Introduction
In various fields under the label of nutrition and specifically in relation to growth, work played by the gastrointestinal (GI) tract (GIT) is the first physiological stage in animals and man and concerns the transformation of the diet into nutrients and then their absorption across the intestinal wall. All these phenomena are the consequences and/or the causes of many regulations. Most of them depend on a complex regulatory system more and more recognised as a unique system with different components including hormonal, nervous and immune (Besedovsky & Rey, Reference Besedovsky and Rey1996; Guilloteau et al. Reference Guilloteau, Biernat, Wolinski, Zabielski, Zabielski, Gregory and Westrom2002). The link in this unique system is composed of a number of substances which are supposed to translate and transduce the signals. It is frequently stated that the GIT represents ‘the largest endocrine organ in the body’ (Thompson et al. Reference Thompson, Greeley, Reyford and Townsend1987). Indeed, more than 100 regulatory substances are released from the GI mucosa under a variety of conditions and from a variety of cells. Besides histamine and serotonin (important examples of non-peptide regulators), most of the other regulatory substances (often referred to as hormones) released by the enteroendocrine cells are peptides (Guilloteau & Zabielski, Reference Guilloteau and Zabielski2005a). Among them, the gut regulatory peptides including the peptides of the cholecystokinin (CCK)–gastrin family, are considered as major substances which play a pivotal role in the digestive functions. Indeed, these gut-regulatory peptides are chemical messengers mostly implicated in the regulation of GI and pancreatic functions, including regulation of secretions, motility, absorption, digestion and cell proliferation. Moreover, peptides from this family share many of the same attributes, such as the presence of large precursor molecules, multiple active isoforms, and multiple and/or similar membrane-bound receptors.
In 1905, Edkins discovered gastrin, a substance produced by the stomach mucosa and implicated in the postprandial regulation of gastric acid secretion (Edkins, Reference Edkins1905). Gregory & Tracy (Reference Gregory and Tracy1964), 60 years later, described as gastrins the two almost identical heptadecaspeptide amides, GI and GII, they had isolated from hog antral mucosa. Following a quarter of a century after gastrin discovery, Ivy & Oldberg (Reference Ivy and Oldberg1928) isolated a hormone from the intestine that contracts the gallbladder and relaxes the sphincter of Oddi, and named it cholecystokinin. Harper & Raper (Reference Harper and Raper1943) isolated a hormone that stimulates pancreatic enzyme secretion and named it pancreozymin. Over 20 years later, Jorpes & Mutt (Reference Jorpes and Mutt1966) established that pancreozymin was the same substance as CCK. Moreover, later on it became evident that both regulatory substances did not totally fit into the classical hormonal definition as the other humoral substances act through blood circulation to induce specific biological effects in their target organs, since neurocrine, paracrine and luminocrine effects of CCK and/or gastrin have been reported (Konturek et al. Reference Konturek, Tasler, Bilski, de Jong, Jansen and Lamers1986a, Reference Konturek, Zabielski, Konturek and Czarnecki2003b; Owyang, Reference Owyang1996; Deng & Whitcomb, Reference Deng and Whitcomb1998). Therefore, it may be more proper to call gastrin and CCK gut-regulatory peptides (belonging to the CCK–gastrin family of peptides) rather than hormones.
Kopin et al. (Reference Kopin, Lee, McBride, Miller, Lu, Lin, Kolakowski and Beinborn1992) and Wank et al. (Reference Wank, Pisegna and de Weerth1992) purified and cloned the gastrin and CCK receptors and then it became evident that the two peptides act on their target cells through a common class of seven transmembrane domain motif receptors. Gastrin and CCK, therefore, exert their biological and physiological effects on cells by binding to specific G protein-coupled receptor (GPCR) subtypes. Receptors for the CCK–gastrin family peptides have been classified into two subtypes (Kopin et al. Reference Kopin, Lee, McBride, Miller, Lu, Lin, Kolakowski and Beinborn1992; Wank et al. Reference Wank, Pisegna and de Weerth1992) on the basis of their affinities for a structurally and functionally related family of peptides with identical COOH-terminal pentapeptide sequences, but with differences in sulfation at their sixth (gastrin) and seventh (CCK) tyrosyl residues, also with differences in their responses to specific antagonists (Jensen et al. Reference Jensen, Wank, Rowley, Sato and Gardner1989; Silvente-Poirot et al. Reference Silvente-Poirot, Dufresne, Vaysse and Fourmy1993). The CCK1 receptor binds to sulfated CCK at 500- to 1000-fold higher affinity than to gastrin, whereas the CCK2 receptor interacts with gastrin and CCK with almost the same affinity (Jensen et al. Reference Jensen, Wank, Rowley, Sato and Gardner1989). These two subtypes of receptors were previously called CCK-A and CCK-B (or CCK-B/gastrin), respectively, and they were renamed CCK1 and CCK2 receptors following the International Union of Pharmacology Committee on Receptor Nomenclature and Drug Classification (Vanhoutte et al. Reference Vanhoutte, Humphrey and Spedding1996; Noble et al. Reference Noble, Wank, Crawley, Bradwejn, Seroogy, Hamon and Roques1999). The main characteristics of these two major subtypes of CCK and gastrin receptors known until now have been well described along with the transduction mechanisms responsible for their message translation (Wank, Reference Wank1995; Yassin, Reference Yassin1999; Fourmy et al. Reference Fourmy, Escrieut and Archer2002; Miyasaka & Funakoshi, Reference Miyasaka and Funakoshi2003).
In the present review, we report recent knowledge on the involvement of CCK and gastrin in controlling digestive functions of the stomach, gut and pancreas, and particularly the interaction between nutrients and the two gut-regulatory peptide families. For this purpose, we have examined the release of CCK and gastrin peptides, paying special attention to paying their molecular forms and their specific receptors. Moreover, physiological and pathological effects are also described.
Release of gastrin and cholecystokinin from the gastrointestinal tract
Due to difficulties in purifying native CCK cells, little information is available on secretion of this peptide at the cellular level (Liddle, Reference Liddle1997) and the same is true for gastrin. For both peptides, the mechanisms responsible for their synthesis and their storage in their specific cells are well documented (Liddle, Reference Liddle, Walsh and Dockray1994; Walsh, Reference Walsh, Walsh and Dockray1994; Guilloteau et al. Reference Guilloteau, Biernat, Wolinski, Zabielski, Zabielski, Gregory and Westrom2002; Schneider & Sayegh, Reference Schneider and Sayegh2002; Rehfeld et al. Reference Rehfeld, Bungaard, Friis-Hansen and Goetze2003; Stepan et al. 2003; Varro & Ardill, Reference Varro and Ardill2003), along with production of active peptides with several molecular forms.
Molecular forms
The complexity and molecular heterogeneity of the CCK–gastrin family peptides have been revealed and it is now known that proCCK and progastrin, the two precursor molecules, are extensively processed into a wide variety of peptide products that are released from their cells of origin (Häkanson & Rehfeld, Reference Häkanson and Rehfeld2002).
Gastrin
Gastrin is characterised by a pair of heptadecapeptide amides (gastrin with seventeen amino acid residues or G17) differing only in the presence or absence of a sulfate ester on a tyrosine residue at position 6 from the COOH-terminus (Gregory & Tracy, Reference Gregory and Tracy1964). Later, NH2 terminally extended forms of G17, consisting of thirty-four amino acid residues (G34), were identified (Gregory & Tracy, Reference Gregory and Tracy1972). The major site of gastrin synthesis and secretion remains the gastrin-containing cell (G-cell) in the antropyloric mucosa. Other minor sites of production include the endocrine cells of the small intestine, the pancreas, the pituitaries and the extra-antral G-cells (Thomas et al. Reference Thomas, Hellmich, Townsend and Evers2003). However, there are several peptides derived from the biosynthetic precursors of G17 and G34. The major products are the COOH-terminal Gly-extended gastrins (i.e. the Gly-gastrins such as G34-Gly). Other small COOH-terminal fragments of fourteen (G14 or mini gastrin) and six residues (G6) may occur in tissues (Gregory et al. Reference Gregory, Tracy, Harris, Runswick, Moore, Kenner and Ramage1979, Reference Gregory, Dockray, Reeve, Shively and Miller1983), but are not thought to be functionally important. In man, relatively small amounts of the NH2-terminally extended form of G34 may occur which is now known to correspond to a seventy-one-residue peptide (Rehfeld & Johnsen, Reference Rehfeld and Johnsen1994). A large form of gastrin originally named ‘big big gastrin’ is now thought to be an artifact. In man, the main circulating forms of gastrin are typically G17 and G34 (Varro & Ardill, Reference Varro and Ardill2003).
Cholecystokinin
CCK was first isolated as a thirty-three-amino acid peptide (CCK33), but CCK58 is the best characterised, larger form of biologically active CCK. All the other forms are proteolytic carboxy terminal fragments of CCK58. Thus, many other molecular forms are now known, including the CCK4, 8, 22, 39, 58 and 83 (Wank et al. Reference Wank, Pisegna and de Weerth1992, Reference Wank, Pisegna and de Weerth1994; Liddle, Reference Liddle, Walsh and Dockray1994, Reference Liddle2000). In human tissues and blood, CCK33, CCK8 and perhaps an intermediate form are the predominant forms of CCK (Liddle, Reference Liddle1997; Rehfeld, Reference Rehfeld1998a,Reference Rehfeldb). However, considerable debates continue regarding the abundance of CCK58 (Liddle, Reference Liddle2000). CCK is produced and secreted by I-cells within the mucosa of the small intestine. I-cells have not been shown to contain other gut hormones. Moreover, CCK is a member of the growing family of the ‘brain–gut peptides’. Thus, CCK is one of the most abundant neuropeptides in the brain while gastrin-containing cells are very rare; CCK is also present in peripheral nerves (Liddle, Reference Liddle, Walsh and Dockray1994).
