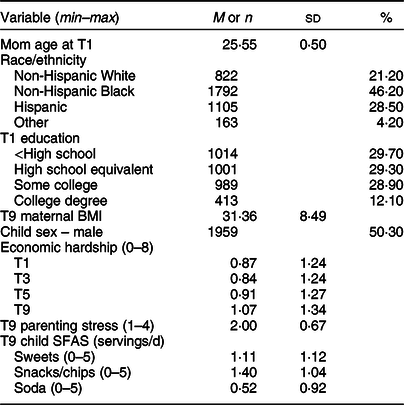
Primary caregivers in the final sample included mostly mothers (98 %) and will henceforth be referred to as ‘mothers’. At the time of their child’s birth, mothers were 26 years old, on average. Most were non-Hispanic Black (46·2 %), followed by Hispanic (28·5 %) and non-Hispanic White (21·2 %). Approximately 30 % of mothers had less than a high school education, 29 % reported having a high school degree or equivalent, 29 % had some college and 12 % reported having a college degree. Average EH scores were low and ranged from 0·87 to 1·07 from T1 to T9. At T9, mothers reported their child to have an average of 1·11 servings of sweets, 1·40 servings of snacks and 0·52 servings of soda each day. Parenting stress scores were 2·00, on average, at T9. See Table 1 for more details on sample characteristics and descriptive statistics.
Table 1. Sample characteristics and descriptive statistics (n 3846)
Latent growth curve modelling and structural equation modelling results
Economic hardship change from T1 to T9
Estimated and sample means of EH across each wave of data collection show a slight decline in average levels of hardship from T1 to T3, an upward trend in hardship from T3 to T5 and a steep increase from T5 to T9 (Fig. 1). The quadratic slope function was used for analysis based on estimated and sample means that show a curvilinear trend in EH from T1 to T9. The quadratic function was a good fit to the data (χ 2 = 2·62, df = 1, RMSEA = 0·02 (<0·001–0·05), CFI = 1·00, TLI = 1·00, Akaike Information Criterion (AIC): 39 331·71), similar to the linear model (χ 2 = 1·42, df = 2, RMSEA (90 % CI) < 0·001 (<0·001, 0·03), CFI = 1·00, TLI = 1·001, AIC: 30 902·82). The mean intercept (β = 0·98, se = 0·03, P < 0·001) and quadratic slope values (β = 0·15, se = 0·05, P < 0·001) were significant (Fig. 2).
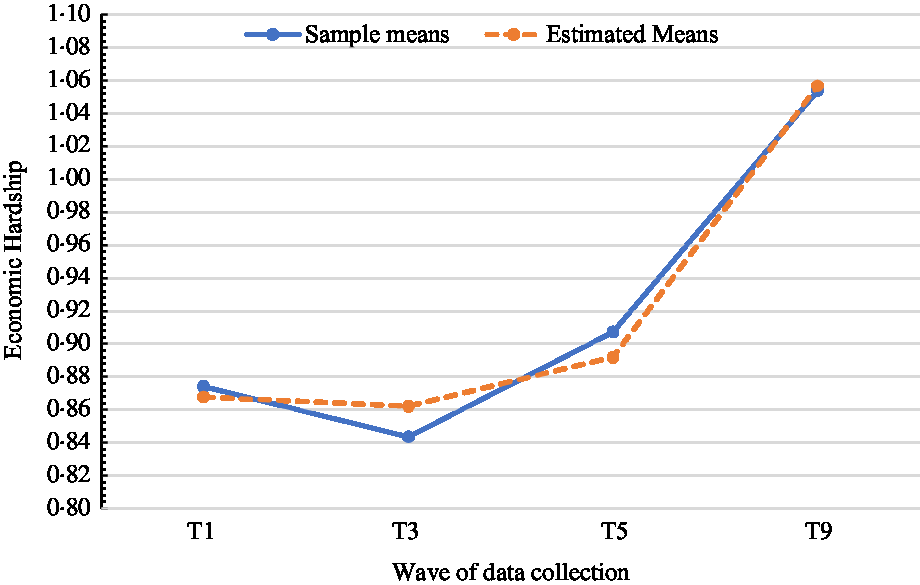
Fig. 1 Observed and estimated curves for T1–T9 economic hardship (EH) quadratic slope
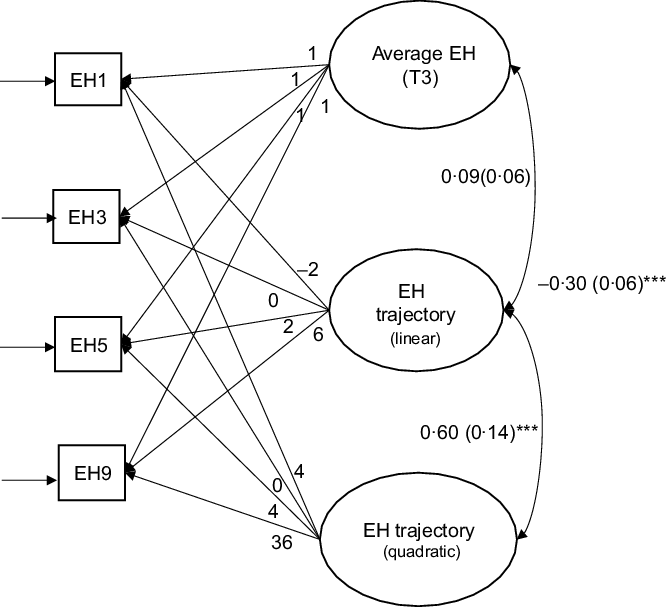
Fig. 2 Latent growth curve modelling for T1–T9 economic hardship (EH) quadratic growth curve, centred at T3. ***P < 0·001
