Adolescence is a critical period in the lives of young people and a time to reap lasting benefits from interventions that improve nutrition and maternal and child health. As suggested in the 2013 Lancet series on nutrition, the focus on nutritional interventions for adolescents is warranted as “interventions to improve nutrition and child development during this period have high rates of return”(Reference Ruel and Alderman1). This conclusion is based on recognition of nutrition’s impact on future productivity, maternal and child health and child growth and cognitive development. Nutrition during adolescence potentially can contribute to a range of health and development outcomes for young women and the health of their families(Reference Taylor, Dangour and Reddy2,Reference Keats, Rappaport and Shah3) .
The government of Zambia has committed to improving the nutritional status of adolescents, pregnant women and their children. Nonetheless, adolescent girls in Zambia remain at risk for macro- and micronutrient deficiencies that have deleterious impacts on growth, development and maternal and child health(4–Reference Ji, Cui and Liu6). Among non-pregnant adolescents 15–19 in Zambia, 16 % are undernourished (5 % severely) and 3 % stunted(4). Among children less than five years old, 40 % are stunted and 15 % are underweight for their age(4). A high prevalence of anaemia (28 %) also has been reported among reproductive-aged women(4). Dietary iron needs increase during adolescence, and iron-deficient anaemia in late childhood and adolescence is associated with neurological impairment, lower physical endurance and decreased immune function(Reference Brabin and Brabin5,Reference Grantham-McGregor and Ani7–Reference Ekiz, Agaoglu and Karakas10) . Additionally, anaemia in pregnant adolescents can result in premature births and low birth weights, with offspring at risk for anaemia-related cognitive and growth deficits(Reference Scholl and Hediger11). In Zambia, an estimated 29 % of girls aged 15–19 years have experienced pregnancy, yet only 55 % of pregnant women in this age group used oral iron supplementation for ≥90 days during their last pregnancy, with 4 % not receiving any iron supplementation(4).
While nutritional education may not be sufficient to produce adolescent behaviour change(Reference Naeeni, Jafari and Fouladgar12), nutritional knowledge is considered one of a basket of critical factors required to promote positive changes in diet and health(Reference Brug13–Reference Worsley15). The Nutrition Education in Basic Schools programme targeting Zambian children at grades 2, 4 and 6 led to increases in nutritional knowledge, but limited behavioural changes, possibly due to limited autonomy and family financial conditions(Reference Sherman and Muehlhoff16). There is a lack of evidence regarding the effect of nutritional education on health behaviour and outcomes in adolescents, particularly when provided as part of a comprehensive, adolescent-focused empowerment programme. This paper reviews the impact of a nutritional education module embedded within a broader adolescent girls’ empowerment intervention. It is hypothesised that by providing adolescents with tailored nutritional information in the context of a multi-health, multi-sectoral empowerment programme, we will observe significant improvements in adolescent nutritional knowledge, better dietary practices and improved nutritional indicators for adolescents and their children.
Methods
Intervention design
The nutritional intervention evaluated here was conducted in Zambia as a sub-study of the Adolescent Girls Empowerment Program (AGEP). The AGEP intervention targeted approximately 11 000 vulnerable adolescent girls 10–19 years old in 2013 and was implemented over 2 years, starting in mid-2013, with implementation initiation staggered by study site. AGEP was implemented in ten total sites (five urban and five rural), within four of Zambia’s ten provinces: Lusaka, Central, Copperbelt and North-Western provinces. The selection of provinces was purposeful based on programmatic objectives, although study sites within the provinces were randomly selected. In urban areas, programme sites were geographically compact, high-density housing compounds, while in rural areas, sites encompassed numerous square kilometres. Programme sites were further divided into geographic clusters, which were randomly selected to receive different components of the AGEP programme (described below). The geographic demarcation of a cluster was based on census supervisory areas, as delineated by the Zambia Central Statistical Office. Eligible adolescent girls were selected from a household census conducted in the study sites. The most vulnerable adolescent girls were selected to receive invitations to the programme via a vulnerability score, which was generated through an analysis of whether the girl was behind in school grades completed relative to her age(Reference Hewett, Austrian and Soler-Hampejsek17). A more complete description of AGEP and technical design details of its evaluation are in the published study protocol and baseline report(Reference Hewett, Austrian and Soler-Hampejsek17,Reference Hewett, Austrian and Soler-Hampejsek18) .
AGEP was a direct-to-girls asset-building programme, focusing on developing girls’ health, economic and social assets by building and improving their knowledge, self-efficacy, aspirations and resource access. The central element of AGEP was weekly girls’ group meetings conducted over 2 years in which 20–30 girls met with a programme-trained mentor to discuss a curriculum-guided topic, as well as to discuss personal matters and to socialise. The weekly groups were stratified by age (10–14, 15–19 years) and marital status, so that the girls received age-appropriate programme content. In addition to the weekly girls’ group meetings, through random assignment at the cluster level within programme sites, a subset of girls was offered the option of opening an adolescent-friendly bank account at the National Savings and Credit Bank of Zambia. Similarly, through random assignment at the cluster level, a subset of girls was offered health vouchers for reproductive health services at partner public and private healthcare facilities(Reference Hewett, Austrian and Soler-Hampejsek17).