Factors affecting the production of molecular forms
The mammalian species is the first factor affecting molecular forms in blood. Thus, CCK8 and CCK22 are predominant in the pig whereas CCK33 and CCK58 are the major circulating forms in man (Liddle, Reference Liddle, Walsh and Dockray1994), dogs (Sun et al. Reference Sun, Chang, Xue, Wey, Lee and Chey1992) and probably also in young calves (P Guilloteau and JA Chayvialle, unpublished results; Fig. 1). CCK58 is also the only endocrine form of CCK in the rat (Reeve et al. Reference Reeve, Green, Chew, Eysselein and Keire2003a). The intestine is known to produce the larger molecular forms of the CCK–gastrin family peptides (which are characterised by longer half-lives than their shorter forms) than other organs, for example, the stomach, pancreas and central nervous system (CNS) (Guilloteau et al. Reference Guilloteau, Biernat, Wolinski, Zabielski, Zabielski, Gregory and Westrom2002). For example, in the CNS, CCK8 is by far the most abundant peptide with larger forms present only in trace amounts in the brain (Rehfeld et al. Reference Rehfeld, Bungaard, Friis-Hansen and Goetze2003). In the human pyloric antral mucosa, the concentration of G17 is over 20-fold higher than that of G34, while in the duodenum G17 and G34 occur in similar proportions (Walsh, Reference Walsh, Walsh and Dockray1994). The number of I-cells are concentrated in the duodenum and proximal jejunum and decrease in number distally throughout the small intestine (Polak et al. Reference Polak, Pearse, Bloom, Buchan, Rayford and Thompson1975; Buffa et al. Reference Buffa, Solcia and Go1976; Larsson & Rehfeld, Reference Larsson and Rehfeld1978). Moreover, there are differential distributions of molecular forms along the small intestine. For example, in man and pigs, there is a marked change in ratios of CCK8:CCK33/39 down the intestine from 1:0·8 in human proximal jejunum to 1:5·6 in mid-intestine and from 1:1·5 in porcine distal jejunum to 1:5·6 in mid-intestine (Maton et al. Reference Maton, Selden and Chadwick1984).

Fig. 1 Molecular forms of gastrin (A) and cholecystokinin (CCK) (B) in calves fed milk replacer, the protein of which was provided mainly by skimmed milk powder (milk) or whey powder (whey). Pooled calf plasma collected in either portal vein (PV) or sub-hepatic vein (SHV) or hepatic artery (HA) of six calves, 30 min after ingestion of milk, was analysed using gel chromatograthy on 1·5 × 100 cm superfine G50 Sephadex columns run at 4°C, 10 ml/h. Columns were calibrated with dextran blue (exclusion volume, about 40 ml), porcine CCK33, synthetic CCK8, non-sulfated human G34, non-sulfated human G17 and 22Na (total volume, about 160 ml). For gastrin, 5 ml of pooled calf plasma were supplied on the column. For CCK, 50 ml of pooled plasma were concentrated on C18 Sep Pak cartridge (Waters). The retained phase was eluted with acetonitrile, dried under N2 and reconstituted in 5 ml of elution buffer before application. NI, not identified. (P Guilloteau and JA Chayvialle, unpublished results).
The respective proportions of G17 and G34 in the blood vary in different circumstances. For example in human subjects, G34 predominates in fasting plasma (Varro & Ardill, Reference Varro and Ardill2003) and the three forms of CCK (CCK22, 33 and 58) are less abundant in the fasting state than postprandially (Rehfeld et al. Reference Rehfeld, Bungaard, Friis-Hansen and Goetze2003). In young calves fed milk replacer, the origin of dietary proteins modifies the production and profile of molecular forms in the blood. Thus, the ratios G34:G17 and CCK33:CCK22 were decreased in calves fed with non-clotting proteins in the stomach (whey powder) in comparison with those receiving clotting proteins (skimmed milk powder) since they were 2·2–8·0 v. 1·4–2·0 for immunoreactive gastrin and 1·2–2·2 v. 0·2–0·7 for immunoreactive CCK (Guilloteau et al. Reference Guilloteau, Chayvialle, Le Huërou-Luron, Mouats, Durand, Bernard, Bauchart and Toullec1994, Reference Guilloteau, Le Huërou-Luron, Chayvialle, Toullec, Zabielski and Blum1997; P Guilloteau and JA Chayvialle, unpublished results). In addition, these ratios vary in the general blood circulation (Fig. 1).
Globally, the metabolic clearance rate of the CCK–gastrin family peptides is proportional to the size of the molecule (Thompson et al. Reference Thompson, Greeley, Reyford and Townsend1987). For example, the rate of G34 is about five-fold lower than that of G17 (Walsh et al. Reference Walsh, Debas and Grossman1974). The disappearance half-time (T½) of the various molecular forms of exogenously infused gastrin has been reported in dogs: 1·8 min for minigastrin, 2·1 min for heptadecapeptide gastrin and 15 min for big gastrin (Walsh et al. Reference Walsh, Debas and Grossman1974). Moreover, the disappearance half-life of endogenous CCK has been found to be 5–7 min, but the half-time of exogenous CCK is between 2 and 3 min in both human subjects and dogs (Thompson et al. Reference Thompson, Greeley, Reyford and Townsend1987). This means that the regulatory substances produced and secreted by the small intestine could act for a longer time for less produced peptide, giving the small bowel a relatively important role in regulation.
Signalling pathways mediating the cholecystokinin–gastrin family peptide effects
The I- and G-cells belong to a morphologically distinct population of epithelial cells which constitute the diffuse endocrine system in the GIT. The apical membrane of these cells contacts the luminal contents while the basal membrane is commonly thought to be a major site of regulatory peptide release into the bloodstream. Although gastrin and CCK were initially described as solely endocrine products, subsequent studies have shown that they can act in an autocrine or paracrine fashion to affect cellular functions. CCK may also serve as a transmitting agent for nervous impulses discharged into blood vessels after nervous stimulation in a true neurocrine fashion (Thomas et al. Reference Thomas, Hellmich, Townsend and Evers2003).
Endocrine, autocrine and paracrine actions
Single or multiple forms of gastrin and CCK are produced from (pre)propeptides and secreted from peptide-producing cells into the interstitial fluid as well as in the blood (Walsh & Dockray, Reference Walsh and Dockray1994). From circulating blood, CCK and gastrin may specifically act on their target cells and/or organs to regulate the functions of the GIT, including the pancreas and gallbladder. The paracrine route for the action of these two hormones also has to be seriously considered as suggested by van der Schaar (Reference van der Schaar, Bremer, Lamers and Masclee2001) who observed in human subjects that a carbohydrate-rich meal with exogenous CCK did not induce gastric fundic relaxation, whereas a fat-rich meal without exogenous CCK did, despite similar plasma CCK levels. Moreover, they are interestingly implicated in the regulation of other physiological processes unrelated to digestive organ functions such as appetite regulation via the CNS and insulin secretion from pancreatic β-cells (Gibbs et al. Reference Gibbs, Young and Smith1973; Schonhoff et al. Reference Schonhoff, Giel-Moloney and Leiter2004).
Neurocrine actions
CCK is the most abundant neurotransmitter in the brain (Dockray, Reference Dockray1978) and coexists with dopamine in mesolimbic dopamine neurons (Crawley, Reference Crawley1991). CCK is produced by neurons of the brain as well as the peripheral nervous system of the GIT. Ultrastructural studies demonstrate that the CCK-producing cells are identical to I-cells of the human intestine. CCK neurons are found in the myenteric plexus, submucosa plexus and circular muscle layers of the distal intestine and colon. Postganglionic CCK nerve fibres are found in the pancreas surrounding the islets of Langerhans. Furthermore, although CCK has not been found in the intrinsic neurons of the stomach and duodenum, I-cells are in the celiac plexus and can be found in the vagus nerve, especially after injury (Thomas et al. Reference Thomas, Hellmich, Townsend and Evers2003). Some CCK1 and CCK2 receptors have been identified in capsaicin-sensitive vagal afferent neurons (Kurosawa et al. Reference Kurosawa, Uvnas-Moberg, Miyasaka and Lundeberg1997; Sternini et al. Reference Sternini, Wong, Pham, De Giorgio, Miller, Kuntz, Reeve, Walsh and Raybould1999). CCK1 receptors appear to mediate the transmission of sensory information from the gut to the brain. CCK is released from the intestine after a meal and then activates CCK1 receptors on the vagus nerve in order to transmit sensations of fullness to the brain which subsequently terminates feeding behaviours (Kurosawa et al. Reference Kurosawa, Uvnas-Moberg, Miyasaka and Lundeberg1997; Noble et al. Reference Noble, Wank, Crawley, Bradwejn, Seroogy, Hamon and Roques1999; Sternini et al. Reference Sternini, Wong, Pham, De Giorgio, Miller, Kuntz, Reeve, Walsh and Raybould1999) or GIT responses. Recently, the responses to intestinal lipids (chylomicron components) and proteins involving this neurohormonal pathway were documented in detail by Glatzle et al. (Reference Glatzle, Wang, Adelson, Kalogeris, Zittel, Tso, Wei and Raybould2003) and Darcel et al. (Reference Darcel, Liou, Tome and Raybould2005). In the same way, studying the stomach–brain communication in response to luminal acid backdiffusion, gastrin and gastric acid secretion, Danzer et al. (2003) have shown that, first, vagal afferents are stimulated by CCK and gastrin peptides acting on CCK1 receptors and, second, circulating gastrin can excite area postrema neurons that bear CCK2 receptors and project to the nucleus of the solitary tract, even if, to the best of our knowledge, gastrin has not been shown to be a neurotransmittor.
Luminal actions
In addition to their release into the circulation, there is growing evidence for CCK and gastrin release into the gut lumen. Indeed, gastrin was the first regulatory peptide to be detected in the lumen of the stomach in human subjects (Jordan & Yip, Reference Jordan and Yip1972). CCK-like immunoactivity was also detected in the lumen of the small intestine, both under control conditions and following stimulation by feeding, perfusion of the duodenum with nutrients and electrical stimulation of the vagal nerve (Inoue et al. Reference Inoue, Ayalon, Yazigi, Watson, Rayford and Thompson1982; Zabielski et al. Reference Zabielski, Kiela, Podgurniak, Gregory and Pierzynowski1999). Sun et al. (Reference Sun, Chang, Xue, Wey, Lee and Chey1992) showed that CCK is present in the lumen of the canine duodenum in multiple molecular forms including CCK8, CCK33, CCK39 and CCK58 as the predominant one. Interestingly, this was not negligible ‘leakage’, but quite the reverse as considerable amounts of the fully active CCK were found in the gut lumen in comparison with the amount released into the bloodstream. No studies are available on the demonstration of CCK release into the gut lumen. However, Okumiya et al. (Reference Okumiya, Matsubayashi, Maeda and Fujimiya1996) demonstrated the release of gastrin from intestinal G-cells using immunoelectron microscopy. They observed changes of sub-cellular localisation of gastrin granules (massive migration from basal to apical region) as well as gastrin release into the small-intestinal lumen in an apocrine-like manner induced by carbachol. Without carbachol stimulation, gastrin granules were localised mostly in the basal region of the cell and released through the basal cell membrane. It remains unclear, however, whether under physiological conditions, mainly following stimulation of neuronal release of acetylcholine, that it would reproduce the results obtained with carbachol, though the effect of electrical stimulation of the vagal nerve in an anaesthetised calf study would suggest so (Zabielski et al. Reference Zabielski, Kiela, Podgurniak, Gregory and Pierzynowski1999). Nevertheless, these morphological data help to understand the route by which GI regulatory peptides may appear in the intestinal lumen and the interstitial space of the gut mucosa following stimulation. Moreover, CCK1 receptors were detected by immunochemistry in the intestinal mucosa and the blockade of these receptors resulted in a decrease in the pancreatic response to intraduodenal CCK (Zabielski et al. Reference Zabielski, Leśniewska, Borlak, Gregory, Kiela, Pierzynowski and Barej1998b, Reference Zabielski, Morisset, Podgurniak, Romé, Biernat, Bernard, Chayvialle and Guilloteau2002) and it is reasonable to assume that luminal CCK acts in physiological conditions.