Hypothesis 1: Economic hardship and saturated fats and added sugars
There were no direct associations between EH and frequency of child consumption of high SFAS foods. The average level of EH at T3 (intercept direct effect: β = –0·01, se = 0·03, P = 0·63) and T5 (intercept direct effect: β = –0·02, se = 0·03, P = 0·62) was not associated with the frequency of child consumption of high SFAS foods at T9. The change in the trajectory of EH from T1 to T9 was also not significantly associated with the frequency of child consumption of high SFAS foods at T9 when EH was centred at T3 (quadratic slope direct effect: β = 0·04, se = 0·06, P = 0·52) or T5 (quadratic slope direct effect: β = –0·06, se = 0·07, P = 0·42). Both models were a good fit to the data (T3: χ 2 = 94·50 (df = 16); CFI = 0·99, TLI = 0·96, RMSEA = 0·04 (90 % CI 0·03, 0·04); T5: χ 2 = 52·73 (df = 23); CFI = 0·99, TLI = 0·99, RMSEA = 0·02 (90 % CI 0·01, 0·03)). Models testing EH centred at T1 were not a fit to the data.
Hypothesis 2: Parenting stress mediation
Average economic hardship at T3 and T5. Higher levels of parenting stress significantly mediated the association between higher average starting levels of EH (T3: intercept indirect effect: β = 0·03, se = 0·01, P < 0·001; 95 % CI 0·02, 0·04; T5: intercept indirect effect: β = 0·03, se = 0·01, P < 0·001; 95 % CI 0·02, 0·05) and more frequent consumption of high SFAS foods at T9, net of controls. In other words, the average level of EH at both T3 (Fig. 3a) and T5 (Fig. 3b) was positively associated with higher levels of parenting stress at T9 (T3: β = 0·20, se = 0·03, P < 0·001; T5: β = 0·21, se = 0·04, P < 0·001) which was, in turn, associated with more frequent consumption of high SFAS foods at T9 (T3: β = 0·13, se = 0·03, P < 0·001; T5: β = 0·13, se = 0·03, P < 0·001). The structural equation modelling mediation models were a good fit to the data (T3: χ 2 = 99·77 (df = 19); CFI = 0·98, TLI = 0·95, RMSEA = 0·03 (90 % CI 0·03, 0·04); T5: χ 2 = 99·77 (df = 19); CFI = 0·98, TLI = 0·95, RMSEA = 0·03 (90 % CI 0·03, 0·04)).
