Asia has an estimated 4·7 million people living with HIV, of whom half are in India( 1 ). Nearly 21 000 children are newly infected in Asia every year( 1 ). Malnutrition has been reported to be the most common manifestation of HIV( Reference Merchant, Oswal and Bhagwat 2 , Reference Shah, Tullu and Karnat 3 ). A strong correlation exists between HIV and malnutrition( Reference Angami, Reddy and Singh 4 , 5 ). A study from Imphal reported 21·7 % of malnourished children to be infected with HIV( Reference Angami, Reddy and Singh 4 ). In fact, malnutrition has become a leading cause of morbidity and mortality in HIV-infected children( Reference Fergusson, Chinkumbha and Eternod 6 , Reference Padmapriyadarsini, Pooranagangadevi and Chandrasekaran 7 ). Multiple factors imply the presence of malnutrition in HIV, including anorexia, malabsorption, frequent secondary infections and increased energy requirements( Reference Piwoz 8 ).
Although there are studies available from southern India that show malnutrition among HIV-infected children( Reference Padmapriyadarsini, Pooranagangadevi and Chandrasekaran 7 , Reference Shet, Mehta and Rajagopalan 9 ), data are grossly lacking from other parts of the country. Moreover, data regarding the effect of antiretroviral therapy (ART) on the nutritional status of Indian children are limited.
Hence, a retrospective study was conducted in a tertiary care hospital in north India to evaluate the clinico-immunological, nutritional and growth characteristics of HIV-infected children and to study the impact of ART on these parameters.
Methodology
The present study involved a retrospective case review of HIV-infected children attending the paediatric ART clinic of a tertiary care hospital in Delhi since the establishment of the centre in March 2006 until June 2010. The study population included HIV-positive children aged 0–12 years. Data regarding demographic, immunological and clinical profiles were noted from the medical records using a standardized questionnaire. Clinical and immunological profiles were analysed as per WHO guidelines( 10 ). Although the caregivers of all children were counselled nutritionally in terms of energy and protein requirements, nutritional supplementation was not provided to any child. The energy and protein requirements as well as availability of food for each child were assessed by the nutritional counsellor of the ART centre of the hospital. Counselling was done at every visit and patients were explained the nature and amount of food products that would be appropriate for their energy and protein requirements. Children not getting adequate support from their families were offered help from non-governmental organizations, but ensuring that no nutritional supplementation was given.
Weight was recorded using standardized calibrated weighing scales and height/length measured using a stadiometer/infantometer. The patients were further classified according the type of malnutrition using their records and definitions in the WHO( 11 ) and US Centers for Disease Control and Prevention (CDC)( 12 ) guidelines. For children aged ≤5 years, wasting and stunting were defined as moderate or severe based on Z-score, consequently categorized as moderate or severe malnutrition as defined by WHO( 11 ). Children >5 years of age were categorized as underweight if BMI was <5th centile and of short stature if height-for-age was <5th centile as per CDC guidelines. ART, including two nucleoside reverse transcriptase inhibitors (NRTI) plus one non-nucleoside reverse transcriptase inhibitor (NNRTI), was started as per guidelines of the National AIDS Control Organization( 13 ). In the NRTI group, stavudine and lamuvudine were given twice daily; in the NNRTI group, nevirapine was the preferred drug, given as a single dose in the first two weeks followed by twice daily. In cases of severe side-effects or any absolute or relative contraindications, alternative drugs were started as per National AIDS Control Organization guidelines( 13 ). The records were then followed up to look for the variation in nutritional status noted in those started on ART. Children with less than 1 year of follow-up on ART were excluded from the study.
Results
A total of 130 patients were registered over 4 years of which ninety were on regular follow-up. Of the total population, eighty-five were males and remaining the forty-five were females. ART was started in forty patients during this period based on the immunological and clinical classification.
Of the 130 patients registered (Fig. 1), fifty-four children (41·5 %) were ≤5 years of age. Of these, twenty-three (42·5 %) children were stunted and seven (12·9 %) were wasted. In total, twenty-four of fifty-four children (44·4 %) were malnourished, which included those with moderate as well as severe malnutrition. In the age group of >5 years which had a total of seventy-six children, thirty (39·4 %) were underweight (BMI < 5th centile) and thirty-one (40·7 %) were categorized as having short stature (height-for-age < 5th centile).
