Adolescents in West Africa face a high risk of malnutrition during childhood and throughout their life(1,Reference Bosu2) . In this region, malnutrition can be caused by poor and unsanitary living conditions, lack of agricultural productivity combined with rapid population growth leading to food insecurity, as well as geopolitical conflicts and infectious diseases(1). Moreover, West African countries are at the early stages of nutrition transition with increasing incidence of diabetes and obesity(Reference Bosu2–4). While the burden of malnutrition is high, and its consequences on development are salient, the nutritional health of adolescents living in these settings is under-researched(5). Studies on adolescent health in sub-Saharan Africa have mainly focused on sexual and reproductive health(Reference Munakampe, Zulu and Michelo6) and HIV/AIDS(Reference Zgambo, Kalembo and Mbakaya7), but other topics remain neglected(Reference Kabiru, Izugbara and Beguy8). Adolescents in such societies are usually considered healthy in comparison with others in the population(9). Furthermore, adolescence is seen as a period of great change, with increasing autonomy(Reference Cissé, Fall and Jacquemin10). Taking adolescents’ perspectives into account is essential to developing interventions and global health responses that address their needs and priorities and understand the contexts in which they live. Despite growing awareness of the importance of engaging adolescents in this process(Reference Bulc, Al-Wahdani and Bustreo11), few studies have done so. To our knowledge, adolescents’ and caregivers’ perspectives on diet and physical activity remain under-documented in West Africa(Reference Glozah12,Reference Bello, Fatusi and Adepoju13) .
In low-income settings, nutritional practices are often shaped by education and a lack of resources rather than perceptions and knowledge, as has been described in a quantitative study with mothers in Senegal(Reference Oh, Kang and Cho14). We wanted to explore this potential gap between behaviours and knowledge using a qualitative approach that incorporated the voices of adolescents and their caregivers. Thus, our objective was to explore adolescents’ perceptions, knowledge and behaviours in relation to nutrition and physical activity, taking into consideration their caregivers’ perspectives and their living conditions in low-income districts of Abidjan, Côte d’Ivoire.
Methods
Setting, participants and research design
Abidjan is the economic capital of Côte d’Ivoire. It is characterised by increasing urbanisation due to a rural exodus and successive geopolitical crises in 2002 and 2011, which has led to the development of unplanned and informal settlements. The study took place in two districts of Abidjan. The first community was the settlement of Micao, an industrial zone in the municipality of Yopougon, in Northern Abidjan. Yopougon is the largest and most populated municipality with 1 million inhabitants in an area of 153 km2. The second district was the settlement of Derrière Wharf, in the municipality of Port-Bouët, in Southern Abidjan, along the coast and close to the international airport, with 420 000 inhabitants in an area of 111 km2(15). These two communities mainly comprise low-income families living in poor housing conditions (such as limited space, access to electricity and poor sanitation). Food supplies are purchased from market stalls along the main roads or close to public buildings such as schools.
Younger (aged 10–12 years) and older (aged 15–17 years) adolescents and their caregivers were recruited using a purposive sampling technique. The head teacher and head of community for each settlement acted as intermediaries passing on information about the study to schools and community-based associations. After giving their written and oral informed consent, participants filled out a preliminary quantitative survey. Then, a sub-sample of those who wanted to talk further about their health, nutrition and physical activity, and who were fluent in French, was selected to engage in focus group discussions (FGD). Four FGD were conducted with adolescents, one per age group and for each gender; two FGD were conducted among caregivers, one including a mixed group of mothers and fathers from Yopougon and one group of mothers from Port Bouet.
Data collection
FGD were conducted by two trained qualitative researchers (Editorial, this issue) (E.K., nutritionist, as facilitator; J.J., epidemiologist, as observer). Research assistants, all postgraduates with training in nutrition, sociology or anthropology, administered the preliminary quantitative questionnaire.
This quantitative questionnaire was used to describe the characteristics of the FGD participants and their peers who lived in the same neighbourhood, documenting their socio-economic level, as well as their nutritional habits, their mobile phone use and screen time. Weight and height were measured using standard methods, and malnutrition was defined following the WHO Child Growth Standards(Reference de Onis, Onyango and Borghi16). Diet quality was assessed with Dietary Diversity Questionnaires and the Minimum Dietary Diversity Score for Women(17). More information on the conduct and the results of the quantitative questionnaire in each study setting can be found in this issue (Fall et al., this issue).
