Osteoporosis is a major public health concern for an estimated 44 million Americans or 55 % of those aged 50 years and older(1). In the USA, 10 million individuals are estimated to already have the disease and almost 34 million more are estimated to have low bone mass, placing them at increased risk for osteoporosis(Reference Parker, Noakes and Luscombe2). Eighty per cent of those affected by osteoporosis are women(1).
Protein intake has been implicated in previous studies as being both detrimental and beneficial to bone health(Reference Heaney and Layman3). While dietary protein has long been known to increase renal Ca excretion and create negative Ca balance(Reference Itoh, Nishiyama and Suyama4–Reference Kerstetter and Allen6), many population-based studies(Reference Hannan, Tucker and Dawson-Hughes7–Reference Geinoz, Rapin and Rizzoli13), but not all(Reference Mazess and Barden14–Reference Wang, Luz Villa and Marcus18), have shown that protein intake is beneficial for the skeleton. Both protein and Ca are major components of bone tissue and play active roles in bone metabolism(Reference Dawson-Hughes19). Recent studies suggest that the influence of protein on bone health may differ according to Ca intake. A randomized placebo-controlled trial of elderly men and women concluded that higher protein intake may have a favourable effect on change in bone mineral density (BMD), but only in individuals supplemented with calcium citrate and vitamin D(Reference Dawson-Hughes and Harris20). Therefore, the long-term influence of typical protein intakes may depend on concurrent Ca intakes. Our prior work showed an association between low protein intake and greater bone loss in elderly men and women in the original Framingham Study cohort at advanced ages(Reference Hannan, Tucker and Dawson-Hughes7). It is unclear if this relationship exists in middle-aged adults and if it depends on Ca intake, as some evidence suggests that higher protein intake may enhance Ca absorption(Reference Hunt, Johnson and Fariba Roughead21). In the present study, we hypothesized that greater protein intake would be associated with higher BMD and less BMD loss in largely middle-aged adults participating in the Framingham Offspring Cohort. Further, we hypothesized that high protein intake would be most protective against BMD loss when Ca intake was high.
Participants and methods
The Framingham Heart Study Original Cohort is a population-based cohort study that was initiated in 1948 to examine risk factors for heart disease. The Offspring Cohort was recruited in 1971 and included 5124 adult children and their spouses (aged 26–86 years) of the Original Cohort participants, and has been examined approximately every 4 years. For the current study we present data from Offspring Cohort participants with BMD and dietary information in 1995–2001. All participants provided informed consent for their participation and the study was approved by Institutional Review Boards at Boston University and Hebrew SeniorLife.
Cross-sectional analyses
Offspring Cohort participants included in the cross-sectional analyses consisted of the 1280 men and 1639 women who had both valid FFQ information, collected in either 1995–1998 or 1998–2001, and a BMD assessment completed in 1996–2001.
Longitudinal analyses
Participants included in the longitudinal analyses were a subset of the Offspring Cohort and consisted of 497 men and 680 women who had both valid FFQ information, collected in either 1995–1998 or 1998–2001, along with baseline BMD assessed in 1996–2001 and follow-up BMD assessed in 2002–2005. Follow-up time ranged from 1·5 to 8 years, with an average of 4·6 years.
Assessment of dietary protein intake
Usual dietary intake was assessed with a semi-quantitative, 126-item Willett FFQ(Reference Rimm, Giovannucci and Stampfer22, Reference Willett and Stampfer23) in either 1995–1998 or 1998–2001. Questionnaires were mailed to the study participants prior to their scheduled clinic visit. They were asked to complete them, based on their intake over the previous year, and to bring them to the examination site, where they were reviewed with the participants by the clinic staff. Questionnaires with more than twelve items left blank in the FFQ, or with energy intakes <2·51 or >16·74 MJ, were considered invalid and excluded. This FFQ has been validated for many nutrients, including protein, in several populations against multiple diet records and blood measures(Reference Ascherio, Stampfer and Colditz24, Reference Jacques, Sulsky and Sadowski25).. Intakes of total protein (g/d), dietary Ca (mg/d), dietary vitamin D (IU/d), total energy (kcal/d) and Ca supplement use (yes/no) were assessed using the food list section of the FFQ. We calculated protein intake % as the percentage of total energy intake from protein in each cohort.
