Nepal has been recognised as an international leader in advancing the health of children. Nepalese children are among the highest to be fully vaccinated,(1) and the prevalence of childhood night blindness has decreased from 1·4 % in 1989(Reference Khatry, West and Katz2) to 0·27 % in 1998(Reference Gorstein, Shreshtra and Pandey3) due to the National Vitamin A program that was established in 1993. Progress in the nutritional health of Nepalese children has been largely realised from expanded health coverage, particularly in rural areas where Nepal’s large network of female health volunteers have led community-based programmes. Other factors such as an increase in the number of community-based nutrition programs, increased socio-economic mobility and improved sanitation have all synergistically contributed to reduced malnutrition among Nepalese children.
Global goals focused on further improving the nutritional health of children have been established by the Sustainable Development Goals. These target the reduction of stunting by at least 40 % by 2025, wasting to be no higher than 5 % in 2025 and no increase in children with overweight/obesity(Reference Chitekwe, Torlesse and Aguayo4,5) . Nepal has achieved the targeted reduction in stunting by reducing its prevalence from 57 % in 2001 to 25 % in 2022(6). However, additional efforts are needed for Nepal to meet the Sustainable Development Goals for wasting and overweight. The prevalence of wasting has decreased from 11 % in 2001 to 8 % in 2022 and the proportion of children who were overweight increased from 0·7 % in 2001 to 1 % in 2022(6). Thus, the sustained presence of wasting classifies nutritional status among children a high public health priority based upon standards set forth by the WHO(7). At the same time, the increase in overnutrition places excess nutrition as an emerging public health issue. Continued progress will likely require more sophisticated approaches focused on the prevention and management of both undernutrition and overnutrition. To accomplish this, healthcare centres will need dedicated highly skilled and well-trained nutritionists/dieticians.
Kanti Children’s Hospital (KCH) is the only government paediatric hospital in Nepal. In 2020–2021, nearly 60 000 children and adolescents from different territories of Nepal visited the outpatient department and an additional 21 086 received emergency services(8). KCH is among the top three institutions in Nepal providing care to children diagnosed with severe acute malnutrition; however, precise figures are unavailable as national health surveys obtain data at the community level and may not reflect the hospital setting(1,6) .
In 2018, KCH established a collaboration with the International Initiative for Pediatrics and Nutrition, located at Columbia University Irving Medical Center (New York), with the shared objective of advancing the provision and quality of nutritional care and conducting high-quality research in childhood nutrition(Reference Damasco-Avila, Sagastizado and Carrillo9). International Initiative for Pediatrics and Nutrition provides clinician education, clinical infrastructure and mentorship in research to the clinical staff. Prior to the establishment of an expanded nutrition service within the Department of Pediatrics at KCH, it is essential to determine the prevalence of malnutrition, the variety and severity of nutritional conditions and predictors of poor nutrition status so that clinical research programmes may be efficiently designed and implemented. To this end, we report on the nutritional health and predictors of nutritional status in children and adolescents visiting Kanti Children’s Hospital.
