Milk is recognised for its nutritional quality, as it contains proteins of high biological value, significant quantities of vitamin A and B complex vitamins(1) and is an important source of Ca, which is essential to bone formation and maintenance as well as the regulation of neuronal function(Reference Bueno and Czepielewski2). The main carbohydrate in milk is lactose, which contributes to the intestinal absorption of Ca, Mg and P(1). The highest concentration of fat in whole milk is saturated (75 %) and contributes to the absorption of liposoluble vitamins, cholesterol and carotenoids(1).
Milk consumption is indicated for individuals to reach the daily recommendation for Ca, which is stipulated to be 1000 mg for adults and 1200 mg for older people(3). Besides being an important nutrient for bone formation and maintenance(Reference Rozenberg, Body and Bruyère4), Ca has been recognised in several meta-analyses for lowering the risk of rectal cancer(Reference Aune, Lau and Chan5), obesity(Reference Visioli and Strata6) and type II diabetes mellitus(Reference Aune, Norat and Romundstad7). Despite all these properties, questions are raised regarding milk consumption by adults and older people, especially due to the possibility of lactase non-persistence, allergy to milk protein, as well as an increased risk of prostate and ovarian cancer(Reference Lu, Chen and Niu8,Reference Qin, Moorman and Alberg9) and diseases related to saturated fat intake(Reference Lawrence10,Reference Hooper, Martin and Abdelhamid11) .
The prevalence of lactase non-persistence in the world population is estimated to be 70 %(1,Reference Heyman and Care12) . However, this rate varies considerably among countries, ranging from 5 % in northeastern Europe(Reference Almon, Engfeldt and Tysk13) to approximately 100 % in Asia and the Middle East(Reference Sahi14). In Brazil, a study conducted with adults estimated the prevalence of lactase non-persistence to be 57 % among whites and 80 % in the black population(Reference Mattar, Matins and Carrilho15). In contrast, the estimated prevalence of allergy to milk protein among adults in the world is < 0·5 %(Reference Fiocchi, Brozek and Schünemann16).
As whole milk has a high saturated fat content, dietary guides in different countries(1) recommend that adults and older people consume low-fat versions to reduce the risk of developing CVD(Reference Lawrence10,Reference Hooper, Martin and Abdelhamid11) . However, this recommendation has been questioned, as recent meta-analyses and cohort studies have shown that there is no clear, consistent evidence that the saturated fat in milk is a risk factor for an increase in the incidence of CVD or mortality due to such diseases(Reference O’Sullivan, Hafekost and Mitrou17–Reference Bhupathi, Mazariegos and Rodriguez22).
Several types of milk are available on the Brazilian market, such as A, B, C and ultra-high temperature, which differ in terms of requirements of hygiene, milking and transportation(23). Type A is a milk of excellent microbiological quality being pasteurised and packed in the farm(23). Type B is a milk of good microbiological quality, but with higher levels of micro-organisms due to the time interval between milking (performed in the farm) and pasteurisation (performed in dairy products plants)(23). Type C is a milk of low microbiological quality because it is transported to dairy products plants at room temperature(23). Ultra-high temperature milk undergoes a process of heating, sterilisation and cooling ensuring the elimination of all micro-organisms(24). Ultra-high temperature milk is available in the types of whole milk (3 % fat or more), reduced fat (0·6 and 2·9 %) and skimmed (≤ 0·5 % fat) as well as lactose-free, low-lactose, enriched with Ca, Fe, vitamins, collagen or fibre, and flavoured(24).
Considering the nutritional quality of milk, questions regarding its consumption by adults and older people, the diversity of available products and the few studies evaluating whether milk consumption meets the recommendations of Brazilian dietary guideline(25), the aim of the present study was to estimate the prevalence of milk consumption and identify factors associated with frequent milk consumption and the consumption of low-fat/skimmed milk among adults and older people, evaluating adherence to existing guideline(25).
Methods
A population-based cross-sectional study was conducted with data from the 2015 Campinas Food Intake and Nutritional Status Survey and the 2015 Campinas Health Survey conducted in the city of Campinas, state of São Paulo, Brazil. The respondents were community-dwelling residents of urban areas of the city, divided into three age domains: adolescents (10–19 years), adults (20–59 years) and older people (60 years or older). In the present study, we only considered adults and older people, totaling a sample of 1710 individuals.
