An estimated 22·5 million adults and children were living with HIV/AIDS in sub-Saharan Africa in 2009(1). Access to triple combination antiretroviral therapy (ART) has led to significant decreases in morbidity and mortality(Reference Hogg, Heath and Yip2–Reference Lima, Hogg and Harrigan4). On the basis of the new WHO criterion for treatment initiation (CD4 cell count: ≤350 cells/mm3), ART was accessed by an estimated 37 % of sub-Saharan Africans in need of ART by the end of 2009(5). The United Nations Food and Agriculture Organization estimates that 239 million people were chronically undernourished in sub-Saharan Africa in 2010(6). A significant proportion of people living with HIV/AIDS in the region are simultaneously affected by nutritional deficiencies(7). The WHO classifies nutritional status by BMI as mild (BMI = 17·00–18·49 kg/m2), moderate (BMI = 16·00–16·90 kg/m2) or severe (BMI < 16·00 kg/m2, bilateral pitting oedema)(8). Cross-national population-based data suggest that the prevalence of mild and moderate malnutrition among adults living with HIV/AIDS is 15·4 % and 10·3 %, respectively, in sub-Saharan Africa(Reference Ahoua, Umutoni and Huerga9, Reference Uthman10), and is also elevated among young children living in AIDS-affected households(Reference Magadi11).
The disproportionate burden of HIV/AIDS and nutritional deficiencies in sub-Saharan Africa is of particular concern as each condition may perpetuate and aggravate the severity of the other(Reference Gillespie and Kadiyala12). HIV/AIDS affects people during the most productive years of their life, resulting in decreased household economic capacity and agricultural output and increased caregiver burden(Reference Bukusuba, Kikafunda and Whitehead13). HIV infection may worsen nutritional status or compound pre-existing malnutrition by increasing an individual's metabolic rate and resting energy expenditure(14–Reference Salomon, de Truchis and Melchior16) and by reducing one's ability to effectively absorb and utilize nutrients(Reference Salomon, de Truchis and Melchior16–Reference Mangili, Murman and Zampini18). Conversely, nutritional deficiencies have been shown to result in poorer clinical outcomes among HIV-infected individuals, including those on ART, in both high- and low-resource settings(Reference Grinspoon and Mulligan19). Compliance with dietary requirements has been shown to be important for the absorption of certain antiretroviral drugs(Reference Boffito, Acosta and Burger20). Demands of food costs have been cited as barriers to ART uptake in Africa(Reference Mshana, Wamoyi and Busza21, Reference Tuller, Bangsberg and Senkungu22). Among individuals receiving ART, food insecurity and poor nutritional status have been associated with decreased adherence to ART(Reference Au, Kayitenkore and Shutes23–Reference Weiser, Fernandes and Anema25), reduced CD4 cell count and incomplete HIV RNA suppression in marginalized urban populations of high-resource countries(Reference Sanjobo, Frich and Fretheim24, Reference Normén, Chan and Braitstein26–Reference Weiser, Bangsberg and Kegeles28). Food insecurity among individuals on ART has been additionally associated with poorer survival, even when controlling for ART medication adherence(Reference Weiser, Fernandes and Brandson29). Several Africa-based studies have found that low BMI and severe anaemia are independently associated with increased risk of mortality within the first 3 months of ART among adults and children alike(Reference Stringer, Zulu and Levy30–Reference Johannessen, Naman and Ngowi32).
In order to mitigate the adverse effects of food insecurity on HIV outcomes, international organizations such as the WHO, the Joint United Nations Programme on HIV/AIDS, the World Food Program (WFP) and major HIV initiatives such as the US President's Emergency Plan for AIDS Relief (PEPFAR) recommend the integration of nutritional support services, specifically nutrition assessment, education and counselling, into HIV/AIDS treatment and care programmes, with PEPFAR allocating $US 130 million to support the integration of HIV and nutritional support services in 2010(7, 15, 33–36). Since 2006, PEPFAR implementation guidelines have recommended the provision of nutritional evaluation and food support to all orphans and vulnerable children, to HIV-positive pregnant and lactating women and to all adults receiving ART with clinically defined malnutrition. However, little is known about the extent to which nutritional support services are available in HIV care and treatment programmes across sub-Saharan Africa.