Materials and methods
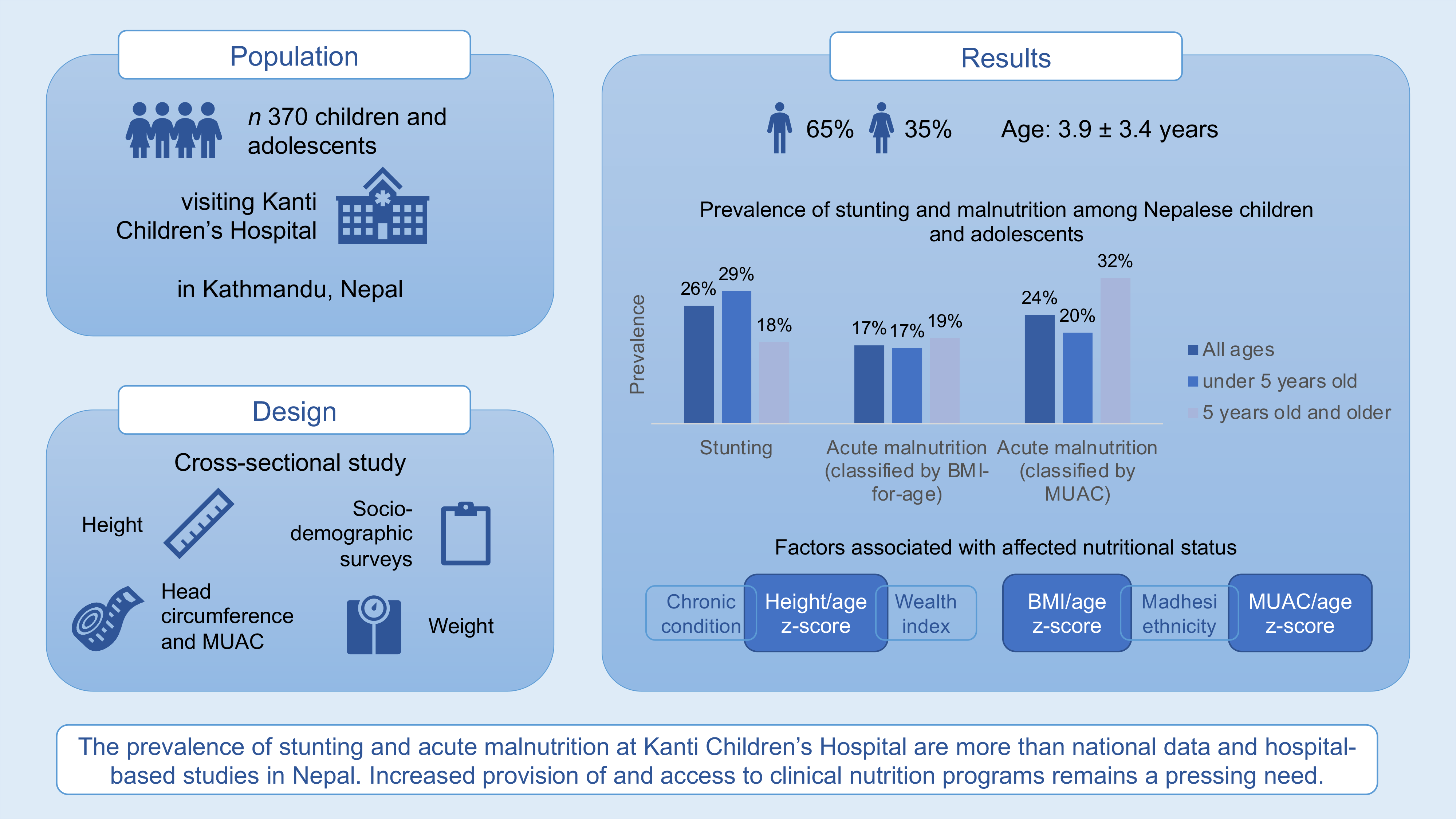
Utilising a cross-sectional design for this pilot study, we recruited children and adolescents aged 0–15 years visiting either the inpatient or outpatient setting at KCH in Kathmandu, Nepal, during a 1-month period (April 2022). After written consent was obtained in the parent’s primary language, nutritional anthropometrics were assessed, and socio-demographic questionnaires were administered. Clinical data (e.g. reason for admission or visit to outpatient clinic) were abstracted from the medical chart. The study was approved by KCH’s Ethical Review Committee (reference number 963).