The FGD guides were developed during the first Transforming Adolescent Lives Through Nutrition (TALENT) workshop (see Barker et al., this issue) and then tested during four pilot FGD with mixed groups of caregivers and adolescents in settings with similar socio-economic status (Abobo district and another settlement of Yopougon). The FGD guides were then finalised in collaboration with a local sociologist and a local nutritionist to adapt the level of language to suit the younger adolescents. Three main topics were explored as follows:
-
1. Nutrition (including definitions/understandings of healthy diets and foods, nutritional habits, perspectives on their own diet).
-
2. Health (for instance, definitions of health and what it means to be healthy).
-
3. Physical activity (e.g., views on, and definitions of, their own engagement with exercise and opportunities for/barriers to physical activity in their own environment).
The FGD were conducted in unoccupied school buildings at weekends. Participants were supplied with bread and water, and a meal was offered at the end of the study. A digital audio recorder (Olympus VN-541PC) was used to capture the discussions. At the beginning of each FGD, the discussion topics were briefly introduced, along with details about confidentiality and etiquette (e.g., mute phone, talk freely, respect others). The FGD conducted with adolescents lasted approximately 60 min and 90 min with caregivers. To build rapport, general questions were asked about their favourite classes, foods and games. To put participants at ease, some opted to sing or tell jokes or stories.
Data analysis
The FGD were carried out and transcribed verbatim in French, before being translated and analysed in English, to aid analysis across the TALENT data sets. Transcriptions, completed by one professional, were checked by both investigators. Two professionals translated the transcripts into English. The caregiver FGD were translated by a professional from France with a background in local expressions used in Côte d’Ivoire. The adolescent FGD were translated by a professional from Abidjan, who collaborated with the investigators to ensure accuracy. The illustrative examples given in the article are translations as close to the original meaning as possible. All transcripts were read repeatedly to aid familiarisation and then the English transcripts were uploaded into the qualitative data analysis software package NVivo (version 12) and coded by the FGD facilitator. Braun & Clarke’s(Reference Braun and Clarke18) step-by-step guide to thematic analysis shaped the process. Final codes were discussed and approved by the observer and qualitative researchers from TALENT. The codes were developed deductively from the FGD guide (e.g., perceptions, knowledge and behaviours on nutrition, health and physical activity) and inductively from study findings (e.g., economic difficulties, conflicts between caregivers and adolescents, environment constraints and solutions). The codes were organised into categories from which a thematic map (Fig. 1) was developed to describe relationships between the themes. Two workshops with the entire TALENT group helped with the development of the coding frame and identification of the main themes (Barker et al., this issue). Relevant direct quotes from the transcripts are shown in English for each topic, indicating from which FGD they originate. We adhered to the Consolidated Criteria for Reporting Qualitative Research guidelines(Reference Tong, Sainsbury and Craig19).

Fig. 1 Thematic map of the focus group discussions conducted on nutrition and physical activity perceptions, knowledge and practices of adolescents and their caregivers in Abidjan, 2018. A Transforming Adolescent Lives Through Nutrition (TALENT) study
Results
Overall, six FGD were conducted with seventy-two participants (forty-six adolescents and twenty-six caregivers). The sample reflected the diversity of those who responded to the preliminary quantitative survey, which included 109 adolescents. The main results of this survey are summarised in Table 1. Respectively, 8, 10 and 17 % were stunted, wasted or overweight/obese, with differences by age (older adolescents being more often stunted) and by gender (girls being more often overweight). Overall, 76 % scored 5 out of 10 or more on the dietary diversity score. The main sources of drinking water were ‘public tap’ and ‘piped to house’, and 81 % had their own toilet (pit or flush). More than 90 % had access to electricity, 10 % had internet access, 50 % owned a fridge, 89 % had a TV, 28 % had a computer, 22 % had a car and 50 % reported to have a table. Also, respectively, 34 and 67 % of 10- to 12-year-old and 15- to 17-year-old adolescents had their own phone, which was a smartphone in 70 % of cases. They reported spending on average 3 h/d watching entertainment programmes and 2 h/d playing on a computer.
