African American (AA) and Hispanic/Latino (HL) adults suffer from higher rates of heart disease( Reference Davis, Vinci and Okwuosa 1 ), obesity( Reference Flegal, Carroll and Ogden 2 ) and diabetes( Reference Peek, Cargill and Huang 3 ) than their Caucasian peers. A diet high in fat (≥30 % of total energy from fat) and excess energy is associated with chronic diseases and obesity( Reference Mente, de Koning and Shannon 4 – Reference Kuller 6 ), and large proportions of AA and HL adults consume excess energy from fat( Reference Kirkpatrick, Dodd and Reedy 7 ). Identifying determinants of diet and obesity among AA and HL women may provide intervention targets for reducing obesity among these high-risk groups.
Ecological models posit that health behaviours such as dietary intake are influenced by individual-, sociocultural-, organizational-, community- and policy-level factors( Reference Lee and McAlexander KM Banda 8 – Reference Spence and Lee 11 ). The number and type of eating establishments available in one's environment represent community-level factors that influence behaviour. Fast-food restaurants (FFR) are widely available, particularly among low-income and minority neighbourhoods( Reference Larson, Story and Nelson 12 – Reference Azuma, Gilliland and Vallianatos 15 ), and serve mostly high-fat, energy-dense, nutrient-poor foods( Reference Prentice and Jebb 16 , Reference Lin, Frazao and Guthrie 17 ). Frequent fast-food consumption has been related to higher fat intake( Reference Larson, Story and Nelson 12 , Reference Satia, Galanko and Siega-Riz 18 – Reference Bowman and Vinyard 20 ) and poor health( Reference Pereira, Kartashov and Ebbeling 21 – Reference Mehta and Chang 24 ). Availability of FFR in one's residential neighbourhood increases the likelihood of consuming fast foods( Reference Li, Harmer and Cardinal 23 , Reference Sharkey, Johnson and Dean 25 , Reference Sharkey, Johnson and Dean 26 ), having poor diet quality( Reference Larson, Story and Nelson 12 , Reference Boone-Heinonen, Gordon-Larsen and Kiefe 27 ) and being obese( Reference Li, Harmer and Cardinal 23 , Reference Mehta and Chang 24 , Reference Giskes, Avendano and Brug 28 – Reference Fleischhacker, Evenson and Rodriguez 30 ). However, not all individuals within a given environment will have a poor diet or become obese; some studies did not find an association between residential neighbourhood availability of FFR and diet( Reference Richardson, Boone-Heinonen and Popkin 31 – Reference Zenk, Schulz and Matthews 33 ) or obesity( Reference Pearce, Hiscock and Blakely 32 ), while some found the inverse to be true (greater neighbourhood FFR availability associated with lower BMI)( Reference Kestens, Lebel and Chaix 34 ). Identifying qualities or individual factors that make some individuals more likely to become obese in an obesogenic environment where FFR are prevalent will allow the development of targeted policies and interventions with greater effectiveness.
The relationship between neighbourhood FFR availability and fast-food consumption appears to be moderated by sensitivity to external reward cues and sense of control over the environment( Reference Paquet, Dube and Gauvin 35 , Reference Paquet, Daniel and Knauper 36 ). Neighbourhood FFR availability and fast-food consumption were more positively related among those who were sensitive to external reward cues( Reference Paquet, Daniel and Knauper 36 ) and had a higher sense of control over their environment( Reference Paquet, Dube and Gauvin 35 ). Sensitivity to reward cues and low sense of control are qualities of binge eaters( Reference Bulik, Brownley and Shapiro 37 , Reference Mathes, Brownley and Mo 38 ). Binge eating refers to overeating with loss of control and associated feelings of guilt and shame( Reference Bulik, Brownley and Shapiro 37 ), and it is commonly reported by 15–20 % of non-clinical AA and HL women( Reference Regan and Cachelin 39 ). External cues trigger impulsive binge eating episodes via their effects on reward and motivation centres of the brain( Reference Mathes, Brownley and Mo 38 , Reference Sobik, Hutchison and Craighead 40 – Reference Wardle 42 ). It is possible that FFR serve as binge triggers for those with a tendency to binge eat; therefore for bingers, greater FFR exposure may trigger more frequent binge episodes. In addition, FFR provide highly palatable, energy-dense foods to customers very quickly and conveniently, making impulsive binge eating very easy and convenient.