The aim of the 2015 Campinas Health Survey was to analyse living and health conditions of the population. The sample was obtained using probabilistic, stratified, two-stage, cluster sampling. Seventy census sectors were selected in the first stage and households were selected in the second stage. The sample sizes were calculated considering an estimated proportion of 0·05, a 95 % CI (z = 1·96), sampling error of 4–5 percentage points and a design effect of 2. The minimum sizes were defined as 1400 for adults and 1000 for older people. Assuming response rates of 78 and 80 %, respectively, 929 households were selected for interviews with adults and 2853 were selected for interviews with older people. In each household, interviews were held with all residents in the age domain for which the household was selected(Reference Alves, Escuder and Claro26). The information was collected by trained interviewers through direct interviews with the selected individuals with the aid of an electronic device (tablet).
The 2015 Campinas Nutrition Survey was conducted with the same sample as the health survey. Information was collected on food consumption and nutritional status involving a 24-h recall and questions addressing the frequency of certain foods, self-reported weight and height, body perception, self-rated diet quality, practices developed for weight loss, etc. Trained interviewers through direct interviews collected the information with the selected individuals with the aid of a questionnaire. The data were entered into a databank developed using the EpiData 3.1 program (EpiData Assoc.).
Variables
The dependent variables for the current study (taken from the 2015 Campinas Nutrition Survey) were (a) frequent consumption (five to seven times per week) of milk (any type) and (b) the consumption of low-fat/skimmed milk among the individuals who reported consuming milk. The choice of dependent variables considered the recommendation of the Brazilian current dietary guide(25), which does not establish the amount of daily milk intake but encourages the frequent consumption of in natura and minimally processed products such as milk and its derivatives, giving preference to low-fat/skimmed milk(25).
The following sets of variables were considered for the analysis of associated factors:
-
Demographic and socio-economic variables: sex, age, self-declared race/skin colour, family income per capita (using the Brazilian monthly minimum wage as the unit of analysis) and schooling (in years of study).
-
Health-related behaviours: smoking, frequency of alcohol intake and physical activity in the leisure context. The latter variable was evaluated using the International Physical Activity Questionnaire and the participants were categorised as active (at least 150 min per week distributed among at least 3 d), insufficiently active (not meeting the requirements for the active category) or inactive (no physical activity in the leisure context) (27).
-
Food frequency: obtained by the food frequency questions of the 2015 Campinas Nutrition Survey, from which the following were selected: legumes, raw and cooked vegetables, whole foods and fruit. Frequency was categorised as < five times per week or ≥ five times per week.
-
Self-rated health: categorised as excellent/very good/good or regular/poor/very poor.
-
Number of chronic diseases on the following checklist: hypertension, diabetes, angina, myocardial infarction, arrhythmia, other heart diseases, cancer, rheumatism/arthritis/arthrosis, osteoporosis, asthma/bronchitis/emphysema, rhinitis/sinusitis, tendinitis/repetitive stain injury/work-related musculoskeletal disorder and vascular problems.
-
BMI: calculated from self-reported weight and height. The cut-off points recommended for adults(28) and older people(29) were used and the categories were underweight, ideal weight, overweight and obesity.
Associations between the dependent and independent variables were evaluated using the χ 2 test with the Rao–Scott correction. Poisson multiple regression analysis was used for the calculation of prevalence ratios and respective 95 % CI adjusted by sex and age. A hierarchical Poisson regression model was created using the stepwise backward method in two steps. In the first step, the socio-demographic variables with a P-value < 0·20 in the bivariate analysis were incorporated into the model and those with a P-value < 0·05 after the adjustments remained in the model. In the second step, the clinical and behavioural variables with a P-value < 0·20 in the bivariate analysis were incorporated into the model with the variables that remained in the first step and those with a P-value < 0·05 after the adjustments remained in the final model. The statistical analyses were performed with the aid of the Stata 14.0 program (Stata Corp.), which enables considering weights resulting from the sampling process.
Results
Among the households selected for interviews with adults and older people, the non-response rate was 8·7 % due to refusals and other reasons. Among the adults and older people identified to be interviewed in the households, the refusal rate was 21 % and loss rate for other reasons rate was 1·8 %. During the 2015 Campinas Nutrition Survey, there was an additional loss rate of 13·2 %. Thus, the sample analysed in the present study was composed of 1710 adults and older people.
