Depression is a highly prevalent mental disorder influenced by a complex interplay of factors(1). Mindfulness-based interventions led to reductions in depressive symptoms(Reference Hedman-Lagerlöf, Hedman-Lagerlöf and Öst2–Reference Khoury, Sharma and Rush5). Recently, more evidence has been gathered on the associations of lifestyle factors, such as quality of food intake and BMI, with depression(Reference Cabout, Brouwer and Visser6–Reference Milaneschi, Simmons and Rossum9). As mindfulness-based interventions with an eating component were much more effective in reducing maladaptive eating behaviours compared with interventions without a mindful eating component(Reference Warren, Smith and Ashwell10,Reference O’Reilly, Cook and Spruijt-Metz11) , previous research started to examine associations between mindful eating and mental well-being. Mindful eating can be defined as ‘eating with awareness and attention’ and was associated with (change in) depressive symptoms(Reference Winkens, van Strien and Brouwer12,Reference Winkens, van Strien and Brouwer13) . Underlying mechanisms are not clear yet. Could food intake potentially mediate the association between mindful eating and change in depressive symptoms?
Both quantity and quality of food intake may be associated with mindful eating and depression. Food quantity is the total weight of the foods consumed and is generally, but not necessarily, reflected in the total amount of energy consumed. Food quality is the extent to which the diet meets specific dietary recommendations. The quantity and quality of the diet are thus two different concepts and are not necessarily related. However, when energy intake is high, a person is more likely to meet a specific food group (e.g. fish) requirement. Gougeon et al. found in a community-dwelling older population that dietary patterns were not related to depression, whereas energy intake was(Reference Gougeon, Payette and Morais14). This suggests that both can be independently associated with depression. Food intake might be associated with depression through its influence on different physiological processes that are involved in the development of depression, such as hypothalamic–pituitary–adrenal axis disturbances, inflammation and neurotransmitter imbalances(Reference Lopresti, Hood and Drummond15,Reference Winter, Hart and Charlesworth16) .
Mindful eating was the underlying mechanism in the association between higher general mindfulness and smaller serving size of energy-dense foods(Reference Beshara, Hutchinson and Wilson17). In a review on mindfulness interventions for weight loss and eating behaviours, findings from three out of four studies on attendance to the sensory properties of food did not find significant reductions in immediate amount of food consumed(Reference Tapper18). However, significant reductions in later amounts of food intake were found in a normal-weight and an overweight/obese population(Reference Tapper18). This finding was replicated for later snack intake in a sample of normal-weight men and women(Reference Seguias and Tapper19), while there was no reduced later snack intake in other experimental studies(Reference Whitelock, Gaglione and Davies-Owen20,Reference Whitelock, Higgs and Brunstrom21) . In patients with type 2 diabetes mellitus, a mindful eating intervention led to reduced energy intake immediately following the intervention and at the 3-month follow-up(Reference Miller, Kristeller and Headings22). In pregnant women, higher awareness for eating was associated with higher intake of fruit and vegetables(Reference Hutchinson, Charters and Prichard23).
There is very limited knowledge on mechanisms of action for the associations between mindful eating and food intake, but some potential explanations can be given. A reduction in eating automaticity and a prioritization of the amount of pleasure obtained from food instead of reaching satiation could explain the associations between mindful eating and decreased energy intake(Reference Tapper18). Increased interoceptive awareness (the ability to recognize and respond to internal states such as emotions, hunger and satiety) was associated with higher reliance on hunger and satiety cues(Reference Herbert, Blechert and Hautzinger24,Reference Herbert and Pollatos25) , and mediated the association between reliance on hunger and satiety cues and BMI(Reference Herbert, Blechert and Hautzinger24). This suggests that mindful eating might influence habitual food intake through an increase in interoceptive awareness. Another potential explanation is that mindful eating reduces cravings for food(Reference Tapper26,Reference Paolini, Burdette and Laurienti27) , which is associated with higher intake of unhealthy food products(Reference Chao, Grilo and White28). Finally, mindful eating could lead to increased self-regulation, which then leads to a more healthy food intake(Reference Kristeller and Wolever29).
Mindful eating may thus be related to food intake, but research is scarce and findings are mixed. The majority of the studies are not conducted in general population samples. Furthermore, those studies investigated specific dietary aspects, such as intake of high-energy foods, serving size and energy consumed after experimental manipulations, whereas habitual food intake measured over a longer time period may better reflect actual intake. In the last decades, nutritional research has shifted its focus from nutrients and foods towards dietary patterns(Reference Hu30). The Mediterranean Diet Score (MDS) is a useful tool to measure adherence to a healthy diet(Reference Sofi, Cesari and Abbate31,Reference Ocké32) and is associated with a lower risk of depression(Reference Molendijk, Molero and Sánchez-Pedreño33–Reference Nicolaou, Colpo and Vermeulen35). Higher energy intake was related to more depressive symptoms in adolescents(Reference Mooreville, Shomaker and Reina36), but in older samples lower energy intake may also be predictive of depression due to declining general health(Reference Gougeon, Payette and Morais37).
The aim of the present study was to investigate mediation of associations of mindful eating domains (Focused Eating; Eating in response to Hunger and Satiety Cues; Eating with Awareness; Eating without Distraction) with 3-year change in depressive symptoms by (i) diet quality as indexed by the MDS and (ii) diet quantity as indexed by total energy intake. Hypotheses were that mindful eating would be related to higher diet quality and lower diet quantity and that this would be related to lower depressive symptoms. There were no specific hypotheses regarding the different mindful eating domains.