Binge eating is a shameful and secret behaviour for those who struggle with it( Reference de Zwaan 43 ). Binge eating is far more likely to occur at home( Reference de Zwaan 43 – Reference Abraham and Beumont 45 ), in the evening( Reference Smyth, Wonderlich and Sliwinski 46 ), on weekends( Reference Smyth, Wonderlich and Sliwinski 46 ) and when alone( Reference de Zwaan 43 – Reference Abraham and Beumont 45 , Reference Waters, Hill and Waller 47 ). In one study, 72 % of participants reported that going home after work or school was a binge trigger( Reference Abraham and Beumont 45 ). In another study, one-third of those with a tendency towards binge eating did so in the car( Reference Glass, Mitchell and de Zwaan 48 ). These common binge eating characteristics suggest that food cues in the neighbourhood environment around one's home may be more salient in influencing diet and weight status for binge eaters than non-binge eaters.
The aims of the current study were to determine: (i) whether binge eating moderated the association between neighbourhood FFR availability and diet (i.e. total energy intake and percentage of total energy intake from fat); and (ii) whether binge eating moderated the association between neighbourhood FFR availability and BMI. Neighbourhood FFR availability was operationally defined as an 800 m (0·5 mile) radius around each participant's residence. We hypothesized that: (i) the relationship between neighbourhood FFR availability and diet would be positive and stronger among bingers than non-bingers; and (ii) the relationship between neighbourhood FFR availability and BMI would be positive and stronger among bingers than non-bingers.
Method
Design and sample
A unique descriptive cross-sectional study was conducted using baseline data from a larger longitudinal, multisite, randomized controlled trial called Health is Power( Reference Lee, Medina and Mama 49 – Reference Lee, Mama and McAlexander 51 ). The purpose of Health is Power was to test a transcultural, community-based intervention to increase physical activity and improve dietary habits among AA and HL women from Houston and Austin, TX, USA( Reference Lee, Medina and Mama 49 , Reference Lee, Mama and Medina 50 , Reference Lee, O'Connor and Smith-Ray 52 ). Four hundred and ten apparently healthy AA and HL women (311 in Houston and ninety-nine in Austin) were recruited for Health is Power. In Houston, 84·6 % identified as AA and 15·4 % identified as HL; all women in Austin identified as HL. The study sample and design have been described previously( Reference Lee, Medina and Mama 49 , Reference Lee, Mama and Medina 50 ). However, briefly, an uneven sample design was used because it was determined that a smaller comparison group would provide enough power to determine effects; and in year 2, the funders cut the budget by over 25 % prematurely cutting off recruitment in the second site (Austin). Women who were recruited completed baseline questionnaires including the Binge Eating Scale (BES) and a demographic survey and had researchers assess their residential neighbourhoods. At baseline, these women were provided a run-in packet that included the National Cancer Institute's Dietary History Questionnaire (DHQ). The run-in packet method was used to encourage early withdrawal by those who are less motivated and likely to drop out later in the intervention. Women were randomly assigned to the intervention only when the run-in packet was returned.