Socio-demographics
Three questionnaires were utilised to collect information on socio-demographics. To ensure standardisation in the administration of the instruments and ensure representation from illiterate parents/caregivers, questions were read to study participants by the administrants. The WHO’s World Health Survey (2002) collected information on demographic and socio-economic characteristics, including parental education, occupation and self-reported ethnic group(10). The Demographic and Health Wealth Index collected information on the family’s economic status as per previously published methodology(Reference Rutstein and Johnson11). The Demographic and Health consists of questions related to the household’s ownership of assets, such as a refrigerator or bicycle. The Food Insecurity Experience Scale questionnaire collected information on experiences and behaviours related to food access either due to lack of money or other resources, reflecting different levels of food insecurity(Reference Wambogo, Ghattas and Leonard12). The Food Insecurity Experience Scale questionnaire is composed of eight dichotomous (yes or no) questions related to food access over the preceding 12 months. Responses were aggregated with scores ranging from 0 to 8 and classified into three categories based on the global standard: food secure (0 to 3), moderately food insecure (4 to 6) and severely food insecure (7 to 8)(Reference Wambogo, Ghattas and Leonard12).
Nutritional assessment
Anthropometric data were obtained and recorded by a study investigator. Height was measured to the nearest 0·1 cm using a portable stadiometer for children, and weight was measured to the nearest 0·05 kg using a calibrated digital scale. BMI and height Z scores for age and sex were classified based on the WHO standard growth charts(13). A child with a height-for-age Z score of <-2 was classified as stunted(14). A BMI-for-age Z score <-2 indicated wasting and >+2 indicated overweight(14,15) .
Mid-upper arm circumference (MUAC) was measured to the nearest 1 millimeter (mm) using a non-stretch tape around the midpoint between the olecranon process of the ulna and the acromial process of the scapula. For children 6 to 59 months old, a value <125 mm indicated wasting(15). For children 5 years and older, MUAC was classified by Z score with a Z score of <-2 indicating wasting(Reference Mramba, Ngari and Mwangome16). All groups of patients were classified by Z score for regression analysis using WHO reference standards(17) for children less than 5 years old and Mramba et al.(Reference Mramba, Ngari and Mwangome16) reference standards for children 5 years and older.
Head circumference was measured to the nearest 1 mm for all children under 5 years old using a non-stretch tape at the broadest part of the forehead, above the eyebrow and the ears and at the most prominent part of the back of the head. Classification was based on WHO growth reference standards where a Z score <-2 indicated microcephaly(17).
Statistical analysis
Demographic, clinical and nutritional data were input into a REDCap database and summarised using frequencies and proportions for categorical variables. For continuous variables with a normal distribution, mean and SD were reported, and for categorical values, number of patients (n) and percentages were reported. Individual wealth indices were derived utilising a multistep process that has been previously described(Reference Grosh and Glewwe18). Briefly, the dichotomous responses (yes or no) for patients’ assets (electricity, radio, etc.) were transformed into zero if negative or one if positive. Principal component analysis was then performed to obtain the relative contribution of each asset in the model(Reference Rutstein and Johnson11,Reference Khudri, Rhee and Hasan19) . The asset with the largest contribution in differentiating the variance in households’ wealth was considered the first component (PC1). The PC1 value was then multiplied by one for ‘yes’ responses and zero for ‘no’ responses resulting in a summary of the values. Results were then divided in tertiles, and individual scores were classified as Group 1 for scores ≤25th percentile (e.g. lowest wealth), Group 2 for scores >25th to <75th percentile and Group 3 for scores ≥75th percentile (e.g. highest wealth).
For comparison between groups, χ 2 test and multivariate binary logistic regression were used for categorical outcomes (e.g. stunting or healthy height). To investigate whether demographic and socio-economic status were prognostic indicators of nutritional status, groups were divided by age (under 5 years old and 5 years old and older) to align with standard reporting of nutritional indicators in children(20,21) . To determine variables related to the outcome of interest, a stepwise sensitivity analysis was performed. Variables with a significant association (P < 0·05) in a univariate model were included in the multivariate binary logistic regression model, with resulting variables yielding OR and 95 % CI. Statistical significance was set at P < 0·05. Data were analysed using Statistical Package for the Social Sciences (SPSS, version 23.0) and to perform the principal component analysis, PAST4 Software Package for Education and Data Analysis. WHO Anthro (version 2.0) and AnthroPlus (Geneva, Switzerland) software were used to graph nutritional indicators.