Mean age was 44 years (95 % CI 42·5, 45·4). The sample was composed predominantly of women (52·7 %), individuals with self-declared white skin colour (68·0 %), individuals with < 9 years of schooling (41·0 %), individuals with a family income per capita less than the Brazilian monthly minimum wage (35·0 %) and individuals without private health insurance (52·5 %). Based on the BMI, 41·7 % of the sample were in the ideal weight range, 33·5 % were overweight and 21·5 % were obese (data not presented in tables).
A total of 26·2 % (95 % CI 23·2, 29·4) of the sample did not consume milk, 29·8 % (95 % CI 26·1, 33·5) consumed milk four times per week or less and 44·0 % (95 % CI 39·5, 48·7) consumed milk five to seven times per week. Among those who consumed milk, 81·1 % (95 % CI 76·9, 84·7) drank whole milk, 18·4 % (95 % CI 14·8, 22·6) drank low-fat/skimmed milk and 0·5 % (95 % CI 0·17, 1·2) drank lactose-free milk. Individuals who drank soya milk, who accounted for 0·8 % (95 % CI 0·4, 1·6) of the overall sample, were not counted as milk consumers. Among those who reported drinking low-fat/skimmed milk, 76·2 % (95 % CI 67·1, 82·1) consumed it five to seven times per week (data not presented in tables).
The prevalence of frequent milk consumption (five to seven times per week) was significantly higher among women and older people. The prevalence of low-fat/skimmed milk consumption was higher among women, individuals with 12 or more years of schooling and those with an income per capita of the Brazilian monthly minimum wage or higher. The prevalence of low-fat/skimmed milk consumption was lower among individuals with self-declared black or brown skin colour (Table 1).
Table 1 Prevalence and prevalence ratios of frequent milk consumption (five to seven times per week) and low-fat/skimmed milk consumption according to demographic and socio-economic characteristics. Campinas, SP, Brazil, 2015
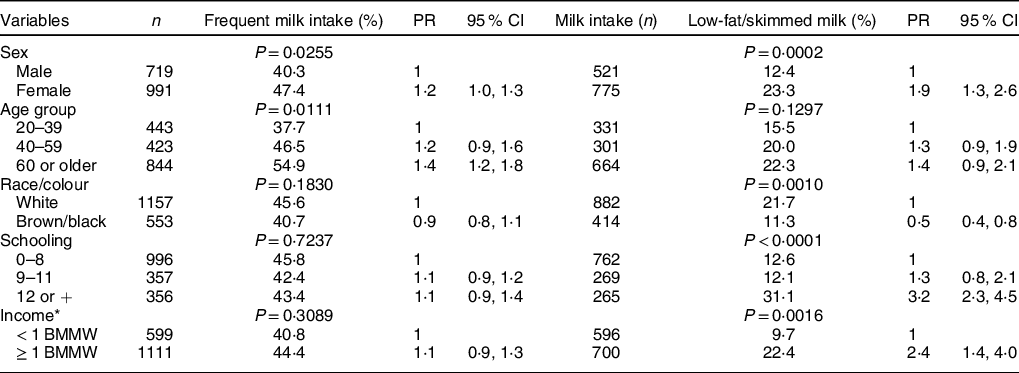
n, number of individuals in unweighted sample; PR, prevalence ratio adjusted by sex and age; BMMW, Brazilian monthly minimum wage.
* Family income per capita.
Frequent milk consumption (five to seven times per week) was not associated with health status and morbidities variables. Low-fat/skimmed milk consumption was lower among underweight individuals and increased gradually with the increase in the number of chronic diseases (Table 2). Among the individuals who reported drinking low-fat/skimmed milk, 68·4 % (95 % CI 51·9, 78·2) had some type of CVD (data not presented in tables).
Table 2 Prevalence and prevalence ratios of frequent milk consumption (five to seven times per week) and low-fat/skimmed milk consumption according to health status and morbidities. Campinas, SP, Brazil, 2015
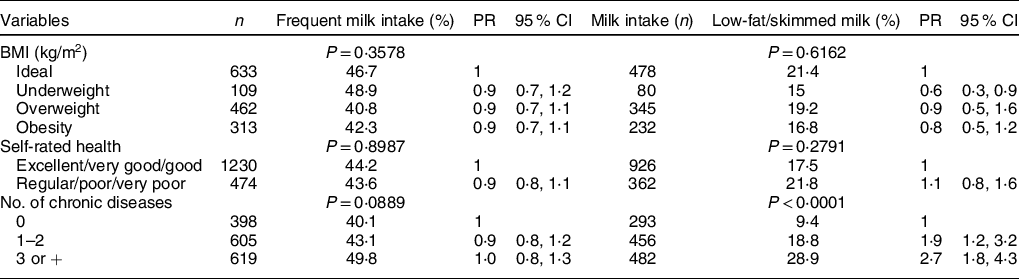
n, number of individuals in unweighted sample; PR, prevalence ratio adjusted by sex and age.