Within the weekly girls’ groups meetings, three core curricula were used by the mentors to guide the individual sessions: (1) health and life skills, (2) financial education and (3) a nutritional curriculum. The AGEP nutritional curriculum was tailored to provide age-appropriate information through six weekly sessions on nutrition: (1) Nutrition Needs for Adolescent Girls; (2) the Role of Food in the Body; (3) Anaemia in Adolescent Girls; (4) Nutrition for Pregnant Adolescents; (5) Infant Feeding from Birth through Six Months and (6) Young Child Feeding and Growth Monitoring. Girls aged 15–19 years took part in all six sessions, while girls aged 10–14 years participated in the first three sessions. Sessions were conducted over consecutive weeks and were repeated in programme years one and two. The curriculum used innovative educational and interactive components whose objective was to maximise knowledge acquisition and engagement of the girls, without being didactic.
Evaluation design and sample
The evaluation reported here was based on a nested, single-blinded randomised cluster design within a larger impact evaluation of the AGEP programme. Geographic clusters within the ten selected AGEP sites were first randomised through public lottery at each of the ten study sites to the three programme arms (forty clusters per arm) or to control (forty clusters). The main AGEP impact evaluation had three intervention arms (weekly girls’ groups only; weekly girls’ groups + health vouchers; weekly girls’ groups + health vouchers + savings accounts); these are not further discussed as they do not have an impact on the analysis or results presented here(Reference Austrian, Soler-Hampejsek and Behrman19).
The study-participant flow diagram is presented in Fig. 1. A total of 4661 (87 %) adolescent girls completed the AGEP baseline survey among a sampled eligible population of 5304 for the main research study (including intervention and control areas); a parallel selection process was used to identify the control participants(Reference Hewett, Austrian and Soler-Hampejsek17). Eligibility criteria included being, in 2013, age 10–19 years, never-married, residing in selected study clusters and randomly selected for participation; selection of girls was stratified by site and age group. Of the 3515 girls invited to participate in AGEP, 2660 (76 %) attended at least one AGEP girls’ group session. Significant predictors of participation in AGEP included living in rural areas, being younger, attending school, having basic numeracy skills and being the biological daughter of the head of household(Reference Hewett, Austrian and Soler-Hampejsek17).
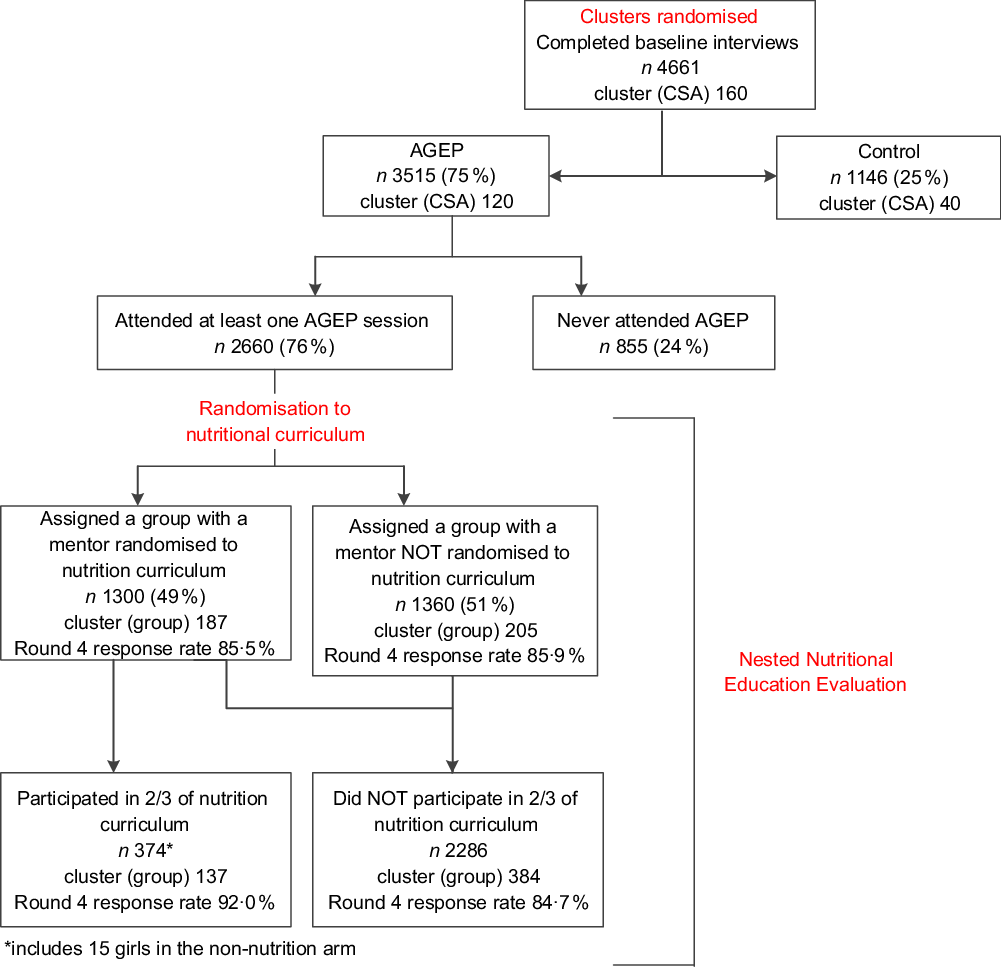
Fig. 1 Study-participant flow diagram
The nested nutrition evaluation was based on a second level of randomisation, with the mentors of the adolescent girls’ groups randomised to one of two study arms through an ordered random number generation in Microsoft Excel®: (1) an intervention arm composed of weekly girls’ groups assigned the nutritional curriculum or (2) a control arm consisting of weekly girls’ groups not assigned the nutritional curriculum. Of the 392 AGEP weekly girls’ groups, 187 (48 %) were assigned the nutritional curriculum in their sessions, with 1300 girls (49 %) exposed. The remaining 205 groups (52 %) were assigned to not use the nutritional curriculum, including 1360 girls (51 %) not exposed. Of all girls attending AGEP weekly girls’ groups at least once, 374 girls (14 %) participated in two-thirds or more of sessions that included discussions of the nutritional curriculum.
