Previous systematic reviews suggest improvements in clinical outcome with oral nutritional supplements (ONS)(Footnote 1 ), although the role of high-protein ONS has not been widely addressed. Thus, a systematic review has been undertaken to investigate the effect of high-protein ONS v. routine care on clinical outcomes. This review has already highlighted a significant reduction in complications with high-protein ONS(Footnote 2 ). However, the review also aimed to investigate the effect of high-protein ONS on healthcare use, including length of stay in acute and community settings and hospital readmissions.
A systematic review using searches of electronic databases and bibliographies (up to January 2007) identified twenty-seven randomised controlled trials (RCT; n 2730) of multi-nutrient high-protein ONS (≥20% total energy from protein(Footnote 3 )) used in addition to diet and compared with routine care. Seven RCT (n 968) reported length of stay in hospital, including acute and community-based rehabilitation hospitals but only five RCT (n 847) had full data (mean and sd) available for analysis. Only one RCT (n 445) had data on hospital readmissions. High-protein ONS (prescribed daily intake 624–4165 kJ (149–995 kcal) energy, 18–50 g protein, 28 d–6 months) were given to patients with hip fracture (four RCT) or acutely-ill elderly patients (one RCT) in hospital or in both hospital and community settings. Meta-analysis was performed on all length-of-stay data (five RCT, n 847), and separately for acute hospital stay (three RCT) and acute and community-based rehabilitation hospital stay (two RCT) using Comprehensive Meta-Analysis version 2 (Biostat Inc., Englewood, NJ, USA).
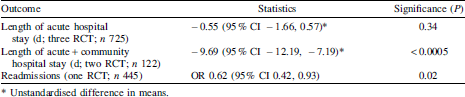
Although meta-analysis of all trials combined suggested that high-protein ONS reduced length of stay compared with routine care (−2.05 (95% CI −3.07, −1.04) d), significant heterogeneity meant a separate analysis according to setting was more appropriate (Table). The reduction in acute hospital length of stay with high-protein ONS was <1 d (7% shorter than routine-care group) but there was a much greater (20%, about 10 d) difference when community-based hospital stays were considered. The RCT that had data on hospital readmissions showed a significant reduction with high-protein ONS given in hospital and after discharge (Table).
This systematic review and meta-analysis suggests that ONS high in protein (with ≥20% total energy from protein) can significantly reduce both length of stay and hospital readmissions compared with routine care, with economic implications.