Results
Our cross-sectional sample consisted of 370 participants. Similar to regional data(Reference Bennett, Eisele and Keating22,Reference Pokhrel, Snow and Dong23) , 65·1 % were males and represented families from several provinces across Nepal (Table 1, Fig. 1). The mean age of the children was 3·9 years (sd ± 3·4 years). Children were recruited from the outpatient (n 165) and inpatient (n 205) settings. More than half of the participants (n 208) were being treated for an acute condition, while 43·8 % (n 162) were undergoing treatment for a chronic medical condition. The most common acute conditions included fever and pneumonia, while the most common chronic conditions were oncologic/haematologic (n 21), neurologic (n 15) and nephrology (n 10). Almost one-third of families (30·3 %) reported moderate to severe food insecurity and 41·6 % of participants reported affiliation with the Brahmin/Chhetri ethnicity, followed by the Janajati ethnicity (37·4 %) (Table 2).
Table 1 Participant and clinical characteristics

OPD, outpatient department; PICU, paediatric intensive care unit.

Fig. 1 Geographical distribution of participants (n (%))
Table 2 Socio-demographic characteristics

* One patient did not answer the socio-demographic questionnaire.
Nutritional indices
The prevalence of children classified as stunted was 25·9 % (Table 3). The prevalence of stunting was higher among children under 5 years of age (29·2 %) compared with children and adolescents 5 years of age and older (17·9 %; P = 0·026).
Table 3 Distribution of nutritional assessment of the study participants

MUAC, mid-upper arm circumference; NS, not significant; NA, not applicable.
*Forty children under the age of 6 months old; 1 child with no data who is under the age of 4.
†Head circumference for age: Only applicable to children <5 years.
For children under 5 years of age, 16·7 % were classified with wasting according to BMI, whereas 20·2 % were classified with wasting according to MUAC. For children 5 years of age and older, 18·9 % were classified with wasting by BMI, and 32·1 % were classified with wasting by MUAC. A small percentage (2·2 %) of children and adolescents were classified as overweight. No significant differences in excess weight were observed by age groups. The prevalence of microcephaly was 14·8 % and was more prevalent among the Madhesi and Dalit groups with 14·3 % and 40 % (P = 0·002) of children diagnosed with microcephaly, respectively.
To understand the growth of Nepalese children in relation to the WHO growth charts, Z score distributions from our dataset were compared with the WHO reference values (Fig. 2(a–d)). For both height- and BMI-for-age Z scores, the mean Z scores for Nepalese children were below the reference indicators. For both indicators, there was a left shift of the growth curve suggesting that Nepalese children are not developing as per global standards set forth by WHO. We then analysed growth curves by socio-demographic factors. Family self-reported ethnicity revealed poor growth was particularly evident for the Madhesi ethnicity followed by the Dalit ethnicity (see online Supplemental Fig. 1). For all ethnicities, height-for-age Z scores were below global reference values.

Fig. 2 (a-d) Comparison of participants with the WHO child growth reference
Predictors of nutritional status
Univariate analysis revealed a significant association with nutritional status and medical condition (acute v. chronic), ethnicity, wealth index and education; however, no association was observed with food insecurity (see online Supplemental Table 1). Logistic regression analysis was performed to estimate the OR for stunting, wasting (defined by BMI-for-age and MUAC-for-age Z scores) and food insecurity (Table 4).
Table 4 Predictors of nutritional status and food insecurity*

MUAC, mid-upper arm circumference.
* Variables with a significant association (P < 0·05) in the univariate model as predictors of nutritional status and food insecurity were included in the multivariate binary logistic regression model.