Intestinal absorption of the peptides
The mechanism of absorption of luminally released CCK and gastrin is far from being understood, though an enterocyte transcellular pathway seems quite probable under physiological conditions rather than a paracellular process. In newborns, the canaliculo-vesicular system present in the enterocytes could be an ideal means of a non-specific transport of all large-size molecules, in particular during the first days of life when the so-called ‘transport vacuoles’ exist (Baintner, Reference Baintner, Zabielski, Gregory and Weström2002). The contents of ‘transport vacuoles’ are not affected by the lysosomal enzymes, thereby the absorbed molecules retain their biological activity. Colostrum and milk bioactive polypeptides and proteins, including immunoglobulins, hormones, growth factors, etc, can be readily absorbed by this route. Until 3–4 weeks of life, the enterocytes of the neonate contain the ‘digestive vacuoles’ that may continue the process of macromolecule absorption, though, to our knowledge, it has not been demonstrated so far. Moreover, the vacuolated enterocytes that contain the digestive vacuoles are located in the lower two-thirds of the jejunum and in the ileum. In the young and adults, it seems probable that luminal CCK would permeate through the enterocyte lineage from the gut lumen to the interstitial fluid together with TAG, lipoproteins and other lymph constituents. Even regulatory peptides are at least in part hydrolysed by GI enzymes (Laster & Walsh, Reference Laster and Walsh1968; Bunnett et al. Reference Bunnett, Debas, Turner, Kobayashi and Walsh1988); Su et al. (Reference Su, Amidon and Lee2002) recently demonstrated that CCK8 can be absorbed through the GI membrane in the adult rat in a site-dependent manner. Moreover, the systemic availabilities of peptides given intraluminally can be significantly increased by preventing their degradation by the brush-border enzymes and their absorption is not limited by permeability. These results agree with those obtained by Glatzle et al. (Reference Glatzle, Wang, Adelson, Kalogeris, Zittel, Tso, Wei and Raybould2003) who had shown the presence of only small amount of CCK in the upper part of the rat mesenteric lymph duct (about 9 pm). Neither information on the CCK concentration in the interstitial fluid just behind the epithelial cell layer nor on the CCK hydrolysis in the mucosa and lymph is provided in their work.
Factors regulating gastrin and cholecystokinin release
In the present review, we will neither report on the aspects concerning the synthesis of the CCK–gastrin family peptides nor the transduction system when the signal is transmitted as well as on factors implicated, since recently synthesis has been well documented at the genomic, molecular and cellular levels (Liddle, Reference Liddle1997; Dockray et al. Reference Dockray, Varro, Dimaline and Wang2001; Thomas et al. Reference Thomas, Hellmich, Townsend and Evers2003; Dockray, Reference Dockray2004). The factors affecting peptide release can be linked to the animal or human subject itself or to its environment. We report here the effects measured by gastrin and CCK-specific RIA for total gastrin or CCK.
Animal species, digestive status and age
In single-stomached species, ingestion of food stimulates CCK and gastrin release; in ruminant species after the completion of weaning, no elevation of blood peptide concentrations is observed (Le Dréan et al. Reference Le Dréan, Le Huërou-Luron, Gestin, Romé, Plodari, Bernard, Chayvialle and Guilloteau1998). This phenomenon is, globally, due to the more regular stomach distension and the flow rate of digesta from the stomach to the duodenum as well as to the relative stability of pH of the duodenal content at about 2·75 during the preprandial and prandial phases. In preruminant calves, however, short-lasting variations in plasma CCK (but not in gastrin) in relation to the duodenal migrating myoelectric complexes (MMC) were observed. Feeding transiently affected the intestinal MMC and abolished CCK fluctuations. The fluctuations of plasma CCK in calves were apparently associated with the portions of coagulated milk that entered the duodenum from the abomasum, since the phenomenon was not observed in the calves fed milk formula which did not produce a clot in the abomasum (Zabielski et al. Reference Zabielski, Dardillat, Le Huerou-Luron, Bernard, Chayvialle and Guilloteau1998a). In dogs, plasma CCK and gastrin did not show fluctuations in phase with duodenal MMC during the interdigestive period (Konturek et al. Reference Konturek, Thor, Bilski, Bielański and Laskiewicz1986b), indicating that fluctuations in plasma CCK are not related to the mechanism which generates the MMC, and are the result of stimulation by the digesta that pass the duodenum during phase II of MMC. In the rat, intact dietary proteins are effective stimulants of CCK release, but in canine and human species their digestion is required (Liddle, Reference Liddle1997). In the rat, ageing impairs CCK release, resulting in tissue accumulation and a decrease in the synthesis of CCK; however, that impaired release of central and peripheral CCK associated with ageing was observed in male rats, not in female rats (Ohta et al. Reference Ohta, Tanaka, Masuda, Miyasaka and Funakoshi1995; Miyasaka et al. Reference Miyasaka, Kanai, Ohta and Funakoshi1997a). In newborn rats, serum gastrin concentration was low, then it increased gradually until it peaked at about 2–3 weeks of age at the time of weaning (Ekelund et al. Reference Ekelund, Hakanson, Hedenbro, Rehfeld and Sundler1985). But gastrin is being produced in the newborn rat at the time when enterochromaffin-like (ECL) cells are few and a role for gastrin in initiating the development of these ECL cells has been studied (Björkqvist et al. Reference Björkqvist, Dornonville de la Cour, Zhao, Gagnemo-Persson, Hakanson and Norlen2002). In calves receiving milk replacer based on skimmed milk powder, plasma concentrations of gastrin decreased from 1 to 3 weeks of age, but this is reversed for CCK (Guilloteau et al. Reference Guilloteau, Chayvialle, Toullec, Grongnet and Bernard1992a,Reference Guilloteau, Le Huërou-Luron, Chayvialle, Mouats, Bernard, Cuber, Burton, Puigserver and Toullecb, Reference Guilloteau, Le Huërou-Luron, Chayvialle, Toullec, Zabielski and Blum1997); after weaning, the basal and stimulated plasma concentrations of these two peptides increased (Toullec et al. Reference Toullec, Chayvialle, Guilloteau and Bernard1992).
Moreover, it is suggested that CCK may modulate gastric leptin expression and secretion in pre-weaning milk-fed calves (Yonekura et al. Reference Yonekura, Kitade, Furukawa, Takahashi, Katsumata, Katoh and Obara2002) as well as in rats (Brzozowski et al. Reference Brzozowski, Konturek, Konturek, Pajdo, Duda, Pierzchalski, Bielanski and Hahn1999). Inversely, duodenal leptin stimulates CCK secretion and there is evidence for a positive leptin–CCK feedback loop (Guilmeau et al. Reference Guilmeau, Buyse, Tsocas, Laigneau and Bado2003). Yonekura et al. (Reference Yonekura, Kitade, Furukawa, Takahashi, Katsumata, Katoh and Obara2002) also studied the effects of ageing and weaning on mRNA expression of the leptin and CCK receptors in the calf rumen and stomach. In the mucosa, the changes of CCK receptor mRNA expression (as well as that of leptin) coincided with ageing and changes in nutritional conditions. This is true particularly for the CCK1 receptor subtype in the rumen which is predomninant, whereas CCK2 receptor mRNA is scarcely expressed in the rumen of 3- and 13-week-old animals. By contrast, in the stomach, CCK2 receptor transcription gradually decreased between 3 weeks of age and the adult stages but CCK1 receptor mRNA was expressed at very low level.
Meal, diet composition and digestive products
The release of CCK and gastrin is stimulated by the ingestion of a meal and its chemical composition in most single-stomached species (Liddle, Reference FitzGerald, Ghatei, Mandir, Bloom, Iversen and Goodlad1997, Reference Folsch, Winckler and Wormsley2000). For example, in human subjects, the basal blood levels of CCK are approximatively 1 pm and increase to 5–10 pm after a mixed meal (Liddle et al. Reference Liddle, Goldfine, Rosen, Taplitz and Williams1985). Carbohydrates are the least potent stimuli of CCK release when compared with fat and protein (Liddle, Reference Liddle1997). Ethanol feeding in experimental animals and human subjects stimulates CCK secretion (Liddle et al. Reference Liddle, Goldfine and Williams1984). In the rat, it has been shown that it occurs by effecting on CCK-releasing factor (Saluja et al. Reference Saluja, Lu, Yamaguchi, Hofbauer, Runzi, Dawra, Bhatia and Steer1997). In most of the species with a single stomach, the most active stimulants of CCK secretion are the digestion products of fat and protein (Brodish et al. Reference Brodish, Kuvshinoff, Fink, McFadden, Turkelson and Solomon1994a,Reference Brodish, Kuvshinoff, Fink, Turkelson, McFadden and Solomonb). Hydrolysis of TAG to fatty acids with chain lengths of nine (or twelve) or more carbons results in effective CCK stimulation (Dockray et al. Reference Dockray, Varro, Dimaline and Wang2001). Among the amino acids, tryptophan and phenylalanine are the most potent stimuli in canine and human species. For gastrin, the well-recognised luminal stimuli are amino acids (particularly aromatic amino acids), dietary amines and Ca (Dockray et al. Reference Dockray, Varro, Dimaline and Wang2001). Moreover, intravenous infusion of amino acids stimulates CCK secretion (Liddle, Reference FitzGerald, Ghatei, Mandir, Bloom, Iversen and Goodlad1997, Reference Folsch, Winckler and Wormsley2000). In the rat, food restriction induces a reduction of pancreatic function (decrease of amylase secretion) by a mechanism that evidently involves a decrease of CCK release and a down regulation of the CCK receptors (reduction of CCK receptor affinity and capacity) (Chowdhury & Rayford, Reference Chowdhury and Rayford2001); these data suggest that CCK plays an important physiological role in adaptation of eating less food and thereby to a lowering of body size in rats and possibly in other mammals. In calves fed milk replacer, when dietary proteins are mainly from soya products instead of skimmed milk powder, post-feeding patterns of plasma gastrin and CCK concentrations are similar but more emphasised with highest variations (250–275 % of basal values v. about 200) (Le Dréan et al. Reference Le Dréan, Le Huërou-Luron, Chayvialle, Philouze-Romé, Gestin, Bernard, Toullec and Guilloteau1997). In these species, the modifications in the release of gastrin and CCK induced by the nature of the dietary proteins are related to the ability of these proteins to clot in the stomach and consequently to the pattern of gastric emptying (Le Huërou-Luron et al. Reference Le Huërou-Luron, Gestin, Le Dréan, Romé, Bernard, Chayvialle and Guilloteau1998). Finally, the anatomy of the G- and I-cells, with their apical surface open to the lumen of the intestine, makes it so that food, digestive products or secretions (and perhaps CCK-releasing factors such as described later – monitor peptide and luminal CCK-releasing factor; LCRF) can interact directly with the cells producing regulatory peptides (Liddle, Reference Liddle2000).