We describe here the reported availability of different types of nutritional support services in a sample of 336 HIV care and treatment sites in nine sub-Saharan African countries, as well as correlates of their availability and changes in reported availability over time.
Methods
The present study involved 336 HIV care and treatment sites from nine sub-Saharan African countries (Kenya, Tanzania, Ethiopia, Rwanda, Mozambique, South Africa, Nigeria, Lesotho and Cote d'Ivoire) that were receiving technical support from the International Center for AIDS Care and Treatment Programs (ICAP; www.columbia-icap.org) at Columbia University's Mailman School of Public Health.
Programme and facility characteristics
Data on programme-level characteristics were gathered through routinely conducted, structured site assessments completed by ICAP field staff. Programme and Facility Characteristics Tracking System (PFaCTS) assessments capture information through interviews with facility staff regarding: the type of facility (primary, secondary or tertiary), availability of other HIV-related services (e.g. prevention of mother to child transmission programme, voluntary counselling and testing (VCT), tuberculosis treatment), ancillary patient support services (e.g. peer education, outreach for patients who miss clinic visits, nutrition or food support), laboratory services (e.g. availability of CD4 testing) and staffing characteristics (e.g. number or type of providers). Three rounds of site assessments had been conducted at the time of interview (January 2007, July 2007 and July 2008). Reliability of survey responses between rounds was assessed for 305 sites and was found to be 91 % overall and 89 % for the nutrition-related questions. Test–retest agreement was recently assessed at fifty-eight ICAP-supported sites in seven of the nine countries included in the present analysis by comparing survey responses with those assessed through repeat survey administration by a supervisory team. For the thirty-one questions that were assessed, agreement between the two methods was 83 % overall and 75 % for the nutrition-related questions that were assessed.
The PFaCTS survey prompted facility staff to report on the availability of nutritional evaluation (measurement of height and weight), nutritional counselling, micronutrient supplementation, treatment for severe malnutrition in adults and children, and food rations. Clinical admission into supplementary and therapeutic feeding programmes to treat moderate and severe acute malnutrition, respectively, is determined by national guidelines or WHO cut-off points(33).
Inclusion criteria and survey response rate
Our sample included a total of 336 (96 %) of the 351 ICAP-supported HIV care and treatment sites that completed at least one PFaCTS survey by July 2008. Fifteen sites were not included in our analysis because of incomplete data or information. Among the 336 sites included in our analysis, 174 sites had completed all three survey rounds (January 2007, July 2007 and July 2008).
Statistical analyses
Bivariate analysis
In order to assess the site-level correlates of each type of nutritional support service, we conducted four separate bivariate analyses that focused on the reported availability of the following nutritional support services: (i) nutritional counselling (including general nutritional counselling for adults and infant feeding counselling for mothers); (ii) micronutrient supplementation (including multivitamin with or without mineral supplements, Fe supplements and vitamin A); (iii) treatment for severe malnutrition (including treatment of adults and children under 5 years of age); and (iv) food rations (including rations intended to promote adherence and household food security for adults and children). We examined correlates of the reported availability of each type of nutritional support service using the most recent survey data (July 2008) in relation to the following site-level covariates: time since the site's start of ART service provision (≤2 v. >2 years before the survey); the cumulative number of individuals who had initiated ART by the time of the survey (dichotomized at the median of 260 patients); site location (rural v. urban); type of site (primary v. secondary or tertiary); reported presence of nutritionist on site (yes v. no); and reported availability of weight-for-height assessments (yes v. no).