Survey instruments and measures
Comprehensive annual surveys were conducted at baseline in 2013 (Round 1) and for 4 subsequent years, through 2017 (Round 5). Survey data from Rounds 1–4 are used in this paper, as we expect impact of the intervention to be first observed in Round 4. The Round 4 data represent information collected from adolescents 1 year after the AGEP programme was completed and the nutritional education ended. The survey instruments measured a wide range of adolescent attitudes, behaviours, transitions and outcomes. Survey instruments were implemented using electronic data capture. All questionnaires were translated into Nyanja, Bemba and Kaonde, the primary languages spoken in the programme areas. Literacy was measured by whether the respondent could read simple sentences out loud in Nyanja, English or another local language of their choice (Bemba and Kaonde). Numeracy was accessed using progressively more difficult questions selected from Zambia Ministry of Education textbook for grade three; tasks included ordering numbers, addition, subtraction, multiplication, division, fractions and simple word problems. A cognitive assessment was conducted using a subset of the Raven’s Coloured Progressive Matrices. Household wealth was measured using a series of questions about asset ownership (radio, TV, phone, table, etc.) and housing quality (toilet facilities, floor materials); a score was created from principal components analysis, separately for urban and rural households.
Micro and macro dietary composition was measured based on self-reported nutritional intake in the 24 h prior to the interview for the adolescents and their children 2 years or older; only the Round 4 data were used. Dietary diversity for the adolescents was computed using the Minimum Dietary Diversity for Women, which defines diversity as consuming at least five out of ten food groups in the previous 24 h prior to the interview: (1) grains, white roots, tubers and plantains; (2) pulses; (3) nuts and seeds; (4) dairy; (5) meat, poultry and fish; (6) eggs; (7) dark green leafy vegetables; (8) Vitamin A-rich fruits and vegetables; (9) other vegetables and (10) other fruits(20). The survey instrument combined response categories for food groups 2 and 3 and 9 and 10, and we scored our Minimum Dietary Diversity for Women twice if they responded positively for these combined categories. Therefore, our indicator of Minimum Dietary Diversity for Women may be biased towards overestimating dietary diversity. We expect, however, the bias will be distributed equally across randomised groups and therefore does not affect the results of the impact assessment. Eating iron-rich foods was based on recall of eating organ meat, beef, pork, lamb, goat, chicken, duck and fish. Eating Vitamin A-rich foods was based on reported consumption of plant and meat-based sources, including pumpkins, carrots, squash, yellow or orange sweet potatoes, dark green vegetables, mangoes, papayas, apricots, watermelon, meat, eggs or milk products.
Girls’ attendance at each of the girls’ group meetings was recorded by mentors. The curriculum topic and sub-session covered were also recorded, providing measures of exposure by curriculum topic. The monitoring data of the sessions allowed for measurement of whether the adolescents attended two-thirds or more of sessions including the nutritional curriculum. The monitoring data were collected using Open Data Kit with Android smart phones and synced to AGEP’s cloud-based monitoring platform and were uploaded on a weekly basis.
Anthropometric measurements
For the adolescent girls and their children aged 2 years or older, height was measured by the study enumerators to the nearest 0·1 cm using SECA® 217 portable stadiometers positioned on hard and flat surfaces. For infants younger than 2 years of age, body length was recorded using an SECA® 417 infant measuring board with the children lying on their backs. Adolescents and children who could stand independently were weighed to the nearest 0·1 kg on a digital scale (SECA® 874); infants were weighed while being held by their mother. For children aged 6–59 months, mid-upper arm circumference (MUAC) to the nearest 0·1 cm was obtained using UNICEF MUAC measuring tapes; moderate to severe malnutrition was designated as a MUAC of under 12·5 cm. Anthropometry z-scores for adolescents who were 10–14 at baseline, as well as all children under 5 years old at Round 4, were calculated using the Zanthro command in Stata 13.0, based on WHO reference populations(21). BMI (weight[kg]/height[m2]) was used for nutritional status for adolescents who were 15–19 years of age at baseline. Any children with MUAC below the WHO criteria (<11·5 cm) for severe acute malnutrition were referred to local health facilities for further evaluation and counselling.
