Early childhood malnutrition accompanied by rapid weight gain later in childhood increases the risk of chronic diet-related diseases in adolescence and in later adulthood(Reference Victora, Adair and Fall1). Worldwide, around 155 million children are stunted, and about 41 million children are overweight. All forms of malnutrition occur predominantly in low- and middle-income countries (LMIC). In particular, Asia contains 62 % of stunted children and 49 % of overweight children under-five(2). The co-existence of overnutrition and undernutrition can be defined as a double burden of malnutrition (DBMN) at population, household and individual levels and is a growing public health concern in LMIC(Reference Jehn and Brewis3–Reference Popkin, Corvalan and Grummer-Strawn5). Rapid economic and social development has led to changes in diet and activity patterns over the last two decades and the occurrence of DBMN(Reference Popkin6).
DBMN can occur at the individual level(Reference Popkin, Richards and Montiero7–Reference Urke, Mittelmark and Valdivia10). It arises in children who are concurrently stunted and overweight, known as ‘stunting-overweight,’ due to inadequate child feeding practices and morbidity during early childhood, and then who are subsequently overfed as a result of the rapid nutrition transitions occurring in LMIC(Reference Bates, Gjonça and Leone11,Reference Wells, Sawaya and Wibaek12) . This DBMN can be distinctly different from its stunted or overweight counterparts(Reference Popkin, Richards and Montiero7,Reference Fernald and Neufeld9,Reference Mamabolo, Alberts and Steyn13–Reference Varela-Silva, Dickinson and Wilson16) and can potentially become a significant public health issue. A handful of studies have documented DBMN at both the individual and population levels in LMIC, particularly in Southeast Asian countries(Reference Bates, Gjonça and Leone11,Reference Minh Do, Lissner and Ascher17) . Consequently, assessing its prevalence and understanding its determinants are essential for guiding policies and programmes(Reference Tzioumis and Adair18).
Over the last few decades, Thailand has reduced undernutrition, especially among young children and women. However, there have been increases in overweight and obesity across all age groups(Reference Chavasit, Kasemsup and Tontisirin19,Reference Aekplakorn and Mo-Suwan20) . According to the Multiple Indicator Cluster Survey (MICS) 2015–2016(21), the prevalence of stunting and wasting was 10·5 and 5·4 %, respectively, with the prevalence of overweight being approximately 10 %. On the other hand, DBMN at the individual child level has not been examined. Hawkes et al. (Reference Hawkes, Ruel and Salm22) have pointed out that addressing undernutrition can raise risks of overnutrition, especially in countries undergoing a rapid nutrition transition. Consequently, there is a need to consider how to effectively address malnutrition in all its forms in a more holistic way. Accordingly, this study’s objectives were, first, to determine the prevalence of concurrent stunting-overweight at the individual level and to identify the determinants of wasting, stunting, overweight and stunting-overweight among Thai children under-five. Second, given the significance of infant and young child feeding practices (IYCF) and the nutritional status of children aged 6–23 months, the associations between IYCF and all forms of malnutrition were explored. This study has notable implications for health professionals and policymakers concerned with the extent and/or emergence of all forms of malnutrition and implications for appropriate interventions.
Methods
Study data
This study is a secondary data analysis based on the Thailand MICS 2015–2016(21). The MICS was carried out under the Statistics Act by the National Statistical Office and UNICEF in collaboration with relevant Thai Ministries(21). The MICS was a national representative sample using multi-stage sampling and covering fourteen provinces in five geographical regions of the country (i.e. Bangkok, Central, North, Northeast and South). Urban and rural areas within each province were included. A specified number of census enumeration areas were selected systematically with probability proportional to size within each stratum(21). A systematic sample of twenty households was used in each enumeration area containing ten households with children under-five and ten households without children under-five. Out of 12 313 children under-five eligible for the survey, survey questionnaires were completed by mothers or caregivers for 12 250 children, giving a response rate of around 99·5 %. According to UNICEF guidelines, written informed consent was obtained at the time of primary data collection from all mothers or caregivers after explaining the study objectives and assurance of the confidentiality of their identity. In addition, it was made clear that if individuals did not want to participate in the survey, they would not be at any disadvantage. Details of the MICS have been described elsewhere(21).
Variables
Height-for-age and weight-for-height Z-scores below −2 sd and BMI-for-age Z-scores above 2 sd of the WHO Child Growth Standard were used to define stunting, wasting and overweight, respectively(23). A child who was simultaneously stunted and overweight was considered as having BMI-for-age Z-scores greater than +2 sd and height-for-age Z-scores below −2 sd and computed into a variable named stunting-overweight.
