Introduction
Obesity in childhood is of national and global public health concern (World Health Organization, 2006). The Health Survey for England (HSE) 2006 reported a 17% prevalence of obesity in boys and 15% in girls (aged 2–15 years), compared with 10.9% and 12.0% in 1995 (The Information Centre, 2008a). Concern relates both to the increasing prevalence and the well-documented detrimental health consequences of childhood obesity in childhood and adulthood (Reilly et al., Reference Reilly, Methven, McDowell, Hacking, Alexander and Stewart2003).
Lord Darzi’s recent review stresses the need for the National Health Service (NHS) to realise its role in prevention, as well as management, of ill-health, highlighting obesity as a priority for the healthcare community (Darzi, Reference Darzi2008). Current recommendations of the National Institute for Health and Clinical Excellence (NICE) suggest a multi-component approach to prevention interventions aimed at reducing childhood obesity, focusing on nutrition and physical activity, as well as targeting upstream environmental factors (NICE, 2006a).
The lack of evidence regarding community interventions for prevention of childhood obesity involving health professional advice in primary care settings highlighted by NICE (2006a), is supported by the findings of the literature review carried out to inform this study. A limited evidence base suggests brief interventions for adults delivered in a primary care setting, which focus on nutrition and physical activity, can achieve behavioural change in adults and prove acceptable to health professionals. However, these studies do not report anthropometric outcomes (Booth et al., Reference Booth, Nowson, Huang, Lombard and Singleton2006; NICE, 2006b; Sacerdote et al., Reference Sacerdote, Fiorini, Rosato, Audenino, Valpreda and Vineis2006). Brief interventions in primary care for adults can be effective in encouraging smoking cessation (Lancaster and Stead, Reference Lancaster and Stead2004; Rice and Stead, Reference Rice and Stead2008) and reducing alcohol consumption in heavy drinkers (Kaner et al., Reference Kaner, Beyer, Dickinson, Pienaar, Campbell and Schlesinger2007).
Brief interventions are defined variably in the literature (NICE, 2006a). NICE propose a simple description: ‘interventions involving opportunistic advice, discussion, negotiation or encouragement……commonly used in many areas of health promotion… interventions vary from basic advice to more extended, individually focused (interventions)…’ (NICE, 2006b: 4).
The importance of primary prevention of childhood obesity in primary care is highlighted by Scott Brown (Brown, Reference Brown2006), however no UK-based studies evaluating such practices were identified in the current literature. Discussion centres mainly on management or treatment, rather than prevention.
The fundamentally social determinants of obesity have raised concerns within UK primary care about responsibility for its management (Pryke and Docherty, Reference Pryke and Docherty2008). These concerns are compounded by a lack of good quality evidence of effective primary care management interventions for both adults and children (Brown, Reference Brown2006; Jarvis, Reference Jarvis2006; Williams and De Zulueta, Reference Williams and De Zulueta2006; Pryke and Docherty, Reference Pryke and Docherty2008).
These findings emphasise the need for evaluative studies in primary care to address both the lack of exploratory evidence, providing greater understanding of the current situation within primary care, and the lack of interventional evidence.
This article outlines the exploratory evaluation of a novel brief intervention, which promotes healthy eating behaviours in young children. The intervention was delivered in primary care settings by general practitioners (GPs) and practice nurses in Worcestershire. The emphasis upon the role of GPs and practice nurses in prevention is chosen as a particular point of study interest, as the role of health visitors in primary prevention work is well defined. The evaluation focuses upon the value and acceptability of the brief intervention from health professional and parent perspectives and developing an understanding of current primary care activities in this area.
Participants and Methods
Design
A mixed-methods study design was employed, using an intervention group only, a post-intervention evaluation of parental views and a ‘before and after’ evaluation of health professional perspectives. Qualitative and quantitative data was collected by questionnaire, using a combination of guided and open response options. Telephone interviews were carried out with all health professionals and a randomly selected sample of consenting parents; the results of which are not presented here.
GPs and practice nurses from five general practices (13 health professionals in total) in Worcestershire were recruited by convenience sampling. At least one GP and one practice nurse were recruited from each practice.
The intervention involved providing the ‘Mealtime Magic’ leaflet, on a universal basis, to parents with children aged five years and younger presenting to primary care, alongside verbal reinforcement of three main messages. The intervention was delivered over a six-week period.