Anaemia testing
Anaemia testing was added at survey Rounds 3–4 and conducted for adolescents aged 15 years and older and any of their children aged 6–59 months. Anaemia was measured with the point-of-care HemoCue® Hb 201 testing system using handheld testing spectrophotometers, capillary blood samples and a microcuvette blood collection device(Reference Sharman22). Results were obtained immediately. Designations of severe, moderate and mild anaemia based on haemoglobin levels were determined by age-appropriate WHO guidelines for women (by pregnancy status) and children between 6 and 59 months. Designations were also adjusted for elevation (below 1000 m; 1000–1499 m, 1500 m and above); Garmin® eTrex 10 handheld GPS Navigators were used to measure altitude(23,24) . After testing, the adolescents were provided information about anaemia symptoms and behaviours to reduce anaemia. Referrals to the local health facilities were provided to participants who were found to be moderately or severely anaemic.
Sample sizes estimates and statistical methods
Minimal detectable effect sizes (MDES) given a fixed number of clusters and girls per cluster for the nutritional indicators were calculated, accounting for statistical power (0·80), significance of α (0·05) and effect-size variability (0·05). The MDES were calculated using Optimal Design Software version 3.0 for a multi-site randomised trial with treatment at the cluster level(Reference Spybrook, Bloom and Congdon25). For example, the MDES for adolescent girls’ anaemia were determined to be ten percentage points difference between treatment (receiving nutritional curriculum) and an estimated anaemia prevalence of 22 % in the control sample. The MDES for children’s anaemia were 16 percentage points difference between treatment (mothers’ receiving nutritional curriculum) and an estimated anaemia prevalence of 53 % in children born to mothers in the control sample. Note that the power calculations and MDES were considered conservative estimates as greater power was expected because covariates would be introduced in estimation.
Means and 95 % CI were estimated for key characteristics for each treatment and control group. To check for potential pre-intervention differences, Pearson chi-square tests for categorical variables and linear regressions for continuous variables, accounting for sample clustering, were used. Means and 95 % CI were also estimated for all outcome variables measured pre- (if available) and post-intervention. Pre-post intervention changes were evaluated, and P-values obtained using McNemar’s χ 2 test. The primary analysis to assess the impact of the interventions estimated the impact of the “intent-to-treat” (ITT) using a difference-in-differences approach for outcomes that were measured pre- and post-intervention, and a simple difference approach for outcomes measured only post-intervention. The ITT was defined for girls assigned to AGEP groups randomised to the nutritional curriculum, irrespective of girls’ actual exposure to the curriculum material. Generalised least squares regressions with girl-level random effects were estimated to obtain the difference-in-differences coefficients. Linear regressions were estimated to obtain the simple difference coefficients, and logistic regressions were also estimated for binary outcomes. All regressions were estimated with robust se accounting for clustering at the weekly girls’ group level(Reference Hewett, Austrian and Soler-Hampejsek17). For adolescent outcomes, the regressions were estimated including site fixed effects and covariates for select individual- and household-level characteristics measured at baseline. For child outcomes, models controlled for site fixed effects, child age and sex.
To account for various levels of participation in AGEP due to programme drop-out or absences, and thus different exposures to the nutritional curriculum, a secondary analysis was conducted that assessed impact of the “treatment on the treated” for the nutritional curriculum intervention. To statistically account for selectivity of exposure, the treatment on the treated analysis was conducted as a two-stage, instrumental-variables (IV) estimation, with the first stage predicting participation of the adolescent in at least two-thirds of the nutritional sessions (four of six sessions for 10–14- year-olds; eight of twelve sessions for 15–19-year-olds). The instrument in the first stage is whether the group that the girl had been assigned to was led by a mentor randomised to the nutritional curriculum. Generalised two-stage least squares IV regressions with girl-level random effects and bootstrapping to account for clustering at AGEP groups were estimated to obtain the difference-in-differences coefficients. Two-stage least squares IV regressions with clustered se were estimated to obtain the simple difference coefficients. The validity of the instrumental variable was assessed with F-tests on excluded instruments, the Wald F-statistic and the Hansen statistic for over-identification. All regressions were estimated in Stata® 13.0.
Finally, to test whether the treatment had differential impacts across sub-groups of girls, all regressions were re-estimated including interaction terms with key characteristics of interest, specifically educational attainment and household wealth at baseline. For example, to test whether in the ITT analysis the intervention had higher impact for girls with higher grade attainment, the ITT regressions were re-estimated including interactions of the difference-in-differences with a variable indicating the highest grade the girl had completed. The coefficient of this interaction indicates whether the impact of the intervention differs by girls’ grade attainments.