Multivariate analysis
Multivariate logistic regression analyses were conducted to determine independent predictors of reported availability of each of the above-mentioned four nutritional support services. Variables with P values <0·2 in the bivariate analysis were included in the multivariate model. Thereafter, a backward selection procedure based on the Akaike Information Criterion was used to determine the final multivariate model(Reference Lachin37). Model fit was assessed using the Hosmer–Lemeshow statistic for determining goodness of fit(Reference Hosmer and Lemeshow38). Categorical explanatory variables were analysed using Pearson's χ 2 and Fisher's exact tests and continuous variables were analysed using the Wilcoxon rank-sum test. All statistical analyses were performed using the SAS statistical software package version 9·1 (SAS Institute, Cary, NC, USA). All tests of significance were two-sided, with a cut-off P value of 0·05 used to designate a statistically significant association.
Time-trend analysis
For the 174 sites for which three survey rounds had been completed, we examined changes in the reported availability of nutritional support services over the three time points during an 18-month period from January 2007 to July 2008. We assessed the prevalence of reported availability of each type of nutritional support service at each of the three survey time points (January 2007, July 2007 and July 2008). Statistical significance of changes in the prevalence of each type of service was assessed using the Cochran–Armitage trend test.
Results
Table 1 describes the location, site characteristics and prevalence of the reported availability of nutritional support services in the sample of 336 HIV care and treatment sites in the nine sub-Saharan African countries. Of these, 185 (55 %) were situated in urban areas and 151 (45 %) in rural areas. By July 2008, these sites had cumulatively enrolled 467 175 patients in HIV care and treatment (including 40 430 (9 %) children and 429 745 adults (91 %)), of whom 210 019 individuals (45 %) had initiated ART (including 16 507 (8 %) children and 193 512 (92 %) adults). Of the 336 sites surveyed, 303 (90 %) reported the availability of at least one form of nutritional support service.
Table 1 Enrolment, clinical characteristics and location and prevalence of nutritional support service availability in 336 HIV care and treatment sites in sub-Saharan Africa, July 2008
ART, antiretroviral therapy.
*Denominator used: 303.
Among the 303 HIV care and treatment sites for which at least one form of nutritional support service was available, 140 (46 %) were primary care sites, 152 (50 %) were secondary care sites and eleven (4 %) were tertiary care sites; twenty-one sites (7 %) had a nutritionist onsite and weight-for-height evaluation was available at 282 (93 %) sites. Among these 303 HIV care and treatment sites, the extent of availability of specific nutritional support services varied substantially (Fig. 1). Nutritional counselling was reported to be available at 98 % of sites (range across countries (RAC): 94–100 %). Nutritional counselling for adults was reported to be available at 95 % of sites (RAC: 75–100 %) and infant feeding counselling for mothers with infants at 91 % (RAC: 81–100 %) of sites. Micronutrient supplementation was reported to be available at 64 % of sites (RAC: 2–100 %) and multivitamin and mineral supplementation at 25 % (RAC: 0–97 %) of sites. Vitamin A supplementation to infants, postpartum women and other adults/non-infant children was reported to be available at 52 % (RAC: 2–89 %), 41 % (RAC: 0–77 %) and 19 % (RAC: 0–58 %) of sites, respectively, and Fe supplementation was reported to be available at 47 % (RAC: 0–89 %) of sites. Treatment for severe malnutrition was reported to be available at 36 % of sites (RAC: 0–72 %). Treatment for severely malnourished adults was reported to be available at 23 % (RAC: 0–72 %) of sites and services for infants and children aged <5 years were available at 33 % (RAC: 0–69 %) of sites. Food rations were reported to be available at 31 % (RAC: 2–97 %) of sites, including rations for adults to promote medication adherence and household food security at 18 % (RAC: 0–87 %) and 4 % (RAC: 0–13 %) of sites, respectively. Food rations were reported to be available for children aged <5 years to promote medication adherence and household food security at 13 % (RAC: 0–77 %) and 7 % (RAC: 0–22 %) of sites, respectively.