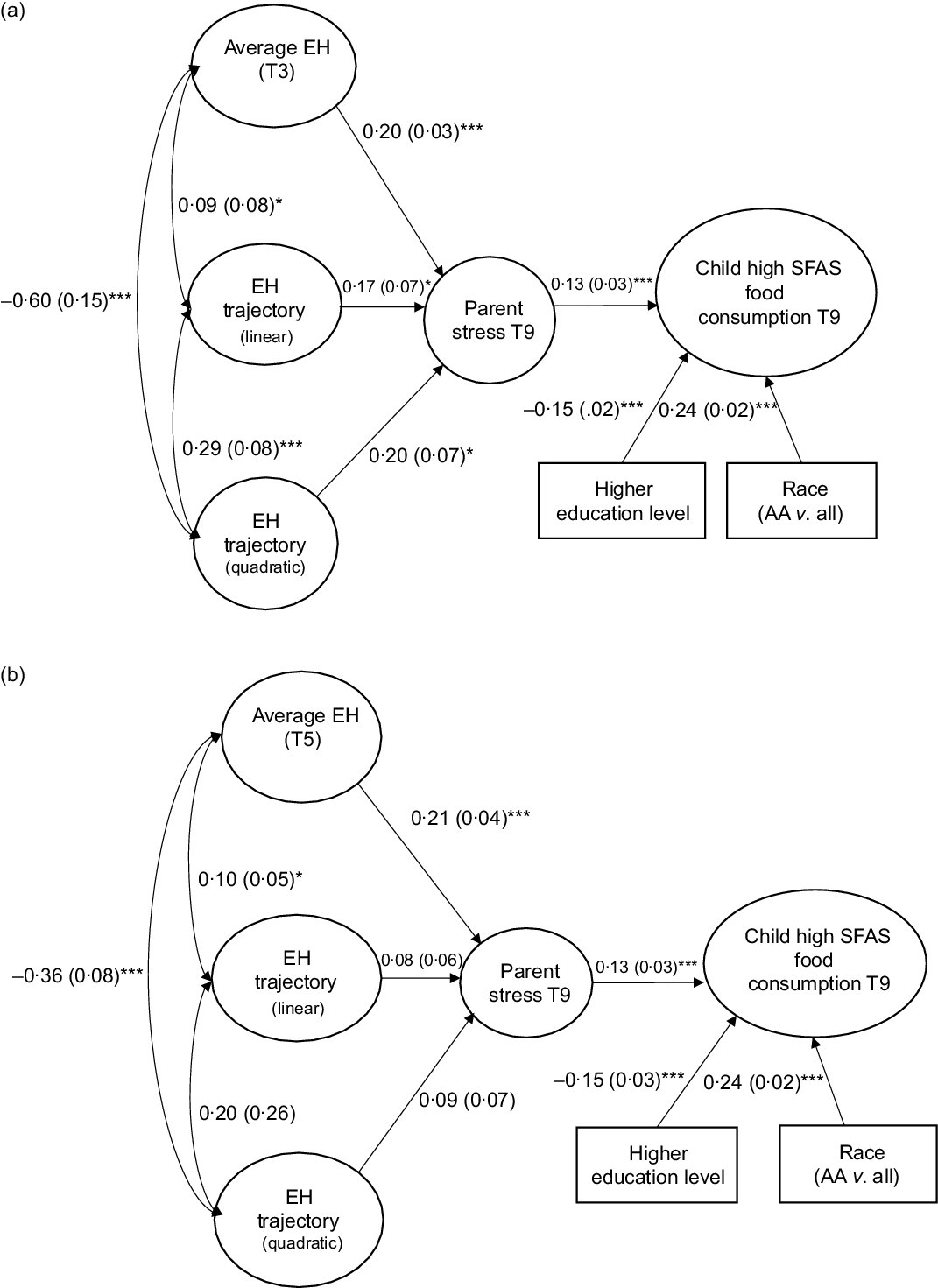
Fig. 3 Structural equation modeling (SEM) standardised estimates for T1–T9 economic hardship (EH) with parenting stress mediation. *P < 0·05, ***P < 0·001
Change in economic hardship from T1 to T9
When centred at T3, higher levels of parenting stress significantly mediated the association between change in hardship from T1 to T9 and more frequent consumption of high SFAS foods at T9 (slope indirect effect: β = 0·02, se = 0·01, P = 0·03; 95 % CI 0·01, 0·05), net of controls (Fig. 3a). The slope of EH from T1 to T9 was positively associated with higher levels of parenting stress at T9 (β = 0·20, se = 0·07, P = 0·007) which was, in turn, associated with more frequent SFAS food consumption at T9 (β = 0·13, se = 0·03, P < 0·001). When centred at T5, change in EH from T1 to T9 was not significantly associated with parenting stress or frequency of child consumption of high SFAS foods (quadratic slope: β = 0·09, se = 0·07, P = 0·21). See online supplementary material, Supplemental Table 1 for standardised parameter estimates of control covariates in each model.