Methods
Participants and procedure
Data were collected within the Longitudinal Aging Study Amsterdam (LASA), an ongoing cohort study in a representative sample of Dutch older adults aged 55 years or above, which started in 1992. The sampling and data collection procedures have been described in detail elsewhere(Reference Hoogendijk, Deeg and Poppelaars38,Reference Huisman, Poppelaars and van der Horst39) . Ethical approval for LASA was given by the Medical Ethics Committee of the VU University Medical Center Amsterdam and all participants provided written informed consent.
Mindful eating and food intake were measured in the ancillary ‘LASA Nutrition and Food-related Behaviour study’ that was conducted between the autumn of 2014 and the spring of 2015(Reference Winkens, van Strien and Barrada40). Depressive symptoms and antidepressant use were measured in the regular measurement waves of LASA: baseline data were measured in either 2011–2012 (cohorts 1 and 2) or 2012–2013 (cohort 3); and follow-up data were collected in 2015–2016. By using the depressive symptoms score at the follow-up measurement as outcome variable and adjusting analyses for baseline depressive symptoms, the outcome was interpreted as ‘change in depressive symptoms’. However, it should be noted that mindful eating and food intake were measured in-between this follow-up period, thereby making strict longitudinal interpretation of associations impossible.
Measures
Depressive symptoms
The Center for Epidemiologic Studies Depression scale (CES-D)(Reference Radloff41) was used to measure depressive symptoms in the past week and was administered in face-to-face interviews. The scale has twenty items with a 4-point scale ranging from 0 (rarely or none of the time; less than 1 d) to 3 (most or almost all the time; 5–7 d). A higher score indicates a higher level of depressive symptoms. Cronbach’s α of the CES-D was 0·87 (cohorts 1 and 2; n 494) and 0·85 (cohort 3; n 435) at baseline, and 0·85 at the follow-up measurement. The continuous CES-D score at the follow-up measurement was used as outcome variable, while controlling for the baseline CES-D score.
People with antidepressant use at baseline and/or the follow-up measurement were excluded from all analyses. Data on antidepressant use were retrieved by asking about medicine use. Medication names were recoded into Anatomical Therapeutic Chemical codes, which were used to define the use of antidepressants (yes/no)(42).
Mindful eating domains
The Mindful Eating Behavior Scale (MEBS)(Reference Winkens, van Strien and Barrada40) was used to measure the level of four different domains of mindful eating: (i) Focused Eating (five items, e.g. ‘I notice how my food looks’); (ii) Eating in response to Hunger and Satiety Cues (five items, e.g. ‘I trust my body to tell me when to eat’); (iii) Eating with Awareness (three items, e.g. ‘I eat something without being really aware of it’, reversed item); and (iv) Eating without Distraction (four items, e.g. ‘I multi-task when I am eating’, reversed item). Answer options ranged from 1 (‘never’) to 5 (‘very often’). Higher scores indicate a higher level of mindful eating. Cronbach’s α of the mindful eating domains was 0·85 for Focused Eating, 0·90 for Eating in response to Hunger and Satiety Cues, 0·82 for Eating with Awareness and 0·70 for Eating without Distraction.
Food intake
Food intake was assessed using a 238-item semi-quantitative FFQ with a reference period of 4 weeks, that was developed for the HEalthy LIfe in an Urban Setting study (HELIUS)(Reference Beukers, Dekker and de Boer43). This FFQ is an adapted version of an existing validated FFQ for a Dutch population(Reference Siebelink, Geelen and de Vries44). To calculate nutrient intakes, all food items were linked to a nutrient database that was based on the Dutch Food Composition Database(45).
Energy intake was calculated by summing the consumed kilocalories of all food items per day to achieve the total amount (kcal/d; 1 kcal = 4·184 kJ).
The MDS, an a priori, theoretically defined dietary pattern assessing diet quality, provides a measure of the adherence to the Mediterranean diet, which is characterized by high intakes of cereals, legumes, fruit, vegetables, olive oil and fish. The MDS was found to be a useful tool to measure adherence to a healthy diet(Reference Trichopoulou, Costacou and Bamia46,Reference Panagiotakos, Pitsavos and Arvaniti47) . Previous studies showed associations between Mediterranean-like dietary patterns and health benefits, also in non-Mediterranean countries(Reference Bonaccio, Di Castelnuovo and Costanzo48). The MDS was calculated by summing scores from 0 to 5 based on the intake in weekly or daily servings of eleven food groups(Reference Herbert, Blechert and Hautzinger24). The total score ranged from 0 to 55. A higher score indicates a healthier diet.
Confounders
Confounders in different models were sex, age, educational level, smoking status, physical activity level, alcohol consumption and BMI, because demographic and lifestyle factors have shown to be related to both mindful eating and depression and might therefore bias the associations under study. These variables were measured at the baseline measurement (2011–2013).
Sex and age were derived from the municipal registries.
Educational level was self-reported and categorized into low (none, elementary school), medium (secondary education, lower and intermediate vocational training) and high (higher vocational training, college and university education).
Smoking status (never/former/current) was self-reported.
Physical activity was measured using the validated LASA Physical Activity Questionnaire (LAPAQ)(Reference Stel, Smit and Pluijm49). Frequency and duration of walking outdoors, bicycling, light and heavy household activities and sports in the past 2 weeks were asked. Total time in minutes per day spent on these activities was calculated.
Alcohol consumption was assessed by asking respondents about the number of days per week they drank alcohol and the number of alcoholic drinks on these days(50). The number of alcoholic consumptions per week was calculated.
