Article contents
A clinical review of human disease due to Paragonimus kellicotti in North America
Published online by Cambridge University Press: 27 July 2021
Abstract
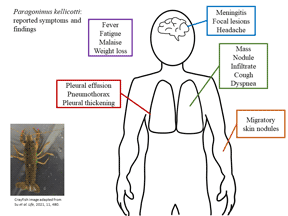
Human autochthonous infections with the trematode Paragonimus kellicotti are increasingly being reported in North America, but the true prevalence and geographic distribution are unknown. Ingestion of raw crayfish is reported in most human cases, typically in the context of alcohol intoxication. Risk of infection varies depending on what part of the crayfish is ingested as metacercariae of P. kellicotti (>50% mature to adults) localize to the heart and pericardium of the crayfish. Reported human cases have manifested primarily in otherwise healthy young adults presenting with severe eosinophilic pneumonia, pleuritis, systemic symptoms, dermatologic lesions and cerebral involvement. However, it is likely that many infections go unreported due to lack of awareness, mild illness or the absence of rapid commercially available diagnostic tests. Promising advances have been made related to novel diagnostic targets. Conservation of these antigen targets among at least four Paragonimus species could make these antigens viable for diagnostic testing of P. kellicotti specifically as well as other Paragonimus species, but additional studies and funding investments are required. Public and physician awareness may have improved due to targeted education campaigns, but ongoing activities to raise awareness are needed, particularly in areas where cases have not been frequently reported to date.
- Type
- Review Article
- Information
- Parasitology , Volume 149 , Special Issue 10: Foodborne Trematodes – time to rise from neglected status , September 2022 , pp. 1327 - 1333
- Copyright
- Copyright © The Author(s), 2021. Published by Cambridge University Press
References
- 5
- Cited by