Discussion
Study findings indicate that among a high-risk sample, there is significant variation in the average level of EH experienced among families. EH levels changed significantly from T1 to T9, such that there were significant increases in EH, on average, between the ages of 3 and 9 years. Contrary to our hypotheses, neither the average level of EH during early childhood (aged 3 and 5 years) nor the change in EH from ages 1 to 9 directly predicted more frequent consumption of high SFAS foods. However, parenting stress at T9 significantly mediated the association between average starting levels of EH as well as increasing levels of EH and more frequent child consumption of high SFAS foods at age 9. Collectively, these findings suggest that early and sustained exposure to EH may increase parenting stress, which in turn may increase risk of more frequent child consumption of high SFAS foods.
Prior studies have found direct associations between indicators of EH and child consumption of SFAS or diet quality(Reference Jansen, Kasper and Lumeng3,Reference Fram, Ritchie and Rosen4,Reference Lorson, Melgar-Quinonez and Taylor6,Reference Pabayo, Spence and Cutumisu7,Reference Webb, Zimmer-Gembeck and Scuffham11,Reference Lee, Andrew and Gebremariam12) . Current study findings indicate that EH is not directly associated with consumption of high SFAS foods(Reference Pearson, Biddle and Gorely40) but may operate through parenting stress. One explanation for differences in present study findings compared with prior research may be due to the focus on consumption of high SFAS foods rather than a specific focus on access to healthy foods. EH may be more likely to directly link to the consumption of fewer healthful foods, such as fruits and vegetables, given that healthful foods are commonly more costly, and the absence of economic resources is more likely to affect a family’s ability to purchase such items. This may in part explain why some studies found associations between indicators of EH and overall diet quality (e.g., total amount of energy content and nutrients consumed)(Reference Jansen, Kasper and Lumeng3,Reference Fram, Ritchie and Rosen4) , and other studies are equivocal in their findings when broken down by the type of food eaten (e.g., total amount of energy content and nutrients consumed)(Reference Pabayo, Spence and Cutumisu7,Reference Grimes, Riddell and Campbell9,Reference Larson, Story and Eisenberg10,Reference Pearson, Biddle and Gorely40) . Foods high in SFAS are often lower cost, easily accessible and are less likely to be affected by the amount of economic resources a family has.
EH experienced in early childhood operated through parenting stress to associate with the frequency of child consumption of high SFAS foods, indicating that consumption of SFAS may be affected by the degree of stress experienced by the parent. The association between parenting stress and more frequent child consumption of high SFAS foods is consistent with prior research that has found associations between similar concepts, such as higher parenting stress and higher fast food consumption(Reference Baskind, Taveras and Gerber60), poorer parent feeding practices that link to lower quality diet(Reference Berge, Tate and Trofholz67), higher levels of child emotional overeating(Reference Mandelbaum, Moore and Silveira68), better general family functioning and lower preschooler sugar consumption(Reference Nanjappa, Hector and Marcenes62). Further, studies have consistently linked parenting stress(Reference Shankardass, McConnell and Jerrett1,Reference Baskind, Taveras and Gerber60,Reference Tate, Wood and Liao65) or more stressful social circumstances (e.g., intimate partner violence, maternal depression and maternal substance use)(Reference Suglia, Duarte and Chambers21) with higher risk of childhood obesity, even after adjusting for parental weight(Reference Baskind, Taveras and Gerber60). However, study findings differ from previous research that has found no consistent link between higher levels of family stress and child consumption of snack foods(Reference Webb, Zimmer-Gembeck and Scuffham11) or added sugars(Reference O’Connor, Maher and Belcher61,Reference Shonkoff, Dunton and Chou90) . These prior studies measured EH as a single-item indicator at one point in time (i.e., family income, child recipient of free or reduced priced lunch)(Reference Webb, Zimmer-Gembeck and Scuffham11,Reference Shonkoff, Dunton and Chou90) , whereas this study uses a comprehensive measure that includes multiple elements of EH and importantly examines the longitudinal effects of such EH. Given trends in increasing levels of overconsumption of foods high in SFAS(Reference Reedy and Krebs-Smith27–Reference Blaine, Fisher and Taveras29,91) , results of the current study extend the results of prior research by providing important information about the role of early life EH in predicting parenting stress and more frequent child consumption of SFAS.