Organ and digestive secretions
According to the distribution of the I-cells in the proximal v. distal gut, nutrients experimentally introduced into the stomach or into the proximal small intestine are more effective secretagogues than when administered into the distal part. Endogenous bile (or bile acids) exerts a tonic inhibition on CCK secretion (Koide et al. Reference Koide, Okabayashi and Otsuki1993). Gastrin release is suppressed by gastric acid which probably acts by releasing the paracrine inhibitor somatostatin (Walsh, Reference Walsh, Walsh and Dockray1994).
Pancreatic and gut epithelial peptides that release cholecystokinin
Substantial evidence has indicated that at least one mechanism causing CCK release involves endogenously produced releasing factors that are secreted into the lumen of the intestine and under the proper conditions to stimulate CCK secretion (Lu et al. Reference Lu, Louie and Owyang1989; Miyasaka et al. Reference Miyasaka, Guan, Liddle and Green1989; Spannagel et al. Reference Spannagel, Green, Guan, Liddle, Faull and Reeve1996; Wang et al. Reference Wang, Prpic, Green, Reeve and Liddle2002). There is now strong evidence that a feedback mechanism exists in the chicken, pig, rat, dog and man. The existence and description of at least two types of CCK-releasing factors have been reported (Liddle, Reference FitzGerald, Ghatei, Mandir, Bloom, Iversen and Goodlad1997, Reference Folsch, Winckler and Wormsley2000). One of these, LCRF, was isolated from rat intestinal washings, while the other, diazepam-binding inhibitor, was identified in porcine intestine. These CCK-releasing factors are of intestinal origin and are present in the gut under basal conditions. By contrast, another peptide, the monitor peptide, also known as pancreatic secretory trypsin inhibitor-I or PSTI-61, is produced by pancreatic acinar cells and is secreted into pancreatic juice where, upon reaching the intestine, it stimulates CCK release (Iwai et al. Reference Iwai, Fukuoka, Fushiki, Kodaira and Ikei1986; Liddle, Reference Liddle1997). These releasing factors appear to mediate negative-feedback regulation of CCK secretion and the mechanism by which LCRF affects I-cell function in human subjects was recently studied (Wang et al. Reference Wang, Prpic, Green, Reeve and Liddle2002).
Neural factors
The regulation of CCK release by neural factors seems complicated when examined in vivo. The effect of vagal innervation on CCK release has been examined in vagotomised patients who demonstrated an exaggerated CCK response to a liquid meal (Hopman et al. Reference Hopman, Jansen and Lamers1984a,Reference Hopman, Jansen and Lamersb). However, it remains unclear whether vagal innervation directly regulates CCK secretion or it modifies release indirectly through effecting on other targets such as the pancreas or gallbladder (Hopman et al. Reference Hopman, de Jong, Rosenbusch, Jansen and Lamers1987). Bombesin (BBS), a tetradecapeptide originally isolated from the skin of the frog, is analogous to mammalian gastrin-releasing factor (GRP). BBS or GRP and cholinergic agonists increase gastrin secretion and tachykinins inhibit the secretion (Varner et al. Reference Varner, Modilin and Walsh1981; Hirschowitz & Molina, Reference Hirschowitz and Molina1983; Smith et al. Reference Smith, Stanley, Verderame and Zagon2004). GRP stimulates CCK release and I-cells possess its receptor (Kanayama & Liddle, Reference Kanayama and Liddle1991; Snow et al. Reference Snow, Prpic, Mangel, Sharara, McVey, Hurst, Vigna and Liddle1994); therefore, GRP-containing nerves in the mucosa may modulate CCK release. This substance also stimulates gastrin secretion from G-cells (Seensalu et al. Reference Seensalu, Avedian, Barbuti, Song, Slice and Walsh1997).
Other regulatory substances
In man, loparemide, a peripherally acting opiate receptor agonist, enhances postprandial CCK secretion (Thimister et al. Reference Thimister, Hopman, van Roermund, Willems, Rosenbusch, Woestenborghs and Jansen1997) but the effects of other opiates and the exact site of action for stimulating CCK secretion remain unknown. BBS has been shown to directly stimulate CCK release (Snow et al. Reference Snow, Prpic, Mangel, Sharara, McVey, Hurst, Vigna and Liddle1994). Several gastric peptides, such as apelin, proxenopsin and leptin have been shown to stimulate CCK release by classical pathways, as well as by the luminal way (Guilmeau et al. Reference Guilmeau, Buyse, Tsocas, Laigneau and Bado2003; Wang et al. Reference Wang, Anini, Wei, Qi, O'Carroll, Mochizuki, Wang, Hellmich, Englander and Greeley2004). A recent study suggests that leptin does not act directly on the rat pancreatic acinar cells but inhibits the secretion of pancreatic enzymes indirectly via a neurohormonal CCK–vagal-dependent mechanism (Matyjek et al. Reference Matyjek, Herzig, Kato and Zabielski2003). Gastrin release is stimulated by BBS, GRP and inhibited by secretin, glucagon, gastric inhibitory polypeptide (GIP) and vasoactive inhibitory polypeptide (Thompson & Marx, Reference Thompson, Marx and Ravitch1984). Moreover, somatostatin inhibits the synthesis and release of the peptides of the CCK–gastrin family. Somatostatin is considered as a hormone which terminates the prandial phase of gastric and pancreatic secretions. Finally, CCK inhibits gastrin secretion independently of paracrine somatostatin secretion (Schmidt et al. Reference Schmidt, Hansen, Hilsted and Holst2004). In patients infected with Helicobacter pylori, plasma gastrin concentrations are higher than in controls. Studies on the mechanisms implicated showed that in vivo cytokines, for example, IL-8 and inflammatory cells might mediate the effects of H. pylori infection on gastrin release (Lehmann et al. Reference Lehmann, Golodner, Wang, Chen, Avedian, Calam, Walsh, Dubinett and Soll1996; Beales et al. Reference Beales, Blaser, Srinivasan, Calam, Perez-Perez, Yamada, Scheiman, Post and Del Valle1997). Reduced acid secretion caused by H. pylori also contributes to the hypergastrinaemia (Levi et al. Reference Levi, Beardshall, Swift, Foulkes, Playford, Ghosh and Calam1989).
Physiological effects of gastrin and cholecystokinin
The cellular and molecular mechanisms by which gastrin and CCK act on the target cells are well described in original papers and reviews (Walsh & Dockray, Reference Walsh and Dockray1994; Greenly, Reference Greenly1999; Ikeda & Fukuoka, Reference Ikeda and Fukuoka2003; Miyasaka & Funakoshi, Reference Miyasaka and Funakoshi2003; Prinz et al. Reference Prinz, Zanner and Gratzl2003; Thomas et al. Reference Thomas, Hellmich, Townsend and Evers2003; Dockray, Reference Dockray2004; Dockray et al. Reference Dockray, Dimaline and Varro2005). Briefly, gastrin or CCK peptide-stimulated signal transduction occurs with the binding of peptides to their cognate cell surface receptors, the GPCR (CCK1 and CCK2). These receptors are characterised by an extracellular N-terminal segment, seven transmembrane α-helices, three extracellular loops (exoloops), three cytoplasmic loops (cytoloops) and one C-terminal segment (Ji et al. Reference Ji, Grossmann and Ji1998). It was originally thought that, for the occurance of GPCR signalling, specific interactions between the GI peptide and the receptor were necessary to produce conformational changes in the receptor and to stimulate intracellular signal transduction networks. However, recent studies suggest a more complex regulation of the GPCR through: (1) dimerisation with themselves (homodimerisation) and other receptors (heterodimerisation) (see pp. 270–271); (2) activation of differing G proteins; (3) internalisation and desensitisation; (4) ability to change their conformation and interactions with empty or inactive receptors. It is suggested that this complex mechanism of regulation allows peptides to interact with GPCR, to stimulate diverse intracellular signalling pathways, and ultimately affect multiple physiological functions depending on cell types (Thomas et al. Reference Thomas, Hellmich, Townsend and Evers2003). In this review, these mechanisms were not discussed but the receptor subtypes are taken into account to describe the effects of CCK–gastrin family peptides through CCK1 or CCK2 receptors in physiological conditions as well as in the case of diseases (Table 1). Moreover, another class of receptor subtype, discovered by Yu et al. (Reference Yu, Huang, Wank, Mantey, Gardner and Jensen1990) and more recently characterised (CCK-C receptor) (Biagini et al. Reference Biagini, Monges, Vuaroqueaux, Parriaux, Cantaloube and De Micco1997; Yassin, Reference Yassin1999) is also reported (Table 2).
Table 1 Summary of the recent knowledge on the involvement of cholecystokinin (CCK)–gastrin family peptides and their receptors in the control of digestive functions and more generally their role in the field of nutrition in mammals, in physiological conditions

ECL, enterochromafin-like; PP, pancreatic polypeptide.