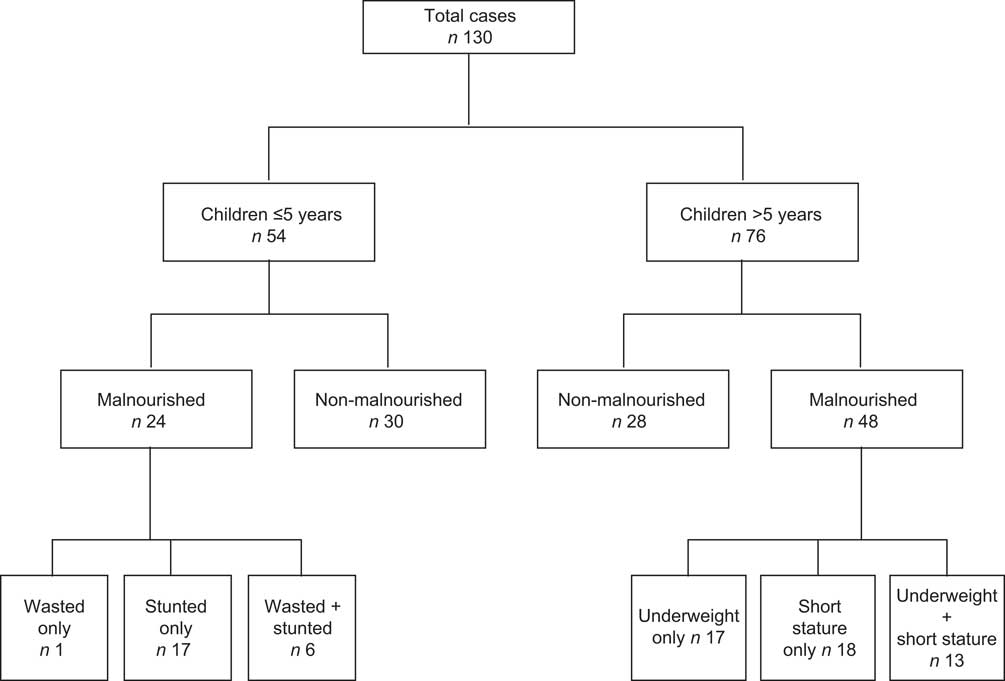
Fig. 1 Flowchart showing distribution of children's nutritional status during the study period
Data on the clinical profile of the 130 children at the time of enrollment showed that the majority of them presented to us in clinical stage 1 as per WHO staging( Reference Shet, Mehta and Rajagopalan 9 ) (Table 1), as most children (60·0 %) were asymptomatic at presentation. Diarrhoea was the most common presentation in symptomatic children. A total of forty children were started on ART, of whom thirty-nine were malnourished and one was not. In children ≤5 years of age, two children in the severe malnutrition group and two in the moderate malnutrition group required ART. Improvement in nutritional status was observed in three out of the four children started on ART, all within 1 year of therapy. Stunting, on the contrary, persisted in all four malnourished patients aged ≤5 years receiving ART, although one patient did show improvement in severity of stunting after 2 years of follow-up.
Table 1 Clinical staging of the study population: HIV-positive children aged 0–12 years, Delhi, India
The data revealed that among the thirty underweight children in the age group >5 years, eighteen children were started on ART. Of these, eight showed an improvement and attained BMI > 5th centile after an average follow-up of 1·5 years, nine children continued to be in the same BMI centile and one was excluded as his follow-up duration was less than 1 year. Out of thirty-one children who were classified as short stature, twenty-one required ART. Eighteen children were followed up and three were excluded due to short follow-up period of less than 1 year. The height-for-age of all eighteen children continued to remain below the 5th centile.
In the clinical staging of the forty children started on ART (Tables 2 and 3), 18/40 (45·0 %) children were in clinical stage 3. Immunologically, 35·0 % children (14/40) had severe immunodeficiency. During follow-up ranging from 1 to 4 years, twenty-seven children (67·5 %) showed improvement in clinical stage, all within 1 year of therapy, eight children remained in the same clinical stage, one showed worsening of the clinical status, three were excluded from the study and one was lost to follow-up. Immunologically, twenty-five children (62·5 %) improved and showed a rise in CD4 count, nine continued to be in the same immunological stage, two showed a fall in CD4 levels, three were excluded and one patient was lost to follow-up. Of the two children who showed immunological deterioration, one showed worsening of clinical status as well and persisted to remain underweight and short stature. The other child, although showing clinical improvement after 1 year of treatment, did not show any improvement in anthropometric parameters.