Bone mineral density
BMD (g/cm2) of the hip (femoral neck (FN) and trochanter (TR)) and lumbar spine (LS; L2–L4) was obtained at baseline, in 1996–2001. For a subset of the study cohort, BMD was measured at the subsequent follow-up in 2002–2005. The right hip was scanned unless there was a history of fracture or hip replacement, in which case the left hip was scanned. Measurements completed in 1996–2001 were obtained using a LUNAR DPX-L dual-energy X-ray absorptiometer (Lunar Corp., Madison, WI, USA) and were repeated using a GE Lunar Prodigy (GE Lunar, Madison, WI, USA) in 2002–2005. Percentage change in BMD over follow-up was calculated as(Reference Hannan, Felson and Dawson-Hughes26): [(BMD at follow-up – BMD at baseline exam)/BMD at baseline] × 100, adjusting for change in technology from DPX-L to Lunar Prodigy using already published equations(Reference Gagnon, McLean and Hannan27). Annualized percentage change in BMD was then calculated as the percentage change in BMD divided by the time difference (years) between the two BMD measures.
Covariates
Covariate information on age (years), height (inches), weight (pounds), smoking (current v. non-current) and physical activity was measured at the same time as the BMD measurement. Height was measured while participants were shoeless; measurements of weight were taken with a standardized balance-beam scale. The smoking status of the participants was assessed via questionnaire as current cigarette smoker (smoked regularly in the past year), former smoker or never smoker; former and never smokers were combined into the group ‘non-current smokers’. For oestrogen use, women were divided into two groups: those currently oestrogen using at the time of the exam and those who had never used or who had formerly used oestrogen. Physical activity was measured with use of the Physical Activity Scale in the Elderly (PASE)(Reference Washburn, Smith and Jette28). The PASE at the previous exam (1991–1995) was used for the participants with missing PASE values. Furthermore, menopause status (yes/no) and osteoporosis medication use (yes/no) were also determined at the same time as BMD measurement.
Dietary covariates were taken from the FFQ measurement. Total energy (MJ/d), dietary Ca (mg/d), dietary vitamin D (IU/d), Ca supplement use (yes/no), vitamin D supplement use (yes/no), alcohol use (g/d), caffeine intake (g/d) and oestrogen use were measured in this cohort. For stratification by total Ca and dietary Ca intake we used a cut-off of 800 mg/d (approximating the median intake), rather than using the current, higher, RDA values of 1000–1200 mg/d for this age group(29) to ensure enough power for the interaction analyses.
Statistical analysis
Analyses were conducted separately by sex. Protein intake % as well as protein (g/d) were modelled as both a continuous variable and categorized into quartiles. For continuous analyses, to determine the association between protein intake % and BMD as well annualized change in BMD at each site, we used multivariable linear regression to calculate regression coefficients (β) estimating the difference in BMD and bone loss associated with a 1-unit increase in protein intake %. We used ANCOVA to compare least-squares adjusted BMD as well as bone loss among quartiles of protein intake % and to test for linear trend across quartiles. For quartile analysis, we used the residual method for energy adjustment(Reference Willett, Howe and Kushi30).
The models were initially adjusted for total energy intake, age, height and weight. Subsequent models were further adjusted for dietary vitamin D and Ca intakes, use of vitamin D and Ca supplements, current smoking, caffeine and alcohol intake, physical activity, osteoporosis medication use and, for women only, current oestrogen use and menopausal status. Longitudinal change models were also adjusted for baseline BMD.