Procedure
Individual data collection
The study protocol was approved by the University of Houston's Committee for the Protection of Human Subjects before recruitment began. Women were recruited via community advertisements throughout Houston and Austin to participate in a health promotion intervention. Interested participants contacted study staff, who conducted a telephone-administered screening( Reference Lee, Mama and Medina 50 ). Physically inactive women between 25 and 60 years old were invited to give written consent and complete a baseline (T1) health assessment( Reference Lee, Mama and Medina 50 ). At the T1 assessment, participants completed an interviewer-administered questionnaire, anthropometric measures of BMI and body fat, and were given a take-home packet to complete prior to the next meeting (approximately one week later). The packet contained more detailed questionnaires not found in the interviewer-administered questionnaire, including the DHQ( Reference Lee, Medina and Mama 49 , Reference Lee, Mama and Medina 50 , Reference Lee, O'Connor and Smith-Ray 52 – Reference Mama, Quill and Fernandz-Esquer 57 ).
Environmental data collection
To complete environmental assessments, neighbourhoods were first mapped using Geographical Information Systems (GIS) technology. Participants’ addresses were geocoded, and a participant's neighbourhood was defined as the area within an 800 m (0·5 mile) radius circumscribed around her home. Defining the neighbourhood as the area within the boundaries of the circle has several advantages that have been discussed exhaustively in previous work by the authors( Reference Lee, Medina and Mama 49 , Reference Lee, Booth and Reese-Smith 58 ). Advantages of using a 800 m circular buffer are: (i) it captures all area to which a resident may be exposed on a daily basis during both foot and automobile travels; (ii) the straight-line distance allows for capture of distance travelled on footpaths and other ‘short cut’ routes that may not be captured by using a street network strategy; and (iii) it may reduce the effect of spatial correlation that arises from using census boundaries where points near the boundary of the census area are influenced by factors in adjacent census areas. Next, an Intersect command in ArcGIS was used to combine the neighbourhood buffers and street centrelines to create a buffer streets layer. Field assessors completed an interactive training using standardized PowerPoint training slides with pictures and operational definitions over the course of half a day and completed at least 4 h of mentored field training. Environmental assessment procedures have been previously described in detail( Reference Lee, Medina and Mama 49 , Reference Lee, Mama and McAlexander 51 , Reference McAlexander, Mama and Medina 56 , Reference Lee, Booth and Reese-Smith 58 – Reference Lee, Heinrich and Medina 60 ). Assessors completed field assessments in teams of two and took GIS maps to guide them and ensure that all street segments were assessed. The Goods and Services Inventory (GASI) is an in-person, street-level neighbourhood audit measurement tool. Assessment teams of two people walked the segmented areas and counted the number of various types of goods and services (e.g. FFR, pawn shops) within the 800 m buffer using the GASI according to operational definitions( Reference Lee, Medina and Mama 49 , Reference Lee, Mama and McAlexander 51 , Reference McAlexander, Mama and Medina 56 , Reference Lee, Booth and Reese-Smith 58 – Reference Lee, Heinrich and Medina 60 ).
Individual measures
Demographics
The Maternal and Infant Health Assessment (MIHA) was used to measure the participant's education, parents’ education and income. The MIHA is modelled on the Centers for Disease Control and Prevention's Pregnancy Risk Assessment Monitoring System (PRAMS), and items have been used with ethnically diverse samples and socio-economic status categories( Reference Sarnoff and Hughes 61 ).
Binge Eating Scale
The BES is a self-report questionnaire that measures binge eating symptoms but does not provide a clinical diagnosis of binge eating disorder( Reference Gormally, Black and Daston 62 ). The BES has sixteen groups of items that describe both the behavioural manifestations and feelings/cognitions surrounding a binge episode( Reference Gormally, Black and Daston 62 ). Participants are asked to choose one statement in each group of items that best describes the way they feel; each item in a group of items represents a rating from 0 to 3( Reference Gormally, Black and Daston 62 ). Adding the responses to each question provides an overall score of binge eating, with a higher score indicating greater severity of binge eating symptoms( Reference Gormally, Black and Daston 62 – Reference Timmerman 64 ). Studies in samples of AA and white women have demonstrated strong internal consistency, with values of α ranging between 0·88 and 0·91( Reference Harrington, Crowther and Henrickson 65 , Reference Mitchell and Mazzeo 66 ). Studies in samples of Hispanic, AA and white women showed that the BES is a widely used valid measure of binge eating symptomatology( Reference Grupski, Hood and Hall 67 – Reference Goodrick, Poston and Kimball 70 ). Based on the criteria developed by Marcus et al.( Reference Marcus, Wing and Hopkins 71 ), participants were categorized into groups of non-bingers (BES score <18) and bingers (BES score ≥18).