Table 2 Clinical staging of the population started on antiretroviral therapy: HIV-positive children aged 0–12 years, Delhi, India
Table 3 Immunological staging of the population started on antiretroviral therapy: HIV-positive children aged 0–12 years, Delhi, India
Discussion
Results showed that about 40 % of our population of HIV-positive children in age groups ≤5 years and >5 years had stunting and short stature, respectively; these values can be compared with those in two separate studies on HIV-positive children conducted in south India, which showed a prevalence of 58 %( Reference Padmapriyadarsini, Pooranagangadevi and Chandrasekaran 7 ) and 46 %( Reference Shet, Mehta and Rajagopalan 9 ) for stunting. Similarly, the percentage of wasting in our population was 12·9 % whereas data from south India reported 34 %( Reference Padmapriyadarsini, Pooranagangadevi and Chandrasekaran 7 ) and 16 %( Reference Shet, Mehta and Rajagopalan 9 ) in the two studies. Although this difference may not be statistically significant because of the small sample size, the variation in results should be evaluated in terms of the general living conditions, socio-economic status, feeding practices, immunization status and prevalence of communicable infections in various states. An important factor that could be responsible for the slightly better results in Delhi was the nutritional counselling done at our centre, starting from the antenatal period by the nutritionist, and the support provided by members of the various non-governmental organizations associated with the centre.
The percentage of wasting in our population was 12·9 %, whereas that of underweight was 39·4 %. The proportion of children who were underweight was about three times greater than the proportion with wasting, possibly because of the progressive weakening of the immune system leading to intercurrent infections and higher chances of weight loss. The normal Indian population has 48 % stunting and 20 % wasting in the under-5s age group( Reference Arnold, Parasuraman and Arokiasamy 14 ). The difference in the percentage of wasting compared with the national figure in our children aged ≤5 years could be due to the smaller sample size.
When we followed up the malnourished patients who were started on ART, we noted a similar pattern of response in both age groups. For children ≤5 years of age, wasting improved, but stunting persisted. Similarly in those aged >5 years underweight showed an improvement of nearly 50 %, but short stature persisted in all. This shows that the acute insult from HIV infection had slowed down, but the chronic damage continued. Whether this effect occurs with nutritional supplementation alone is not known. As we have already seen that nutritional counselling is implicated as one possible factor for the lower rates of stunting and wasting in Delhi, it becomes essential to study the role of nutritional supplementation in these children. The major limitation of our study remains that only four children in the ≤5 years age group and thirty-six children in the >5 years age group could be started on ART and assessed for the response to therapy. Hence, a larger trial is needed to further support the above findings.
The study also sought to identify the common clinical feature in HIV-positive children. Malnutrition was the most common clinical feature on examination, although the clinical presentation with which maximum symptomatic children presented to the centre was diarrhoea. Some 60 % of the children were asymptomatic at presentation. This was probably because of early registration of children of HIV-positive parents. This mobilization has largely been brought by the associated non-governmental organizations which routinely counsel parents for an early visit, both for their own well-being and their baby's.
As already mentioned, a study from Imphal reported 21·7 % of malnourished children to be infected with HIV, but similar data are not available from other states. We could not extrapolate their finding for the rest of the country but, knowing their results, we feel it is essential to study the prevalence of HIV in malnourished children as the latter is one of the leading causes of morbidity and mortality in these children( Reference Fergusson, Chinkumbha and Eternod 6 , Reference Padmapriyadarsini, Pooranagangadevi and Chandrasekaran 7 ).
We observed that nearly 70 % of the population started on ART showed a clinical improvement on first-line drugs and about 60 % showed immunological improvement. Knowing the rising trend of resistance to first-line drugs and use of second-line drugs in adults( 15 ), it was important to assess the success rate of first-line drugs in children.
Conclusion
In the present population of HIV-positive children, giving ART restored immune system function to the extent that the incidence of acute infections decreased; hence an improvement was seen in the children's clinical status and short-term parameters of nutritional status, but the chronic insult continued to persist. We also found first-line ART to be effective in the majority of our HIV-positive children.
Acknowledgements
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors. There are conflicts of interest. N.C. collected the data and wrote the initial manuscript; S.G. designed the study; S.G. and M.N. searched the literature and critically analysed the manuscript. All authors approved the final manuscript.