Results
Descriptive results
As is indicated in Table 1, a total of 2660 baseline AGEP participants were included in the analytical sample for the nested nutritional evaluation. The response rates across the survey rounds are similar across the randomised groups and are not statistically significantly different in any round of survey. Non-response by Round 3 is approximately 10 % against baseline, which increases to 15 % against baseline by Round 4. Analysis of attrition (not shown) indicates that while attrition is correlated with baseline covariates, it is independent of the intervention arms; those who participated in the nutritional curriculum were no more likely to be retained in the study than those who did not.
Table 1 Analytical sample response rates, by survey round and evaluation group

AGEP, Adolescent Girls Empowerment Program.
Tested for differences between arms with χ 2 tests, no significant differences found.
Excludes 1146 AGEP control and 855 girls who never attended AGEP and therefore were never assigned a nutrition-randomised mentor.
The baseline characteristics of the sample originally eligible for inclusion in the evaluation are presented in Table 2; no statistically significant differences across the randomised nutritional study arms were observed. The adolescents were, on average, 14 years old and had completed a little more than 5 years of schooling, which is less than the expected six to seven grades of schooling to be completed by age 14 in Zambia. Although a sizable percentage (approximately 80 %) of girls were in school at baseline, their ability to read simple sentences in English or a local language, complete grade-appropriate numeracy evaluations and perform well on cognitive exams suggest deficiencies in the acquisition of academic and other skills. Finally, the data indicate that one-third of girls do not co-reside with their mothers, with a bit more than one-tenth having mothers that are deceased. Fathers’ co-residence is even less common, with more than half not living with their fathers and nearly a quarter having deceased fathers.
Table 2 Sample baseline characteristics by evaluation group (% unless otherwise indicated)

AGEP, Adolescent Girls Empowerment Program.
Clustered by census supervisory area.
* Pearson χ 2 tests for categorical variables and linear regression for continuous variables.
† Household wealth was measured at household census completed before baseline.
Table 3 shows univariate descriptive statistics for nutritional indicators of interest (knowledge, behaviour, nutritional outcomes) for adolescents at Round 1 and Round 4. Indicators not measured at baseline do not have values in the appropriate cells of the table. Thinness was not included in the impact analysis that follows due to low sample variances, while the indicator for obesity was combined with overweight in the impact analysis.
Table 3. Study Round 1 and Round 4 adolescent nutritional indicators (%, 95 % CI)

MDD-W, Minimum Dietary Diversity for Women.
CI clustered by programme group.
Indicators not reported at baseline were not measured until Round 3 of data collection (after the programme was complete).
P-values reported from McNemar’s χ 2 tests comparing baseline and Round 4 values.
* Sample sizes vary according to outcome.
† Defined as consuming at least five out of ten food groups in the previous day prior to the interview. The survey instrument combined food groups 2 and 3 and 9 and 10 and therefore MDD-W may be over-estimated in the sample.
‡ All currently pregnant girls excluded from BMI analyses.
Nutritional knowledge
By Round 4, basic nutritional knowledge was quite limited among the sample of girls, with only one out of four girls able to correctly identify six foods as being healthy (e.g., vegetables) or unhealthy (e.g., foods with lots of salt). Further less than half the sample of girls were able to correctly identify at least one cause of anaemia (e.g., poor nutrition) and one symptom of anaemia (e.g., being tired, feeling weak). Among older adolescents aged 15 years and older, knowledge of proper infant feeding (e.g., duration of exclusive breast-feeding) was also limited, with only one in five girls able to answer at least three of four questions correctly; being pregnant at interview had no significant impact on pregnancy-related nutritional knowledge (results not shown). When analysed by age (results not shown), a greater percentage of girls aged 15 years and older displayed retained knowledge for all variables compared to younger girls (all at P < 0·01).
Nutritional behaviour
Only approximately 35 % of adolescents at baseline and 59 % at Round 4 had sufficient dietary diversity (Minimum Dietary Diversity for Women ≥ 5) to obtain adequate micronutrients. Additionally, only 67 % had eaten food at Round 4 that was iron rich in the previous 24 h; despite increased iron needs for older adolescents and pregnant girls, these two groups were not more likely than younger or non-pregnant girls to consume iron-rich foods (data not shown). Near universal intake of vitamin A foods was achieved due to a significant percentage of girls who ate dark green, leafy vegetables (94 % at Round 4). Trend comparisons of behaviours indicate improved nutritional intake as the girls aged, with the trends in all indicators statistically significant at P < 0·001.
Nutrition-related outcomes
Of girls aged 10–14 years at baseline, approximately, 17 % at baseline and 13 % at Round 4 could be considered stunted given their height for age. The decline in stunting is significant over time (P < 0·001). While very few adolescent girls who were 10–14 years old at baseline were thin at Round 4 when they were 13–17 years old, a moderately higher percentage (9 %) of older girls who were 18–23 years old at Round 4 were underweight. As girls aged, there was an observed increase in being overweight (P < 0·001) for all girls and being obese for the older girls (P < 0·05). Finally, one of the more prevalent indicators of nutritional problems for adolescent girls was anaemia, with just over one-fifth of sample of older adolescents being moderately or severely anaemic and an additional one-fifth being mildly anaemic at Round 4.