Diet History Questionnaire
The National Cancer Institute's DHQ( Reference Subar, Thompson and Smith 72 , Reference Subar, Thompson and Kipnis 73 ) measured usual consumption of 124 food items over the past 12 months. The DHQ has adequate validity (r s = 0·49 in men, 0·48 in women) and reliability (r = 0·70 to 0·85) in large diverse samples when compared with other established and validated FFQ( Reference Subar, Thompson and Kipnis 73 , Reference Subar, Ziegler and Thompson 74 ). It has been widely used to assess diet among AA and HL populations since its development (e.g. references Reference Williams, Satia and Adair75–Reference George, Thompson and Midthune78). Total energy intake and the percentage of total energy intake from fat were calculated for the present study.
Environmental measures
The Goods and Services Inventory
Trained field assessors used the GASI( Reference Ledoux, Mama and O'Connor 79 , Reference Adamus, Lopez and Das 80 ) (© 2010) to tabulate all goods and services available within an 800 m (0·5 mile) radius of participants’ home addresses. The twenty types of goods and services included on the GASI are: (i) table-service restaurants, (ii) FFR, (iii) other types of restaurants, (iv) supermarkets, (v) grocery stores, (vi) gas stations/convenience stores, (vii) pharmacies, (viii) banks/credit unions, (ix) pawn shops, (x) cheque-cashing stores, (xi) liquor stores, (xii) tobacco stores, (xiii) bars or nightclubs, (xiv) adult video stores, (xv) sex-related businesses/adult sex clubs/strip bars, (xvi) places of worship, (xvii) salons/barbers/beauty shops, (xviii) schools, (xix) day cares and (xx) libraries, within a particular geographically defined area. The GASI has been validated and showed good inter-rater reliability in multiple cities( Reference Lee, Heinrich and Medina 60 ). The present study used only the items assessing FFR, as most foods served in these establishments contribute to a high-fat diet. An FFR was defined as a restaurant in which ‘Orders and food pick-up completed at the counter or from a car. There is no table service’. This includes restaurants that produce solely ‘carry-out’ food, and may or may not have a ‘drive through’. FFR did not include other types of table-service restaurants or convenience store foods.
Statistical analyses
Data were screened for data-entry errors or outliers before initiating data analysis. The data were not weighted individually, as would be done in a survey sample with probability of selection, since this was not a probability sample. A cluster command was not used because there were only two clusters, which creates a fixed difference not an intercluster variance. Including site as a covariate accounted for that fixed difference. Participants who reported eating <3347 kJ/d (<800 kcal/d) were considered outliers and excluded from analyses. After exclusions were made, a sample of 170 remained for study analyses. Preliminary data inspection confirmed assumptions of normality, homogeneity of variance, linearity and homogeneity of regression slopes. A series of 2 (bingers v. non-bingers) × 2 (0 neighbourhood FFR v. ≥1 neighbourhood FFR) ANCOVA with age, race and city of recruitment (i.e. Austin or Houston) serving as covariates were conducted to examine main and interaction effects on BMI, energy intake and fat intake. Analyses were performed using the statistical software package IBM SPSS Statistics 20. The level of significance was set at P < 0·05.
Results
Four hundred and ten women completed baseline data for the parent study. Two hundred and five participants did not return the run-in packets which included the dietary data and some were excluded because they reported consuming <3347 kJ/d (<800 kcal/d; n 17). There were no differences between those not included in the final data set (under-reporters or those without dietary data) and those who were on age, BMI, BES score or neighbourhood FFR availability. AA women were more likely to not report or under-report dietary intake than HL women (P = 0·03). Of the remaining 188 participants, 170 provided complete data on all study variables and were included in ANCOVA.