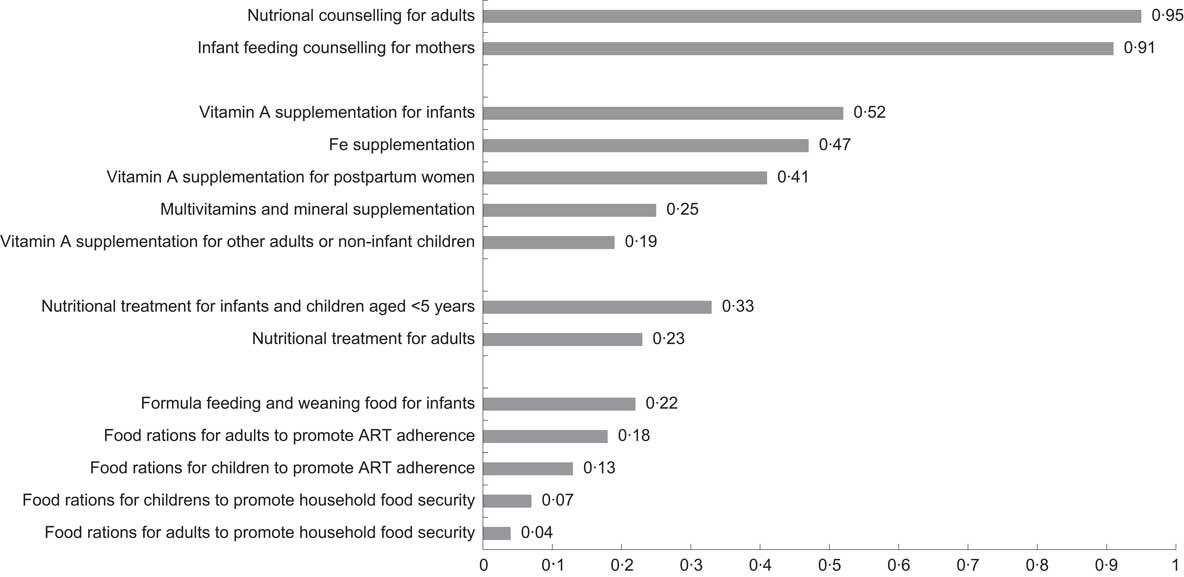
Fig. 1 Prevalence of nutritional support services available in 303 HIV care and treatment sites in nine sub-Saharan African countries, July 2008 (ART, antiretroviral therapy)
In bivariate analysis (Table 2), nutritional counselling was more commonly reported to be available at secondary or tertiary care sites compared with primary care sites (93 % v. 85 %, P = 0·026) and at sites where weight-for-height evaluation was available (98 % v. 39 %, P < 0·001). Micronutrient supplementation was more commonly reported to be available in rural compared with urban sites (65 % v. 52 %, P < 0·016) and at sites where weight-for-height evaluation was available (65 % v. 17 %, P < 0·001). Treatment for severe malnutrition was more commonly reported to be available at sites providing ART services for over 2 years (50 % v. 21 %, P < 0·001), at sites that reported a nutritionist on staff (57 % v. 31 %, P = 0·013) and at sites where weight-for-height evaluation was reported to be available (38 % v. 4 %, P < 0·001). The reported availability of food rations was higher at sites providing ART for at least 2 years (45 % v. 18 %, P < 0·001) and at sites where weight-for-height evaluation was reported to be available (33 % v. 2 %, P < 0·001).
Table 2 Bivariate analysis of factors associated with availability of nutritional counselling, micronutrient supplementation, treatment for severe malnutrition and food rations to people living with HIV/AIDS in HIV care and treatment sites in nine sub-Saharan African countries, July 2008 (n 336)
ART, antiretroviral therapy.