Globally, control of satiety, gallbladder contraction, pancreatic exocrine secretion, gastrin, pepsinogen and leptin secretions, gastric emptying and gut motility are the best known actions of CCK which are mediated by CCK1 receptors (Silvente-Poirot et al. Reference Silvente-Poirot, Dufresne, Vaysse and Fourmy1993; Bado et al. Reference Bado, Levasseur and Attoub1998; Wank, Reference Wank1998). Action of CCK–gastrin family peptides which occur through the CCK2 receptors include modulation of anxiety and pain perception; this involves CCK2 receptors of the CNS (Crawley & Corwin, Reference Crawley and Corwin1994; Noble et al. Reference Noble, Wank, Crawley, Bradwejn, Seroogy, Hamon and Roques1999). The CCK2 receptor is also widely and abundantly expressed by cells in peripheral organs such as the stomach, the kidney and the pancreas where it mediates gastrin-stimulated gastric acid secretion, changes in renal K and Na absorption and glucagon secretion, respectively (Saillan-Barreau et al. Reference Saillan-Barreau, Dufresne and Clerc1999; Von Schrenck et al. Reference Von Schrenck, Ahrens and de Weerth2000; Dockray et al. Reference Dockray, Varro, Dimaline and Wang2001; Lindström et al. Reference Lindström, Chen, Norlen, Andersson and Hakanson2001). CCK and gastrin also play a role in the control of cell proliferation, differentiation as well as in GI protection (Thompson & Marx, Reference Thompson, Marx and Ravitch1984; Rehfeld & van Solinge, Reference Rehfeld and van Solinge1994; Dockray et al. Reference Dockray, Varro, Dimaline and Wang2001; Trulsson et al. Reference Trulsson, Svanvik, Permert and Gasslander2001; West & Mercer, Reference West and Mercer2004). The peptides of the CCK–gastrin family have also indirect actions via the secretion of other regulatory substances. As an example, it was recently suggested that gastrin is a potential candidate for the postprandial decrease of ghrelin secretion in the rat (Lippl et al. Reference Lippl, Kircher, Erdmann, Allescher and Schusdziarra2004).
Global effects of gastrin and cholecystokinin in the gut
In this first part, some aspects on the effects of CCK on the activity of vagal mucosal afferent nerves are described. Then, we report on the physiological effects of the CCK–gastrin family peptides through the CCK1 receptor pathway on the one hand and via the CCK2 receptors on the other hand.
Cholecystokinin affects the activity of vagal mucosal nerves
Low concentrations of CCK8 have been reported by Cottrell & Iggo (Reference Cottrell and Iggo1984) to excite vagal afferent receptors located in the mucosa of the proximal duodenum in sheep. Blackshaw & Grundy (Reference Blackshaw and Grundy1990) have demonstrated in ferrets that close intra-arterial injection of CCK8 increases the electric discharge in single fibres originating from the gut segment where the hormone was applied. The CCK-responsive fibres were identified as the tension receptor afferents related to contractile activity as well as the mucosal receptor afferents with a conduction velocity in the C-fibre range. The mucosal receptor afferents were localised in the stomach corpus and antrum but mostly in the duodenum, and could respond to low doses of CCK8 but not to intraduodenal glucose, tryptophan or to distension. The responses of mucosal receptor afferents were enhanced by a mucolytic agent, acetylcysteine, which shortened the latency and increased the amplitude of responses, which were not affected, however, by cholinergic blockade with atropine and hexamethonium. Blackshaw & Grundy (Reference Blackshaw and Grundy1990) concluded their study by suggesting that although activation of mucosal fibres from the gut by luminal stimuli has weak effects on vagal efferent fibre discharge, the reflexogenic potency may be enhanced if a large number of mucosal afferents would be stimulated simultaneously. Richards et al. (Reference Richards, Hillsley, Eastwood and Grundy1996) provided further evidence in anaesthetised rats by showing that mesenteric nerve bundles contained one to two afferent fibres responding to CCK8 in a dose-related manner (threshold dose < 5 pmol), and that the administration of CCK1-receptor antagonist (devazepide) abolished an enhanced discharge in vagal afferent fibres induced by CCK8 application. The CCK-sensitive subpopulations of mesenteric afferent nerves slowly adapted to luminal hydrochloric acid and were not sensitive to intestinal distension. Luminal application of lignocaine transiently abolished the response to CCK, which further confirms the localisation of receptor afferents within the intestinal mucosa. Abdominal vagotomy eliminated the responses to CCK suggesting that the CCK-sensitive mucosal afferents exclusively follow the vagal pathway to the CNS to trigger various reflexes controlling behavioural and GIT effects involving inhibition of gastric motility and stimulation of pancreatic secretion. Consistently, studies in rats have indicated that intraduodenal sodium oleate, a major stimulator of pancreatic secretion, evoked the firing in the mucosal afferent fibres that could be abolished by the CCK1 receptor antagonist, devazepide (Lal et al. Reference Lal, Kirkup, Brunsden, Thompson and Grundy2001).
The existence of CCK receptors in the gut mucosa suggested by electrophysiology recordings have been further supported by autoradiographic studies in rats by Lin & Miller (Reference Lin and Miller1992) and Moriarty et al. (Reference Moriarty, Dimaline, Thompson and Dockray1997). Their competition studies using selective CCK ligands revealed that the vagal CCK receptors are heterogeneous. Accordingly, Miyasaka et al. (Reference Miyasaka, Masuda, Kawanami and Funakoshi1996) have found expression of the CCK1 and CCK2 receptors' mRNA in the duodenal mucosa of the rat using the RT-PCR technique. More recently, an association of mucosal CCK1 and CCK2 receptors with neural components of the small intestine has been indicated in calves and rats using immunocytochemistry (Zabielski et al. Reference Zabielski, Morisset, Podgurniak, Romé, Biernat, Bernard, Chayvialle and Guilloteau2002). The CCK receptors were localised in the intestinal villi within the lamina propria; however, little immunoreactivity could be observed close to the basal part of the enterocytes. In order to visualise the vagal sensory innervation of the gut, Berthoud et al. (Reference Berthoud, Kressel, Raybould and Neuhuber1995) labelled the vagal afferents in vivo using injection of the lipophilic carbocyanine dye DiI into the nodose ganglion of rats. The DiI-labelled vagal afferent fibres were found with terminal arborisations mainly between the crypts and in the villous lamina propria. In both areas, vagal terminal branches came in close contact with the basal lamina, but did not appear to penetrate in it so as to make direct contact with epithelial cells or to penetrate between the epithelial cells into the lumen. The overall density of vagal afferent mucosal innervation was variable in their preparations. Many villi showed no evidence for such innervation while other areas had quite dense networks of arborising terminal fibres in several neighbouring villi. Using a similar approach, Berthoud & Patterson (Reference Berthoud and Patterson1996) examined the anatomical relationship between vagal afferents and I-cells in the rat small intestine. They demonstrated that the CCK immunoreactive cells were more abundant than vagal afferent fibres, and that both of them were present throughout the small intestine in the crypt and villi region. Most of the labelled vagal afferent axons distributed within the crypt and villous lamina propria were at distances of tens to hundreds of μm to the nearest CCK immunoreactive cell. Only a few of the CCK immunoreactive cells were in close ( < 5 μm) anatomical contact with vagal afferent axons. These anatomical studies suggest that CCK released from the I-cells may act on vagal sensory fibres in a paracrine fashion and help to understand the sense of the luminal release of CCK; since only some of the villi contain the sensory fibres for CCK, the release of CCK into the gut lumen might be a safe way (little biodegradation in the lumen) to spread the stimulus over a larger receptive area. Accordingly, the process of luminal CCK absorption by enterocytes may be an important link between the food and CCK–vagal mechanisms controlling GI function.
There is also growing evidence that gastrin may act through CCK2 receptors located on the vagal afferents. Moriarty et al. (Reference Moriarty, Dimaline, Thompson and Dockray1997) demonstrated by autoradiography approximately three-fold higher abundance of CCK1 receptors compared with CCK2 receptors, and no significant representation of CCK-C receptors on afferent fibres in the rat vagal nerve. They also demonstrated that CCK1 and CCK2 receptors are synthesised by nodose ganglion cells and that the receptor proteins are transported to the periphery along afferent fibres. Immunocytochemistry studies in rat and calf mucosa showed a co-localisation of CCK1 and CCK2 receptors with neural fibres (Zabielski et al. Reference Zabielski, Morisset, Podgurniak, Romé, Biernat, Bernard, Chayvialle and Guilloteau2002). Our more recent studies in preruminant calves suggest that gastrin administrated into the duodenal lumen may stimulate the exocrine pancreas via CCK2 receptors localised on vagal afferents in the duodenal mucosa (Zabielski et al. Reference Zabielski, Normand, Romé, Chayvialle, Wolinski and Guilloteau2004). Danzer et al. (Reference Danzer, Jocic, Samberger, Painsipp, Bock, Pabst, Crailsheim, Schicho, Lippe and Holzer2004) found that vagal afferents transmit physiological gastrin stimuli from the stomach to the brain stem in rats. Further studies on the involvement of vagal nerves would be helpful to define the mechanism more precisely.
Effects of the cholecystokinin—gastrin family peptides through cholecystokinin 1 receptor occupation on normal organs: secretion of pancreatic enzymes
From studies performed on isolated rat pancreatic acini, it was demonstrated that physiological concentrations of CCK caused amylase release (Wank, Reference Wank1995), an effect totally blocked by the CCK1 receptor antagonist L-364,718 (Chang & Lotti, Reference Chang and Lotti1986). The potent secretagogue action of CCK was shown in healthy human subjects by increasing pancreatic lipase concentrations in duodenal fluid (Conwell et al. Reference Conwell, Zuccaro, Morrow, Van Lente, O'Laughlin, Vargo and Dumot2002). A similar action on dog pancreatic amylase secretion was also confirmed in vivo under constant CCK8 infusion, an effect also blocked by the specific CCK1 receptor antagonist L-364,718 (Hosotani et al. Reference Hosotani, Chowdhury, McKay and Rayford1987). However, in man, pancreatic acini cells do not seem to respond directly to CCK1 and CCK2 receptor activation, and this is probably due to an insufficient level of receptor expression (Ji et al. Reference Ji, Bi, Simeone, Mortensen and Logsdon2002). Moreover, it was recently shown in rodents that the isolated duck pancreatic acini possess both CCK1 and vasointestinal polypeptide–pituitary adenylate cyclase-activating polypeptide receptors and that simultaneous activation of both is required for each to play a physiological role (Xiao & Cui, Reference Xiao and Cui2004). The stimulatory effects of CCK and analogues on pancreatic enzyme secretion were also observed in guinea-pigs and mice and that are resulted from occupation of the CCK1 receptor (Sankaran et al. Reference Sankaran, Goldfine, Bailey, Licko and Williams1982; Jensen et al. Reference Jensen, Wank, Rowley, Sato and Gardner1989). Indeed, the presence of CCK1 receptor on rat and mouse pancreatic acinar cells was visualised by immunofluorescence with a specific CCK1 receptor antibody (Bourassa et al. Reference Bourassa, Lainé, Kruse, Gagnon, Calvo and Morisset1999). In preruminant calves, the presence of CCK1 receptor was shown in the pancreas tissue (Le Meuth et al. Reference Le Meuth, Philouze-Rome, Le Huërou-Luron, Formal, Vaysse, Gespach, Guilloteau and Fourmy1993) and functional studies with the use of specific pharmacological CCK1 and CCK2 receptor antagonists indicated that endogenous CCK controls pancreas enzyme secretion via a direct action on the pancreatic acini as well as via a neurohormonal mechanism associated with the presence of CCK receptors on vagal afferent nerves in the duodenal mucosa (Zabielski et al. Reference Zabielski, Leśniewska, Borlak, Gregory, Kiela, Pierzynowski and Barej1998b, Reference Zabielski, Morisset, Podgurniak, Romé, Biernat, Bernard, Chayvialle and Guilloteau2002, Reference Zabielski, Normand, Romé, Chayvialle, Wolinski and Guilloteau2004). The relative contribution of these mechanisms may depend on the stage of postnatal development of the duodenum and pancreas (Biernat et al. Reference Biernat, Zabielski, Sysa, Sosak-Świderska, Le Huerou-Luron and Guilloteau1999). Studies in anaesthetised rats with CCK peptide and CCK1 receptor antagonists administrations showed similar results (Li & Owyang, Reference Li and Owyang1993, Reference Li and Owyang1994), leading to a conclusion that in physiological conditions the prandial secretory response of the exocrine pancreas is chiefly driven by a neurohormonal mechanism, and a direct interaction of CCK with CCK1 receptor on pancreatic acini is just a pharmacological effect (Owyang, Reference Owyang1996).