Formal sample size calculations were not appropriate for the purposes of this pilot study. Estimated minimum sample sizes required were chosen pragmatically based on the primary care experience of the study team.
Intervention
The Mealtime Magic leaflet was designed to convey eating behaviour messages, in order to help parents adopt recommended nutritional practices. The content of the leaflet is discussed in
Box 1. The leaflet itself can be requested from the authors.
Box 1
The leaflet was developed by a GP (RP, co-author) and a registered dietician. It was initially piloted through a health visitor and patient focus group. Messages are consistent with recommended behavioural approaches (Birch and Fisher, Reference Birch and Fisher1998; Scottish Intercollegiate Guidelines Network, 2003; James et al., Reference James, Thomas and Cavan2004; Kellogg’s, 2005; Reilly et al., Reference Reilly, Armstrong, Dorosty, Emmett, Ness and Rogers2005) and with the recently published Department of Health (DH) Change4Life material (DH, 2009). All dietary recommendations are endorsed by the Food Standards Agency and British Medical Association.
Ethical considerations
Confirmation was received from the National Research Ethics Service that ethical approval was not required for this study, considered a service evaluation. This was endorsed by the Local Research Ethics Committee and NHS Research and Development teams.
Measures
Questionnaires were designed to measure outcomes related to the specific messages in the ‘Mealtime Magic’ leaflet and aims of the study. Validated tools were screened but found to be inappropriate for this purpose. Pre-piloting of the questionnaires and subsequent development was undertaken with five parents from a nursery at the University of Warwick, recruited sequentially during a visit to the nursery, and five GP colleagues of the research team.
Health professionals: initial measures
The pre-intervention questionnaire evaluated health professional opinions, experiences and practices with regard to childhood obesity prevention. It also explored perceptions of the value of the proposed intervention in relation to current practice. Age, gender and ethnicity of health professionals were recorded.
Health professionals: post-intervention measures
The post-intervention questionnaire completed following intervention dissemination, sought health professional views about the brief intervention, including practicalities and barriers to delivery.
Parents: post-intervention measures
Consenting parents were sent a questionnaire two months post-intervention. Pre-intervention measures were not taken. For decliners, health professionals sought consent to record demographic information to be used anonymously.
Demographic characteristics
The following demographic information was collected: age, gender, ethnicity, postcode, parental self-reported height and weight, and number and age of children.
Value and acceptability of intervention
The primary parental outcome measures considered whether the leaflet was read, how easy it was to read, how helpful the leaflet was, and whether the leaflet had been shown to others. A combination of Likert scales, check boxes and free text response options were used. Questions regarding potential confounding factors were included; parental participation in other health promotion interventions or initiatives, whether messages in the leaflet were new, receipt of healthy eating advice from other sources, how healthy the family diet was perceived to be, and concerns about children’s weight.
Confidence
Parents were asked to rate personal confidence on a 3-point Likert scale (less confident, about the same, more confident) with respect to carrying out several of the leaflet’s suggestions, compared with prior to reading the leaflet. Responses were scored 1 (less confident), 2 (about the same) and 3 (more confident). Total confidence scores were calculated for each parent, to be used in analysis.
Behaviour
Parents were asked to retrospectively report how often they carried out specific healthy eating and mealtime behaviours, both before and after reading the ‘Mealtime Magic’ leaflet. Responses were indicated on a 5-point Likert scale (never, rarely, sometimes, often, always). The change in reported frequency of behaviour, comparing before and after reading ‘Mealtime Magic’, was scored (+1 or −1 corresponding to movement up or down the Likert scale by one category). Cumulative reported behaviour change scores were calculated for each behaviour by summing the individual behaviour change scores of all parent respondents.
Analysis
Health professional outcomes
Health professional outcomes are presented descriptively. Cumulative outcomes, where appropriate, were calculated by summing responses of all professionals.
Parent outcomes
Categorical parental outcomes are presented descriptively and potential relationships of interest between parental demographic characteristics and other questionnaire responses were considered. Variables were categorised where appropriate and cross-tabulated. The χ 2 (or Fisher’s exact tests) were performed.
Given the risk of false positive associations, relationships for which there are insufficient plausible explanation, variables which are not independent and/or relationships based on sub-samples of the parent sample (which may not be representative) are not presented. The remaining significant relationships, as well as the non-significant relationships useful for addressing the aims of the study, are presented. P-values are not corrected for multiple testing, as analyses are exploratory.