BMI (kg/m2) was calculated by dividing measured weight by the square of measured height. Weight was measured to the nearest 0·1 kg using a calibrated bathroom scale (Seca model 100; Lameris, Utrecht, The Netherlands). Corrections were made to adjust the measured body weight for clothing, shoes or a corset (–1 kg for one of those elements and –2 kg for more than one) when people did not wear underclothing only. Height was measured to the nearest 0·001 m using a stadiometer. Corrections were made to adjust the measured height for shoes (–1 cm) when people did not take their shoes off.
Statistical analysis
The proposed associations (mediation and confounding variables) are depicted in Fig. 1. All analyses were conducted using the statistical software package IBM SPSS Statistics version 23.0. People were included who had data on depressive symptoms at both the baseline and follow-up measurement. People who did not fill out the questionnaire of the ‘LASA Nutrition and Food-related Behaviour study’ themselves or who had missing values on one of more of the used variables were excluded from the analyses. For the calculation of the MDS and total energy intake, >10 missing values on the FFQ questions was used as a criterion for exclusion of participants. People with extreme values for energy intake based on sex-specific cut-offs were also excluded (<3347·2 kJ (<800 kcal) or >16 736 kJ (>4000 kcal) for men and <2092 kJ (<500 kcal) or >14 644 kJ (>3500 kcal) for women)(Reference Willett51). People with antidepressant use at baseline and/or the follow-up measurement were excluded because of possible distortion of the CES-D scores.
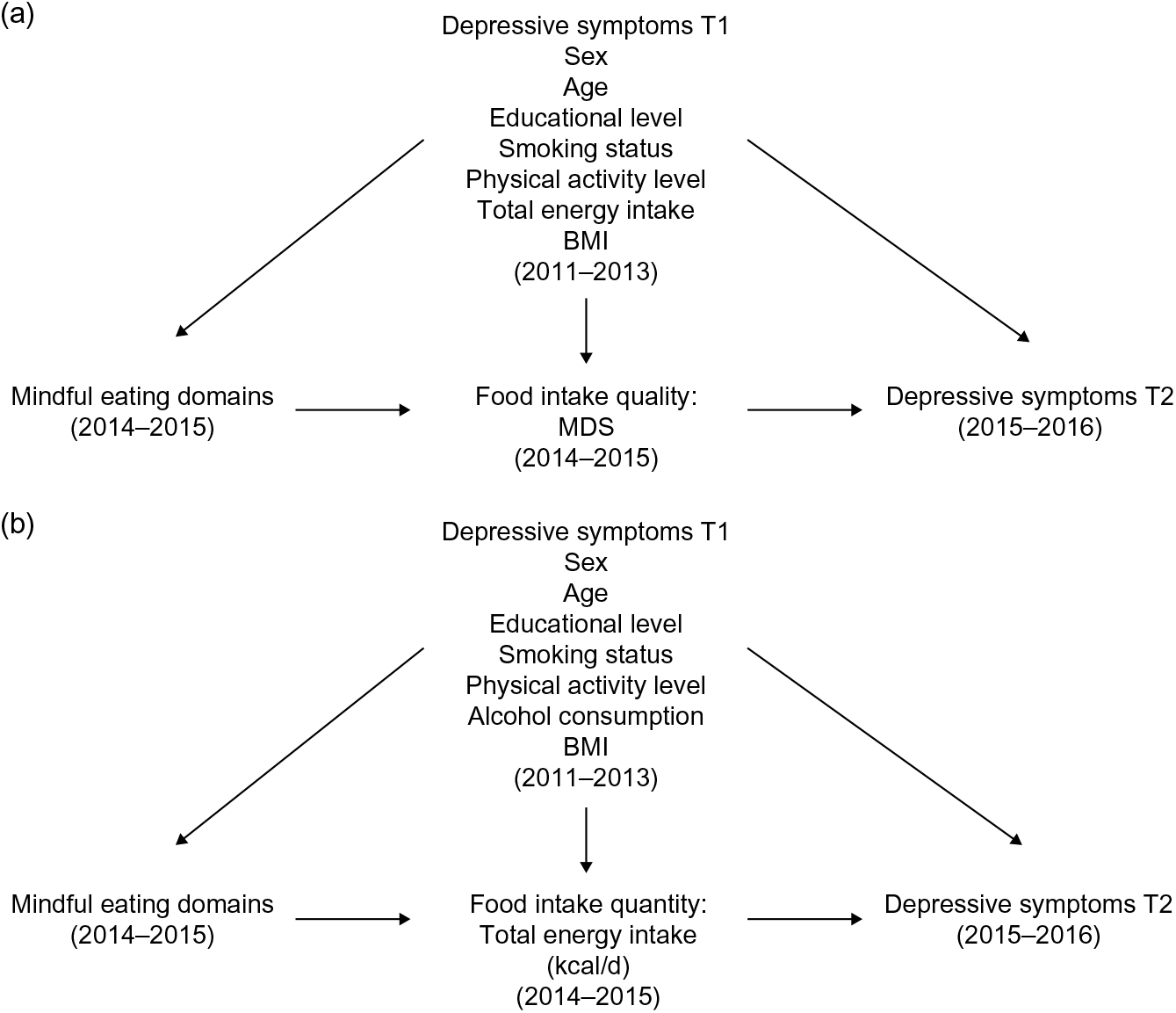
Fig. 1 Directed acyclic graph for proposed associations: (a) mediation by diet quality (Mediterranean Diet Score; MDS) in the association between mindful eating and 3-year change in depressive symptoms; (b) mediation by diet quantity (total energy intake; kcal/d; 1 kcal = 4·184 kJ) in the association between mindful eating and 3-year change in depressive symptoms (T1/T2, baseline/follow-up of the Longitudinal Aging Study Amsterdam)
Descriptive statistics were calculated to describe the sample.