Table 1 Descriptive characteristics of participants from the quantitative survey, living in low-income settings of Abidjan, Côte d’Ivoire, June 2018, Transforming Adolescent Lives Through Nutrition (TALENT) study
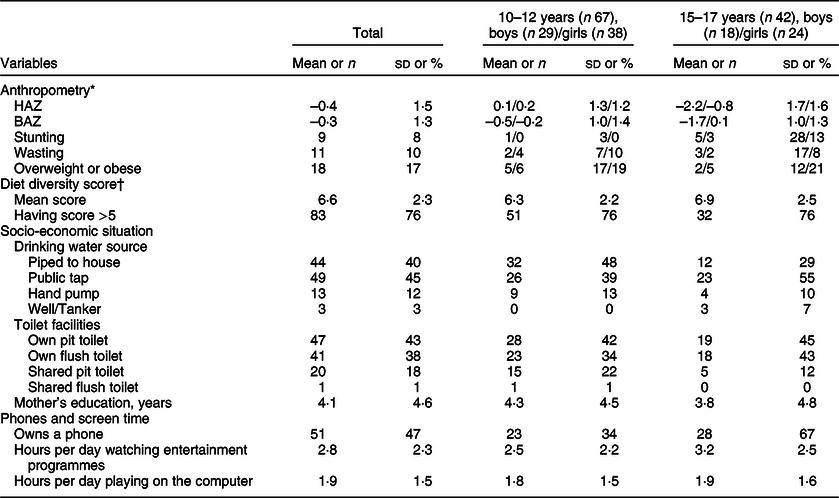
HAZ, height-for-age z-score; BAZ, BMI-for-age z-score.
* WHO 2007 Growth Standards. Stunting = HAZ < −2 sd, wasting = BAZ < −2 sd, overweight or obese = BAZ > +2 sd).
† Minimum dietary diversity score for women, from 0 to 10, FAO 2016.
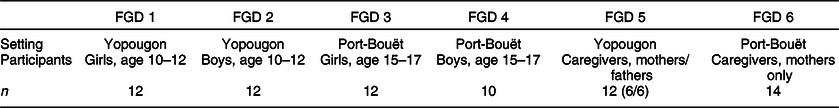
Table 2 describes the composition of each FGD.
Table 2 Composition of each focus group discussion (FGD) group, Transforming Adolescent Lives Through Nutrition collaboration, June 2018, Abidjan, Côte d’Ivoire
Across the data set, two main themes were identified. The first one concerned the perceptions and knowledge of adolescents and their caregivers about health, nutrition and physical activity. The second one was related to economic difficulties and environmental barriers to achieving good nutritional habits and physical activity practices, with differences between caregivers’ and adolescents’ feelings regarding their socio-economic situation and possible solutions.
Theme 1: Perceptions and knowledge about adolescent health, nutrition and physical activity
Perceptions of health
For both adolescents and their caregivers, health was related to their lifestyle habits. They perceived that someone healthy ate well, had a good appetite and exercised regularly, while someone who had an undiversified diet, ate too much or was inactive was unhealthy. Health was also reported to be linked to their environment, which must be clean and safe to be healthy, while a dirty, polluted environment (litter and air pollution) where there is violence was seen as unhealthy. Also, some participants mentioned mental health as salient, stating that a healthy person was someone who felt comfortable and happy. Health was also related to physical condition. Someone viewed as healthy was described as being in good shape, fit, having a powerful body and/or gaining weight (i.e., recovering from malnutrition without becoming overweight). Finally, one caregiver reported that being healthy meant having financial resources:
They (caregivers) say our health is not good because all of the foods we eat, it just makes our body unhealthy because it’s filled with garbage, it’s filled with sugar because we eat a lot of chocolate, and candy. (FGD 1, younger girls, Yopougon).
Many older adolescents felt that their caregivers considered them to be very healthy, and except for routine consultations for deworming, for example, would not take them to the hospital:
Sometimes when we say that we are sick and we have a headache, they don’t take it seriously. As long as we are not bed bound, they will not take us to the hospital. (FGD 3, older girls, Port-Bouët)
They don’t worry about anything because when they see us grow up, they think everything is fine. They don’t actually know what is going on in our bodies. All parents don’t take their children to the hospital for consultation or medical check-up. (FGD 4, older boys, Port-Bouët)
Overall, adolescents and their caregivers had similar understandings of what it meant to be healthy/unhealthy, which were systematically related to nutrition and physical activity, the two other main themes of our discussions. In the following sections, we will highlight specifically their perceptions and knowledge about nutrition and physical activity.
Perceptions and knowledge about nutrition
For both caregivers and adolescents, a healthy diet had to be diverse, balanced and rich in fruits and vegetables. Nutrients, vitamins and proteins were also mentioned:
Good food is a food which brings us vitamins and which helps us to grow well […] is when there is no sugar in it or salt, when it is not too salty or too sweet. (FGD 1, younger girls, Yopougon).