Relationships between demographic (parental age, index of multiple deprivation 2007 score (IMD 2007), self-reported parental body mass index (BMI)) and non-demographic numerical variables (total confidence and behaviour scores) were considered through calculation of Pearson’s correlation coefficients (continuous variables) and Spearman’s rank correlation coefficients (discrete variables). Analyses were performed using SPSS version 16.0.
IMD 2007 scores for the parent sample were obtained by matching scores with postcode data. IMD 2007 scores indicate the comparative level of deprivation within geographical and administrative areas. Lower super-output areas scores were used; these apply to geographical areas with populations of approximately 1000 people. The composite IMD 2007 scores are based on seven domain scores relating to: income, employment, health and disability, education skills and training, barriers to housing and services and crime and the living environment.
Potential confounding factors, such as IMD and reported BMI as confounders of relationships with age, and reported confidence scores as a confounder of relationships with reported behaviour, were considered through analyses of the relationships between the outcome variables and the confounding variables.
Results
Health professionals: process evaluation and demographic characteristics
Five GP practices took part: six GPs, seven practice nurses (11 females and two males). Twelve health professionals were of White British and one of White Irish ethnicity. Three practices contacted (six health professionals) declined to take part. Two practices gave time constraints as a reason; a nurse from the third practice, who may have participated, was on maternity leave.
The number of interventions delivered by each practice were: 27, 36, 50, 51 and 58, respectively. Five of 13 health professionals reported delivering the intervention to all presenting parents with children aged five years and younger. Of the remaining professionals, the most common reason given for delivery was if it was thought parents would be receptive (six of 13).
Health professionals: pre-intervention evaluation
Current views: importance of childhood obesity prevention
The majority of health professionals recognised the importance of childhood obesity in relation to other healthcare priorities; 10/13 reporting it to be ‘important/very important’, three of 13 ‘moderately important’ and one of 13 ‘of little importance’.
Current practice
Current primary care practice regarding promotion of healthy weight maintenance in children more often involved provision of dietary and exercise advice than healthy eating behaviour advice. Responding on a Likert scale (never, rarely, sometimes, often, always), when giving advice seven of 13 professionals would often/always give exercise advice, compared with four of 13 (dietary advice) and one of 13 (healthy eating behaviour advice). Advice was reportedly given most often when a child or parent is overweight, and least often as part of routine consultations. Ten of 13 health professionals stated they would often/always give advice if a child is overweight, eight of 13 if a parent is overweight and five of 13 as part of routine consultations.
Responsibilities
The main responsibility for childhood obesity prevention was attributed to parents, followed by children (over 12 years of age) or schools (for children under 12 years of age). Please see Figure 1.
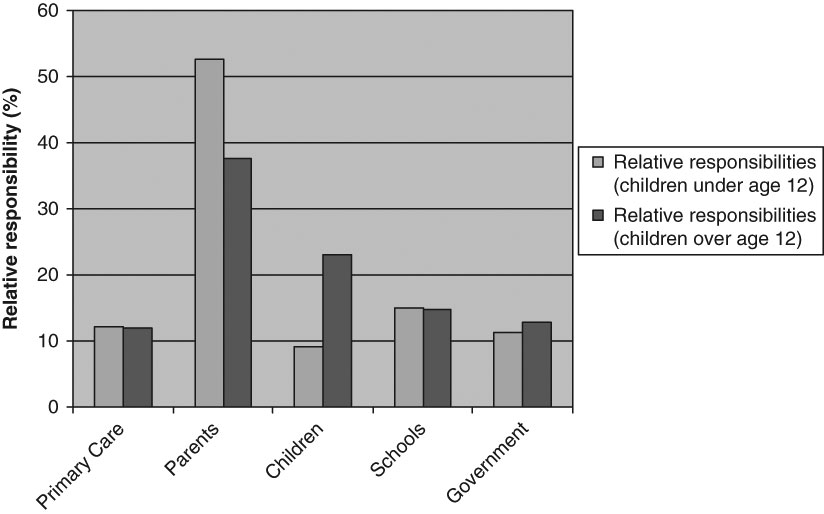
Figure 1 Childhood obesity prevention – relative responsibilities
Health professionals: post-intervention evaluation
Value and acceptability of brief intervention
All health professionals reported that most or all parental responses to the leaflet were positive. All health professionals found the brief intervention moderately to very easy to deliver and 12 of 13 professionals stated they would use the ‘Mealtime Magic’ leaflet sometimes or often in the future. Eight of 13 professionals suggested that appropriate funding would be necessary for the intervention to be taken on in general practice more widely.