Effects of the cholecystokinin—gastrin family peptides through cholecystokinin 1 receptor occupation on normal organs: secretion of islet hormones
CCK is also involved in endocrine pancreas secretion as it induces insulin secretion in vivo through CCK1 receptor occupation (Rosseti et al. Reference Rosseti, Shulman and Zawalich1987; Karlson & Ahren, Reference Karlsson and Ahren1992). This regulatory peptide was also associated with pancreatic polypeptide release (Liddle et al. Reference Liddle, Gertz, Kanayama, Beccaria, Gettys, Taylor, Rushakoff, Williams and Coker1990) and possibly glucagon (Schweiger et al. Reference Schweiger, Erhard and Amselgruber2000). These CCK1 receptors were indeed localised on islet cells (Bourassa et al. Reference Bourassa, Lainé, Kruse, Gagnon, Calvo and Morisset1999) and more specifically on insulin and glucagon cells in at least seven different species (Morisset et al. Reference Morisset, Julien and Lainé2003).
Effects of the cholecystokinin—gastrin family peptides through cholecystokinin 1 receptor occupation on normal organs: growth of the pancreas
CCK given in an amount that will induce plasma levels that are comparable with those following a meal induced enzyme secretion as well as growth of the rat pancreatic gland (Solomon et al. Reference Solomon, Petersen, Elashoff and Grossman1978) as indicated by significant increases in pancreatic weight, in total enzyme and protein contents as well as RNA and DNA (Solomon et al. Reference Solomon, Vanier and Morisset1983). This trophic action of CCK can be obtained whether CCK was exogenously administered (Solomon et al. Reference Solomon, Vanier and Morisset1983) or endogenously released either by feeding a high-protein diet (Morisset et al. Reference Morisset, Guan, Jurkowska, Rivard and Green1992) or following pancreatic juice diversion (Rivard et al. Reference Rivard, Guan, Maouyo, Grondin, Bérubé and Morisset1991) and CCK exerts this trophic effect, not via a vagal afferent pathway, but directly on the pancreas, in vivo (Yamamoto et al. Reference Yamamoto, Otani, Jia, Fukumitsu, Yoshikawa, Akiyama and Otsuki2003). In each situation, the CCK1 receptor implicated as the response to CCK was abolished by the specific CCK1 receptor antagonist L-364,718 (Rivard et al. Reference Rivard, Guan, Maouyo, Grondin, Bérubé and Morisset1991; Morisset et al. Reference Morisset, Guan, Jurkowska, Rivard and Green1992) Moreover, CCK and gastrin are implicated in the growth of the exocrine pancreas by causing hypertrophy and hyperplasia (Baldwin, Reference Baldwin1995) and increasing DNA, RNA and the protein contents of rat pancreas (Johnson, Reference Johnson1981). Administration of CCK8 caused both increased proliferation and apoptosis in the pancreas. In the case of continuous administration of CCK8, the proliferation outweighs the apoptosis, causing hyperplasia, but, in the case of intermittent administration, the opposite effect was observed (Trulsson et al. Reference Trulsson, Svanvik, Permert and Gasslander2001).
Effects of the cholecystokinin—gastrin family peptides through cholecystokinin 1 receptor occupation on normal organs: gallbladder contraction
CCK1 receptors were identified on human gallbladder smooth muscle and are responsible for the action of CCK in stimulating gallbladder contraction (Schjoldager et al. Reference Schjoldager, Molero and Miller1989), a physiological response blocked by the CCK1 receptor antagonist devazepide (Liddle et al. Reference Liddle, Gertz, Kamayama, Beccaria, Coker, Turnbull and Marita1989). From CCK8 binding studies, the CCK1 receptor was also identified on human gallbladder muscles (Tang et al. Reference Tang, Biemond and Lamers1996). Studies performed on dog gallbladder smooth muscle layers in vitro indicate that their contractions in response to CCK8 were atropine and tetradotoxin resistant, but completely eliminated by devazepide. However, postprandrial gallbladder contractions were partially inhibited by atropine and hexamethonium, and completely abolished by devazepide. These studies suggested that postprandial CCK-induced gallbladder contractions are controlled by CCK1 receptors both on the vagal nerve in stimulating endogenous acetylcholine release and on the gallbladder for stimulating muscle contraction (Sonobe et al. Reference Sonobe, Sakai, Satoh, Haga and Itoh1995). The relative contribution of these CCK1 receptors was elucidated in human subjects by Zhu et al. (Reference Zhu, Han, Chen, Jiang and Zhang2005), who found interactive relationships between the gallbladder motor function, plasma CCK and CCK2 receptor of gallbladders in patients with cholesterol stone disease. As a conclusion, these studies indicate that CCK affects gallbladder contractions chiefly in a hormonal manner, which is in contrast to a neurohormonal (CCK1 and vagal-dependent) mechanism dedicated to the exocrine pancreas.
Effects of the cholecystokinin—gastrin family peptides through cholecystokinin 2 receptor occupation on normal organs: secretion of pancreatic enzymes
The control of pancreatic enzyme secretion in rodents involves occupation of the CCK1 receptors on acinar cells as described earlier. However, the presence of these CCK1 receptors on pancreatic acinar cells of larger mammals has not yet been documented nor confirmed; at least, they were not found on calf, pig, horse and human acinar cells by immunofluorescence (Morisset et al. Reference Morisset, Julien and Lainé2003). The presence of CCK2 receptors in the pancreas was firstly observed in the calf (Le Meuth et al. Reference Le Meuth, Philouze-Rome, Le Huërou-Luron, Formal, Vaysse, Gespach, Guilloteau and Fourmy1993; Desbois et al. Reference Desbois, Huerou-Luron, Dufresne, Estival, Clerc, Rome, Clemente, Guilloteau and Fourmy1999) and then in the pig (Philippe et al. Reference Philippe, Lhoste, Dufresne, Moroder, Corring and Fourmy1997) by binding and photoaffinity labelling studies or by in situ hybridation and in man by storage phosphor autoradiography after radioligand binding to a tissue section (Tang et al. Reference Tang, Biemond and Lamers1996). Similarly, amylase release from isolated pig acini in response to caerulein indicated stimulation in the nm range, a typical CCK2 response not inhibited by the CCK1 receptor antagonist MK-329 (Morisset et al. Reference Morisset, Levenez, Corring, Benrezzak, Pelletier and Calvo1996). More recently, however, it was clearly demonstrated that freshly isolated human pancreatic acini neither release amylase in response to CCK8 nor to gastrin; a secretory response to carbachol was shown to document viability of the acini preparation as well as a response to CCK8 following CCK2 receptor transfection in these acini (Ji et al. Reference Ji, Bi, Simeone, Mortensen and Logsdon2001). To understand how pancreatic enzyme secretion is controlled by CCK in larger mammals and also possibly in rodents, future studies will have to focus on vagovagal reflex stimulation as elegantly described and documented by Konturek et al. (Reference Konturek, Zabielski, Konturek and Czarnecki2003b) from an earlier observation that pancreatic enzyme secretion induced by CCK and secretin in human subjects was inhibited not only by the CCK1 receptor antagonist loxiglumide but also by atropine. It suggests that neuronal pathways play an important role in the action of CCK on pancreatic enzyme secretion (Gabryelewicz et al. Reference Gabryelewicz, Kulesza and Konturek1990; Owyang, Reference Owyang1996) (see pp. 260–262).
Effects of the cholecystokinin—gastrin family peptides through cholecystokinin 2 receptor occupation on normal organs: growth of the pancreas
The factors regulating intra-uterine fetal growth of specific organs have remained largely unknown. The estimation that fetal pancreas contains between 2·2 and 4 ng of gastrin (Brand & Fuller, Reference Brand and Fuller1988) and a majority of CCK2 receptors (Morisset et al. Reference Morisset, Wong, Walsh, Lainé and Bourassa2000b) lets us believe that this CCK2 receptor subtype could be involved in fetal pancreas development. From studies performed with a CCK2 receptor antagonist (Morisset et al. Reference Morisset, Lainé and Mimeau-Worthington1999) and gastrin immunoneutralisation (Feurle et al. Reference Feurle, Hamscher and Firat1995), both infused subcutaneously in the back of the dams for 28 d, showed that gastrin was involved in fetal pancreatic organogenesis. It remains to be seen if these gastrin effects are confined to rodents' pancreas. However, after birth, gastrin mRNA expression and the hormone content disappeared in the rat pancreas (Morisset et al. Reference Morisset, Lainé and Mimeau-Worthington1999) and the CCK2 receptors remained on the endocrine Δ cells (Morisset et al. Reference Morisset, Julien and Lainé2003); so it was not surprising to observe that postnatally, gastrin lost its trophic effect on the pancreatic gland as documented by many investigators (Chen et al. Reference Chen, Nylander, Norlen and Hakanson1996). Recently, evidence was presented for heterodimerisation of type 1 and 2 CCK receptors and that this complex can, once formed in transfected cells, become a powerful unit in promoting cell growth (Cheng et al. Reference Cheng, Harikumar, Holicky and Miller2003). It is therefore believed that future studies on control of pancreas growth in large mammals should pay attention to this heterodimerisation phenomenon (see pp. 270–271) of the CCK receptors, now that we know that the pig pancreas can regenerate after pancreatectomy (Morisset et al. Reference Morisset, Morisset, Lauzon, Côté, Lainé, Bourassa, Lessard and Echavé2000a). In another way, whereas vagal hyperactivity itself stimulates cell proliferation of pancreatic β- and acinar cells primarily through a cholinergic receptor in man (Kiba et al. Reference Kiba, Tanaka, Numata, Hoshino, Misugi and Inoue1996), it was recently shown that CCK exerts a trophic effect not via a vagal afferent pathway but directly on the pancreas in the rat (Yamamoto et al. Reference Yamamoto, Otani, Jia, Fukumitsu, Yoshikawa, Akiyama and Otsuki2003).