Most of the adolescents reported consuming sweets and sweet fizzy drinks, popular because of their taste. Some suggested that soda helped with digestion. Also, many participants, both adolescents and caregivers, linked excessive sweet consumption to diseases such as diabetes:
Sugar is not good because it gives diabetes. And it is a dangerous disease that leads to death. (FGD 3, older girls, Port-Bouët)
He (his child) must reduce the quantities of sugar, because with too much sugar, he is at risk of having diabetes. (FGD 5, father, Yopougon)
Caregivers were particularly concerned about sugar consumption and their adolescent’s health and felt either responsible or powerless to deal with the problem:
As a matter of fact, there is no way to control this. Outside of the house, people buy them sweets. (FGD 6, mother, Port-Bouët)
The sweet consumption of my teenager is too much! Because I am addicted myself. I like anything sweet. […] So, my daughter has inherited this from me (FGD 5, mother, Yopougon)
Besides food consumption, healthy nutritional practices were also related to hygiene. As most purchased their supplies from street markets, they were concerned about cleanliness and adequate food storage:
It’s bad food because it is sold near gutters or near dirty water that makes the food rotten, that makes the food smell bad (FGD 1, younger girls, Yopougon)
For both adolescents and caregivers, nutritional knowledge seemed to be enhanced in school where they participated in classes on the topic. TV advertisements and their local doctor were also influential:
I impose eating habits, including to myself. After all, we went to school up to secondary school, so, we learnt how to diversify our food, in particular for children under 10 or 15. (FGD 5, father, Yopougon).
Since we watch TV shows and documentaries a lot, we were recommended to avoid eating foods that are too salty, sweet or fatty. (FGD 4, older boys, Port-Bouët).
My mum teaches me how to eat well, because sometimes when I choose a food, she tells me not to eat it because it contains too many things that are not good. (FGD 3, older girls, Port-Bouët).
Perceptions and knowledge about physical activity
Most participants defined themselves as physically active. Some caregivers stated that being physically active formed part of their everyday lives, with many undertaking manual labour and/or relying on walking as their only means of transport:
We, who live in the lower neighborhood, do not necessarily need to “play” sports. Because we practice exercise every day. We do. We are running here and there all the time (FGD 5, mother, Yopougon).
We struggle a lot every day and waste much energy. That is why we eat heavy stuff each day. (FGD 5, mother, Yopougon).
Adolescents, both the oldest and the youngest, talked about the benefits of physical activity and sport on their physical development. They felt that it helped them to be fit and in good shape, gave them strength and reduced fatigue. Some of them, especially the youngest, saw sport as a means of relaxation, making them feel happy and providing them with an opportunity to play with their friends.
Although the FGD with adolescents and caregivers suggested that many had adequate knowledge about nutritional requirements and that they were keen to participate in/encourage participation in sport, there was a gap between what they would like to achieve in terms of nutritional habits and physical activity and what their socio-economic conditions would allow.
Theme 2: Socio-economic constraints on nutritional choices and physical activity practices for adolescents
Economic difficulties
Participants, mostly caregivers, were concerned about their lack of resources to afford their children the balanced, diverse diet they needed to grow and thrive. They were keen to send their adolescents to private sports clubs but lacked the resources to do so. Many struggled to buy good quality food in their neighbourhood. This lack of food choices was reported by most participants who complained about their monotonous diet and eating rice every day:
The truth is that it is a matter of resources that we don’t have. Because times are hard here, and what we earn is not enough to feed the children properly. […] Today, when we cook the same thing twice, the kids get upset, they refuse to eat and things become difficult at home. So, I really think that it is because we lack resources that we often eat the same dishes, and not because we like this. (FGD 5, mother, Yopougon)
Adolescents were asked what, if given more resources, they would eat. Some replied that they would like to eat more fruits and vegetables, varieties that were not available or unaffordable. Some wished to go to restaurants, but these were either too expensive or just absent from their suburb.
Food choices and resource limitations were seen by caregivers as a source of conflict with their adolescents whom they felt were bored of their diet and sometimes reluctant to eat at home. Two different attitudes were reported. On one hand, caregivers were simply not in a position to offer adolescents a choice because the family lacked resources to offer a range of foods. On the other hand, some caregivers felt responsible for providing their children with a sustainable, good quality diet.
I would like to state that, currently, where we are, the child does not have any choice to make. (FGD 5, mother, Yopougon).
To properly feed children, you need foods of strength, of growth, of protection. This is not the case with us. With poverty and what we earn, it is what we cook in the pot that the child has to eat. (FGD 6, mother, Port-Bouët).