To test whether MDS and total energy intake mediated the associations of mindful eating domains with change in depressive symptoms, percentile-corrected bootstrap confidence intervals for the indirect effects were calculated in separate mediation models. The PROCESS macro of Hayes(Reference Hayes52) was used to test the mediation role of MDS and total energy intake on the association of a mindful eating domain and change in depressive symptoms. Change in depressive symptoms was defined as depression at T2 over and above depression at T1 (by performing the regression of depression at T2 v. depression at T1 in the analysis). This analysis was conducted for each of the four mindful eating domains. Bootstrapping with 5000 samples was used. Results were considered significant if the upper and lower bound of the percentile bootstrap 95 % confidence interval did not contain zero.
To analyse changes in depressive symptoms, all analyses were adjusted for baseline depressive symptoms (model 1). Analyses were additionally adjusted for sex, age, educational level, smoking status and physical activity level (model 2). When assessing MDS as mediator, analyses were additionally adjusted for total energy intake (model 3). When assessing total energy intake as mediator, analyses were additionally adjusted for alcohol consumption (model 3). It was also tested if any of the associations changed when the analyses were additionally adjusted for BMI (model 4).
For the significant mediation analyses, sensitivity analyses were conducted using the ‘medsens’ command of the R package ‘mediation’, which calculates true indirect and direct effects for different values of the sensitivity parameter (ρ)(Reference Tingley, Yamamoto and Hirose53). The sensitivity analysis quantifies the degree of violation of sequential ignorability based on the correlation between the error terms of the mediator and of the outcome(Reference Imai, Keele and Tingley54). Bootstrapping with 5000 samples was used.
Results
Analytical sample
Complete baseline data on depressive symptoms were available for 2268 people (1261 from cohorts 1 and 2; 1007 from cohort 3), of whom 1684 people had complete CES-D data on the follow-up measurement as well. Of them, 1302 people had data on the ancillary ‘LASA Nutrition and Food-related Behaviour study’. People were excluded who did not fill out the questionnaire of this ancillary study themselves (n 103), who had one or more missing values on the MEBS (n 59) or missing values on any of the confounding variables (n 84). People with extreme values for energy intake based on sex-specific cut-offs (n 16) were excluded, as well as people with >10 missing values on the FFQ (n 3). People with antidepressant use at baseline and/or follow-up (n 75) as well as people with missing values on the questions on antidepressant use (n 33) were also excluded, which resulted in an analytical sample of 929 people. The characteristics of this sample are described in Table 1. Pearson correlations between variables are shown in Table 2.
Table 1 Baseline characteristics of the study sample of Dutch people aged 55 years or above from the Longitudinal Aging Study Amsterdam (n 929)
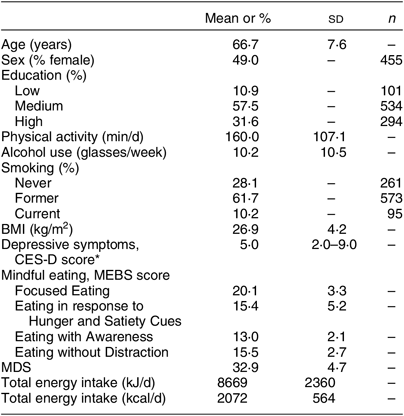
CES-D, Center for Epidemiologic Studies Depression scale; MEBS, Mindful Eating Behavior Scale; MDS, Mediterranean Diet Score.
* The median score and interquartile range of depressive symptoms are presented because of a skewed distribution.
Table 2 Pearson correlations between the mindful eating domains, food intake, depressive symptoms and descriptive characteristics among the study sample of Dutch people aged 55 years or above from the Longitudinal Aging Study Amsterdam (n 929)
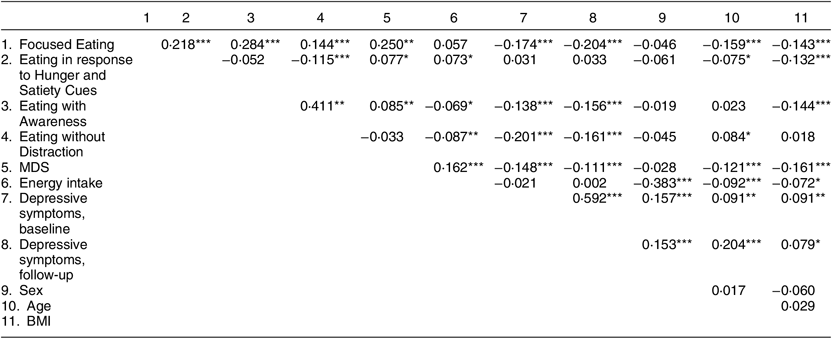
MDS, Mediterranean Diet Score.
*P < 0·05, **P < 0·01, ***P < 0·001.
Mediation analyses: dietary quality
Significant direct effects were found for the domains Focused Eating, Eating with Awareness and Eating without Distraction with change in depressive symptoms, but not for the domain Eating in response to Hunger and Satiety Cues (see Figs 2 and 3). However, mediation can exist and be tested even in the absence of such an overall significant association(Reference Hu30,Reference Sofi, Cesari and Abbate31) . We therefore proceeded to examine whether food intake mediated the association between Eating in response to Hunger and Satiety Cues and depressive symptoms.