Interactions with intake of total Ca (>800 mg/d, yes/no), dietary Ca (>800 mg/d, yes/no) or Ca supplement use (yes/no) were tested by introducing an interaction term between Ca intake and protein intake % in the full model. For middle-aged to older adults, the RDA for Ca intake is between 1000 and 1200 mg/d. To achieve balanced numbers of participants in the stratified analyses, we chose to use a cut-off of 800 mg/d. If the interaction term was statistically significant (P < 0·05), we examined the association of protein intake % with BMD and annualized change in BMD within subgroups of total Ca intake (<800 mg/d and ≥800 mg/d), dietary Ca intake (<800 mg/d and ≥800 mg/d) and Ca supplement use (yes/no). The models stratified by dietary Ca intake included Ca supplement use (yes/no) as a covariate. Similarly, the models stratified by Ca supplement use (yes/no) also included dietary Ca intake (mg/d) as a covariate. All analyses were performed with the statistical software package SAS version 9·1, 2001. A nominal two-sided P value of 0·05 was considered statistically significant for all analyses.
Results
The mean age of men and women was 61 and 60 years, respectively (age range: 29–86 years; Table 1). Total protein intake was 77 g/d in women and 81 g/d in men (higher than the RDA for this age group). Dietary Ca intake was 762 mg/d in women and 763 mg/d in men. More than 40 % of men and 60 % women had dietary Ca intake <800 mg/d. Approximately three-quarters of men (74·5 %) and two-thirds of women (59·6 %) did not reach the RDA for Ca intake. More women than men used Ca supplements (56 % v. 24 %) and vitamin D supplements (53 % v. 40 %).
Table 1 Characteristics of the Framingham Offspring Cohort at the baseline exam

Protein intake %, percentage of total energy intake from protein; FN, femoral neck; BMD, bone mineral density; TR, trochanter; LS, lumbar spine.
†Values are presented as mean and standard deviation, unless otherwise noted as percentage.
Results from the cross-sectional analyses showed that protein intake % was positively associated with FN (P = 0·04), TR (P = 0·02) and LS (P = 0·04) BMD in women, while no significant associations were seen in men at any bone site (P range: 0·28–0·72; Table 2). Similar results were observed for categorical analyses, where women in the highest quartile of protein intake % (mean protein intake of 92 g/d v. 68 g/d in the lowest quartile) had the highest FN-BMD compared with the lower quartiles (Q4 v. Q1: P = 0·03; Q4 v. Q2: P = 0·04; Q4 v. Q3: P = 0·003) although the trend did not reach statistical significance (P trend = 0·08). Similarly, higher protein intake % was associated with higher TR-BMD (P = 0·02) but not with LS-BMD (P = 0·23) in women, while no significant associations were seen in men at any bone site (P range: 0·20–0·53; data not shown).
Table 2 Cross-sectional association of protein intake% and BMD (g/cm2) in men and women from the Framingham Offspring Cohort
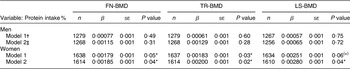
Protein intake %, percentage of total energy intake from protein; BMD, bone mineral density; FN, femoral neck; TR, trochanter; LS, lumbar spine.
Regression coefficient and standard error significant at (*)P < 0·1, *P < 0·05.
†Model 1 adjusted for total energy intake (kcal/d), age (years), height (inches) and weight (pounds)
‡Model 2 adjusted for model 1 and dietary vitamin D intake (IU/d), vitamin D supplement use (yes/no), Ca supplement use (yes/no), dietary Ca intake (<800 mg/d or ≥800 mg), current smoking (yes/no), menopausal status (yes/no), current oestrogen use (yes/no) in women alone, caffeine intake (g/d), Physical Activity Scale in the Elderly (PASE), osteoporosis medication use (yes/no) and alcohol intake (none, moderate and heavy intake (in males: 0, 0–26·4 g/d, >26·4 g/d; in females: 0, 0–13·2 g/d, >13·2 g/d)).
No significant interactions were observed with protein intake % and dietary Ca or supplemental Ca intake and BMD in men or women (P for interaction range: 0·07–0·90). However, significant interactions between protein intake % and total Ca intake were observed in women (P for interaction range: 0·002–0·02). Upon stratification by total Ca intake (<800 mg/d v. ≥800 mg/d), among women with total Ca intake of <800 mg/d, protein intake % was positively associated with FN (P = 0·05), TR (P = 0·04) and approached significance with LS (P = 0·10) BMD (Table 3). No significant associations were observed in women with total Ca intake ≥800 mg/d (P range: 0·12–0·26).