Following delivery of the intervention, more health professionals thought the intervention was a practical means of opening discussions (eight of 13 compared with six of 13), with fewer stating ‘maybe’ (five of 13 compared with seven of 13).
Four health professionals reported baby clinics or immunisation clinics as the most appropriate for intervention delivery. Other settings mentioned included post-natal/six-week baby checks, child health surveillance clinics, asthma clinics and during child rather than parental appointments.
The barriers to intervention delivery described most frequently by professionals were time constraints (13/13), and inappropriateness of delivery in all consultations (13/13). Prior to delivery of the intervention, 10 health professionals cited resource constraints as a barrier to childhood obesity prevention work.
Following delivery, five health professionals described concerns regarding lack of evidence for achieving behavioural change and for effective obesity management in general. Four health professionals described parental concerns about whether they are able to change behaviour as a barrier and four described the problem of perceived parental discomfort with the subject.
Reported health professional confidence in their knowledge of evidence-based messages improved following the intervention period. One hundred percent of health professionals stated to be ‘not at all’ or ‘moderately confident’ before delivery of the intervention. Following delivery of the intervention, 31% stated being ‘confident/very confident’. Please see Figure 2.
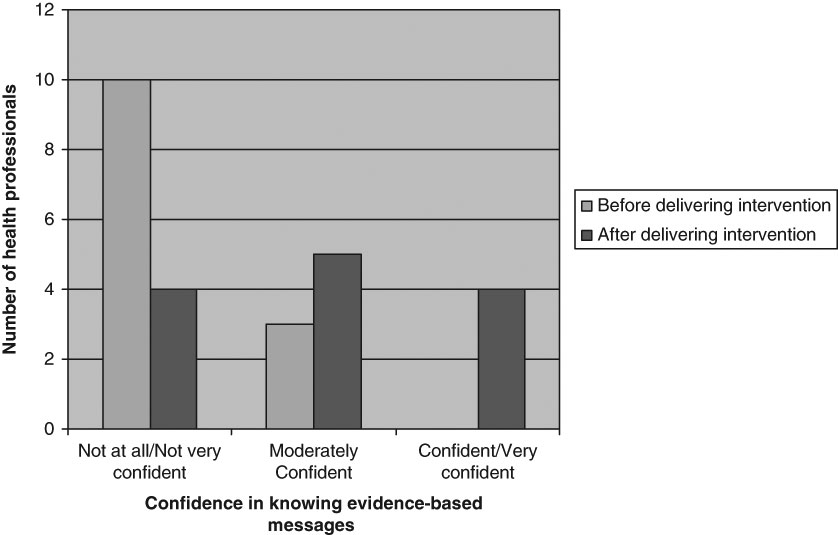
Figure 2 Confidence in knowledge regarding healthy eating behaviour messages
Parents: post-intervention evaluation
Process evaluation and demographic characteristics
Two hundred and twenty-three parents consented to participate in the study, eight declined. Only one of the declining parents consented to use of their demographic details. One hundred and thirteen parents returned the questionnaire, 110 of which were completed appropriately. Please see Table 1.
Table 1 Demographic profile of parent sample

Fifty-four of 110 parents had the intervention delivered by a practice nurse, 56 by a GP. Fifty-one of 110 parents reported receiving healthy eating advice from other sources. The most frequent sources of advice were books and other media (16 responses) and health visitors (15 responses). Information provided by nurses and doctors was least frequently noted (one response each). Nine of 110 parents stated having concerns regarding their child(ren)’s weight, six of these related to underweight and one to overweight.
Sixty of 110 parents stated that they considered their family diet was as healthy as it could be. Thirty-three of 60 of these affirmative responders reported positive changes in behaviours suggested by the leaflet. Cost, being busy (each cited by 28 parents) and children not eating healthy food (24 parents) were the most frequently stated reasons for the family diet being less healthy than it could be.