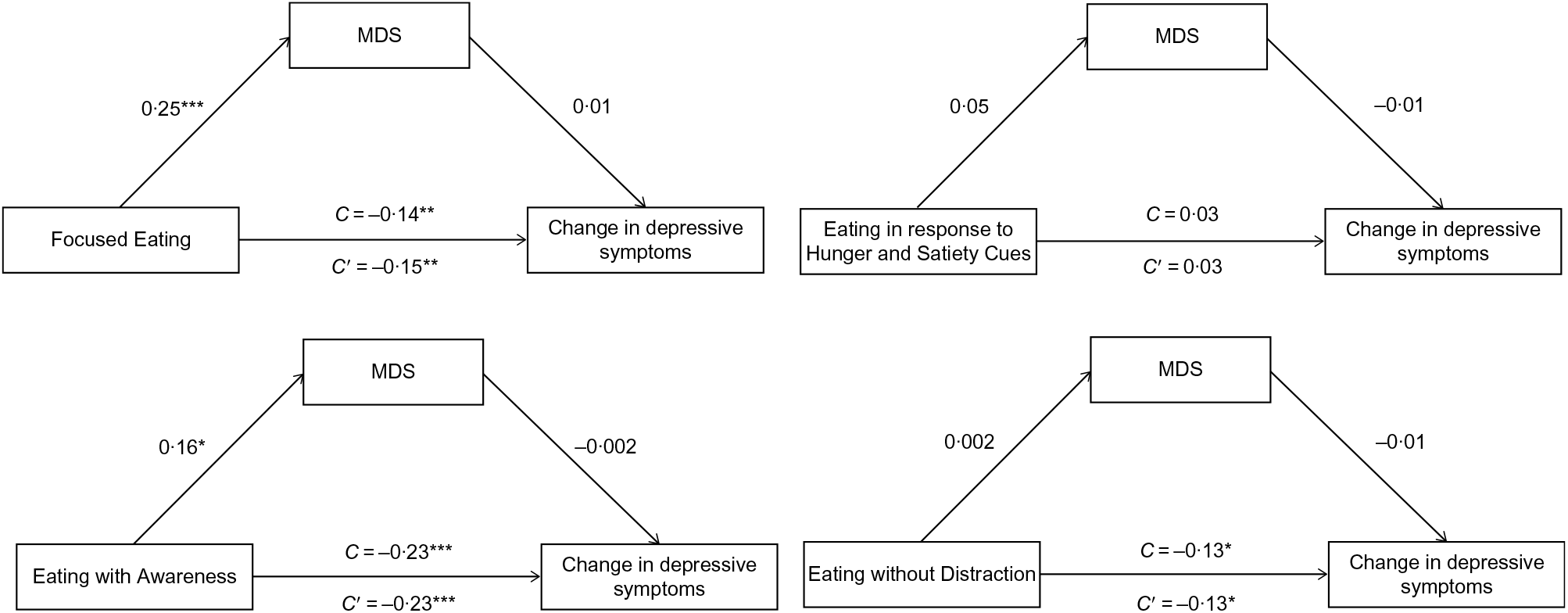
Fig. 2 Mediation models of the associations between four mindful eating domains and 3-year change in depressive symptoms via diet quality (Mediterranean Diet Score; MDS) in a sample of people aged 55 years or above from the Longitudinal Aging Study Amsterdam (n 929). Unstandardized regression coefficients from a bootstrap procedure with 5000 samples are provided along the paths. Analyses are adjusted for baseline depressive symptoms, sex, age, educational level, smoking status, physical activity level and total energy intake (model 3). C, total effect; C′, direct effect; *P < 0·05, **P < 0·01, ***P < 0·001
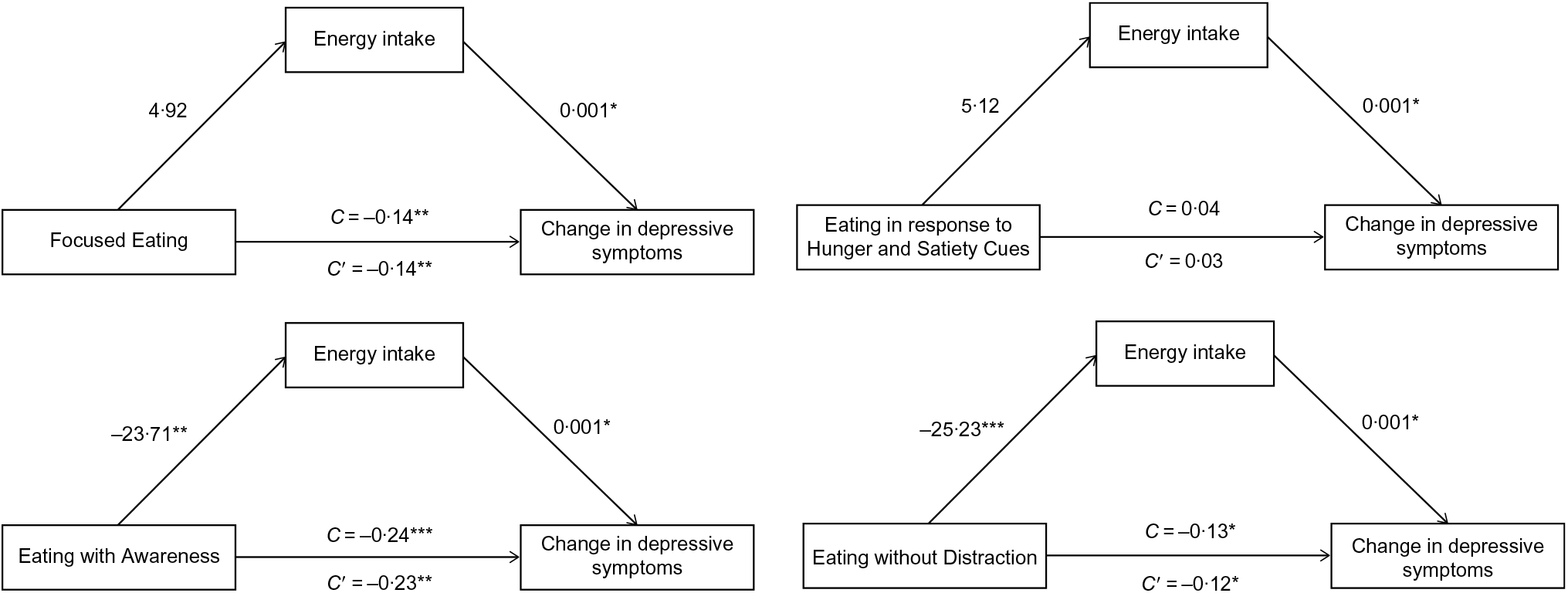
Fig. 3 Mediation models of the associations between four mindful eating domains and 3-year change in depressive symptoms via diet quantity (total energy intake; kcal/d; 1 kcal = 4·184 kJ) in a sample of people aged 55 years or above from the Longitudinal Aging Study Amsterdam (n 929). Unstandardized regression coefficients from a bootstrap procedure with 5000 samples are provided along the paths. Analyses are adjusted for baseline depressive symptoms, sex, age, educational level, smoking status, physical activity level and alcohol consumption (model 3). C, total effect; C′, direct effect; *P < 0·05, **P < 0·01, ***P < 0·001
The indirect effects of the adjusted models of the mediation analyses of the MDS in the associations of the mindful eating domains with depressive symptoms are shown in Table 3. There was no mediation by the MDS for any of the four mindful eating domains in all of the adjusted models (indirect effects fully adjusted models: B = 0·002, 95 % CI −0·015, 0·021 for Focused Eating; B = −0·001, 95 % CI −0·006, 0·003 for Eating in response to Hunger and Satiety Cues; B = 0·0001, 95 % CI −0·016, 0·015 for Eating with Awareness; B = 0·001, 95 % CI −0·004, 0·005 for Eating without Distraction).
Table 3 Indirect effects from mediation analyses of diet quality (Mediterranean Diet Score; MDS) and diet quantity (total energy intake; kcal/d; 1 kcal = 4·184 kJ) in the associations of four mindful eating domains with 3-year change in depressive symptoms in a sample of people aged 55 years or above from the Longitudinal Aging Study Amsterdam (n 929)
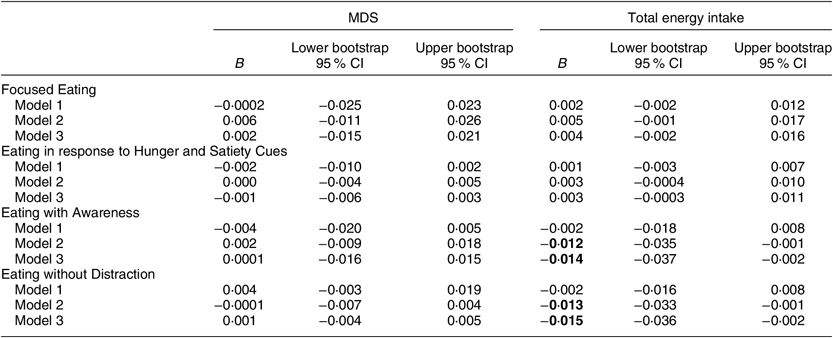