Variables on potential determinants included in the analysis were: child age (0–5, 6–11, 12–23, 24–35, 36–47 and 48–59 months), child sex (boys or girls), maternal education (no formal education, primary school, secondary school, or college and above), family wealth index tertiles (low, middle or high), number of children under-five in the family (1 or 2+), language of the household head (Thai or non-Thai) and place of residence (urban or rural).
This study further analysed the association between nutritional status in children aged 6–23 months and four IYCF indicators(24), namely, currently breast-feeding, minimum dietary diversity, minimum meal frequency and minimum acceptable diet among children aged 6–23 months (n 3251). Minimum dietary diversity was defined as receiving foods from at least four of seven food groups: (1) grains, roots and tubers, (2) legumes and nuts, (3) dairy products (infant formula, milk, yogurt and cheese), (4) flesh foods (meat, fish and liver/organ meats), (5) eggs, (6) vitamin-A-rich fruits and vegetables and (7) other fruits and vegetables(21,24) . Minimum meal frequency was defined as children who also received solid, semi-solid or soft foods two times or more daily for children aged 6–8 months and three times or more daily for children aged 9–23 months among currently breast-feeding children. For non-breast-feeding children, it was defined as receiving solid, semi-solid or soft foods or milk at least four times daily(21,24) . The minimum acceptable diet was defined as receiving the minimum dietary diversity and the minimum meal frequency for breastfed children. For non-breastfed children, it further required at least two milk feedings and minimum dietary diversity being achieved without counting milk fed(21,24) .
Statistical analyses
All analyses were performed with weighting factors for children from the data set using SAS version 9.4 (SAS Institute). The weighted prevalence of wasting, stunting, overweight and stunting-overweight was calculated. The χ 2 test was used to test differences in the distribution of malnutrition variables according to sociodemographic factors at a significance level of P < 0·05. The prevalence ratio with a 95 % CI was determined by a Poisson regression with a robust estimation of the variance using PROC GENMOD. The justification for using the Poisson model, instead of the logistic regression model, was due to the study (nutritional status of children) and the easier interpretation of prevalence ratios(Reference Zocchetti, Consonni and Bertazzi25). The simple and multiple Poisson regression modelling approaches produced crude and adjusted associations between each of the malnutrition variables and selected characteristics.
Results
The weighted prevalence of wasting, stunting and overweight was 5·3, 10·5 and 10·1 %, respectively (Table 1). When stunting and overweight estimates were amended to exclude stunted-overweight children, the prevalence became slightly lower: stunting 8·9 %, overweight 8·5 % and stunting-overweight 1·6 % (data not shown).
Table 1 Distribution of wasting, stunting, overweight and stunting-overweight according to sociodemographic factors among children aged 0–59 months

All values are presented as unweighted number and weighted percentages.
Table 1 indicates that the prevalence for wasting and stunting was higher among those from a low wealth index tertile, households headed by a non-Thai household head and rural residence (P < 0·05). In terms of age, there was a higher prevalence of wasting for children under 6 months and a higher prevalence of stunting among children aged 24–35 months. Male children and households with more than one child under-five were also associated with stunting (P < 0·001). Regarding overweight, there was a higher prevalence among children aged 24–59 months, male children, households in middle or rich wealth tertiles, households having only one child under-five and urban settings. For stunting-overweight, a higher prevalence was observed among the age group 24–47 months, male children, households where mothers had a secondary education, households in the middle wealth tertile, households having only one child under-five, households where the household head was non-Thai, and in urban areas.
Table 2 presents the adjusted prevalence ratio (APR) with a 95 % CI of malnutrition by sociodemographic factors. Older children and those living in urban areas were less likely to be wasted, while those from low or middle wealth index tertiles were more likely to be wasted. For stunting, children in the age group of 48–59 months and those in households having only one child under-five were less likely to be stunted, while male children, those in households with a low wealth tertile and those in households headed by a non-Thai head were more likely to be stunted. On the other hand, older age, male children and those living in households with only one child under-five were more likely to be overweight compared with their counterparts. Children in the low wealth tertile were more likely to be overweight than those in the high wealth tertile. Also, children in the age range between 24 and 47 months, male children, children with mothers who had secondary education, those from a household with a non-Thai household head, those from a one-child household and those from urban areas were more likely to be stunted-overweight compared with their counterparts.