Of the total sample in the study, 115 participants (67·6 %) were non-bingers (scored <18 on the BES) and fifty-five (32·4 %) were bingers (scored ≥18 on the BES). Ninety-five participants had no FFR in their neighbourhood and seventy-five had ≥1 neighbourhood FFR (range: 1–15). Fifty-five per cent (n 89) of those who provided data on income had incomes >401 % of the federal poverty level, 44 % (n 70) had incomes 100–400 % of the federal poverty level, and 1 % (n 2) had incomes below the federal poverty level. See Table 1 for means and standard deviations on continuous variables related to sample characteristics.
Table 1 Characteristics of the study sample: African American (AA) and Hispanic/Latino (HL) women aged 25–60 years, Houston and Austin, TX, USA
BES, Binge Eating Scale; FFR, fast-food restaurant.
BMI
After adjusting for age, city and race, there was a main effect of binge eating on BMI (F (1, 163) = 5·53, P = 0·02), with a small effect size (partial η 2 = 0·03), but there was no significant main effect of neighbourhood FFR availability (F (1, 163) = 0·105, P = 0·75). After adjusting for age, city and race, there was a marginally significant interaction effect of binge eating and neighbourhood FFR availability on BMI (F (1, 163) = 3·61, P = 0·06), with a small effect size (partial η 2 = 0·002). Binge eaters with ≥1 FFR in their neighbourhood had higher BMI than binge eaters with 0 FFR in their neighbourhood, but non-bingers with ≥1 FFR in their neighbourhood had lower BMI than non-bingers with 0 FFR in their neighbourhood (see Fig. 1 and Table 2).
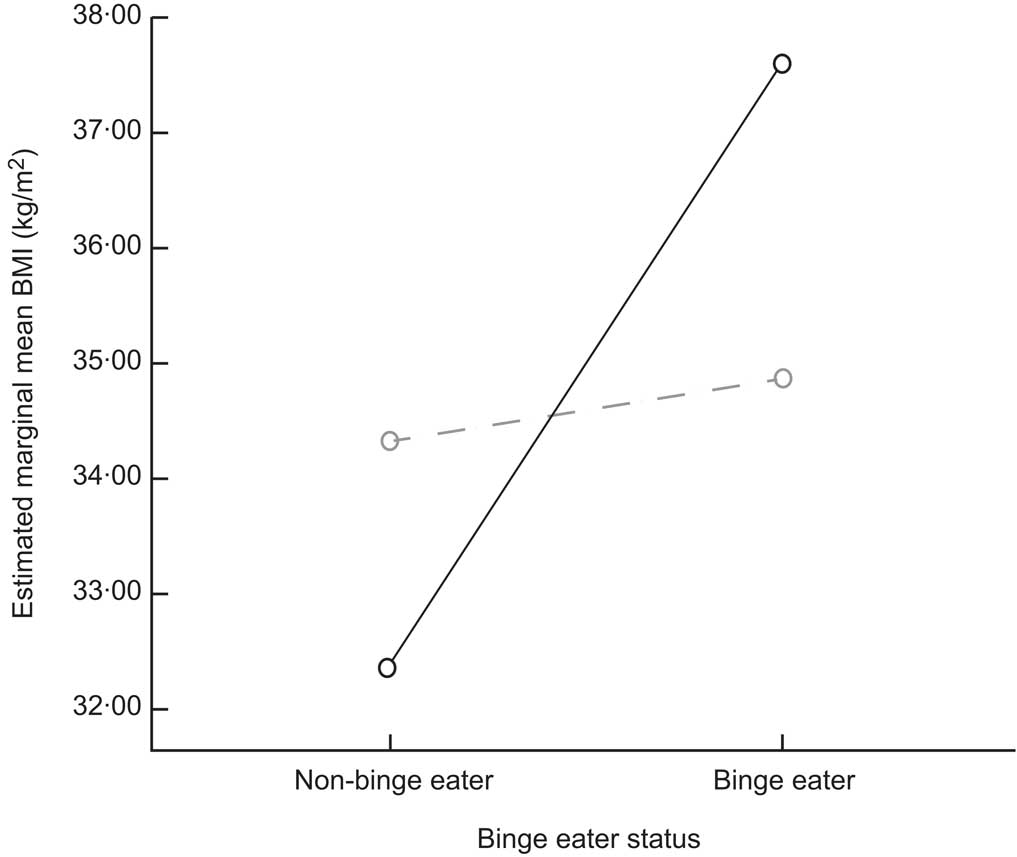
Fig. 1 Interaction effect of binge eater status and neighbourhood fast-food restaurant (FFR) availability (– – ○ – –, 0 FFR; ——○——, ≥1 FFR) on BMI among African American and Hispanic/Latino women aged 25–60 years, Houston and Austin, TX, USA. Covariates appearing in the model are evaluated at the following values: ethnicity (by identification) = 0·61, study site = 1·30 and age (years) = 45·7661
Table 2 Group means and standard deviations of BMI, total energy intake and percentage of total energy intake from fat according to neighbourhood fast-food restaurant (FFR) availability and binge eating: African American and Hispanic/Latino women aged 25–60 years, Houston and Austin, TX, USA
a,bMean values within a row with unlike superscript letters were significantly different (P < 0·05).
Total energy intake
After adjusting for age, race and city, there was a main effect of binge eating on total energy intake (F (1, 164) =5·50, P = 0·02), with a small effect size (partial η 2 = 0·03). Bingers had higher total energy intake than non-bingers (see Table 2). There was no significant main effect of neighbourhood FFR availability (F (1, 164) = 1·68, P = 0·20) and no significant interaction effect on total energy intake (F (1, 164) = 0·73, P = 0·39).
Percentage of total energy intake from fat