Give food to the child, rather than letting him go and buy it on his own.[…] I have to impose my choice because I care for his health, because these habits bring diseases, and when these come, we parents, have to spend money to treat them. (FGD 5, father, Yopougon).
This group reported disagreements between themselves and their children who sometimes preferred to avoid eating altogether. At times, caregivers felt powerless, unable to convince them otherwise:
I would like to know what to do with the children’s behavior, I mean, they often confront parents who don’t have resources, and they behave in such a way, we should find a way to make them reasonable. What can we do to convince the kids that they should eat? (FGD 5, mother, Yopougon).
To avoid conflict, some caregivers provided their children with money to buy their own food, for example, at street markets:
We complain, but she does not eat. Now, when we realize that she does not eat, we give her the money and she goes out to buy something else. (FGD 5, mother, Yopougon)
Caregivers also saw it as a way of affording their children freedom and independence, to teach them how to make their own choices while they were growing up:
I also think that the child should exercise his choice. That’s the way things are: we, grown-ups, have choices, so children have their choices too. (FGD 5, mother, Yopougon)
The adolescents did not report any conflicts with their caregivers. Some of them mentioned that they could buy food with their own money, mostly the oldest group, while the others, mostly the younger participants, stated that their parents were in charge of their diet.
Barriers due to the environment
Caregivers and adolescents both discussed environmental barriers to accessing safe, good quality food and clean, safe places to engage in physical activity. Most schools in these suburbs did not provide food, requiring adolescents either to buy food outside from sellers located near the school entrance, or to go home, where most would eat an undiversified diet. All the adolescents described the local environment as dirty, polluted and potentially disease ridden. Street markets sometimes provided unsecured, poorly stored food, with health risks of which participants were aware:
To be healthy in our suburb, you have to avoid buying too much food on the street, food that is not clean, you have to control what you buy. […] and avoid paying for food that is not secured. (FGD 2, younger girls, Port-Bouët)
When people drink the water in the plastic bags, they throw it everywhere, that’s what makes our environment dirty, because all sanitary towels are thrown everywhere. (FGD 1, younger girls, Yopougon)
Finally, perceptions of risk/safety in these suburbs were also regarded as having an impact on their health, especially on opportunities to engage in physical activity. Indeed, both of these low-income suburbs were facing multiple problems, including violence and the presence of gangs of youths – known as ‘Microbes’ – renowned for their criminal activity. These gangs appeared after the political-military crisis in the early 2000s:
The neighborhood is full of “microbes” – Facilitator: “Microbes are young people who have knives, who drink? Children in conflict with the law?” – “yes” (FGD 1, younger girls, Yopougon).
There are many drug addicts everywhere who attack people – That is why we cannot go for a stroll along the beach. When strolling, they attack and rape some girls. (FGD 3, older girls, Port-Bouët).
Every time we play, there are people who come and smoke around. (FGD 4, older boys, Port-Bouët).
Opportunities for physical activity were also hindered by a lack of space dedicated to exercise. This was reported by every group:
I like exercising but I don’t do it at home because our house is not big enough. There is no place where I can go and workout; there is no center around here. (FGD 3, older girls, Port-Bouët).
What makes it difficult is the fact that there is no infrastructure to facilitate the games and no equipment required to play. There are people who are available and good at playing but we can’t play for lack of equipment. (FGD 4, older boys, Port-Bouët).
Most of the time, there is lack of fields. For instance, people have destroyed the former field where we use to play football in order to build companies and warehouses. (FGD 4, older boys, Port-Bouët).
Different responses from caregivers and adolescents on how to cope with these challenges
At the end of each FGD, participants were asked how these challenges could be resolved. Adolescents and caregivers gave different responses. Most caregivers felt either powerless or accepting their fate:
They (the tenants) consider that, because we live in these lower neighborhoods, we are not aware of our rights. […] What can we do? Nothing! So, we sit down, we watch them, and we live in the mess. (FGD 5, mother, Yopougon)
It is thanks to God that we are kept alive in this neighborhood. (FGD 5, mother, Yopougon)
Humans do not ask God to let them live in poverty, but if you don’t have the resources, you must accept your fate. (FGD 6, mother, Port-Bouët)
All reported that these FGD were the first time anyone had shown any interest in their situation. A political response to solve their socio-economic difficulties was mentioned, as well as NGO and development aid programmes. Also, specific TV programmes and training sessions on how to negotiate with their adolescent children were requested.