Strengths and limitations
Results of this study add to existing research in two important ways. First, a comprehensive measure of EH was used to assess cumulative risk over the early life course, a critical period of changes in food parenting and development of children’s dietary behaviours. This allowed for an examination of how multiple elements of EH and changes in a family’s experience with EH over time might associate with parenting stress and child consumption of high SFAS foods. The measure of EH used in this study provides an extensive view of a family’s experience with EH over the first 9 years of a child’s life. Second, this study adds to the literature by assessing how a potential pathway of parenting stress may play an important role in establishing an indirect association between EH and child consumption of SFAS foods, providing a potential target for interventions aiming to improve diet quality and reduce overconsumption in childhood.
There are also several limitations in this study. While the EH measure in this study is comprehensive, single-item indicators of EH that are more closely related to food and eating, such as food insecurity, may be more correlated with SFAS consumption. For example, with the EH measure, the proxy item to index degree of food insecurity in the family, received free food/meals was positively and significantly correlated with the US Household Food Security Survey Module raw scale scores(Reference Bickel, Nord and Price92) at T3 (r = 0·24, P < 0·001) and T5 (r = 0·28, P < 0·001). However, this proxy item was not significantly associated with SFAS consumption at any time point (T1 t = –0·004, P = 0·99, T3 t = 0·70, P = 0·48, T5 t = –0·14, P = 0·09, T9 t = 0·67, P = 0·49). Further, given that the FFCW represents ‘high-risk’ families (i.e., oversampled families with unmarried parents and racial and ethnic minorities), variability in EH may be more limited than in nationally representative samples, limiting the generalisability of findings and presenting limitations in the potential to detect differences in more widely varying levels of EH. This study assessed self-reported parent stress and SFAS food consumption cross-sectionally at a single point in time, not allowing for an assessment of temporal associations. Future research should examine how stress may fluctuate over time with changes in EH and include objective measures of stress in addition to parental perceptions to assess longitudinal effects of parenting stress on child SFAS consumption. Child consumption of high SFAS food was measured by parent report. Foods assessed in this study are key sources of SFAS intakes among young children but may not reflect the whole of SFAS consumption. Further, our SFAS measure focuses on frequency and does not capture energy contribution to diet. Given such, results may be subject to response bias in that parents may be more likely to under-report the frequency of consumption of less healthful foods. Future research should include established, validated measures of diet quality and include consumption of both healthful and unhealthful foods.
Twenty-six percent of the original sample was missing SFAS food consumption outcome data. Although the entire FFCW is a ‘high-risk’ sample, the analytic sample had higher levels of education and fewer participants identifying as Hispanic and non-Hispanic Black compared with non-Hispanic White. Because lower levels of education and racial and ethnic minority status have been associated with higher SFAS consumption(Reference Pabayo, Spence and Cutumisu7–Reference Grimes, Riddell and Campbell9), effects of EH on parenting stress and SFAS consumption may be stronger than present study results indicate. The total variance explained was small, indicating that there are other factors that may influence child consumption of high SFAS foods. Factors that may influence high SFAS food consumption are complex and can involve multiple interacting mechanisms. Indicators of EH that are more directly related to diet (e.g., neighbourhood level food access, food insecurity) and other factors that may affect parenting stress, such as parent mental health, were not tested in this study and may play an important role in understanding child SFAS consumption outcomes. Future research should account for the complexity of factors at individual, household and community levels that may influence overconsumption, including child temperament and behaviour, parent mental health, parenting styles, parent–child relationships and access to quality and affordable foods in the environment. Finally, although a strength of the study was its longitudinal design, we are still not able to infer causality from these data.