The distribution of IMD 2007 scores for parents who provided valid postcodes and that for Worcester, Bromsgrove and Redditch local authority areas are presented in Figure 3. Chi-squared tests performed to compare categorised scores did not show a statistically significant difference between the two distributions (P = 0.31). The rank of average lower super-output area scores for Worcester local authority area is 162 (English local authorities are ranked 1–354, 1 is most deprived), in Bromsgrove is 299 and in Redditch is 131. Please note that IMD 2007 ranks of lower numerical value are associated with increased deprivation, whereas IMD 2007 scores of lower numerical value are associated with decreased deprivation.
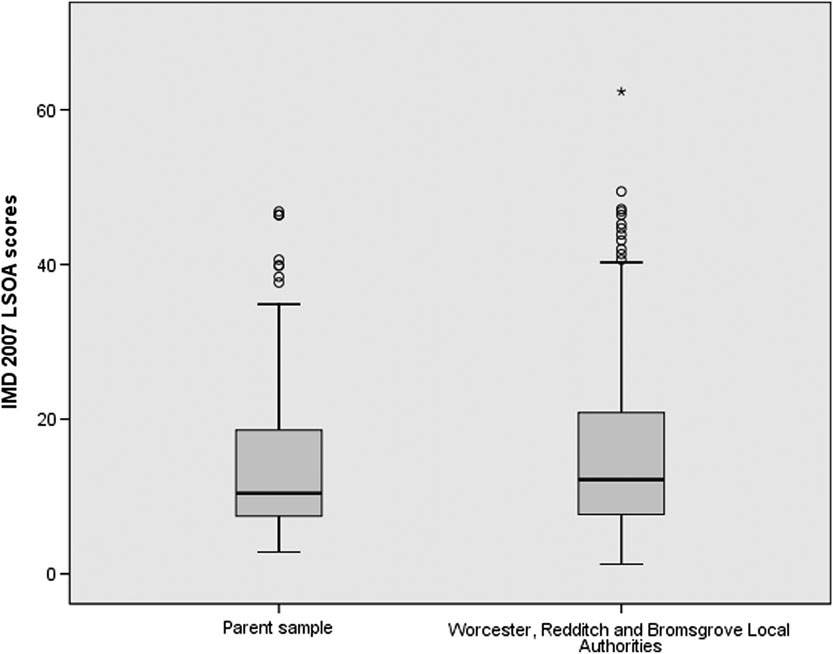
Figure 3 Distribution of index of multiple deprivation 2007 scores: parent sample compared with local area. ○, ⩾1.5* interquartile range distance from upper quartile. *, ⩾3* interquartile range distance from upper quartile value
Comparisons with HSE (2006) results for BMI of females aged 16–54 show a significantly higher proportion of parents in the study sample with a self-reported BMI < 25 (P < 0.05) (The Information Centre, 2008b). There is a significantly lower proportion of parents in the study sample with a self-reported BMI in the range 25–29.99 (P < 0.05), but no significant difference between the two groups in the 30+ ranges.
Chi-squared tests performed on HSE and parent sample data show a statistically significant relationship between increasing BMI and increasing age for the former (P < 0.001) but not for the latter. Age distribution cannot, therefore, explain the high proportion of parents in the study with a healthy range BMI.
Value and acceptability of intervention
All parents read the leaflet (110/110), the majority thought the information content was appropriate (98/108) and that it was easy to read (109/109). The majority of parents found the leaflet and advice from their GP or practice nurse helpful/very helpful (71/109 and 63/109, respectively). Qualitative open response data showed that messages relating to allowing children to stop eating when they are full and needing to offer the same foods a number of times if initially disliked were particularly helpful. For the majority, messages in the leaflet were not new (89/108). Twenty-four of 109 parents had shown or recommended the leaflet to somebody else.
Confidence
Between 30% and 52% of parents reported increased confidence in carrying out particular leaflet suggestions after reading ‘Mealtime Magic’, with the highest proportion seen in relation to ‘allowing child to stop eating when full’. Please see Figure 4.

Figure 4 Reported confidence regarding practice after reading ‘Mealtime Magic’ compared with before
Behaviour
Most positive behaviour change reported related to ‘serving new foods even if disliked at first’ and ‘asking children how much they want on their plate’. The least difference in behaviour was seen in relation to ‘not forcing children to eat disliked foods’. Please see Figure 5.