Table 2 Adjusted prevalence ratios (PR) and 95 % CI of determinants of wasting, stunting, overweight and stunting-overweight among children aged 0–59 months
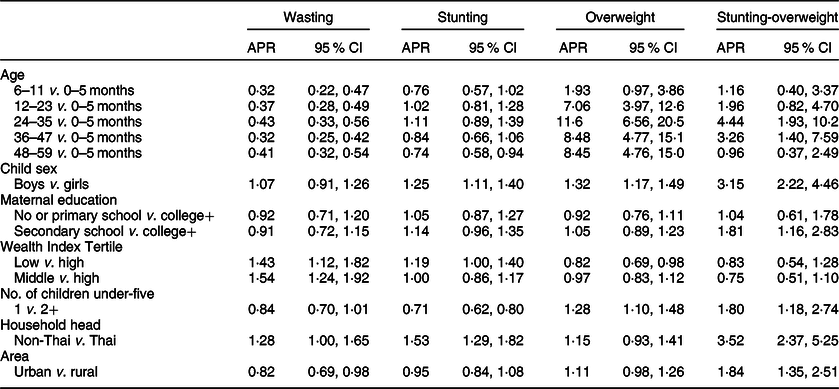
All variables listed in the table were entered to estimate adjusted OR.
Table 3 indicates the prevalence of four young child feeding practice indicators and the crude and APR of malnutrition among children aged 6–23 months. The proportion of children currently breastfed was 32·2 %, and those receiving the minimum meal frequency, minimum dietary diversity and minimum acceptable diet were 82·1, 77·1 and 55·5 %, respectively. The associations between the IYCF indicators and the malnutrition variables were performed before and after adjustment for child’s sex, child’s age, maternal education, wealth index, number of children, the language of household head and the place of residence. While the minimum dietary diversity and minimum acceptable diet did not show significant associations with wasting, currently breast-feeding and minimum meal frequency were associated with wasting in the bivariate and multivariate models (APR 1·82 (95 % CI 1·26, 2·62) and APR 0·37 (95 % CI 0·26, 0·53), respectively). For overweight, an inverse association was found for currently breast-feeding in the bivariate and multivariate models (crude prevalence ratio 0·42 (95 % CI 0·30, 0·60) and APR 0·55 (95 % CI 0·38–0·79)). While a significant association of the minimum meal frequency in the bivariate model (crude prevalence ratio 1·69 (95 % CI 1·12, 2·56)) disappeared after adjustment (APR 1·36 (95 % CI 0·90, 2·07)), the minimum dietary diversity was not significant in the bivariate model (crude prevalence ratio 1·10 (95 % CI 0·81, 1·50)] but appeared significant in the multivariate model (APR 0·70 (95 % CI 0·51, 0·97)). None of the IYCF indicators was significantly associated with stunting. For stunting-overweight, although the minimum dietary diversity was found significant in bivariate analyses, the significant association disappeared in the multivariate models.
Table 3 Association between young child feeding practices and wasting, stunting, overweight and stunting-overweight among children aged 6–23 months
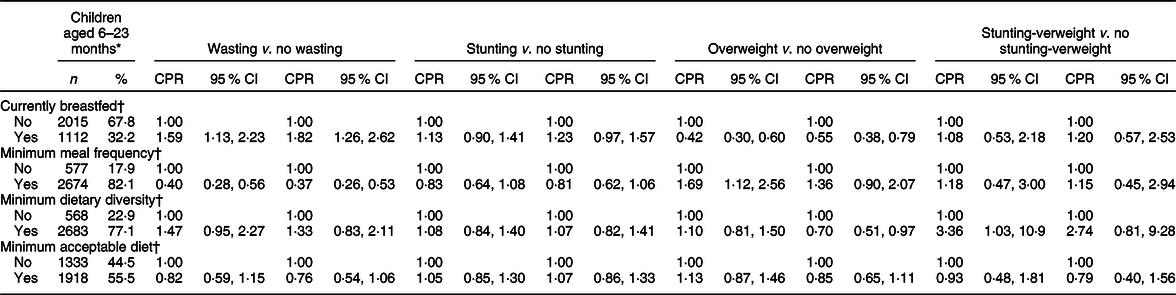
CPR, crude prevalence ratios; APR, adjusted prevalence ratio.
* The values are presented as unweighted number and weighted percentages.
† The feeding practice variables were adjusted for child sex (boys or girls), child age (6–11 or 12–23 months), maternal education (no/primary school, secondary or college/higher), wealth index (low, middle or high), number of children under-five (1 or 2+), language of household head (non-Thai or Thai) and area (rural or urban).