Child outcomes
The nutritional indicators at Round 4 for children less than 5 years of age born of the adolescents in the analysis sample are presented in Table 4. While 97 % of children under the age of 6 months were currently breast-feeding, only 78 % of children under the age of two were still breast-feeding. The decline in breast-feeding occurred predominantly after the first-year of birth, as 96 % of children less than one were reported to be still breast-feeding. Just under two-thirds of children aged 2 years or older had eaten iron-rich foods and 95 % had eaten vitamin A-rich foods in the previous day.
Table 4 Round 4 child nutritional indicators

Clustered by programme group.
* Sample sizes vary by outcome due to age restrictions.
The nutritional status of children under 5 years in the sample indicates a range of nutritional concerns. Over 40 % of children under 5 years were stunted, with stunting more prevalent in males relative to females (47 % v. 36 %, P < 0·001). Stunting was significantly higher for children older than 1 year (when complementary breast-feeding declines), relative to children under age 1 (55 % v. 18 %, P < 0·001); a pattern observed elsewhere(4,Reference Victora, de Onis and Hallal26) . A sizable percentage (12 %) of the sample were underweight and 4 % of children under 5 years were wasted; although at the time of the survey, moderate to severe malnutrition as measured by the MUAC was low. Additionally, half the children had moderate or severe anaemia, with males exhibiting higher rates of anaemia than females (54 % v. 47 %), although the difference was not statistically significant. Children aged between 6 months and 1 year also had higher rates of anaemia than older children (69 % v. 45 %, P < .001).
Impact results
Table 5 presents the estimated impacts of the nutritional curriculum intervention on outcomes for the adolescents and their children on measures that had sufficient variation to assess impact from Tables 3 and 4. The results for adolescents are presented in the top panel; results for their children are in the bottom panel. All models are adjusted for site fixed effects and baseline covariates identified in Table 2.
Table 5 Summary of intent-to-treat (ITT) and treatment-on-treated (TOT) results of nutrition curriculum on nutritional outcomes of adolescents and their children

AGEP, Adolescent Girls Empowerment Program.
All adolescent models control for time since baseline and include the following covariates measured at baseline: programme site, age, school attendance, grade attainment, literate (any language), numeracy score, cognitive score, mother alive/coresident, father alive/coresident, and wealth quintiles. Models for child outcomes include only programme site, child’s age, and child’s sex as covariates.
Treatment in TOT estimates was defined as whether a respondent attended 2/3 of the nutrition sessions (defined as four of six sessions if 10–14 at baseline or eight of twelve sessions if 15–19 at baseline), instrumented by whether the respondent was assigned to a mentor who was randomised to the nutrition curriculum. (A less treatment variable, defined as two sessions if 10–14 at baseline or four sessions if 15–19 at baseline, was also assessed and no meaningful differences were found in the results.)
* ITT coefficients were estimated from logistic regressions for binary outcomes and linear regressions for continuous outcomes clustered by AGEP group. TOT coefficients were estimated from two-stage least squares instrumental variables regressions clustered by AGEP group.
† ITT difference-in-difference coefficients were estimated using generalised least squares regressions with girl-level random effects and robust se clustered by AGEP group. TOT difference-in-difference coefficients were estimated using generalised two-stage least squares instrumental variables regressions with girl-level random effects and bootstrapping to account for clustering by AGEP group.
The ITT and treatment on the treated results indicate that exposure to the nutritional curriculum had limited influence on nutritional knowledge, behaviour or outcomes for adolescents or their children. There was a statistically significant increase in adolescent knowledge of causes of anaemia (P < 0·05), but no other significant changes in knowledge were observed. The nutritional curriculum did not influence dietary diversity, the types of food eaten, anthropometric indicators or whether the adolescent or the child was identified as having moderate or severe anaemia. Further, the results of the treatment on the treated estimate indicate that the impacts were no different for girls who had greater exposure to the nutritional curriculum, that is, attending at least two-thirds of the sessions.
The impacts of the intervention on children’s outcomes were similar. There were no significant changes in the dietary intake of the children, either through increased breast-feeding for children under 2 years or through increases in intake of iron-rich foods for children older than 2 years. The intervention also did not improve a range of child nutritional status indicators, such as low birth weight, stunting, being underweight, wasting or anaemia.
Impact result moderation by socio-demographic characteristics
To determine whether the impacts of the nutritional curriculum were larger for some adolescent girls than others, as well as to potentially explain the consistently null effects of the intervention for the sample overall, interaction terms for sub-groups of interest were added to the ITT estimations, see Table 6. Two variables that were hypothesised by the study team to have the highest possibility of moderating the impact of the intervention were included, specifically highest grade of schooling completed and socio-economic status of the household. It was hypothesised that girls with higher grades of schooling and socio-economic status would have greater ability to absorb the material in the nutritional sessions and to translate the lessons into practice behaviour change.