Depressive symptoms are measured with the Center for Epidemiologic Studies Depression Scale continuous score. Unstandardized regression coefficients (B) and percentile bootstrap confidence intervals are reported (bootstrap sample size = 5000). Bold values indicate statistically significant results.
Model 1 was adjusted for baseline depressive symptoms; model 2 was additionally adjusted for sex, age, educational level, smoking status and physical activity level; model 3 (MDS) was additionally adjusted for total energy intake; model 3 (total energy intake) was additionally adjusted for alcohol consumption.
In Fig. 2, the coefficients of the various paths of the mediation models with MDS as mediator are shown. The MDS was not significantly associated with change in depressive symptoms when controlling for any of the mindful eating domains. The mindful eating domains Focused Eating and Eating with Awareness were significantly associated with the MDS: in the fully adjusted models, a 1 point increase in Focused Eating was associated with an increase of 0·25 points on the MDS, and a 1 point increase in Eating with Awareness was associated with an increase of 0·16 points on the MDS, which is indicative of a healthier diet. Changes in associations when additionally adjusting for BMI (model 4) were negligible (e.g. association between Focused Eating and the MDS model 4: B = 0·24). Inclusion of people with extreme values on energy intake (n 16) did not change any of these results.
Mediation analyses: diet quantity
The indirect effects of the adjusted models of the mediation analyses of total energy intake in the associations of the mindful eating domains with depressive symptoms are shown in Table 3. There was a significant mediation by total energy intake for the mindful eating domains Eating with Awareness and Eating without Distraction in the adjusted models 2 and 3 (indirect effects fully adjusted models: B = −0·014, 95 % CI −0·037, −0·002 for Eating with Awareness; B = −0·015, 95 % CI −0·036, −0·002 for Eating without Distraction). There was however no mediation by total energy intake for the mindful eating domains Focused Eating and Eating in response to Hunger and Satiety Cues in all of the adjusted models (indirect effects fully adjusted models: B = 0·004, 95 % CI −0·002, 0·016 for Focused Eating; B = 0·003, 95 % CI −0·0003, 0·011 for Eating in response to Hunger and Satiety Cues).