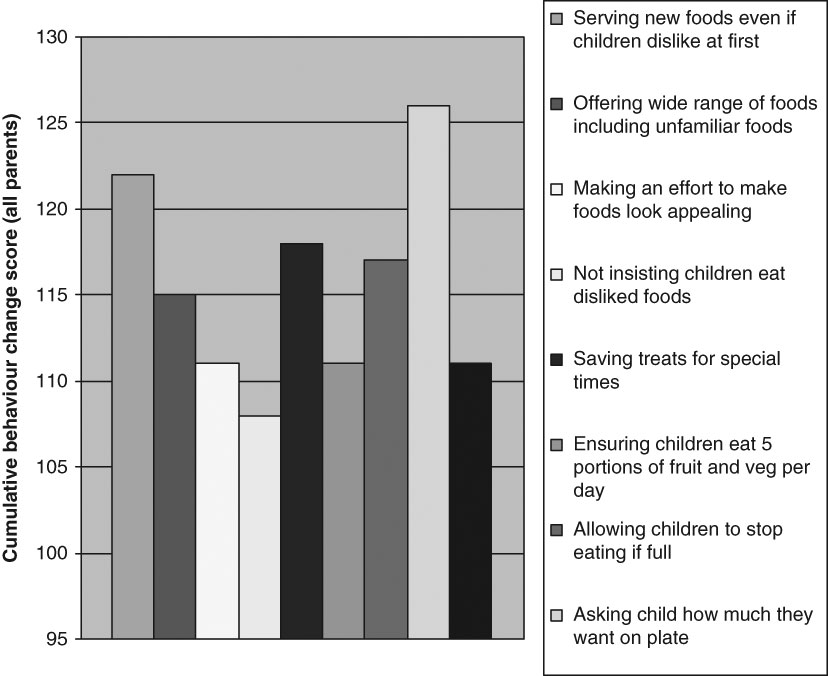
Figure 5 Cumulative reported behaviour change score (all parents)
Inferential statistics
Reported behaviour change scores were higher if messages in the leaflet were new to parents and if parents had not had healthy eating advice from other sources. The relationship between novelty of messages and individual behaviour change items was significant with regard to ‘serving food even if disliked at first’ (P = 0.003), ‘not insisting children eat food that is disliked’ (P = 0.032) and ‘allowing children to stop eating when full’ (P = 0.041), with higher reported behaviour change scores seen for parents for whom the messages in the leaflet were new. The relationship between not having had healthy eating advice from other sources and higher reported behaviour change scores was significant with regard to eating together as a family (P = 0.032) and making foods look appealing (P = 0.032).
Confounders have been considered through analyses of the relationships between the outcome variables and these confounding factors. No significant relationships were found. There are likely to be unmeasured confounding factors not accounted for.
With regard to non-significant relationships of importance, there were no significant differences in parental perceptions of helpfulness of the leaflet or reported confidence and behaviour outcomes, with respect to IMD scores.
A significant positive correlation between total reported behaviour change scores and total reported confidence scores was found, however, no other significant correlations were identified.
Discussion
This exploratory study demonstrates the acceptability, to both health professionals and parents, of a brief intervention regarding healthy eating behaviours in children delivered in a primary care setting in Worcestershire. The self-reported changes in parental confidence and behaviour require additional evaluation to assess the validity of these early findings.
Primary care professionals are well placed to play an important role in primary prevention of childhood obesity. Findings of this study, supported by a small discussion base in the literature, suggest that although the importance of the problem is recognised, primary prevention features very little in the practice of GPs and practice nurses.
Identifying means of overcoming barriers to this type of work, such as time constraints and lack of financial resource, is important, particularly if a shift from reactive to preventive practice is to take place (Brown, Reference Brown2006; Jarvis, Reference Jarvis2006; Darzi, Reference Darzi2008). Professional concern regarding the lack of evidence of effectiveness of interventions also needs addressing, however should not justify inaction.
Health professional views regarding parental responsibility for childhood obesity prevention are consistent with those described in the literature regarding primary care professional views about obesity management (Brown et al., Reference Brown, Stride, Psarou, Brewins and Thompson2007; Walker et al., Reference Walker, Strong, Atchinson, Saunders and Abbott2007). Brown and colleagues (Reference Brown, Stride, Psarou, Brewins and Thompson2007) also describe health professional perceptions of obese individuals as lacking the motivation to change.