Table 6 Summary of intent-to-treat interaction effects on nutritional outcomes of adolescents and their children

AGEP, Adolescent Girls Empowerment Program.
All adolescent models control for time since baseline and include the following covariates measured at baseline: programme site, age, school attendance, grade attainment, literate, numeracy score, cognitive score, mother alive/coresident, father alive/coresident and wealth quintiles. Models for child outcomes only include programme site, child’s age and child’s sex as covariates.
* Interaction coefficients were estimated from linear regressions clustered by AGEP group.
† Difference-in-difference interaction coefficients were estimated using generalised least squares regressions with girl-level random effects and robust se clustered by AGEP group.
The estimation results including these interaction terms do not provide consistent evidence that the intervention impacts were moderated by baseline characteristics of the girls or their households. Neither the adolescents’ education nor the wealth of their households was found to predict adolescent knowledge, dietary practices or nutrition-related outcomes. The findings, however, for educational attainment suggest some limited, but conflicting associations. The nutritional curriculum had greater positive impacts for those with higher baseline schooling attainment on currently breast-feeding children under 2 years of age, meaning girls with higher education were statistically significantly more likely to breastfeed their children. However, those with higher baseline schooling also were more likely to have stunted children under the age of 5 years. Overall, the sub-group results do not present any clear or consistent explanation of null findings of impact for the nutrition-sensitive intervention among adolescents or their children.
Discussion
While basic nutritional knowledge among adolescents was quite limited in this setting, nutritional status, as measured by thinness/underweight and overweight/obesity, indicates a favourable situation for most adolescents at the time of interview. The considerable prevalence of stunting found among adolescents and children is a concern. Similar levels of stunting can be found in the Zambia Demographic and Health Surveys(4). Stunting in this setting may be related to the reoccurring of food insecurity in months of November to February, prior to the harvest, and poor complementary feeding practices of children under 2 years of age(4). Also observed was high levels of anaemia among both adolescents and their children. Given that iron-deficient anaemia in adolescence is associated with lower physical endurance, decreased immune function and neurological impairment and that anaemia in children is associated with adverse impacts on cognitive development, school performance, and increases in morbidity, anaemia is a critical issue that needs to be addressed in this population(Reference Brabin and Brabin5,Reference Grantham-McGregor and Ani7–Reference Ekiz, Agaoglu and Karakas10,27) .
Interventions to address adolescence nutrition are critical and under-studied given the physical, cognitive, social and emotional change occurring during this period of life(Reference Blum, Astone and Decker28). It is also a period of time in which interventions that improve nutritional status might have lasting impacts as adolescents transition to adulthood, including childbearing(Reference Ruel and Alderman1). The literature on interventions that work to improve family nutrition has focused on large-scale interventions with significant investment, including improving agricultural production, school-based feeding programmes, biofortification, supplementation and expanding social safety nets, for example, cash transfers. However, the impact of such interventions for adolescents has not been consistent and compelling for improving nutritional outcomes.
One way identified to potentially improve the impact of programmes is to target women and girls at key life-stage moments to promote their nutritional health, efficacy and empowerment(Reference Ruel and Alderman1,Reference Sawyer, Azzopardi and Wickremarathne29) . The nutrition-sensitive intervention designed and embedded within the AGEP in Zambia sought to improve nutritional knowledge, enhance motivation to achieve nutritional goals and to change nutritional behaviours and improve health outcomes. The primary pathway of impact was through the conveyance of age-appropriate nutritional education during mentor-led weekly girls’ group meetings conducted over 2 years. The AGEP nutritional curriculum, repeated in both years of the programme, touched on topics of relevance to adolescent girls, including what foods were unhealthy to eat, how to prepare healthier foods, how to identify the symptoms of anaemia and how to address anaemia through their diets. For older adolescents on the threshold of starting families in this context, it presented key information on additional nutritional needs during pregnancy, proper infant-feeding practices and the basics of child development and growth monitoring(30).
The impact analysis results presented here, however, suggest that the nutritional education intervention implemented in AGEP was not sufficient to change dietary behaviour or improve nutritionally related outcomes as measured one year after the programme ended. The lack of impacts on behaviour or outcomes is likely due to the fact that it was not observed to improve adolescent nutritional knowledge. This finding was surprising, particularly as an independent mid-term evaluation of the AGEP program found that the programme had a high degree of fidelity to design and the curricula were well designed, interactive and inclusive(31).
It is possible that the educational approach did not meet the learning style of the girls, failed to achieve their buy-in to spark motivational learning or failed to convince them that this was an area in which they had efficacy and control within their household. Additionally, the adolescents in this context have limited formal educational experience and lack many of the basic literacy, numeracy and cognitive skills that are needed for comprehension of complex information.