Effects of the cholecystokinin—gastrin family peptides through cholecystokinin 2 receptor occupation on normal organs: histamine release and hydrochloric acid secretion
Gastric acid secretion from the parietal cells is regulated by the enteric nervous system, the CNS, and neuroendocrine cells whose products act as autocrine and/or paracrine factors. Gastrin is primarily involved in stimulating ECL cells to secrete histamine via CCK2 receptor occupation (Roche et al. Reference Roche, Gusdinar, Bali and Magous1991; Bakke et al. Reference Bakke, Qvigstad, Sandvik and Waldum2001); it also seems to have a minimal effect on the parietal cells through the same CCK2 receptor (Schmidt & Schmitz, Reference Schmidt and Schmitz2004), even if no CCK2 receptor were evidenced on these cells (Bakke et al. Reference Bakke, Qvigstad, Sandvik and Waldum2001). From recent studies performed in gastrin CCK− / − mice, it became clear that the major effect of CCK was to inhibit acid secretion by activating CCK1 receptors on somatostatin cells in the antral mucosa in order to inhibit gastrin release. In the oxyntic mucosa, CCK was shown to control histamine release (Chen et al. Reference Chen, Zhao, Hakanson, Samuelson, Rehfeld and Friss-Hansen2004). This mechanism was also demonstrated in the rat (Woltman & Reidelberger, Reference Woltman and Reidelberger1999; Lloyd et al. Reference Lloyd, Raybould and Walsh1992, Reference Lloyd, Wang and Solomon2001), in sheep (Zavros & Shulkes, Reference Zavros and Shulkes1997) and in man (Schmidt et al. Reference Schmidt, Schenk, Nustede, Holst, Folsch and Creutzfeldt1994) via occupation of the CCK2 receptors present on the ECL cells (Modlin & Tang, Reference Modlin and Tang1996).
Effects of the cholecystokinin—gastrin family peptides through cholecystokinin 2 receptor occupation on normal organs:leptin secretion
Leptin, the product of the ob gene, was initially identified in adipocytes (Zhang et al. Reference Zhang, Proenca, Maffei, Barone, Leopold and Friedman1994) and later in the stomach (Bado et al. Reference Bado, Levasseur and Attoub1998). Control of appetite and body-weight homeostasis are among its most important physiological functions. Leptin secretion was described under the control of gastrin through occupation of the CCK2 receptor (Attoub et al. Reference Attoub, Levasseur, Buyse, Goïot, Laigneau, Moizo, Hervatin, Le Marchand-Brustel, Lewin and Bado1999) as its release in plasma was significantly inhibited in vivo by the CCK2 receptor antagonist YM022. However, leptin was shown to be synthesised and secreted in canine gastric chief cells in response to CCK via the high-affinity state of the CCK1 receptors (Tsunoda et al. Reference Tsunoda, Yao, Park and Owyang2003). Furthermore, gastrin is also involved in leptin synthesis in mesenteric, epididymal and perirenal adipose tissues as it regulates the ob gene and, thus, control the expression of ob mRNA.
Results of cholecystokinin gastrin receptor occupation on normal organs
Gastrin can also bind to the 78 kDa gastrin-binding protein, i.e. the so-called ‘CCKc gastrin receptor’ (Baldwin et al. Reference Baldwin, Chandler, Scanlon and Weinstock1986). It seems that this receptor subtype has been detected on isolated gastric parietal cells. CCKc receptor binds both amidated and non-amidated gastrins at a low affinity and is not related in structure to the classical CCK or gastrin receptors, and belongs to the family of enzymes involved in β-oxidation of fatty acids (Aly et al. Reference Aly, Shulkes and Baldwin2004). CCKc receptors could also be expressed in a large proportion of glioma cells (Lefranc et al. Reference Lefranc, Sadeghi, Metens, Brotchi, Salmon and Kiss2003) but its role on these cells has not yet been characterised.
Local effects of cholecystokinin and gastrin in the gut
Gut development: maturation (remodelling of the gut mucosa) and growth
The trophic effects of plasma gastrin were initially demonstrated 30 years ago. Thus the trophic effects on the stomach and proximal small intestine are well documented but on the colon are not well established (FitzGerald et al. Reference FitzGerald, Ghatei, Mandir, Bloom, Iversen and Goodlad2002) as well as in the oxyntic and duodenal mucosa (Johnson, Reference Johnson1976). In the developing rat (from fetal stage until weaning), the oxyntic mucosa would be under functional and trophic control of circulating gastrin and it was thought therefore that gastrin would play a role in the maturation and growth of the mucosa. This was particularly demonstrated after antrectomy in fetal sheep (Avila et al. Reference Avila, Harding, Young and Robinson1989) following parenteral nutrition or oral ingestion in the rat (FitzGerald et al. Reference FitzGerald, Ghatei, Mandir, Bloom, Iversen and Goodlad2002). But it was recently shown that gastrin affects neither the oxyntic mucosa nor the endocrine cells before weaning in rat stomach. After weaning, CCK2 receptor blockade is associated with a somewhat impaired development of the oxyntic mucosa and the ECL cells. While gastrin stimulation is of crucial importance for the onset of acid secretion during weaning and for the activation of ECL-cell histamine formation and secretion, the mucosa and ECL-cell growth at this stage is only partly gastrin dependent. In contrast, the development of the ghrelin-producing A-like cells is independent of gastrin at all stages (Björkqvist et al. Reference Björkqvist, Dornonville de la Cour, Zhao, Gagnemo-Persson, Hakanson and Norlen2002). Gastrin is implicated in a marked proliferative action on the proximal small intestine which diminishes distally, but evidence for a trophic effect on the colon is very limited (FitzGerald et al. Reference FitzGerald, Ghatei, Mandir, Bloom, Iversen and Goodlad2002; Thomas et al. Reference Thomas, Hellmich, Townsend and Evers2003). CCK stimulates growth of the pancreas in experimental studies (Brants & Morisset, Reference Brants and Morisset1976; Folsch et al. Reference Folsch, Winckler and Wormsley1978). However, evidence for CCK playing a major role in the growth of the GI mucosa (stomach, small bowel and colon) is limited (Thomas et al. Reference Thomas, Hellmich, Townsend and Evers2003). Gastrin administered directly into the lumen of the small intestine of rats produces trophic effects without changes in circulating gastrin (Johnson, Reference Johnson1981), but no effect was observed when gastrin was infused into the stomach, indicating no physiological role for luminal gastrin in the normal acid-secreting stomach. Following an intraduodenal CCK1 receptor antagonist, it was shown in the neonal calf that CCK controls the hyperplasic and hypertrophic development of the pancreas as well as the growth and maturation of the small-intestinal mucosa (mitotic index and depth of crypt, width and surface area of the villi, presence of empty vacuoles) (Biernat et al. Reference Biernat, Zabielski, Sysa, Sosak-Świderska, Le Huerou-Luron and Guilloteau1999). Gastrin, as well as CCK, is present in relatively high concentrations in fetal gastric juice in calves (Guilloteau et al. Reference Guilloteau, Le Huërou-Luron, Le Dréan, Gestin, Philouze-Romé, Artiaga, Bernard and Chayvialle1998) and in sheep (Shulkes et al. Reference Shulkes, Chick and Hardy1984); gastrin in the lumen of the GIT may have a unique maturational role (Grand et al. Reference Grand, Watkins and Torti1976). But, recent studies indicate that the gastrin precursors and intermediates (progastrin and Gly-gastrin) are putative growth factors. Thus, preprogastrin gives a variety of products, each with a distinctive spectrum of biological activity. Progastrin itself stimulates colonic epithelial proliferation; biosynthetic intermediates (Gs-Gly) stimulate colonic epithelial proliferation and gastric epithelial differentiation; C-terminally amidated gastrins stimulate colonic proliferation, gastric epithelial proliferation and differentiation (acid-producing parietal cells and histamine-secreting ECL cells) (Dockray, Reference Dockray1999; Dockray et al. Reference Dockray, Varro, Dimaline and Wang2001). The rise in serum gastrin at weaning coincides with a rapid increase in the number and activity of the ECL cells and an increased thickness of the oxyntic mucosa (Björkqvist et al. Reference Björkqvist, Dornonville de la Cour, Zhao, Gagnemo-Persson, Hakanson and Norlen2002). Moreover, long-term hypergastrinaemia brings about ECL-cell hypertrophy and hyperplasia (Havu, Reference Havu1986).
Gastrointestinal motility
Gastric emptying plays a key role in the regulation of food intake by controlling the flow of nutrients to their absorption sites in the small intestine. Among the many hormones and neuropeptides involved in the regulation of gastric emptying, CCK seems to play a prominent role in the early postprandial period, in postprandial CCK release and in the delay of gastric emptying (Olsson & Holmgren, Reference Olsson and Holmgren2001; Leray et al. Reference Leray, Segain, Cherbut and Galmiche2003). In healthy human subjects, the ingestion of fatty acids, which releases CCK, reduces the volume of liquid delivered into the duodenum, primarily via a CCK-1 receptor-mediated delay in gastric emptying (Lal et al. Reference Lal, McLaughlin, Barlow, D'Amato, Giacovelli, Varro, Dockray and Thompson2004). Chronic nutritional disorders such as protein malnutrition are associated with delayed gastric emptying and increased postprandial plasma CCK levels. In rats adapted to a low-protein diet, gastric emptying was delayed whereas postprandial CCK levels were increased. A low-protein diet enhanced antral muscle contractile response to CCK and caerulein without altering response to acetylcholine. This increased contractility was associated with up regulation of CCK1 receptor mRNA levels in antral muscle. These data suggest that modulation of gastric emptying after adaptation to a low-protein diet involves up regulation of both CCK1 receptors and CCK-induced contraction of antral smooth muscle (Leray et al. Reference Leray, Segain, Cherbut and Galmiche2003). In male rats, oxytocin administration inhibits gastric emptying which occured concomitantly with an increase in plasma CCK concentrations. The results obtained suggest that CCK1, but not CCK2, receptors are involved in the mechanism and are consistent with the concept that oxytocin, in association with CCK, plays important roles in regulating gastric motility and food intake (Wu et al. Reference Wu, Hung, Chang, Pau, Wang and Wang2002).