Most adolescents did not talk about the lack of resources available to them, nor did they discuss parent–child conflict. Like their caregivers, some did ask for an external response, while others suggested initiatives such as the development of canteens:
If they run an advertisement on TV to show how to eat, to adapt to one’s living environment, and to be healthy, it will be fine. (FGD 4, older boys, Port-Bouët))
You should normally build a canteen to encourage us to eat fruits and a few desserts, and also centers where we can study. (FGD 3, older girls, Port-Bouët)
The oldest adolescents requested a youth-friendly place, such as a multi-activities centre, where they could practice sport in a safe environment, and chat with other adolescents. This idea was also suggested by some mothers.
Creating parks for chatting, because when some people want to chat, they are forced to go in narrow streets and corners and it is not safe. (FGD 3, older girls, Port-Bouët)
They could create a center. A center not only dedicated to football, as there are many other sports that kids can enjoy when they do not have to be at school. Also, during the holidays, when the kids are here, wandering in the neighborhood. If there is a center, at least they could practice activities, even competitions maybe, or organize committees. (FGD 6, mother, Port-Bouët)
Thus, a gap was identified between the two main themes developed in these FGD. The main results of each theme and how to fill the gap between them are summarised in Fig. 1.
Discussion
The current study highlighted adolescents’ and caregivers’ awareness of the importance of a healthy diet and the benefits of regular physical activity. They were also conscious that their socio-economic status and the environment in which they lived strongly hindered adolescents’ capacity to adopt good nutritional habits and practice sport/exercise. The quantitative survey showed that these adolescents were living in an environment where the nutrition transition is ongoing, with both undernutrition and overweight prevalence over 10 %. Their socio-economic living conditions were similar across neighbourhoods, with poverty issues and a lack of some material possessions (half of them reported having a fridge at home) that could be related to their difficulties to adopt healthy food choices. To our knowledge, the current study is the first to explore adolescent health, focusing on diet and physical activity, in Côte d’Ivoire, especially in a low-income district of Abidjan. A qualitative study on adolescents living in poor urban settlements in West Africa is innovative and therefore difficult to compare with previous work.
Despite having good knowledge of nutrition and health, participants reported some unhealthy behaviours, such as sweet consumption. Indeed, sweet consumption is rapidly increasing in sub-Saharan Africa, with currently not enough public health efforts to address this issue and its consequences on non-communicable disease development(Reference Audain, Levy and Ellahi20). A study conducted in 2016 in Abidjan found a prevalence of 17·2 % of impaired fasting glycaemia and 0·4 % of diabetes among adolescents; this rate is expected to increase if public policies are not implemented to reduce sweet consumption in these settings(Reference Agbre-Yace, Oyenusi and Oduwole21). In the current study, caregivers were particularly concerned about adolescents becoming accustomed to regularly consuming sugary foods/beverages. This trend is supported by a recent multiregional cross-sectional survey highlighting high levels of soft drink consumption in adolescents living in sub-Saharan Africa, in addition to inadequate fruit and vegetable intake(Reference Berhane, Canavan and Darling22). Environmental hygiene and safety were also pressing issues regarding adolescent health, which have been described in other low-income settings worldwide(Reference Mmari, Lantos and Brahmbhatt23).
Overall, socio-economic constraints played a major role in shaping nutritional and physical activity habits. Poverty and a lack of resources, also described in different settings in sub-Saharan Africa(Reference Mmari, Lantos and Brahmbhatt23–Reference Ozodiegwu, Littleton and Nwabueze27), were barriers to comply with healthy eating habits. The high cost of healthy foods, alongside an unhealthy food environment, is not only associated with undernutrition risk but also with contextual factors influencing overweight and obesity risk, as seen in a qualitative synthesis among women living in sub-Saharan Africa(Reference Ozodiegwu, Littleton and Nwabueze27). The lack of safe neighbourhood spaces was a barrier to physical activity practices, which were previously found in sub-Saharan Africa(Reference Mmari, Lantos and Brahmbhatt23,Reference Ozodiegwu, Littleton and Nwabueze27,Reference Kiawi, Edwards and Shu28) and also in developed countries among poor communities(Reference Findholt, Michael and Jerofke29–Reference Sawyer, Ucci and Jones31). Despite good knowledge and perceptions on health, nutrition and physical activity, these socio-economic and environmental constraints led to a gap between perceptions and behaviours(Reference Oh, Kang and Cho14).