In multivariate analysis (Table 3), secondary or tertiary care sites were associated with a higher odds of nutritional counselling availability (adjusted OR (AOR) AORsecondary/tertiary v . primary: 2·2, 95 % CI 1·1, 4·5). Rural sites (AORrural v . urban: 2·3, 95 % CI 1·4, 3·8) and sites where weight-for-height evaluation was available (AORweight-for-height v . none: 11·0, 95 % CI 5·0, 24·0) reported higher odds of micronutrient supplementation availability. Sites that had provided ART for at least 2 years had a higher odds of having treatment for severe malnutrition (AOR≥2 years v . <2 years: 2·4, 95 % CI 1·4, 4·1). Sites that had provided ART for a minimum of 2 years (AOR≥2 years v . <2 years: 1·6, 95 % CI 1·3, 1·9) and rural sites (AORrural v . urban: 2·4, 95 % CI 1·4, 4·4) had greater odds of reported availability of food rations.
Table 3 Multivariate analysis of factors associated with availability of nutritional counselling, micronutrient supplementation, treatment for severe malnutrition and food rations to people living with HIV/AIDS in HIV care and treatment sites in nine sub-Saharan African countries, July 2008
ART, antiretroviral therapy.
Of the 336 sites, 174 (52 %) had information available from the three consecutive PFaCTS surveys (January 2007, July 2007 and July 2008) and were included in the time-trend analysis. Over the 18-month period, micronutrient supplementation and treatment for severe malnutrition became increasingly more common. The percentage of sites with availability of micronutrient supplementation increased from 19 % in January 2007 to 56 % in July 2008 (P < 0·001). Similarly, the percentage of sites with availability of treatment for severely malnourished individuals also increased significantly (from 24 % in January 2007 to 40 % in July 2008, P = 0·001). No significant trend was detected in the availability of nutritional counselling (P = 0·86) or food rations (P = 0·08), although the prevalence of the former was already high (87 %) in January 2007. In order to verify that no bias resulted from the exclusion of sites without three consecutive surveys, we re-ran the time-trend analysis including all sites. This analysis similarly found a significant increase in the availabilities of micronutrient supplementation (P < 0·001) and treatment for severe malnutrition (P = 0·006) and no significant trend for other nutritional support services.
Discussion
This investigation evaluated the prevalence and correlates of the reported availability of different types of nutritional support services in HIV care and treatment sites in multiple sub-Saharan African countries. Ninety per cent of sites had at least one form of nutritional support service. However, the type of nutritional support services reported to be available varied substantially, including by country, geographical context (urban/rural) and site-level characteristics (type of site, age of programme, reported presence of a nutritionist on staff).
The fact that nutritional counselling to adults and to pregnant and lactating mothers was reported to be available at 95 % and 91 % of sites, respectively, is encouraging. Nutritional counselling is considered to be a cornerstone of HIV treatment support, recommended by multiple international guidelines(36, 39, 40). Nutritional counselling is also important for supporting HIV-affected households. Studies in sub-Saharan Africa have found that HIV-exposed but uninfected children have poorer growth compared with HIV-uninfected children, possibly because of reduced breast-feeding practices by HIV-infected mothers(Reference Filteau41). Exposure to nutritional counselling and education about safe breast-feeding practices is associated with increased weight gain and a reduced risk of postnatally acquired HIV infection among HIV-exposed infants, respectively(Reference Piwoz, Humphrey and Tavengwa42, Reference Tabi and Vogel43). Sustained programme efforts and optimization of general and infant feeding counselling are critical, particularly as rates of exclusive breast-feeding among HIV-infected mothers remain low in many settings where it is recommended(Reference Fadnes, Engebretsen and Wamani44).