Table 3 Cross-sectional association of protein intake % and BMD (g/cm2) stratified by total calcium intake in women from the Framingham Offspring Cohort

Protein intake %, percentage of total energy intake from protein; BMD, bone mineral density; FN, femoral neck; TR, trochanter; LS, lumbar spine.
Regression coefficient and standard error significant at (*)P < 0·1, *P < 0·05.
†Model 1 adjusted for total energy intake (kcal/d), age (years), height (inches) and weight (pounds).
‡Model 2 adjusted for model 1 and dietary vitamin D intake (IU/d), vitamin D supplement use (yes/no), current smoking (yes/no), menopausal status (yes/no), current oestrogen use (yes/no), caffeine intake (g/d), Physical Activity Scale in the Elderly (PASE), osteoporosis medication use (yes/no) and alcohol intake (none, moderate and heavy intake (in females: 0, 0–13·2 g/d, >13·2 g/d)).
For the longitudinal analyses, mean follow-up was 4·6 years. In women, no significant associations were observed between protein intake % and bone loss (all sites P range: 0·12–0·82). However, in men, higher protein intake was associated with more bone loss at TR (P = 0·01), but not at FN and LS (P range: 0·73–0·75, Table 4). Results from quartile analyses showed no significant associations between protein intake % and bone loss in men or women (P trend range: 0·16 to 0·50 in women and 0·20 to 0·87 in men; data not shown). Furthermore, no significant interactions were observed with total Ca, dietary Ca or supplemental Ca intake and annualized change in BMD in women or men (P for interaction range: 0·14–0·97 in women and 0·07–0·97 in men; data not shown).
Table 4 Association of protein intake % and annualized change in BMD (g/cm2)Footnote † in men and women from the Framingham Offspring Cohort
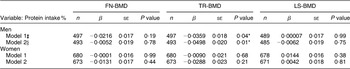
Protein intake %, percentage of total energy intake from protein; BMD, bone mineral density; FN, femoral neck; TR, trochanter; LS, lumbar spine.
Regression coefficient and standard error significant at *P < 0·05.
† Annualized change in BMD = % BMD change/time difference between the two BMD measures, where % BMD change = [(BMD at follow-up − BMD at baseline exam)/BMD at baseline] × 100.
‡ Model 1 adjusted for total energy intake (kcal/d), age (year), height (inches) and weight (pounds).
§ Model 2 adjusted for model 1 and dietary vitamin D intake (IU/d), vitamin D supplement use (yes/no), dietary Ca intake (<800 mg/d or ≥800 mg), Ca supplement use (yes/no), current smoking (yes/no), menopausal status (yes/no), current oestrogen use (yes/no) in women alone, caffeine intake (g/d), Physical Activity Scale in the Elderly (PASE), osteoporosis medication use (in women alone, yes/no), alcohol intake (none, moderate and heavy intake (in males: 0, 0–26·4 g/d, >26·4 g/d; in females: 0, 0–13·2 g/d, >13·2 g/d)) and baseline BMD (g/cm2).
Similar associations were observed when these analyses were repeated with protein intake as g/d (data not shown).
Discussion
Cross-sectional analyses indicated that higher protein intake, as a percentage of total energy intake, was associated with higher BMD in the Offspring Cohort women but not in men. These associations were modified by total Ca intake such that the positive associations were primarily observed in women with total Ca intake of <800 mg/d. Longitudinal analyses suggested that protein intake was not linked to short-term bone loss in middle-aged women, although negative associations were observed for men at TR-BMD. Finally, our findings suggested that Ca intake (total, dietary or supplemental Ca), at least in our cohort of mostly middle-aged adults, did not modify the relationship between protein intake and longitudinal changes in BMD.