Conflicting relationships between caregivers and their adolescents were also frequently mentioned by caregivers. Adolescents did not report these conflicts; they may not perceive these situations as conflicting or did not discuss it out of fear or respect for their parents. Documenting further conflictual relationships between adolescents and their parents regarding nutritional habits and physical activity could allow better understanding nutritional behaviour changes. These intergenerational relationships have been explored in South Africa among daughters and mothers regarding diet and obesity risk, which could help to design appropriate public health response to improve nutrition and physical activity for this population(Reference Phillips, Comeau and Pisa32).This also highlights the importance of taking relational approach to understanding diet and physical activity in families.
Caregivers seemed to be more affected by their living conditions than adolescents. Indeed, caregivers could have lived in another environment prior to residing in the capital, such as a rural region with potentially better access to a more healthy, diversified diet(Reference Hauta-Alus, Korkalo and Freese33), and a larger house with more outside space. The adolescents, however, were more likely to be born and raised in Abidjan and were, perhaps, more accepting of their living conditions. This situation may be very common among families in Abidjan due to the rural exodus occurring in Côte d’Ivoire over the past two decades.
Our findings are in line with the conceptual map developed by Barker et al. (ref. introductory paper, this issue) about the dynamic relations between national, cultural, familial and individual-level factors and adolescent nutritional status. Participants in Côte d’Ivoire emphasised the difficulties of adopting healthy food choices, especially due to poor food availability and affordability. Settings where they live, low-income suburbs in a growing urban city, do not provide them with healthy food choices or the opportunity to engage in physical activity as they would like. Their personal choices in terms of nutritional habits are thus highly impacted by their environment. The national response to address adolescent nutrition challenges currently remains limited in Côte d’Ivoire. There is a growing risk that adolescents are becoming new target customers for food industries that promote junk food, sweetened beverages and other unhealthy food products.
Implications
Participants raised significant socio-economic issues living in undeveloped settlements where they feel neglected and left behind, for which a public health response may not completely solve all their issues. During the FGD, adolescents expressed their desire and willingness to engage in community development and decision-making. The importance of youth participation in social development, as well as the role of peer-educators, has been shown in the HIV field(Reference Campbell, Gibbs and Maimane34–Reference Speizer, Tambashe and Tegang36), but their role in other public health and development sectors is still small. The need for community-based youth services has also been raised in a Kenyan study, emphasising the benefits of a safe environment in terms of physical activity practices(Reference Ssewanyana, Abubakar and van Baar37) and this was also highlighted in other contexts in sub-Saharan Africa(Reference Ozodiegwu, Littleton and Nwabueze27). Our participants requested youth-friendly centres not only to practice sport but also to socialise in a safe environment. Youth-clubs, explored in previous studies in Africa regarding sexual and reproductive health(Reference Self, Chipokosa and Misomali38,Reference Zulu, Goicolea and Kinsman39) , could help them to develop their ideas and empower them while also having broader benefits for their community(Reference Cissé, Fall and Jacquemin10,Reference Patton, Sawyer and Santelli40) . Initiatives for caregivers are also needed to increase their awareness of the importance of adolescent health and nutrition and to help them to communicate and negotiate with their adolescent children on these subjects.
For interventions to be effective in improving the diet and physical activity of adolescents living in resource-limited settings, it is important to assess the community readiness, that is, the ‘degree to which a community is prepared to take action in an issue’(Reference Plested, Edwards and Jumper-Thurman41). This has been examined, for example, in Ghana(Reference Pradeilles, Marr and Laar42) and South Africa(Reference Pradeilles, Rousham and Norris43), where a low community readiness was assessed regarding nutritional intervention to improve diet. This emphasises the need to increase awareness about unhealthy diets before to intervene and to develop initiatives that could be actively shared by the communities involved.
