Gastrointestinal cancer accounts for approximately 37 000 deaths in the UK per year, and overall survival remains poor. Although early EEN after major surgery is becoming more popular in the UK, the evidence required to change practice is inconclusive, and by tradition patients have been kept ‘nil by mouth’ for protracted periods.
Our aim was to determine if EEN improved clinical outcome in terms of length of hospital stay (LOHS), postoperative morbidity and mortality and health related quality of life (HRQoL).
One hundred and twenty-one patients (median age 64 years (range 35–82), eighty-three male, thirty-eight female, sixty oesophageal, thirty-three gastric, twenty-eight pancreatic cancer) were recruited across three NHS Trusts over a 3-year period. They were randomised into two groups, Group A (EEN) received early enteral nutrition via a needle catheter jejunostomy, commenced within 12 h of leaving the operating theatre. Group B (CON) received conventional management remaining ‘nil by mouth’ until deemed safe by the operating surgeon to commence oral diet and fluids. All patients in the study had a feeding jejunostomy inserted intra-operatively. Six patients were deemed palliative at the time of surgery and were therefore not eligible for randomisation.
Median LOHS for the CON group was 19.0 d (range 14–27 d); EEN group was 16 d (range 13–20.75 d), mann whitney U test (U)=1181.5, P=0.009 (Table). There were no statistically significant differences in HRQoL between the groups; however there was a trend towards improved HRQoL in the EEN group at 6, 12 weeks and 6 months post discharge. Major complications were less frequent in the EEN group.
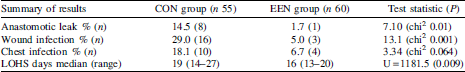
There were three post-operative deaths; two in the EEN group and one in the CON group. All deaths were unrelated to either the use of or the insertion of the jejunostomy. EEN resulted in a cost saving of £1421.17 (£926.17–£5242.18) per patient based on the difference in LOHS and the difference in the statistically significant major complications between the two groups.