Children and adolescents with chronic medical conditions experienced a 2·0 increased odds (95 % CI (1·2, 3·2), P = 0·006) of stunting compared with children and adolescents with acute medical conditions. For children under the age of five, this figure increases to 2·6 (95 % CI (1·5, 4·4), P = 0·002). For wealth, families classified in ≤25th percentile experienced a 2·2 increased odds (95 % CI (1·1, 4·3), P = 0·018) of stunting compared with the reference group (>25th percentile). This was especially apparent for older children who experienced a 19·1 increased odds (95 % CI (1·9, 187·0), P = 0·006) of stunting. Families from the Madhesi ethnic group experienced a 3·3 increased odds (95 % CI (1·5, 7·3), P = 0·003) of wasting by BMI-for-age compared with the reference value. Children and adolescents from the Madhesi ethnic group also experienced a trend towards an increased odds of low MUAC-for-age Z score (OR 2·3, 95 % CI (1·0, 4·8), P = 0·056).
Contrary to the existing literature, there was not an association between nutritional status and food insecurity (see online Supplemental Table 2)(Reference Singh, Singh and Ram24). Logistic regression revealed that children and adolescents in the lowest wealth index category (≤25 percentile) experienced 12·2 increased odds (95 % CI (4·7, 31·6), P < 0·001) of food insecurity compared with the reference group (>25 percentile). Education was also predictive of food insecurity as children from parents with less than primary school education experienced 10·8 (CI (2·4, 49·3), P = 0·001) increased odds of being food insecure as compared with the reference group.
Discussion
Nepal is a low-income country that has achieved significant milestones in advancing children’s health through country-wide supplementation programmes, nutrition programmes and vaccine dissemination. Despite these advances, the prevalence of undernutrition remains high and factors predisposing children to poor nutrition in urban medical centres remain understudied. Our study begins to close this gap in knowledge by investigating the socio-demographic factors that may preemptively identify children who are at elevated risk of poor nutrition. The results from our study may be used to direct resource allocation so that timely and preemptive interventions may reverse or prevent adverse nutritional conditions from developing altogether.
The prevalence of stunting in our sample was 25·9 %. Stunting was higher among younger children compared with older children. Our data are higher than regional data (22 %)(6) and another cross-sectional, hospital-based study (19 %)(Reference Inoue, Dhoubhadel and Shrestha25). This may be reflective economic effects of COVID-19 particularly related to the rising cost of food and supply chain restrictions, but may also be reflective of the socio-demographic characteristics of the children served by this hospital. KCH is a government-supported hospital that provides care for families from a wide range of socio-economic backgrounds and is a preferred facility for the treatment of children from lower socio-economic families. Further, KCH is a regional referral centre for children with the most serious conditions. Our study found that children from the lowest wealth index were at risk for stunting, which is aligned with the findings of other studies in Nepal(Reference Bhusal and Sapkota26,Reference Poudel27) . Children with a chronic condition were at risk for stunting, which may be due to continuous challenges with dietary intake due to the chronic disease itself or alterations in nutrient metabolism as a result of the medical condition. Similar to studies utilising national data(Reference Bhusal and Sapkota26), we found that older age was predictive of stunting, which may be due to a limited number of nutrition rehabilitation programmes in previous years. Children from select ethnicities were at higher risk of stunting and Nepalese children tended to be shorter than norms set by the WHO, possibly due to malnutrition or genetics. Taken together, our data warrant additional research and underscores the importance of routine collection of height for all age groups as systematic monitoring leads to the prevention of stunting from developing altogether among younger age children(Reference Fink, Levenson and Tembo28,Reference Sahu, Rajaa and Vijayageetha29) . As with previous successfully implemented nutrition programmes in Nepal(Reference Chitekwe, Torlesse and Aguayo4), our data suggest that national, multisector initiatives are needed to further achieve reductions in stunting among children and adolescence.
Compared with national data and other hospital-based surveys, we found a higher prevalence of wasting among our sample (8 % and 9·2 % (on admission) v. 17·3 %, respectively)(6,Reference Inoue, Dhoubhadel and Shrestha25) . Several factors may account for this discrepancy. First, the children in our study represent children suffering from either an acute or chronic medical condition, both of which can cause wasting. Additionally, KCH serves as a national referral hospital especially for children with severe disease, refractory conditions or rare diseases. Thus, the children served by KCH may be especially vulnerable to wasting due to the complexity of their condition. Additionally, the majority of children were from middle to low socio-economic families. Similar to our finding among children with stunting, ethnicity was also predictive of wasting. We also found that growth differed by ethnicity as illustrated from comparisons to the WHO growth standards. Despite these variations, our data confirm that wasting remains alarmingly high, as defined by global standards(7), among Nepalese children in the hospital setting and comprehensive nutritional programmes fostering the prompt delivery of nutritional care are urgently needed.