The results of the current study could be of interest to stakeholders and policymakers in designing and delivering interventions for adolescents living in low-income suburbs of Abidjan. Abidjan is a rapidly growing city with an emerging socio-economic middle-class, alongside widening inequalities. The marketing of junk foods, high in saturated fats, sugars or salt, is currently rising, especially in the higher income districts and is expected to spread across the entire city in the next few years, as already observed in other settings in sub-Saharan Africa(Reference Bosu2,Reference Muthuri, Francis and Wachira3) . Suitable interventions need to be developed to prevent wider impact in low-income suburbs where little public health response is currently offered. In our study population, two-third of adolescents aged 15–17 years reported to have a mobile phone, which could be used as a tool to provide messages of health prevention and nutritional advices. Mobile phone programmes for adolescents living in low- and middle-income countries are slowly developing, with promising results to achieve knowledge and behaviour change regarding sexual and reproductive health(Reference Ippoliti and L’Engle44). However, there is currently a lack of data regarding nutritional intervention using mobile technology in adolescents living in resource-limited settings. The need for a public health response by governmental organisations to provide nutritional education and awareness was also raised in other contexts(Reference Ozodiegwu, Littleton and Nwabueze27,Reference Ssewanyana, Abubakar and van Baar37) . Especially, the question of how to adopt healthy habits while living in a poor socio-economic context remains challenging to answer(Reference Phillips, Comeau and Pisa32). Although the current study was conducted before the global COVID-19 epidemic, these results could also suggest that barrier measures imposing physical distancing to prevent this epidemic may be difficult to adopt for these adolescents living in low-income settings in Abidjan, implying, as for the topic of nutrition and physical activity, innovative ways to communicate on this public health problem and to develop solutions with them.
Strengths and weaknesses
Using a qualitative approach provided novel results on this topic, emphasising the opinions of adolescents from different age groups. Including caregivers in this process gave further insights, especially on parent–child conflict around diet and physical activity. Another strength of the current study was the collaborative approach used within the international TALENT consortium. Multiple training workshops and iterative discussions with experienced qualitative researchers helped to develop the FGD guide, conduct the analysis and write the results. Working with local professionals from Côte d’Ivoire was key to building relationships with participants and developing appropriate lines of questioning. For participants, this was the first opportunity to express their views and be listened to by those from outside their community, which helped foster engagement with the project.
Further FGD in different districts of Abidjan with higher income participants, where nutritional habits differ, would also be fruitful. The inclusion of non-French-speaking participants would also help garner a broader range of views. Results related to the topic of health were closely linked to nutrition and physical activity, probably because the investigators introduced the FGD on these grounds. Other perceptions about health could have been raised with a different FGD guide structure(Reference Secor-Turner, Randall and Mudzongo24,Reference Ahanonu and Jooste45) . Information on adolescents’ food choices when they have the money to buy it by themselves would have been interesting(Reference Voorend, Norris and Griffiths46). Conducting the FGD at school may have inhibited some adolescents who could have viewed the facilitator as a teacher. Innovative ways to conduct discussions with young adolescents in those settings should be considered to better engage them in future research projects(Reference Patton, Sawyer and Santelli40,Reference Suleiman, Soleimanpour and London47) .
Conclusions
The study highlighted the gap between perceptions, knowledge and behaviour about adolescent nutrition and physical activity. Adolescents and caregivers were aware that their dietary and physical activity habits were not in line with their definition of good nutritional practices. Their capacity to adopt a healthy diet and engage in physical activity was restricted by a lack of resources and by insalubrity and unsafe in their local environment. Many were, however, willing to actively engage in the lives of their communities, and their ideas could play a key role in the development of new interventions to improve their nutrition and physical activity.
Acknowledgements
Acknowledgements: The authors would like to thank all the adolescents and caregivers who participated in the discussions, Stéphane Ezouatchi for the transcription, Alain Volny Anne and Alvine Goméné for the translations, Emelyne Grès for the quantitative analysis and finally all our partners from Abidjan who helped us to conduct the current study and the TALENT collaboration for its support. This work is dedicated to the memory of Professor Laurence Adonis-Koffy, who passed away on 23 May 2020. She was the principal investigator in Côte d’Ivoire for the TALENT collaboration, and was a pioneer in developing access to pediatric care in West-Africa, with the creation of the first pediatric dialysis center in Côte d’Ivoire in 2012. Financial support: The current study was funded by a Global Challenges Research Fund/Medical Research Council pump priming grant (grant no. MC_PC_MR/R018545/1). The funding agency was not involved in the study design, data analysis or writing of the current article. Conflict of interest: None. Authorship: J.J. wrote the manuscript which has been reviewed by all co-authors. J.J. and E.K. collected and analysed the data, with inputs on the analysis from S.W., P.L., S.K., C.F. and M.B. E.K. developed the FGD guide with inputs from P.L. and J.J. L.A., P.N. and V.L. assisted in the study design and the implementation of the study in Abidjan. C.F. was the main investigator of the project, and L.A. and V.L. were the local investigators in Côte d’Ivoire. All authors approved the final version of the manuscript. Ethics of human subject participation: The current study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving research study participants were approved by the University of Southampton Ethics Committee and the National Research Ethics Review Board of Côte d’Ivoire. Written informed consent was obtained from all subjects.