In Fig. 3, the coefficients of the various paths of the mediation models with total energy intake as mediator are shown. A higher total energy intake was associated with more depressive symptoms when controlling for any of the mindful eating domains: an increase of 418·4 kJ/d (100 kcal/d) was associated with an increase of 0·1 points in the depressive symptoms score in the fully adjusted models. The mindful eating domains Eating with Awareness and Eating without Distraction were significantly associated with total energy intake: a 1 point increase in Eating with Awareness was associated with a decrease of 99·2 kJ/d (23·7 kcal/d), and a 1 point increase in Eating without Distraction was associated with a decrease of 105·4 kJ/d (25·2 kcal/d). Changes in associations when additionally adjusting for BMI (model 4) were negligible (e.g. indirect effect for Eating without Distraction model 4: B = −0·016, 95 % CI −0·038, −0·003; association between Eating without Distraction and energy intake model 4: B = −24·5). Inclusion of people with extreme values on energy intake (n 16) did not change any of these results. Results of the sensitivity analyses for the two significant mediation models can be found in the online supplementary material, Supplemental File S1.
Post hoc analysis: multiple mediation
Simple mediation analyses were conducted as quality and quantity were both independently associated with depression in previous studies and because there was only a small correlation between food quantity and quality in the current study (r = 0·162, see Table 2). However, because of this correlation, multiple mediation analyses with the MDS and total energy intake as parallel mediators were conducted as post hoc analyses. By testing multiple mediators in one model compared with simple mediation models, the likelihood of parameter bias due to omitted variables is reduced(Reference Preacher and Hayes55). A significant total indirect effect is no prerequisite for investigating specific indirect effects; either or both types of effect are interesting and worth investigating(Reference Preacher and Hayes55). Therefore, both the total indirect effect of the set of mediators as well as the specific indirect effects of each individual mediator conditional on the other mediator in the model were reported, together with the corresponding percentile 95 % confidence intervals. It is important to note that the specific indirect effect through either quality or quantity of food intake represents the ability of that variable to mediate the association of mindful eating with depressive symptoms conditional on the inclusion of the other variable in the model: it is thus the unique mediating effect of that variable.
To test whether MDS and total energy intake mediated the associations of mindful eating domains with change in depressive symptoms, percentile bootstrap confidence intervals for the indirect effects were calculated in multiple mediation models. The total and specific indirect effects of the multiple mediation analyses of food quality and food quantity in the associations of the mindful eating domains with depressive symptoms are shown in the online supplemental material, Supplemental File S2. No mediation by food intake was found for the domains Focused Eating (total mediation: B = 0·006, 95 % CI −0·014, 0·025) and Eating in response to Hunger and Satiety Cues (total mediation: B = 0·002, 95 % CI −0·004, 0·009). For the domain Eating with Awareness, only specific mediation by total energy intake was found in the fully adjusted model (B = −0·018, 95 % CI −0·039, −0·001). For the domain Eating without Distraction, both total mediation and specific mediation by total energy intake were found in the fully adjusted model (indirect effect: B = −0·016, 95 % CI −0·036,−0·001 for total mediation; B = −0·017, 95 % CI −0·036, −0·002 for mediation by total energy intake). As these results are similar to the results of the simple mediation analyses, we can conclude that the results of these simple mediation analyses were not biased due to the omitted variable (either food quality or food quantity).
Discussion
The present study is the first to investigate both quality and quantity of food intake as underlying mechanisms in the associations between mindful eating domains and change in depressive symptoms. In the study, higher scores on the mindful eating domains Eating with Awareness and Eating without Distraction were associated with a decrease in depressive symptoms after 3 years through lower total energy intake. No mediation was observed for the domains Focused Eating and Eating in response to Hunger and Satiety Cues.
Regarding diet quality as a potential underlying mechanism, we found that diet quality was no mediator between the mindful eating domains and change in depressive symptoms. This is likely caused by the non-significant associations between the MDS and change in depressive symptoms when controlling for the mindful eating domains, which is in contrast to recent meta-analyses regarding diet quality and (incidence of) depressive symptoms. In these meta-analyses, adherence to a Mediterranean diet was associated with a lower risk of depressive symptoms over time(Reference Molendijk, Molero and Sánchez-Pedreño33–Reference Nicolaou, Colpo and Vermeulen35). A review of longitudinal studies among older adults showed mixed findings(Reference Gougeon56). Gougeon et al. also found in a community-dwelling older population that dietary patterns were not related to depression, whereas energy intake was(Reference Gougeon, Payette and Morais14). It might thus be that quantity of food intake, instead of quality of food intake, becomes more important in explaining changes in depression over time in older adults.
Although the MDS was not a mediating factor in the associations between mindful eating and depression, higher scores on the domains Focused Eating and Eating with Awareness were associated with a higher MDS, indicative of a healthier diet. These results are in concordance with a study showing that higher attentive eating was associated with a higher intake of fruit and vegetables in pregnant women(Reference Hutchinson, Charters and Prichard23), as well as with an experimental study showing that higher general mindfulness was related to more often choosing fruit instead of unhealthy options(Reference Jordan, Wang and Donatoni57). Although there is no indication that a better diet quality is related to depression in our study, mindful eating might be beneficial in increasing general health status through increased diet quality. Further research is needed to investigate this.