Although some type of micronutrient supplementation was reported to be available at 64 % of sites, this mostly included vitamin A and Fe supplementation. The fact that multivitamin and mineral supplementation was reported to be available at only 25 % of HIV care and treatment sites suggests that there is room for improvement. Studies have found that many people living with HIV/AIDS suffer various micronutrient deficiencies and have increased micronutrient needs(Reference DePee and Semba45). However, evidence of the effectiveness of micronutrient supplementation on HIV-infected adults and children remains limited, and findings have been heterogeneous. Supplementation of specific vitamins and minerals has been associated with several clinical benefits among people living with HIV/AIDS, including reduced risk of hospitalization(Reference Burbano, Miguez-Burbano and McCollister46), increased CD4 cell count levels(Reference Kaiser, Campa and Ondercin47) and reductions in all-cause mortality(Reference Irlam, Visser and Rollins48). Among individuals receiving ART, micronutrient supplementation has been variously correlated with improved immunological, virological and clinical status and may facilitate decreases in mitochondrial dysfunction, oxidative stress and metabolic complexities(Reference Drain, Kupka and Mugusi49). A recent meta-analysis found that periodic vitamin A supplementation of HIV-positive children aged >6 months was associated with reduced all-cause mortality, but additional research is required to determine the impact on HIV-infected adults(Reference Irlam, Visser and Rollins48). Results from studies evaluating the impact of other specific micronutrients, such as vitamin E, Se, Zn and Fe, on HIV-infected individuals remain inconclusive(Reference DePee and Semba45). Although the reported availability of micronutrient supplementation at some of the HIV care and treatment sites in our sample is encouraging, the expansion of access to micronutrient supplementation must be evidence-informed via research studies, with scale-up, safety and adherence carefully monitored at site and patient levels to ensure optimal outcomes.
Food rations were reported to be available at 31 % of HIV care and treatment sites. Macronutrient supplementation, commonly comprising corn–soya blend, fortified blended foods and high-energy ready-to-use therapeutic foods (RUTF), is often used as a replacement of, or complement to, regular staple foods(Reference Koethe, Chi and Megazzini50). Supplemental feeding is often used to mitigate the impacts of mild and moderate malnutrition and to prevent further deterioration of nutritional status to severe acute malnutrition.
Studies have noted that provision of food rations may be associated with improved medication adherence and retention in HIV care and treatment in sub-Saharan Africa, which is both a major and persistent challenge of scale-up in the region(Reference Rosen, Fox and Gill51, Reference Brinkhof, Dabis and Myer52). In a qualitative programme evaluation from Kenya, provision of household food rations to food-insecure individuals on ART improved treatment adherence, reduced drug-related side effects and increased appetite satisfaction, weight gain and physical strength(Reference Byron, Gillespie and Nangami53). A randomized controlled trial involving 636 food-insecure adults starting ART in Zambia found that individuals who received home-based WFP rations were 1·5 times more likely to achieve 95 % ART adherence, compared with the control group(Reference Cantrell, Sinkala and Megazinni54). Finally, we reported in a previous ecological analysis of 108 056 individuals initiating ART across ten sub-Saharan African countries that the reported availability of food supplementation was significantly associated with higher retention in HIV care and treatment(Reference Nash, Korves and Saito55). The impact of fortified food supplementation on HIV-affected individuals is varied. A randomized controlled trial in Zambia comparing the impact of a basal v. micronutrient-fortified infant porridge in Zambia found that micronutrient supplementation did not reduce stunting or hospital referrals among HIV-exposed children but did improve Fe status and anaemia(56). Given the high burden of food insecurity in sub-Saharan Africa(6), availability of food supplementation in HIV care and treatment sites to HIV-infected and -affected individuals could promote individual and household food security and clinical outcomes.
Treatment for severe malnutrition was reported to be available at 36 % of HIV care and treatment sites and was more likely to be reported to be available at sites that had been providing ART for more than 2 years. This may be because longer established ART sites have increased logistic capacity, compared with more recently established ART sites(Reference Mapunjo and Urassa57). Interestingly, the likelihood of reported availability of treatment for severe malnutrition was similar at primary, secondary and tertiary care sites. This finding is surprising given that, until recently, the WHO clinical guidelines recommended in-patient hospital admission and prescription of high-energy milk products for the treatment for severe acute malnutrition. Operations research in sub-Saharan Africa now suggests that community-based distribution of RUTF is just as feasible and safe as, and more cost-effective than, hospital-based rehabilitation(Reference Briend, Prudhon and Prinzo58). Our findings that availability of treatment for severe malnutrition has expanded significantly even over a 1·5-year period suggest that ART treatment and care sites may be distributing RUTF products. These findings are promising given that RUTF use has been associated with rapid weight gain, improvements in physical activity and increased uptake of VCT and ART services among HIV-positive individuals with severe acute malnutrition(Reference Bahwere, Sadler and Collins59, Reference Ndekha, Manary and Ashorn60).