Of notable concern, we observed a high prevalence of stunting and wasting among children 5 years of age and older. Global age limitations in access to nutritional rehabilitation products and national nutritional policies focused on children under 5 years of age may be contributing factors. The repercussions of undernutrition in children beyond the age of five are not inconsequential as poor body image, reduced work and learning capacity and poor reproductive health in adolescence have been reported(30,Reference Deshpande and Ramachandran31) . Unfortunately, existing policies continue to focus on children under 5 years of age and adolescent girls(32,33) . Our findings suggest a re-evaluation of current nutritional programmes to ensure adequate provision of nutritional care for older children.
Our results align with previous data in that the use of BMI alone in children and adolescents is not a comprehensive indicator of nutritional status(Reference Mramba, Ngari and Mwangome16,Reference Miller, Mallory and Escobedo34) . There are well-established limitations of the use of BMI alone for classifying nutritional status, and several research groups have underscored the importance, ease of use and low cost of utilising MUAC in the paediatric setting(Reference Miller, Mallory and Escobedo34,Reference Roy and Sekher35) . Our study found that the classification of wasting using BMI-for-age z-score and MUAC among children under the age of five was inconsistent. These results were expected and further highlight the importance of including assessment of height, weight and MUAC in paediatric nutritional assessments(Reference Mramba, Ngari and Mwangome16,Reference Miller, Mallory and Escobedo34) .
Our data revealed that the percentage of children classified as overweight is higher in our study compared with national data, 2·7 % compared with 1 %, respectively(6). However, these figures must be considered recognising that the majority of our population resides in an urban setting. While these numbers remain relatively low compared with surrounding countries, our data suggest that overweight is increasing among Nepalese children and could emerge as a public health crisis in the upcoming years. Importantly, our data advocate for Health Ministries, clinicians and clinical investigators to establish public health programmes targeting the prevention of obesity with the objective of attenuating the rise in overweight status, an objective aligned with the Sustainable Development Goals.
The prevalence of microcephaly was 14·8 %, which is lower than previously reported (24–56 %)(Reference Miller, Joshi and Lohani36,Reference Miller, Neupane and Joshi37) . Head circumference has been shown to vary by ethnic group with it most commonly observed among the Dalit ethnicity(Reference Malla, Mall and Rao38), which we also observed. The lower prevalence may be due to the small representation among our participants. National data suggest that Dalits have consistently poor performance in regard to neonatal and childhood mortality, maternal health service utilisation, childhood nutritional status, wealth index and education(Reference Pandey, Dhakal and Karki39,Reference Bennett, Dahal and Govindasamy40) . Other studies have found that microcephaly is associated with stunting and lower socio-economic status(Reference Sindhu, Ramamurthy and Ramanujam41). The association between microcephaly and socio-economic status may be explained by the high presence of maternal undernutrition in impoverished communities contributing to prenatal nutritional deprivation(Reference Sindhu, Ramamurthy and Ramanujam41). Taken together, specific programmes that reach out to the most underserved and economically disadvantaged groups are needed to close the remaining gaps in maternal and childhood undernutrition in Nepal.
Our study identified several risk factors for undernutrition. Contrary to our expectations, food insecurity, wealth and education were not consistently associated with all nutritional indicators, perhaps due to children in our study already seeking medical care. Our insignificant findings may also be related to the small sample size and limited representation of ‘at-risk’ groups. We found that the prevalence of wasting was high among the Madhesi ethnicity, which has been reported in other studies in Nepal(Reference Ghimire, Aryal and Gupta42). This was an expected finding given that national surveys have demonstrated differences among ethnic groups in terms of health service utilisation and health outcomes in Nepal, where underprivileged groups, such as the Madhesi group, fare far worse than more privileged groups(Reference Pandey, Dhakal and Karki39).