After adjusting for age, race and city, there was a main effect of binge eating on percentage of total energy intake from fat (F (1, 164) = 5·78, P = 0·02), with a small effect size (partial η 2 = 0·03). Bingers consumed a higher percentage of their total energy intake from fat than non-bingers (see Table 2). There was no significant main effect of neighbourhood FFR availability (F (1, 164) = 0·28, P = 0·60) and no significant interaction effect on percentage of total energy intake from fat (F (1, 164) = 1·05, P = 0·31).
Discussion
The purpose of the present study was to determine whether there was a combined effect of neighbourhood FFR availability and binge eating status on BMI and diet among AA and HL women. The average fat intake was 35·77 % of total daily energy intake, which exceeds national recommendations of ≤30 % of total daily energy intake from fat( 81 ). Obesity status and diets high in fat pose significant risks for chronic diseases such as heart disease and diabetes( Reference Mente, de Koning and Shannon 4 – Reference Kirkpatrick, Dodd and Reedy 7 ). Tailored interventions for AA and HL women are needed to improve diet and reduce weight status, thereby reducing risks for chronic diseases.
Results showed a marginally significant small interaction effect of neighbourhood FFR availability and binge eating on BMI, but no interaction effect on energy or fat intake. These results are consistent with a recent systematic review which concluded that the relationship between environment and BMI was more consistently demonstrated than the relationship between environment and diet( Reference Giskes, Van Lenthe and Avendano-Pabon 82 ). The major limitation of assessing diet is that nearly all measures of diet are self-reported, thus the prevalence of reporting bias and errors is high( Reference Livingstone and Black 83 , Reference Klesges, Baranowski and Beech 84 ). Under-reporting has been shown to be particularly prevalent among female, obese and ethnic minority adults( Reference Livingstone and Black 83 ), which includes the women in the present sample. Among bingers and obese non-bingers, under-reporting has been shown to occur by as much as 20 to 33 %( Reference Raymond, Peterson and Bartholome 85 ). Social desirability contributes to under-reporting( Reference Klesges, Baranowski and Beech 84 ). For those who are ashamed of what or how much they eat (e.g. bingers), social desirability may lead to substantial under-reporting of dietary intake. Finally, dietary intake of foods eaten during binge episodes may not have been captured by the dietary assessment measure used in the present study (i.e. DHQ). Binge episodes may have been viewed as abnormal and excluded when asked to report ‘usual’ intakes over the last 12 months as instructed. Studies have shown that dietary intake varies widely between binge and non-binge days( Reference Raymond, Peterson and Bartholome 85 , Reference Reeves, McPherson and Nichaman 86 ). BMI measurements, while imperfect, are an objective measure with less variability due to reporting bias. Environmental associations based on BMI data may carry more validity than those based on dietary assessment data.