Conclusions
Findings provide new evidence that parenting stress may explain associations between influences of early EH on children’s later intake of unhealthy foods. The present study expands our understanding of the reach of family stress, and potential mechanisms by which EH and parenting stress can contribute to suboptimal health behaviours beginning in childhood. Results suggest it may be important to consider parenting stress in early intervention and prevention efforts given the potential lasting effects of early life EH on subsequent child consumption of SFAS foods. Given that parenting stress may be an important mechanism through which the impact of EH may affect child diet quality, addressing EH in early childhood and subsequent parental distress may be important elements for improving our understanding of how to reduce overconsumption of SFAS in subsequent years of child development. It is understandable that families experiencing EH and attendant stress may be inclined to turn to affordable foods high in SFAS as a rewarding treat for children(Reference Fielding-Singh93). Adverse challenges resulting from EH can be unavoidable. This study represents a first step in expanding beyond income-only indicators of hardship. In addition to the supports families may need to address specific forms of hardship (e.g., housing supports, food supports and medical care), results of this study, similar to other studies(Reference Hatem, Lee and Zhao94), suggest that screening for various multiple hardships may provide opportunities to determine when parents also need supports to cope with feelings of stress associated with the experience of parenting in the context of EH. Coping and resilience are major factors in shaping how stress under such circumstances is handled(Reference Sigman-Grant, Hayes and VanBrackle95). Given that a majority of children are resilient to the obesogenic environment, and are not overweight or obese(Reference Sigman-Grant, Hayes and VanBrackle95,Reference Ogden, Carroll and Kit96) , future research should examine the dynamics that protect children from unhealthy eating behaviours and obesity risk, particularly among lower-income families. This includes examining methods that can buffer the degree of stress felt from EH-related stress. This could include assessing therapeutic services to help parents cope with stress, providing resources for stress management and facilitating connections to opportunities for positive social support. Assessing how resources and referrals for financial supports and assisting families in accessing and applying for such supports (e.g., food assistance programmes, Temporary Assistance for Needy Families) may help buffer the effects of EH-related stress and are important directions for future research. Of note, our measure of stress in this study focused on parenting-related stress; it may also be important for future work to be able to articulate between different types of stress parents are experiencing in order to tailor recommendations. Future research should consider the main sources of stress imposed by EH so that methods may be better designed to be responsive to such hardships and determine if specific forms of EH, compared with cumulative EH, are more prominent sources of stress for parents and families. Understanding how EH may be a driver for parenting stress and understanding how parenting stress may then link to child diet provides important direction for interventions to target stress-coping mechanisms, as well as parenting strategies and skills to improve child food consumption(Reference Fisher, Serrano and Foster97).
Acknowledgements
Acknowledgements: The authors acknowledge the support, resources and advisement provided by the Vivian A. and James L. Curtis School of Social Work Research and Training Center of the University of Michigan School of Social Work and the advisement and reviews of Dr Jay Fagan. Financial support: This study was supported by The Robert Wood Johnson Foundation (Grant #74726). The views expressed here do not necessarily reflect the views of the Foundation. Research reported in this publication was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) of the National Institutes of Health under award numbers R01HD36916, R01HD39135 and R01HD40421, as well as a consortium of private foundations. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Conflict of interest: None. Authorship: B.R.S. and A.L.M. conceptualised the study, B.R.S., L.D. and M.C. analysed the data; B.R.S., S.S.D., D.C.H., J.O.F. and A.L.M. wrote the paper, Schuler and Miller had primary responsibility for final content. All authors read and approved the final manuscript. Ethics of human subject participation: This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all families provided informed consent before participating in the study. The Fragile Families and Child Wellbeing Study is a publicly available data set and institutional review board approval was not needed.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980020001366