Discussion
Our study estimated the prevalence of stunting-overweight, an indicator of the individual level DBMN, to be 1·6 %. The prevalence of stunting-overweight in Thailand is seen to be in the low range among LMIC (0·3–11·7 %)(Reference Atsu, Guure and Laar8,Reference Bates, Gjonça and Leone11,Reference Severi and Moratorio26) . Compared with other South and Southeast Asian countries, Thailand’s prevalence of stunting-overweight is lower than that of Bhutan (5·4 % in 2010) and Pakistan (2·3 % in 2012–2013) but higher than that of Lao PDR (1·3 % in 2011–2012), Maldives (1·2 % in 2009), India (1·0 % in 2015), Bangladesh (0·7 % in 2011) and Nepal (0·7 % in 2011)(Reference Bates, Gjonça and Leone11). A few studies in Southeast Asia have shown a high prevalence of stunting-overweight, including those covering Indonesian children aged 2–4·9 years using nationally representative survey data (7·2 %)(Reference Rachmi, Agho and Li27) and Vietnamese cohort children aged 5·5–6·5 years (2·7 %)(Reference Minh Do, Lissner and Ascher17). Wells et al. (Reference Wells, Sawaya and Wibaek12) showed that children in LMIC who were stunted in early childhood and subsequently had rapid weight gain became overweight/obese in later childhood.
In terms of socio-economic status indicators, wealth index showed inverse or positive association with stunting and overweight, respectively. Yet, despite no statistically significant association in multivariate analysis, higher rates of stunting-overweight were found in children in the middle wealth group. For maternal education, there was no statistically significant association with a single form of malnutrition. However, in the multivariate analysis, a statistically significant association was found indicating an increased likelihood of stunting-overweight in children with mothers who had secondary education. Similar results have been found in Ghana, where children from the fourth wealth index quintile had a higher prevalence of stunting-overweight compared with the poorest wealth index quintile(Reference Atsu, Guure and Laar8). In the same study in Ghana, there was no significant association with maternal education(Reference Atsu, Guure and Laar8). However, a study in children aged 24–59 months in Cameroon showed that low-income families and a low maternal educational level are independent risk factors for a child to be stunted-overweight(Reference Said-Mohamed, Allirot and Sobgui28). Another study in Indonesian children aged 2·0–4·9 years showed no significant association with either wealth status or maternal education(Reference Rachmi, Agho and Li27). In terms of child sex, males also had higher prevalence of stunting, overweight and stunting-overweight compared with females. Differences in biological make-up, caregiving and gender preferences may potentially explain these differences(Reference Fuse29). According to a study in Brazil, similar results were found such that male children were found to be associated with the DBMN(Reference Gubert, Spaniol and Segall-Corrêa30). However, other studies have shown no statistically significant differences among the different sexes(Reference Atsu, Guure and Laar8,Reference Rachmi, Agho and Li27,Reference Said-Mohamed, Allirot and Sobgui28) . Our study also found that households with only one child under-five had a higher prevalence of overweight and stunting-overweight. Other studies have also shown that overweight was higher in families with only one child(Reference Hong, Sriburapapirom and Thamma-aphiphol31,Reference Sarki, Robertson and Parlesak32) .
In line with other studies, our study showed that while undernutrition rates were higher in rural areas, overweight and stunting-overweight were higher in urban areas. The high prevalence of stunting-overweight in urban areas may be explained by our recent study showing a persistently high stunting rate and a rising obesity rate among the urban poor over the last decade(Reference Hong, Winichagoon and Khang33). This finding may indicate that poor urban children who were stunted in early childhood may have had poor quality diets due to economic difficulties associated with parents/caregivers not being able to provide healthy food choices. We also found that households headed by a non-Thai speaker had a higher prevalence of wasting, stunting and also stunting-overweight. Children from such households mainly belong to low- or middle-wealth families and may be more likely to consume energy-dense foods, instead of nutrient-rich foods, due to high costs(Reference Popkin, Linda and Ng34). Consequently, future interventions and programmes should focus attention to double-duty actions to reduce the burdens of undernutrition and overnutrition among urban poor children and migrant children. These actions should be based on an accurate understanding of conditions affecting access to and the availability of healthy foods among these populations in Thailand.