Further, the girls in the study may not have the ability to realise change unilaterally, as they may reside in households headed by parents or spouses and have little control over resources, decision making, food availability or diet(Reference Kabeer32). Within empowerment conceptual approaches, the literature as recognised these important facilitating factors as operating within an opportunity structure across the domains of state (civic action), market (economic engagement), and society (social)(Reference Alsop and Heinsohn33) and in the context of an enabling environment using an ecological approach across the individual, relationships, community and societal levels(Reference Svanemyr, Amin and Robles34). In this context, coupling an education-based approach with a family or household-based intervention that addresses access to and control over economic and food resources may be more constructive for improving nutritional outcomes for adolescents and their children. Additionally, nutrition-related education interventions moving forward should consider more extensive formative work and human-centred design approaches for developing complementary interventions to educational approaches. Additional research is required to explore the underlying issues related to nutrition in adolescent girls’ lives in similar contexts and how nutritional information is processed at this life stage(Reference Keats, Rappaport and Jain35).
The widespread stunting and anaemia among children in the study suggest significant need for improved knowledge and feeding practices among young adolescent mothers to improve the outcomes for the youngest children in Zambia, particularly during pregnancy. Programmes with adolescent girls need to solidify knowledge of exclusive breast-feeding through 6 months and work to extend the promotion of continued breast-feeding through 2 years. The data suggest that much information about breast-feeding and child nutrition is only obtained after the birth of the child and may miss a critical period to address nutrition during pregnancy, suggesting the need for nutrition counselling during the antenatal period. Improvements in food preparation for the youngest of children as they transition to solid foods are critical for improving the energetic intake and nutrient diversity of the children.
A strength of this evaluation was the randomised design, which allowed for a rigorous assessment of the impact of the intervention addressing the nutritional needs of adolescents and their children. However, limitations included the fact that a significant percentage of girls had limited exposure to the nutritional components of the programme, with 30 % of the girls randomised to the nutritional intervention sample never attending any nutritional education sessions and only 29 % of adolescent girls attending more than two-thirds of the sessions. An additional limitation is that the nutritional component was contained within an expansive multi-component, multi-sectoral intervention touching on many areas of adolescent well-being, including reproductive health, education and economic empowerment. The broad mandate limited the ability of the programme to intervene more intensively to improve nutrition outcomes, while also constraining the amount of nutrition-specific data collected within the programme evaluation.
Conclusions
The results of this rigorous randomised evaluation indicate that the AGEP nutritional educational component with context-relevant and age-appropriate materials using participatory and interactive approaches did not improve adolescent dietary practice or nutrition-related outcomes. First and foremost, the intervention did not change adolescent nutritional knowledge as was expected. The lack of improvement in nutritional knowledge may explain why change was not observed in behaviour, but other factors affecting adolescent nutrition may have contributed. Secondary analysis to determine whether the programme effect was moderated by baseline characteristics also did not reveal important significant sub-group programme impacts. The evaluation results indicate that even high-quality nutritional educational programmes embedded within existing platforms for adolescents do not assure programme success. Further care is needed in designing programmes to tailor and motivate adolescent girls to improve their nutritional knowledge and practices, while also considering contextual constraints that limit their ability to adopt positive nutritional practices.
Acknowledgements
Acknowledgements: We would like to acknowledge PATH international for their collaboration on the nutritional curriculum; the Population Council AGEP fieldwork team, Zambia office staff and the Population Council Information Technology department; the Ministry of Health and the Ministry of Community Development and Social Welfare. Finally, we like to acknowledge the adolescent girls who shared their thoughts and experiences with us and thank them for participating in both the programme and the research. Financial support: This report/publication was produced through support provided by PATH, under a sub-grant from the UK Government’s Department for International Development (DFI.1836-668930-GRT) and work was also supported through an additional grant from the UK Government’s Department for International Development (40049678). The opinions herein are those of the author(s) and do not necessarily reflect the views of the Department for International Development. DFID had no role in the design, analysis or writing of this article. PATH international contributed to the design of the nutritional curriculum used in the evaluation, but had no role in the design, analysis or writing of the evaluation results. Conflicts of interest: The authors do not have any conflicts of interest to report. Authorship: P.C.H., E.S.H., J.B. and A.L.W. designed the nutrition evaluation. K.A. designed the Adolescent Girls Empowerment Program; P.C.H., K.A. contributed to the nutritional curriculum. P.C.H., A.L.W., E.S.H. drafted the manuscript. J.D. conducted the analysis with direction from E.S.H. and P.C.H. J.D., J.B., K.A. reviewed the draft manuscript, contributed text and provided feedback. All authors read and approved the final manuscript. Ethics of human subject participation: This study was conducted according to the guidelines laid down in the Declaration of Helsinki. All procedures involving research study participants were reviewed and approved by the Population Council Institutional Review Board (PC-IRB), the University of Zambia’s Research Ethics Committee (UNZA-REC) and the Zambian Ministry of Health, which granted authority to carry out the study. Written informed consent (adults) or parental/guardian consent and minor assent (aged < 18 years) was obtained for all aspects of study participation and data collection. Research activities were informed by Ethical Approaches to Gathering Information from Children and Adolescents in International Settings: Guidelines and Resources. The trial was retrospectively registered at ISRCTN (ISRCTN29322231).