Results provide some evidence to suggest that the impact of neighbourhood FFR availability on BMI may depend on binge status; bingers with at least one neighbourhood FFR had higher BMI than bingers without neighbourhood FFR or non-bingers regardless of neighbourhood FFR. Among studies that have examined the association between neighbourhood FFR availability and BMI, one has confirmed this relationship( Reference Fleischhacker, Evenson and Rodriguez 30 ). Results of the present study suggest that the moderating effect of binge eating may explain why the environment has an effect on weight status among some people but not everyone. Results are consistent with recent work from a Canadian group of researchers who showed that there was a stronger association between neighbourhood FFR availability and metabolic risk factors among individuals who had a low sense of control over their environment compared with individuals who had a strong sense of environmental control( Reference Paquet, Dube and Gauvin 35 ). Similarly, binge eating is characterized by loss of control over eating( Reference Mathes, Brownley and Mo 38 ). Additional research by the same Canadian group showed that there was a stronger association between neighbourhood FFR availability and fast-food consumption among individuals who were sensitive to external cues compared with those who were not( Reference Paquet, Daniel and Knauper 36 ). Laboratory human and animal studies have shown that external cues promote binge eating and overeating in the absence of hunger among bingers but not among non-bingers( Reference Mathes, Brownley and Mo 38 ). FFR are often chain franchises with an easily recognizable and distinct store front associated with a specific standardized menu and flavour/quality of highly palatable but unhealthy food( Reference Prentice and Jebb 16 , Reference Lin, Frazao and Guthrie 17 ). Fast-food cravings have been related to greater frequency of eating out( Reference Siwik and Senf 87 ). Among those prone to binge eat, learned associations between the features of FFR and the rewarding properties of fast food may lead to cravings and loss of control, resulting in overeating upon exposure to FFR( Reference Mathes, Brownley and Mo 38 ).
Roughly one-third of the women in the present study were bingers. This is remarkable, as previous reports showed that 15–20 % of a non-clinical multi-ethnic sample were bingers( Reference Regan and Cachelin 39 ). Bingers in the present sample had higher energy intake and higher fat intake than non-bingers but these effects were small. The literature suggests that diets among bingers and non-bingers differ depending on whether the measured day was a binge day or not. On binge days, bingers have greater energy and fat intakes than on non-binge days( Reference Raymond, Peterson and Bartholome 85 , Reference Reeves, McPherson and Nichaman 86 , Reference Raymond, Neumeyer and Warren 88 ). Binge frequencies vary but generally do not occur daily, except in the most extreme cases( Reference Allison and Timmerman 89 ). Energy and fat intakes do not differ significantly among obese non-bingers and bingers on non-binge days, but on binge days energy and fat intakes are significantly higher among bingers than obese non-bingers( Reference Raymond, Peterson and Bartholome 85 , Reference Raymond, Neumeyer and Warren 88 ). Compared with obese non-bingers, obese bingers consume more energy during a laboratory ad libitum eating episode( Reference Raymond, Bartholome and Lee 90 ). In the current study, it is possible that the differences in energy and fat intakes between bingers and non-bingers were driven by binge and non-binge day differences in diet.