Most population-based, cross-sectional observational studies suggest that greater dietary protein intake is associated with higher BMD in middle-aged and older adults(Reference Hannan, Tucker and Dawson-Hughes7, Reference Promislow, Goodman-Gruen and Slymen9–Reference Geinoz, Rapin and Rizzoli13, Reference Coin, Perissinotto and Enzi31). Using cross-sectional data from the Third National Health and Nutrition Examination Survey, Kerstetter et al.(Reference Kerstetter, Looker and Insogna11) found that in adult white women over the age of 50 years, low dietary protein intake (range: 0–43 g/d) was associated with reduced femoral bone density (P = 0·003) compared with women with high protein intake (>75 g/d). This direct relationship also held true for quartiles; compared with the highest quartile of protein intake (>75 g/d), BMD was significantly lower in each lower quartile of dietary protein intake (P = 0·003), even after adjusting for age and body weight. Our cross-sectional findings among women are consistent with the study by Kerstetter et al.
A previous longitudinal study by our group in the older Framingham Original Cohort (mean age 75 years) found that, in both men and women, lower protein intake was significantly associated with greater bone loss over 4 years at both the femoral neck and spine in a dose–response pattern(Reference Hannan, Tucker and Dawson-Hughes7). Participants in the lowest quartile of protein intake showed the greatest bone loss even after controlling for confounders (P < 0·01). These findings were among the first to suggest that adequate protein intake is important in maintaining bone or minimizing bone loss in elderly persons. However, results from the current longitudinal analysis in the Framingham Offspring Cohort (mean age 60 years) are not consistent with the previously reported results in the Original Cohort(Reference Hannan, Tucker and Dawson-Hughes7). In the present study, although the direction of the associations observed in the cross-sectional analyses was in agreement with our previous work, the only statistically significant finding in the longitudinal analysis was unexpected since it showed high TR-bone loss with higher protein intake among men. We recognize that a number of comparisons were made in our examination of dietary protein and bone outcomes. Although our analyses were based upon defined hypotheses, we believe that a single finding may not confirm or invalidate our hypothesis, especially since we did not observe the same associations for other skeletal sites. It is possible that this single significant finding was due to random chance.
Additionally, significant interactions were observed between protein intake % and total Ca intake in the cross-sectional analysis alone. Dawson-Hughes and Harris examined the interaction between protein intake and Ca supplementation using data from a Ca supplementation trial that was conducted in 342 men and women (mean age: 71 years)(Reference Dawson-Hughes and Harris20). They reported that higher protein intake was protective of BMD loss over the 3-year follow-up, but only among the group taking Ca and vitamin D supplements. The authors suggested that greater absorbed Ca in the supplemental group might have offset potential negative effects of protein on Ca balance, thereby allowing positive effects of protein on the skeleton. In another prospective study among French postmenopausal women (age range: 40–65 years, mean age: 56 years) of the Mutuelle Générale de l'Education Nationale (MGEN)(Reference Dargent-Molina, Sabia and Touvier32), there was no overall association between fracture risk and total protein on renal net acid excretion. However, the authors reported that in the lowest quartile of Ca (<400 mg/4184 kJ (1000 kcal)), high protein intake was associated with significantly greater fracture risk (relative risk = 1·51; 95 % CI 1·17, 1·94 for the highest v. the lowest quartile). These studies suggest that the positive effects of dietary protein on bone may only be realized in the setting of adequate Ca intake (mean total Ca = 1346 (sd 358) mg/d in the supplemented group v. 871 (sd 413) mg/d in the placebo group(Reference Dawson-Hughes and Harris20)). However, the stratified analyses in the present study showed that protein intake was positively associated with BMD in women with total Ca intake of <800 mg/d. No significant interactions were observed in the longitudinal analyses. There are several possible reasons for the discrepancy between results from these studies and those from the Offspring Cohort. First, participants in the Offspring Cohort were mostly middle-aged compared with the older adults included in the studies by Dawson-Hughes as well as the Framingham Original Cohort. Furthermore, there may also be different patterns of dietary intakes for protein and other nutrients between age groups. For example, in both of the Framingham cohorts, total Ca intake is similar to mean Ca intake in the placebo group in the study by Dawson-Hughes and Harris. Lastly there may also be an age cohort effect for bone, as noted by others for patterns of hip fracture across age cohorts(Reference Samelson, Zhang and Kiel33, Reference Cooper, Cole and Holroyd34).