Our study has several strengths and limitations. The strengths of our study include the large number of sites, which allowed us to conduct an analysis of the reported availability of nutritional support services in scale-up programmes across several sub-Saharan African countries and settings. We were also able to include rural sites and primary health centres, increasing the generalizability of the findings. All PEPFAR-supported HIV care and treatment sites are situated within the public sector and as such are representative of African countries’ national efforts to scale-up ART access. Although the sites included in our sample are likely not representative of all HIV clinics in the region or within each country, they represent primary, secondary and tertiary scale-up sites from a diverse array of settings and contexts. These sites represent a substantial proportion of all patients initiating ART in sub-Saharan Africa, including over 7 % of the estimated 2·925 million people receiving ART in the continent in 2008(61).
The study survey tool was formally tested for reliability and accuracy and was found to have a good level of reliability between staff- and supervisory-completed responses. The following data management systems likely contributed to this high level of agreement, and additionally contributed to consistency of data quality across study sites and countries: (i) responses to surveys were recorded following a process of discussion and consensus among site staff; (ii) surveys were administered at sites using standard operating procedures, with reference to clearly defined indicators; and (iii) all data were computer-recorded using automated data entry controls and logic checks, followed by systematic data cleaning.
A major limitation is that site surveys solicited information only about the availability of different types of services and did not ascertain the access, quality, comprehensiveness or coverage of the indicated services at the sites. Thus, no information is available on the actual number, proportion or subsets of patients who utilized these services. For example, although the proportion of sites that reported availability of nutritional counselling or weight-for-height evaluation was high, we could not assess the proportion of patients who actually received these services at the sites in our sample(Reference King, Rosen and Tanner62). The amount of micronutrient supplementation available to clients at each site was unknown, and likely varied given the differences between the WHO and regional recommendations for recommended nutrient intake(Reference DePee and Semba45). We were unable to assess what types of food rations were available and whether these were intended for use by all HIV-positive individuals, by specific groups of HIV-infected groups or by HIV-affected households. Finally, we were unable to ascertain the types of treatment that were available for severe malnutrition and the extent to which RUTF products may have contributed to rapid increases in availability. Consequently, these data are most useful for macro-level policy and programmatic planning.
Our study is in alignment with the United Nations General Assembly Special Session (UNGASS) Declaration of Commitment on HIV/AIDS’ goal of monitoring and evaluating process outputs from HIV treatment and care facilities(63). These findings can directly assist national Ministries of Health and their partners’ efforts to monitor the rollout of HIV-related support services in accordance with national policies, to identify time-bound national goals for improving support to people living with HIV/AIDS and to track changes in the availability of these services over time(63). UNGASS 2010 Guidelines on the Construction of Core Indicators failed to explicitly recommend the collection of national programme indicators on nutritional support to adults and children living with HIV/AIDS and their affected households(64). Cross-national health facility data on the availability of nutritional support services are essential to effectively monitor and evaluate global HIV treatment and care outcomes.
Conclusion
Basic nutritional support services were reported to be available at a large number of public sector HIV care and treatment sites across urban and rural settings in several sub-Saharan African countries. Reported availability of specific nutritional support services varies by country, geographical context and clinical or programme characteristics. These findings can inform Ministries of Health and their partners in their efforts to make these services available at sites that provide HIV care and treatment in accordance with national policies(63). Expansion of availability of nutritional services is of critical importance. Further efforts are urgently needed to determine, in addition to availability, the uptake, quality and effectiveness of these services and their impact on programme outcomes such as adherence to ART, retention in care and survival.