This exposes the need for appropriate training for health professionals, and the need to challenge professional perceptions that create barriers to engagement. Although there is a spectrum of opinion regarding individual versus collective responsibilities for health, exploring this within professional training will promote understanding of the complex reasons behind individual choices (Hunter, Reference Hunter2005).
The ‘Mealtime Magic’ brief intervention was found to be acceptable to professionals, easy to deliver, and improved the confidence health professionals reported regarding their knowledge of evidence-based messages to convey regarding healthy eating behaviours. Of those participating professionals who did not deliver the intervention on a universal basis, most delivered the intervention to parents they thought would be receptive. The literature describes health professional concerns regarding the sensitive nature of the subject of weight management, as well as the opposite finding that people are often receptive to discussions of this type (NICE, 2006a; Walker et al., Reference Walker, Strong, Atchinson, Saunders and Abbott2007). The consequences of modifying professional behaviour according to perceptions of sensitivity of subject may indeed fuel inequalities in provision of appropriate healthcare.
Health education alone is insufficient to tackle childhood obesity. Traditional approaches to education need to be challenged and motivational and behavioural approaches require further development. ‘Mealtime Magic’ is a novel intervention, which focuses on the ‘how to’ as opposed to the ‘what to’. This study provides some evidence that healthy eating behaviour messages may be a useful adjunct to traditional diet and exercise advice. The high uptake of the intervention by parents (97%) and response rate to the parent questionnaire (49%) suggests that the topic is considered important.
Self-reported behaviour change and confidence improvements related to the ‘Mealtime Magic’ leaflet reported here are preliminary and should be considered in the light of the study design limitations. If the findings in this study can be validated, beneficial outcomes may be seen, particularly when impact at a population level is considered. A relationship was noted between reported confidence and behaviour measures relating to messages in the ‘Mealtime Magic’ leaflet. Confidence may be a predictor of behaviour in this case, or vice versa. Self-efficacy is proposed to be important in the process of behaviour change (National Institutes of Health, 2005).
Reported behaviour change scores were higher if messages in the leaflet were new to parents and if parents had not had healthy eating advice from other sources. This is an expected relationship and suggests the hypothesis of an effect in terms of short-term reported behaviour change, which may relate to the novelty of the messages in the leaflet. Outcomes relating to reported confidence, behaviour and how helpful parents perceived the leaflet to be did not vary according to parental deprivation, suggesting messages conveyed through the intervention were not differentially received, valued or acted upon.
The small size of this study involving five general practices in Worcestershire, means findings may not be generalisable to other settings. The convenience sampling technique used may have introduced unknown biases. The messages in the leaflet were not new to the majority of parents, likely to reflect either a well-informed population, or the influence of a response or social desirability bias. The latter may have been driven by messages sounding logical and therefore familiar, although not previously known.
A minority of parents reported having concerns regarding their children’s weight or eating habits, and most of those related to underweight. Furthermore, self-reported BMI for our parent sample was lower than expected and may highlight social desirability or responder bias.
However, the socio-economic and ethnicity profiles of parent participants were similar to the local Worcestershire population. It is estimated that 93.3% of the Worcestershire population is of White British origin (Office of National Statistics, 2009), not significantly different (at the 5% level) to the 97.3% of White British parents in our study sample.
It must be noted that IMD scores are collected at a population rather than an individual level and, therefore, our findings may be subject to ecological fallacy. Furthermore, there was no representation from Asian/Asian British or Black/Black British ethnic groups in our study sample. The majority of the health professionals involved were females and all were of Caucasian ethnic origin, again suggesting potential for bias in our results.
Non-validated self-report instruments were used for data collection, in order to answer questions specific to the brief intervention under evaluation. In particular, confidence and behaviour change measures in parents were self-reported and post-intervention, creating potential for recall and social desirability bias. Longer terms follow up would also have been desirable. However, given time and resource constraints, these study design features were considered most appropriate.
A minority of questions were removed from analysis, where responses suggested a lack of question clarity. For example, least reported behaviour change occurred with regard to ‘not insisting children eat disliked foods’, which may reflect lack of questionnaire clarity in distinguishing this discouraged practice, from ‘serving new foods children dislike at first’. Potential response biases may also have resulted from the leading nature of some questions, identified on analysis of questionnaire responses.