The current study is unique in that it presents both cross-sectional and longitudinal findings from a population-based cohort of largely middle-aged individuals. However, the study has limitations. First, we had limited information on dietary intakes (i.e. FFQ only estimates a rank order of usual intakes, not definitive measure). However, this FFQ has previously been validated in several different populations(Reference Ascherio, Stampfer and Colditz24, Reference Jacques, Sulsky and Sadowski25). In a study by Willett et al., the correlation for protein intake from the FFQ v. four 1-week diet records in largely middle-aged women from the Boston area was 0·52(Reference Willett, Sampson and Browne35). Second, the longitudinal analyses included a subset of the Framingham Offspring Cohort. Furthermore, the actual values of longitudinal BMD changes in our middle-aged cohort were small, of the range of 0 to 1 % (BMD change %: FN = 0·03 %, TR = −0·10 % and LS = 0·31 %), making it difficult to detect any effect of protein upon this small change in BMD. Further, our follow-up for longitudinal bone change was about 4 years, and longer follow-up of middle-aged men and women may be needed to consider the long-term effects of diet upon bone health that have been observed in older ages. Furthermore, we did not examine the influence of different protein sources (dairy, meat, fish, vegetables, etc.) in the study. Other studies have suggested that animal protein may be positively associated with BMD, whereas plant protein may be negatively associated with BMD(Reference Promislow, Goodman-Gruen and Slymen9). The positive relationship between animal protein and BMD was also seen in the Framingham Original Cohort, where older women with animal protein intakes up to sevenfold greater than the RDA had the least bone loss(Reference Hannan, Tucker and Dawson-Hughes7). These studies show evidence of a differing association of protein with bone density depending upon protein source. Future investigations should confirm whether animal v. plant protein has different associations with bone density and fracture risk, as this would have significant public health implications. In addition, as with any observational study, residual confounding may occur, despite our attempts to control for the major potential confounders. Lastly, the results of the present study are generalizable primarily to non-Hispanic white men and women, given the composition of the Framingham Offspring Cohort.
Conclusions
Our cross-sectional findings among primarily middle-aged adults suggest that higher protein intake is associated with higher BMD in women (especially those with lower Ca intake) but not men. Longitudinal analyses suggest that higher protein intake may not be associated with less bone loss over 4 years, perhaps with the exception of hip bone loss among men, which increased with higher protein intake. Furthermore, Ca intake does not appear to influence the relationship of protein and bone loss among middle-aged adults. In this age group with limited bone loss that may not be of clinical significance, longer follow-up is required to examine the impact of protein intake on bone loss. While individual macronutrients (protein) and micronutrients (Ca) are of great public health interest, these results indicate that there may be different public health messages for current bone health by age group.
Acknowledgements
Sources of funding: This work was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases and the National Institute on Aging (AR053205 and AR041398); and the National Heart, Lung, and Blood Institute's Framingham Heart Study (contract no. N01-HC-25195). The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies. Conflicts of interest: None; M.T.H., D.P.K., L.A.C., S.S., K.E.B., K.L.T. and R.R.M. have no conflicts of interest to disclose. Ethical approval: All participants provided informed consent for their participation and this study was approved by Institutional Review Boards at Boston University and Hebrew SeniorLife. Authors’ contributions: M.T.H., D.P.K. and L.A.C. were responsible for the conception and design of the study, helped with the data acquisition, obtained funding, and provided administrative and technical support. S.S. conducted the statistical analyses and drafted the manuscript. All authors (S.S., K.E.B., R.R.M., D.P.K., L.A.C. and M.T.H.) contributed towards the writing of the manuscript and were responsible for critical revision for important intellectual content.