Acknowledgements
International Center for AIDS Care and Treatment Programs (ICAP)-supported HIV prevention, care and treatment programmes are funded through the President's Emergency Plan for AIDS Relief. The present research was supported by the Doris Duke Charitable Foundation's Operations Research on AIDS Care and Treatment in Africa. A.A. is supported by the Canadian Institutes of Health Research. R.S.H. has received grant funding from the National Institutes of Health, Canadian Institutes of Health Research National Health Research Development Program and Health Canada. He has also received funding from Agouron Pharmaceuticals Inc., Boehringer Ingelheim Pharmaceuticals Inc., Bristol-Myers Squibb, GlaxoSmithKline and Merck Frosst Laboratories for participating in continued medical education programmes. J.S.G.M. has received grants from, served as an ad hoc advisor to, or spoken at various events sponsored by Abbott, Argos Therapeutics, Bioject Inc., Boehringer Ingelheim, BMS, Gilead Sciences, GlaxoSmithKline, Hoffmann-La Roche, Janssen-Ortho, Merck Frosst, Pfizer, Schering, Serono Inc., TheraTechnologies, Tibotec and Trimeris. He has also received grant funding from the Canadian Institutes of Health Research and National Institutes of Health and for research and continuing medical education programmes from a number of pharmaceutical companies including Abbott, Boehringer Ingelheim and GlaxoSmithKline. The funders had no role in study design, data collection and analysis, nor in the decision to publish or in preparation of the manuscript. The authors have no conflict of interest to declare. A.A. and D.N. conceived of the study aims, objectives and overall study design; A.A., D.N., W.Z. and Y.W. developed the study methodologies; A.A., W.Z. and D.N. wrote the first draft of the manuscript; R.S.H., J.S.G.M., S.W., B.E. and W.E.-S. contributed technical expertise and critically reviewed manuscript drafts; D.N. oversaw all aspects of the study design, as well as survey data collection and data management. The authors thank the headquarters and field staff from the International Center for AIDS Care and Treatment Programs who completed the Program and Facility Characteristics Tracking System survey, including the following staff: Dr Caroline Korves, Ms Suzue Saito, Ms May Tun and Mr Matthew Lamb from the ICAP Headquarters in New York, USA; Senior Monitoring and Evaluation Advisors in the ICAP country offices, including Dr Tsigereda Gadisa (ICAP Ethiopia), Dr Muhsin Sheriff (ICAP Kenya), Ms Melanie Manyasha (ICAP Lesotho), Ms Maria Fernanda Alvim (ICAP Mozambique), Mr Frank Oransaye (ICAP Nigeria), Dr Veronicah Mugisha (ICAP Rwanda), Dr Harriet Nuwagaba-Biribonwoha (ICAP Tanzania), Ms Kanchan Reid (ICAP South Africa) and Mr Hermann Brou (ICAP Cote d'Ivoire); ICAP Clinical Officers in each country who contributed to data collection; and ICAP Country Directors Dr Mark Hawken (ICAP Kenya), Dr Zenebe Melaku (ICAP Ethiopia), Ms Amy Cunningham (ICAP Tanzania), Dr Ruben Sahabo (ICAP Rwanda), Dr Tshiwela Neluheni (ICAP South Africa), Dr Bolanle Oyeledun (ICAP Nigeria), Dr Raphael Ntumy (ICAP Lesotho), Dr Josue Lima (ICAP Mozambique) and Dr Ida Viho (ICAP Cote d'Ivoire) for overall support and guidance. The authors also acknowledge the Ministries of Health from Kenya, Tanzania, Ethiopia, Rwanda, Mozambique, South Africa, Nigeria, Lesotho and Cote d'Ivoire whose HIV care and treatment programmes they endeavoured to support through the present work. Finally, they also thank Dr David Hoos for overall leadership on programme activities.