Strengths of the present study include a large diverse sample, meticulous and detailed objective measurement of neighbourhood food stores, and use of widely used validated measures of study variables. The BES was used to identify those who are prone to binge eating. Scores on this measure are correlated with binge eating disorder, but alone do not provide enough information for a definitive clinical diagnosis. Binge eating in the present study was merely one type of eating behaviour, not a diagnosis. The study sample represented healthy, middle-aged, overweight/obese women with moderate incomes who do not engage in physical activity regularly; therefore results are generalizable only to women who meet these criteria.
The present study has limitations worth noting. It was cross-sectional, which means that causality cannot be inferred from the results. AA women were more likely than HL women to under-report dietary intake data and drop out of the study early, so generalizability of the study's results is limited to those AA women who are likely to participate in a diet and physical activity intervention study (i.e. the parent study). The small sample size may have reduced the ability to detect true interaction effects. While the DHQ is widely used among minority populations and it was validated on diverse samples, the validation samples contained a larger proportion of whites than any other racial/ethnic background. Also, the DHQ could be considered a type of FFQ, which has been shown to have slightly poorer reliability and validity than other dietary assessment methods like 24 h dietary recalls when compared with biomarkers of dietary intake and energy expenditure (e.g. doubly labelled water)( Reference Livingstone and Black 83 , Reference Subar, Kipnis and Troiano 91 , Reference Trabulsi and Schoeller 92 ). Benefits of FFQ are that they are far more cost-effective and feasible than 24 h dietary recalls and far less burdensome on participants than food diaries. For these reasons, they are still widely used in public health research including national surveillance systems (Behavioral Risk Factor Surveillance System).
Existing dietary assessment methods may be particularly problematic for bingers; therefore research may be needed to develop dietary assessment measures specifically for bingers to address binge and non-binge day variations. Bingers in the present sample had higher energy intake and higher fat intake than non-bingers but these effects were small. It is likely that differences in diet on binge days v. non-binge days may be driving the differences in diet between bingers and non-bingers. Future research should determine whether reducing binge frequency without necessarily addressing diet composition would reduce overall intakes of energy and fat among bingers.
Conclusion
High-fat diets and binge eating were common among the AA and HL women in the present sample. These results demonstrate the need for tailored interventions for AA and HL women to reduce energy and fat intakes and BMI. The influence of neighbourhood FFR availability on BMI depended on binge status; bingers with at least one neighbourhood FFR had higher BMI than bingers with no neighbourhood FFR or non-bingers regardless of neighbourhood FFR availability. These results provide some insight into why some but not all individuals may be prone to obesity and overeating in an environment with high availability of FFR. Future research should continue to identify the features of FFR that may promote binge eating among bingers, and also identify additional individual factors that may make some more sensitive to obesity and overeating in response to obesogenic environmental conditions. Additional research should also identify other environmental factors bingers may be sensitive to. Results of these studies would be useful in informing policies to reduce obesogenic features of the environment and also to inform individual-level treatments for obese individuals with binge eating tendencies (e.g. coping with FFR).
Acknowledgements
Sources of funding: This work was supported by the Health is Power study funded by grant 1R01CA109403 from the National Institutes of Health (NIH), National Cancer Institute (NCI) awarded to R.E.L. at the University of Houston. The NIH and NCI had no role in the design, analysis or writing of this article. Conflicts of interest: There are no conflicts of interest to report. Authors’ contributions: T.L. designed the study, conducted analyses and prepared the manuscript; H.A.-L. prepared portions of the manuscript and reviewed drafts of the manuscript; D.P.O. conducted statistical analyses, assisted with the study design and reviewed drafts of the manuscript; S.M. was Project Coordinator on the parent study, facilitated data collection and prepared portions of the manuscript; R.E.L. was Principal Investigator on the parent study, designed the parent study, reviewed drafts of the manuscript and supplied the data. Each author has seen and approved the contents of the submitted manuscript.