Aligned with previous studies(Reference Osei, Pandey and Spiro43–Reference Saaka and Osman45), we found that a large percentage of children with wasting also report moderate to severe food insecurity (60·9 %) despite the results not reaching statistical significance. Our findings may be explained by the majority of families reporting food security or the reallocation of resources to young children when food is scarce(Reference Saaka and Osman45). Studies have shown that households reallocate food to prioritise feeding young children during periods of food insecurity(Reference Leonard46). Other factors may have a stronger effect on malnutrition such as substantial improvements in access to health and nutrition services, household wealth and parental education(Reference Chitekwe, Torlesse and Aguayo4). The association between parental education and nutritional status was only significant when assessed by MUAC, perhaps due to MUAC being a more sensitive indicator of wasting, especially in the setting of disease(Reference Phong, Taylor and Robinson47,Reference Modi, Nasrin and Hawes48) . Parental education has been associated with wasting in other studies in Nepal and elsewhere(Reference Bhusal, Bhattarai and Chhetri49,Reference Akombi, Agho and Merom50) , as mothers who are less educated have been shown to have the poorest child feeding practices(Reference Chitekwe, Torlesse and Aguayo4). With this finding, focused interventions aimed at strengthening maternal education may be drawn.
Our results must be interpreted in light of several limitations. First, this was a single-institution study located in the populous Bagmati province and may not be reflective of other national hospitals within or outside of this province. Our study collected data over a single month and variations in nutritional status over time (e.g. summer v. winter months) was not obtained. Due to personnel limitations, several outpatient clinics were not included in the study including the psychiatric department, burn unit and neonatal intensive care unit. Children from the inpatient setting were recruited at any point during their hospital admission; therefore, duration of hospital stay was also not collected. Finally, we were limited in our analyses due to the relatively small sample size. Our pilot study aimed to establish an initial snapshot of nutritional morbidities in the largest, government-supported children’s hospital in the country and was not intended to establish country-wide indicators on the nutritional health of children in Nepal. Future research, within the context of a clinical research program, is in development at KCH to examine these nutritional conditions prospectively.
Hospital-based nutrition programmes improve the nutritional status of children(Reference De Longueville, Robert and Debande51). However, challenges with adequate resources, particularly in countries with a large youth such as Nepal, is a challenge for the medical field until capacity and skills are further cultivated to meet the need. As KCH and International Initiative for Pediatrics and Nutrition advance their collaboration, several recommendations may be drawn from our study to guide the development of our collaborative hospital-based nutrition programme. First, utilising both MUAC and BMI-for-age to identify wasting is essential due to the limitations of BMI-for-age. Nutritional programmes need to be designed to meet the needs of children of all ages and likely prioritise children with chronic medical conditions as these often require consistent parental education and ongoing monitoring. Nutrition education may be a low-cost intervention for disadvantaged families and may aid in the prevention of all forms of malnutrition(52). Finally, collaboration and referral to community-based nutrition programmes is likely essential to sustain and build upon progress obtained in the hospital.
Acknowledgements
The authors would like to thank the nurses at Kanti Children’s Hospital and volunteers who assisted in data collection. The authors would also like to thank the patients and families of Kanti Children’s Hospital for participating in the study.
Financial support
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Conflicts of interest
There are no conflicts of interest.
Authorship
R.H.C., B.G., J.D. and E.J.D. contributed to formulating the research question. R.H.C., B.G., J.D., M.W., E.D. and E.J.D. contributed to designing the study. T.B., J.D., M.W., K.L. and A.A. contributed to data collection. E.D. and J.B. contributed to data analysis. All authors contributed to interpreting the results, drafting the manuscript and approving the final manuscript.
Ethics of human subject participation
This study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving research study participants were approved by the Ethical Review Committee of Kanti Children’s Hospital. Written informed consent was obtained from all subjects/patients.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S136898002300188X