There is a niche for exploring brief interventions of this type, as it is unknown whether more or less intensive interventions will be most effective with regard to childhood obesity prevention (Health Technology Assessment Programme, 2006). Further research relating to this intervention could take the form of more extensive piloting or focus group work with parents in other UK settings. Analysis of telephone interview data captured as part of this study will provide further insights. Additional work with primary care professionals in different localities, with particular respect to evaluating acceptability among male professionals from a variety of ethnic groups, will also be of value.
Further evaluation should assess more formally the impact of the intervention upon longer-term behaviour change, and the practicalities of wider roll-out of this type of intervention within health promotion settings such as childhood vaccination clinics, identified by health professionals as the most appropriate setting for delivery.
This study demonstrates the acceptability of this low-cost intervention and highlights the potential value of using a brief childhood obesity prevention intervention, particularly at a time of scarce resource options. The intervention has not been designed as a ‘stand-alone’ childhood obesity prevention tool, but to be considered as one of a range of resources to tackle this problem, both in and external to the healthcare setting, at a societal and individual level. Worcestershire Primary Care Trust is now incorporating the ‘Mealtime Magic’ intervention into its list of recommended resources for use by health visitors, school nurses and primary care.
Conclusions
The current limited child obesity prevention activity in primary care does not match the stated high degree of importance that practitioners attach to it. Barriers to activity include time factors, remuneration, practical resources and perception of parental sensitivity. Addressing these barriers may reduce inequality of provision of obesity prevention healthcare.
The ‘Mealtime Magic’ brief intervention was found to be acceptable to both health professionals and parents and to improve reported health professional confidence regarding current evidence-based messages to convey regarding healthy eating behaviours in children.
Positive changes were found in self-reported parental confidence and behaviour regarding healthy family eating habits, following delivery of the ‘Mealtime Magic’ brief leaflet-based intervention: a finding that does, however, require more comprehensive evaluation in other settings.
Furthermore, the study demonstrates that development and evaluation of brief intervention approaches may be fruitful in expanding childhood obesity prevention work in primary care.
Acknowledgments
• With many thanks to the parents who took part in the project.
Other contributors
• Dr Richard Harling – Director of Public Health, Worcestershire Primary Care Trust – arrangement of study funding.
• Professor Sarah Stewart-Brown, Professor of Public Health, Director of Health Sciences Research Institute, Warwick Medical School – educational support provided.
• Dr John Powell, Senior Lecturer in Public Health, Warwick Medical School – educational support provided.
• Dr Tim Davies – Consultant in Public Health, Warwickshire Primary Care Trust – educational support provided.
Participant primary care teams (responsible for intervention delivery)
• Dr Clare Tomlinson – General Practitioner, Spring Gardens Medical Centre, Worcester.
• Yvonne Freeman – Practice Nurse, Spring Gardens Medical Centre, Worcester.
• Mike Arnold – Practice Manager, Spring Gardens Medical Centre, Worcester.
• Dr Catherine McGregor – General Practitioner, Church Hill Medical Centre, Redditch.
• Margaret Sheen – Practice Nurse, Church Hill Medical Centre, Redditch.
• Sheila Roberts – Practice Manager, Church Hill Medical Centre, Redditch.
• Dr Mike Leci – General Practitioner, Churchfield Surgery, Bromsgrove.
• Carol Pearson – Practice Nurse, Churchfield Surgery, Bromsgrove.
• Anne Banner – Practice Manager, Churchfield Surgery, Bromsgrove.
• Amanda Troth – IT/New Contract Manager, Churchfield Surgery, Bromsgrove.
• Dr Sonia Oliver – General Practitioner, Winyates Health Centre, Redditch.
• Donna Jones – Practice Nurse, Winyates Health Centre, Redditch.
• Dr Niall Doherty – General Practitioner, Winyates Health Centre, Redditch.
• Julie Ingram – Practice Manager, Winyates Health Centre, Redditch.
• Isabel Hyde – Practice Nurse Manager, New Rd Surgery, Bromsgrove.
• Anne Roberts and Christine Cross – Practice Nurses, New Rd Surgery, Bromsgrove.
• Dr Penny Dowley – General Practitioner, New Rd Surgery, Bromsgrove.
• Karen Leech – Practice Manager, New Rd Surgery, Bromsgrove.