The prevalence of frequent milk consumption was lower among inactive individuals and smokers and higher among those who reported the frequent consumption of vegetables, whole foods and fruit. The prevalence of low-fat/skimmed milk consumption was lower among smokers and higher among individuals who consumed vegetables, whole foods and fruit five or more times per week and those who consumed alcoholic beverages two or more times per week (Table 3).
Table 3 Prevalence and prevalence ratios of frequent milk consumption (five to seven times per week) and low-fat/skimmed milk consumption according to health-related behaviours and diet quality. Campinas, SP, Brazil, 2015
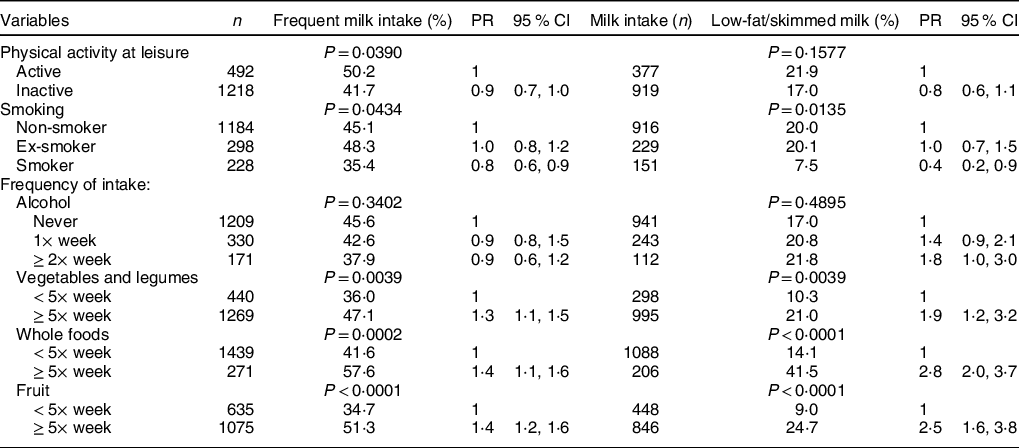
n, number of individuals in unweighted sample; PR, prevalence ratio adjusted by sex and age.
In the final model of frequent milk consumption of any type, the significantly associated variables were sex, age group and the frequent ingestion of whole foods and fruit (Table 4). In the final model of low-fat/skimmed milk consumption, the significantly associated variables were sex, schooling, family income per capita, number of chronic diseases and the frequent ingestion of whole foods and fruit (Table 5).
Table 4 Hierarchical Poisson regression model of factors associated with frequent milk consumption (five to seven times per week). Campinas, SP, Brazil, 2015

PR, prevalence ratio.
* First step: prevalence ratio adjusted by socio-economic and demographic variables.
† Second step: prevalence ratio adjusted by health-related behaviours and morbidities.
Table 5 Hierarchical Poisson regression model of factors associated with low-fat/skimmed milk consumption. Campinas, SP, Brazil, 2015

PR, prevalence ratio; BMMW, Brazilian monthly minimum wage.
* First step: prevalence ratio adjusted by socio-economic and demographic variables.
† Second step: prevalence ratio adjusted by health-related behaviours and morbidities.
Discussion
The present findings reveal that, although milk is rich in proteins, vitamins and minerals and the market offers several options to meet the specific needs of individuals, the population studied does not consume this product in compliance with current guidelines. A total of 26·2 % reported not consuming milk at all, 29·8 % did not consume it frequently (< five times per week) and only 44 % consumed it frequently (five to seven times per week). Moreover, low-fat/skimmed milk consumption was reported by only 18·4 % of the individuals who drank milk.
Studies on frequent milk intake in Brazil are still scarce(Reference Mallmann, Gentleman and Mello30,Reference Muniz, Madruga and Araújo31) . The low prevalence of frequent milk intake (five to seven times per week) was also evaluated in only two other Brazilian studies conducted in the city of Pelotas (46·2 %)(Reference Muniz, Madruga and Araújo31) and in the municipality of Palmeira das Missões (32·6 %)(Reference Mallmann, Gentleman and Mello30), both in Rio Grande do Sul. According to 2008–2009 Brazilian Family Budget Survey (POF 2008–2009)(32), only 17 % of the Brazilian population reported milk consumption in the food diary, showing its low consumption in the country. Regarding milk derivatives, the POF 2008–2009 showed that only 13·5, 4·1 and 1·2 % of the individuals reported consuming cheeses, yogurts and other milk products, respectively(32).