Regarding diet quantity as a potential underlying mechanism, we found that energy intake mediated associations of two mindful eating domains with depression: higher scores on Eating with Awareness and Eating without Distraction were related to lower energy intake per day, which was associated with fewer depressive symptoms. That controlling the analyses for physical activity and BMI did not change any of the conclusions suggests that energy intake is uniquely associated with mindful eating, independent of BMI and physical activity. Previous studies on distracted eating found that listening to a story(Reference Long, Meyer and Leung58,Reference Bellisle, Dalix and Slama59) , watching television(Reference Bellisle, Dalix and Slama59) and listening to music(Reference Stroebele and de Castro60) were associated with higher energy intake. As mechanisms of action for the associations between mindful eating and food intake are still unclear, future research could examine some of these potential mechanisms, such as reduced automaticity, increased prioritization of joy, increased interoceptive awareness, increased self-regulation or decreases in food cravings.
Energy intake was not a mediator in the associations of Focused Eating and Eating in response to Hunger and Satiety Cues with change in depressive symptoms. Both Focused Eating and Eating in response to Hunger and Satiety Cues were not significantly associated with total energy intake. That we did not find an association between Focused Eating and total energy intake is in concordance with studies not showing associations between attentive eating and direct food intake(Reference Tapper18) and with some recent experimental studies that did not find reduced later amounts of intake(Reference Whitelock, Gaglione and Davies-Owen20,Reference Whitelock, Higgs and Brunstrom21) , but is contradictory to other studies that did find these associations with later food intake(Reference Tapper18,Reference Seguias and Tapper19) . It could however be that although higher Focused Eating potentially leads to reduced later amounts of food intake, this is compensated for at other time points, thereby leading to the same amount of total energy consumed in a daily dietary pattern. Energy intake measured after experimental manipulations might not be characteristic of habitual total energy intake. That we did not find any association with the domain Eating in response to Hunger and Satiety Cues might be due to the older age of the sample: changes in hunger, satiety and appetite occur due to the ageing process(Reference Elsner61).
Strengths of the present study are the use of data on both diet quality and quantity and the large national representative sample of Dutch middle-aged and older adults, whereas previous studies investigated specific dietary aspects and mostly used students and female samples. A limitation of this sample is that our results might not be generalizable to younger age samples. Food intake might change during ageing; although a higher energy intake is generally associated with depression, lower energy intake may also be predictive of depression due to declining general health in older adults(Reference Gougeon, Payette and Morais14). However, in the present study, we found that a higher energy intake was associated with more depressive symptoms over time. Another limitation is that mindful eating and food intake were measured at the same time point, whereas in mediation analyses desirably the temporal order of all of the variables is tested. Although the causal order of the mindful eating domains and food intake therefore cannot be established, mindful eating is hypothesized to precede food intake in time. Another limitation regarding the temporality is that mindful eating and food intake were measured in-between the baseline and follow-up measures of depressive symptoms. As a result, depressive symptoms measured at baseline might have influenced mindful eating and food intake measured in the ancillary study. Due to these limitations, the current mediation analyses are only exploratory. Our results provide more insight into possible mechanisms underlying the associations between mindful eating and depression and may generate hypotheses for further study. Further research is needed to test the associations of mindful eating with change in food intake over time and ultimately with change in depressive symptoms.
As food quality mediated only the associations of Eating with Awareness and Eating without Distraction with change in depressive symptoms, further research should investigate other potential underlying mechanisms. In a previous study we found that the psychological eating styles, especially external eating, mediated the association between mindful eating and change in depressive symptoms(Reference Winkens, van Strien and Brouwer13). Another potential mediating variable is obesity, as obesity is bidirectionally linked with depression: the presence of one increases the risk for developing the other(Reference Milaneschi, Simmons and Rossum9,Reference Faith, Butryn and Wadden62) . General mindfulness interventions were effective in reducing weight(Reference Carrière, Khoury and Günak63). More research into associations between mindful eating and BMI, as well as BMI as mediating factor in the associations between mindful eating and depression, would be very interesting.
In the present study, higher scores on two mindful eating domains were associated with a decrease in depressive symptoms through lower total energy intake. Diet quantity, but not diet quality, could be a possible underlying mechanism in the associations between mindful eating and change in depressive symptoms.
Acknowledgements
Financial support: This work was supported by the European Union FP7 MooDFOOD Project ‘Multi-country cOllaborative project on the rOle of Diet, FOod-related behaviour, and Obesity in the prevention of Depression’ (grant agreement number 613598). The Longitudinal Aging Study Amsterdam is supported by a grant from the Netherlands Ministry of Health Welfare and Sports, Directorate of Long-Term Care. The data collection in 2012–2013 was financially supported by the Netherlands Organization for Scientific Research (NWO) in the framework of the project ‘New Cohorts of young old in the 21st century’ (file number 480-10-014). The funding agencies had no role in the design, analysis or writing of this article. Conflict of interest: The authors declare no conflict of interest. Authorship: L.H.H.W., M.V., I.A.B. and T.v.S. designed the study. L.H.H.W. and L.E.M.E. collected the data. L.H.H.W. wrote the first draft with contributions from M.V., I.A.B. and T.v.S. L.H.H.W. conducted the statistical analyses. All authors reviewed and commented on subsequent drafts of the manuscript. All authors approved the final version. Ethics of human subject participation: This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects in LASA were approved by the Medical Ethics Committee of the VU University Medical Center Amsterdam. All participants provided written informed consent.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/S1368980019003732