Interestingly, the prevalence of wasting among those under 6 months of age was as high as 11·4 %, which is considered a serious problem by global criteria. Further studies are warranted to identify what contributes to this high prevalence during early infancy. On the other hand, the highest rates of stunting, overweight and stunting-overweight were found in children aged 24–35 months. It may be related to inappropriate IYCF practices during the first 2 years of life. We examined the cross-sectional association between malnutrition and IYCF practice before and after adjusting for confounders among children aged 6–23 months. Current breast-feeding and minimum meal frequency are associated with a higher likelihood of wasting. The positive association of current breast-feeding, different from a study in Pakistan showing no association(Reference Syeda, Wilson and Maheshwari35), warrants further study due to the fact that weight change is greatly influenced by illness and other environmental factors not explored by this study. On the other hand, current breast-feeding and minimum dietary diversity are associated with lower odds of being overweight. The inverse association of current breast-feeding with being overweight may be supported by our previous study of Thai children showing that longer breast-feeding duration decreased weight gain or overweight risk in children at 24 months of age(Reference Hong, Mongkolchati and Pimpak36).
Meanwhile, the significance of associations in bivariate models changed after controlling for covariates. In non-adjusted models, the significant association between minimum meal frequency and overweight in bivariate model disappeared in the multivariate model, while there was no significant association between minimum dietary diversity and overweight in the bivariate model but the association became significant in the multivariate model. It can be taken account for confounding effect of socio-demographic indicators on the associations between the IYCF indicators and malnutrition. For example, children aged 12–23 months are less likely to be currently breastfed and more likely to meet minimum meal frequency, dietary diversity and dietary diversity, compared with the counterparts (P < 0·001, data not shown). Children with mothers with higher education are less likely to be currently breastfed and more likely to meet minimum meal frequency and minimum acceptable diet (P < 0·01, data not shown), while minimum dietary diversity was not associated with maternal education level. Those residing in urban areas are more likely to meet minimum frequency meals, dietary diversity and acceptable diet (P < 0·05, data not shown), while they are not associated with being currently breastfed. Meanwhile, although the high prevalence ratio in the bivariate model (crude prevalence ratio = 3·36) showed the possibility of an important effect of adequate dietary diversity on stunting-overweight, the wide CI can probably be explained by the small cell size. Further research is needed to examine the natural history of individual DBMN across ages and the impact of appropriate IYCF practice using a prospective longitudinal sample of children.
Limitations of the present study should be acknowledged. First, this study was a cross-sectional design; hence, it cannot explain the causal relationships between child malnutrition and risk factors, including IYCF practices. Consequently, we cannot draw a conclusion with respect to the causes of stunting-overweight or single types of undernutrition and overnutrition. Despite these limitations, the MICS data produce a nationally representative estimate of stunting-overweight among Thai children using appropriate weighting techniques.
This study provides insights into DBMN at the individual level, for which information is still sparse. It allows us to make informed policy decisions to engage in double-duty actions to reduce the burdens of undernutrition and overnutrition among Thai children. These actions can help to ensure that current and future interventions, policies and programmes aimed at one form of malnutrition do not unintentionally increase another(37). Currently, the universal Child Support Grant scheme in Thailand provides a monthly allowance of 600 Baht (approximately 20 USD) for children up to the age of three living in poor households. This scheme was started in 2016(38) to promote child development. However, such a scheme may bring unexpected consequences, such as contributing to the burden of being overweight if caregivers do not have appropriate knowledge on the importance of quality complementary feeding practices and proper child nutrition. Double-duty actions should consider the shared drivers of multiple forms of malnutrition, such as biology, environments and socio-economics(Reference Wells, Sawaya and Wibaek12,Reference Hong, Winichagoon and Khang33) . Through these double-duty actions, it is recommended that Thailand implement and/or strengthen interventions that focus on early life nutrition, such as promotion and protection of breast-feeding, optimising early nutrition, maternal nutrition and antenatal/postnatal programmes, school food policies and marketing regulations for infant and young child food products and low nutritious snacks popularly consumed by young children(37).
In conclusion, this study revealed an estimate of stunting-overweight among Thai children under-five. Despite the low prevalence of stunting-overweight, concrete efforts to tackle the double burden of malnutrition at population and individual levels should be followed by integrated interventions to address all forms of malnutrition.
Acknowledgements
Acknowledgements: None. Financial support: The authors received no specific funding for this work. Conflicts of interest: None. Authorship: L.B., S.A.H. and P.W. conceived and designed the study. L.B. and S.A.H. conducted data analysis. L.B., S.A.H., P.W., P.T. and V.K. contributed to the final version of the manuscript. All of the authors provided critical feedback which shaped the research, analysis and manuscript. All authors approved the final manuscript. Ethics of human subject participation: The data sets for the MICS 2015-2016 were accessed from the MICS website after receiving permission from UNICEF to use the MICS data. Since this secondary analysis study used publicly accessible de-identified data sets, it was exempted from full review and approved by the Human Research Ethics Committee of Mahidol University, Thailand (Approval No.: 2017/031.1105).