Frequent milk consumption (five to seven times per week) and low-fat/skimmed milk consumption were significantly higher among women. These findings have also been reported in other studies conducted in Brazilian cities and other countries(Reference Muniz, Madruga and Araújo31,Reference Bai, Wahl and McCluskey33–Reference Lee and Gerrior36) . The higher prevalence in women may be attributed to greater concern with regard to health, a greater adoption of healthy habits(Reference Wardle, Haase and Steptoe37,Reference Hiza, Casavale and Guenther38) and, in part, the greater incidence of osteoporosis(Reference Silva, Cozzolino and S39) compared with men. Indeed, studies report a considerable difference in the prevalence of osteoporosis between the sexes, ranging from 9 to 38 % among women and 1 to 8 % among men(Reference Wade, Strader and Fitzpatrick40).
Frequent milk consumption and low-fat/skimmed milk consumption were higher among individuals who reported consuming whole foods and fruit with greater frequency. Individuals concerned with having a healthy diet prefer consuming foods in natura and minimally processed foods, such as milk, fruit, vegetables, legumes and whole grains, and avoid highly processed products, such as soft drinks, ready-to-heat foods, sweetened beverages and foods rich in fat(Reference Sichieri, Coitinho and Monteiro41,Reference Barreto, Passos and Giatti42) . No previous studies have evaluated the association between the consumption of this type of milk and the frequent consumption of other foods.
The more frequent consumption of milk among older people than adults is in agreement with data reported by other researchers(Reference Muniz, Madruga and Araújo31,Reference Passanha, Garcia and Cervato-Mancuso35) and is partially linked to a generation effect, as older people had less access to sweetened beverages in childhood and milk consumption was more frequent(Reference Muniz, Madruga and Araújo31,Reference Passanha, Garcia and Cervato-Mancuso35) . It has also been reported that older individuals who live alone end up replacing large meals for snacks that usually include the use of milk(Reference Passanha, Garcia and Cervato-Mancuso35) and that problems with chewing, which are more frequent with the advance of the ageing process, lead to an increase in the consumption of pasty foods and liquids, such as milk(Reference Daniel, Cravo, Canesqui and Garcia43).
Among the milk consumers, 81·1 % reported drinking whole milk, which is similar to rates described in previous Brazilian studies(Reference Mallmann, Gentleman and Mello30,Reference Muniz, Madruga and Araújo31,Reference Tombini, Dallacosta and Bleil44) . According to Casarotti et al. (Reference Casarotti and Jorge45), fat is considered a fundamental component for the sensorial aspects of food, enhancing flavour, creaminess, appearance, aroma and the sensation of satiety after consumption. Thus, the greater presence of fat may make whole milk more appreciated than low-fat or skimmed milk(Reference Casarotti and Jorge45).
Dietary guidelines in most countries, including Brazil, counsel adults and older people to consume dairy products with low-fat content(1) due to evidence of an increase in serum cholesterol and the incidence of CVD caused by the consumption of saturated fat(Reference Lawrence10,Reference Hooper, Martin and Abdelhamid11) . Considering the results of the present study, however, this advice is apparently not heeded much, as only 18·4 % of the adults and older people who drank milk consumed low-fat/skimmed milk, which is similar to the rates found in studies conducted in the cities of Pelotas (19·5 %)(Reference Muniz, Madruga and Araújo31) and Palmeira das Missões (13·9 %)(Reference Mallmann, Gentleman and Mello30) in the state of Rio Grande do Sul, Brazil.
Low-fat/skimmed milk consumption was significantly greater among individuals with higher levels of schooling and income, which is similar to data reported in the 2008–2009 Brazilian Family Budget Survey(32) and the study conducted by Muniz et al. (Reference Muniz, Madruga and Araújo31). A better socio-economic status provides greater access to information on healthy eating and the acquisition of differentiated products(Reference Muniz, Madruga and Araújo31).
The increase in low-fat/skimmed milk consumption with the increase in the number of chronic diseases may be the result of the contraindication of whole milk for individuals with CVD as well as the greater use of healthcare services by individuals with a greater number of diseases, which increases opportunities for receiving advice on health and diet(Reference Capilheira and Silva46). In the present study, 68·4 % of the individuals who drank low-fat milk reported having some type of CVD.
Another important finding of the present investigation and one that has been explored little is the fact that low-fat/skimmed milk consumption was not greater among individuals with excess weight. This type of milk was expected to be consumed more among individuals with overweight and obesity, as a balanced diet is a necessary component of weight control, along with low sugar and fat intake(47).
As mentioned in the introduction, recent studies(Reference O’Sullivan, Hafekost and Mitrou17–Reference Bhupathi, Mazariegos and Rodriguez22) have reported that there is no evidence that the saturated fat in milk(Reference O’Sullivan, Hafekost and Mitrou17), intake of whole milk(Reference Talaei, Hosseini and Van Dam18) and intake of dairy products(Reference Alexander, Bylsma and Vargas19–Reference Bhupathi, Mazariegos and Rodriguez22) are risk factors for mortality and for CVD. In fact, some of them have shown that there is evidence of a low protective effect(Reference Alexander, Bylsma and Vargas19–Reference Yu and Hu21).Considering the lack of evidence of fat milk as a risk factor for CVD, it is necessary to evaluate if the recommendations of low-fat/fat-free milk on the dietary guides could be inducing individuals, who prefer whole milk and want to follow the guides, to stop the intake of any kind of milk probably impairing their health.
The prevalence of lactase non-persistence in Brazil is estimated to be 57 % among whites and 80 % in the black population(Reference Mattar, Matins and Carrilho15). However, a large portion of the population of the city of Campinas consumes milk with lactose. Only 0·5 % of consumers drank lactose-free milk and 0·8 % drank soya milk. It should be borne in mind that a lactose intolerant individual can ingest up to 12 g/d (equivalent to one 200-ml glass) of milk without experiencing any symptoms(Reference Vonk, Priebe and Koetse48).
The present study has limitations that should be considered. The questions on food frequency enabled the evaluation of the frequency of consumption but not the amount consumed. In addition, the frequency of intake of other dairy products was not evaluated to ascertain whether even with low milk consumption people could achieve Ca recommendations by frequent intake of other dairy products. However, as mentioned earlier, the consumption of dairy products by the Brazilian population tends to be low(32). All answers were reported by the interviewees and are therefore subject to information bias. Moreover, the cross-sectional design impedes the establishment of causal relations. The importance of the current study resides in the topical nature of the subject and its objective, as milk consumption in adulthood is a controversial issue and there are few studies on the current pattern of milk consumption in different segments of the population.
Conclusion
Despite the high nutritional quality of milk and the different types available on the market aimed at meeting practically all the needs of individuals, an important portion of adults and older people in the population studied does not heed current recommendations regarding milk consumption(25). Less than half of the individuals consume milk five or more times per week and those with this practice had better diet quality and better self-rated health. Although recommended by dietary guidelines in Brazil and other countries, the consumption of low-fat/skimmed milk was low (18·4 %) and was strongly associated with socio-economic status, diet quality and the occurrence of morbidities. The results revealed no difference in the consumption of low-fat/skimmed milk between individuals with ideal weight and those with excess weight. The consumption of lactose-free milk was also low in the population studied. The results indicate the need for the population to be better informed about the nutritional qualities of milk and its health benefits, keeping in mind that there is perhaps evidence that the saturated fat in milk is a risk factor for CVD. Public policies should encourage the consumption of milk, considering its role in metabolism and in the prevention of diseases, such as osteoporosis.
Acknowledgements
Acknowledgements: None. Financial support: The current study was funded by Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP (State of São Paulo Research Assistance Foundation)) and the Brazilian Health Ministry through the Campinas Secretary of Health. The funders had no role in the design, analysis or writing of the article. R.L. received support from the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES (Coordination for the Advancement of Higher Education Personnel)) and M.B.A.B. received a research productivity grant from Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq (National Council of Scientific and Technological Development)). Conflict of interest: The authors declare no conflicts of interest. Authorship: As the first author, R.L. attests that all authors made substantial contributions to the current study. R.L. was responsible for the literature review, data analysis and writing of the manuscript. M.B.A.B. guided the data analysis and contributed to the writing of the manuscript. D.A., S.M.A.D. and A.A.B.F. contributed to the writing of the manuscript. Ethics of human subject participation: The current study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects were approved by the Human Research Ethics Committee of the School of Medical Sciences (certificate number: 1·669·732). Written informed consent was obtained from all subjects.