Moreover, CCK stimulates intestinal motility and gallbladder contractions (Niedereau & Karaus, Reference Niederau and Karaus1991; Morton et al. Reference Morton, Welsh, Tavares and Shankley2002; Krishnamurthy et al. Reference Krishnamurthy, Cerulli-Switzer, Chapman and Krishnamurthy2003). But the action of CCK on GI motility is complex and dependent on many physiological factors (Romanski, Reference Romanski2004). The distance from the pylorus seems to be essential and an important difference in CCK action on duodenum, jejunum and ileum was observed. This can be caused by the variability in the smooth muscle CCK-receptor density along the small intestine, the spectrum of CCK action as neuropeptide (Sayegh & Ritter, Reference Sayegh and Ritter2003), different hormonal regulation and up and down regulatory processes (Mawe, Reference Mawe1998; Noble et al. Reference Noble, Wank, Crawley, Bradwejn, Seroogy, Hamon and Roques1999). In young milk-fed calves, intraduodenal infusion of CCK9 increased the duration of phase II (irregular spiking activity) without any effect on the duration of phase I (no spiking activity) and III (regular spiking activity). Infusion of gastrin had no effect on duodenal MMC (Zabielski et al. Reference Zabielski, Normand, Romé, Chayvialle, Wolinski and Guilloteau2004). In human subjects, Verkijk et al. (Reference Verkijk, Gielkens, Lamers and Masclee1998) studied the effect of gastrin on the small-intestinal MMC using antroduodenal manometry simultaneous with intraluminal acidity recording. Continuous infusion of gastrin-17 (20 pmol/kg) increased intragastric and intraduodenal acidity and suppressed phase II and phase III motor activity in both antrum and duodenum. Pharmacological block of gastric acid secretion completely antagonised the effect of gastrin on the MMC; thus the authors concluded that the effect of gastrin on interdigestive antroduodenal motility results from increased intraluminal acidity in human subjects.
Intervention of nitric oxide
NO is a messenger molecule that acts via the cellular cGMP pathway and is involved in several regulatory processes. Endogenous NO is generated mainly from the amino acid l-arginine, a process catalysed by NO synthases (NOS) which exists in two constitutive (endothelial NOS and neuronal NOS) and one inducible NOS isoform.
Intervention of nitric oxide: local blood flow
Konturek et al. (Reference Konturek, Bilski, Konturek, Cieszkowski and Pawlik1993) were the first to demonstrate in fistulated dogs, with pancreatic blood flow measured by laser Doppler flowmetry, that endogenous NO affects pancreatic secretion through the changes in the vascular bed. They found that besides sham-feeding and meal feeding, continuous infusions of secretin plus CCK markedly induced pancreatic protein outputs. Infusion of a non-specific inhibitor of NOS (L-NNA) caused a profound inhibition of these secretions, whereas the addition of l-arginine reversed this inhibition in part. NO did not affect basal or CCK-induced amylase release from isolated pancreatic acini. In anaesthetised dogs, infusion of NG-nitro-l-arginine caused a significant reduction in the pancreatic blood flow both while resting and following stimulation with secretin plus CCK but did not affect this flow in animals treated with glyceryl trinitrate. Addition of l-arginine attenuated the decrease in pancreatic blood flow and the increase in systemic blood pressure caused by L-NNA. The authors wrote that a considerable part of circulating CCK and secretin effects is related to vasodilatation produced by NO. Soon their results were confirmed in rat in vivo and in vitro studies (Konturek et al. Reference Konturek, Szlachcic, Dembiński, Warzecha, Jaworek and Stachura1994). In caerulein-induced acute pancreatitis, L-NNA significantly potentiated the inflammatory changes in the pancreas caused by caerulein in rats. Addition of l-arginine enhanced the pancreatic blood flow and ameliorated the pancreatitis induced by caerulein alone or that combined with L-NNA. Iwase et al. (Reference Iwase, Uchizono, Nakamura, Nohara and Iida2003) confirmed that exogenous CCK was a potent vasodilatator of exocrine as well as islet vasculature in the pancreas. Since both the insulinotropic and vasodilatating effects were totally absent in CCK1 receptor-null Otsuka Long-Evans Tokushima fatty (OLETF) rats, these effects were mediated through the CCK1 receptor. CCK mediates vasodilatation of the mesenteric vascular bed through the release of NO by neuronal NOS via its presynaptic CCK2 receptors, suggesting a neural mechanism by which CCK may increase mesenteric blood flow (Sanchez-Fernandez et al. Reference Sanchez-Fernandez, Gonzalez, Beart, Mercer, Ruiz-Gayo and Fernandez-Alfonso2004). Although CCK secreted posprandially from intestinal endocrine cells apparently stimulates pancreatic exocrine secretion and blood flow, the physiological significance of CCK action on islet blood flow is not clear yet. It is possible that the increased islet blood flow may facilitate the disposal of insulin to the target tissue after meals and by the way induce the insulo–acinar axis controlling the exocrine pancreas. In addition, since vagotomy affected basal fractional islet blood flow, the vagus nerve may regulate blood flow distribution within the pancreas (Iwase et al. Reference Iwase, Uchizono, Nakamura, Nohara and Iida2003). NO is a potent vasodilator and has also been shown to play an important role in regulating the gastric mucosal microcirculation (Whittle, Reference Whittle1993).
Intervention of nitric oxide: pancreas growth and secretion
Trulsson et al. (Reference Trulsson, Gasslander, Sundqvist and Svanvik2002), from an in vivo study in rats, demonstrated that endogenous NO production interacts with tissue homeostasis in the pancreas. Their studies on the exocrine pancreas indicate that endogenous NO formation reduces apoptosis both during basal conditions and during simultaneous stimulation with CCK8. Cell proliferation is stimulated by NO under basal conditions. In CCK-induced hyperplasia, NO inhibits the proliferation of acinar cells but stimulates the proliferation of ductal cells. Endogenous NO thus may have a regulatory role in the balance between proliferation and apoptosis in the exocrine pancreas. In a situation of strong growth stimulation by CCK8, NO seems to have a tonic inhibition of both cell synthesis and apoptosis, thus slowing down the acinar cell turnover in the pancreas. Further, during these conditions, NO seems to have a cell-type specific effect, different on acinar and ductal cell proliferation. Treatment of rat pancreatic acinar cells by CCK8 in vitro increases arginine conversion to citrulline as well as cGMP and activation of the l-arginine–NO pathway facilitates basal and stimulated pancreatic secretion in vivo (Trulsson et al. Reference Trulsson, Gasslander, Sundqvist and Svanvik2002).
Intervention of nitric oxide: motility
CCK activates specific enteric neuronal phenotypes in both the myenteric and the submucosal plexus. CCK activates NOS immunoreactive neurons which are probably inhibitory motor neurons in the myenteric plexus and putative intrinsic secretomotor and sensory neurons in the submucosal plexus (Sayegh & Ritter, Reference Sayegh and Ritter2003). These results support a role for CCK in the integration of reflex control of intestinal motility and secretion via actions of both efferent and afferent components of intrinsic intestinal reflex arcs.
Intervention of nitric oxide: cytoprotection
CCK-induced gastroprotection and hyperaemia were mediated by increased release of NO (West et al. Reference West, Helmer, Chang, Cui, Greeley and Mercer2003) and it was suggested that constitutive isoforms of NOS were responsible for mediating CCK-induced gastroprotection and hyperaemia. CCK and CCK secretagogues are potent gastroprotective agents against a variety of luminal irritants, particularly in response to a meal. CCK seems to exert its gastroprotective effects by increasing gastric mucosal blood flow. The mediator appears to be NO, and CCK increases NOS activity. However, basal levels of endogenous prostaglandins also appear to be necessary in order for CCK to fully exert its gastroprotective action (West & Mercer, Reference West and Mercer2004). Endogenous gastrin is released by BBS and activates production of NO (West & Mercer, Reference West and Mercer2005) through activation of constitutive NOS isoforms, and increased cyclo-oxygenase activity leads to increased production of prostaglandins. Thus, CCK8 (but also secretin, carbachol and PG E2) strongly stimulated mucus secretion from cultured rat gastric epithelial cells and gastrin stimulated it weakly (Tani et al. Reference Tani, Suzuki, Kano, Tanaka, Sunaga, Morishige and Tsuda2002). It seems likely that mucus secretion results from the existence of interaction among receptors (Tani et al. 2002).
In the case of pancreatic duct occlusion, Miyasaka & Funokosi (Reference Miyasaka and Funakoshi2003) have found that the changes in the CCK content in the proximal intestine were correlated with increases and decreases in inflammation and then with regenerative change in the pancreas. In the case of cell injury processes of pancreatitis, CCK stimulates apoptosis and death-signalling pathways in rat pancreatic acinar cells, including caspase activation, cytochrome c release, and mitochondrial depolarisation (Gukovskaya et al. Reference Gukovskaya, Gukovsky, Jung, Mouria and Pandol2002). In rat gastric epithelial cancer cells, gastrin shows anti-apoptotic activity through the up regulation of an active protein in the apoptosis processing and surviving (Konturek et al. Reference Konturek, Konturek, Bielanski, Karczewska, Zuchowicz, Hartwich, Rehfeld, Goetze and Hahn2003a).
Intervention of nitric oxide: defence–immune system
The GI system is innervated by the autonomous and the enteric nervous systems. Peptidergic nerve fibres are found in close approximation with immune cells of the GIT and evidence suggests an enteric nervous system influence on the body's immune response. GRP is released early in the digestive process to stimulate release of other neuropeptides such as CCK and gastrin. It was previously demonstrated that lack of enteral feeding with parenteral nutrition administration suppressed CCK secretion (Genton & Kudsk, Reference Genton and Kudsk2003). Parenteral nutrition with supplemental CCK, gastrin (or neurotensin) prevented most of the changes in relation to the gut-associated lymph tissue with this type of nutrition. This suggests that multiple hormone releases in response to feeding is necessary to preserve maximal mucosal immunity. Some neuropeptides, particularly CCK (GRP and neurotensin), appear promising to maintain mucosal immunity in patients who cannot receive enteral feeding during critical illness or after GIT loss (Genton & Kudsk, Reference Genton and Kudsk2003).
Control of pancreatic function through vagal afferent pathways
According to classical hormone theory, exogenous CCK evokes dose-dependent stimulation of pancreatic enzyme secretion. However, effective doses increase the concentration of CCK in the circulating blood to a level that cannot be achieved by any stimulation of endogenous CCK release. Thus, these effects have to be considered pharmacological. On the other hand, low doses of exogenous CCK (keeping the increase in the circulating blood within the physiological range) hardly affect pancreatic secretion and cannot convincingly explain its role in the regulation of pancreatic secretion. Moreover, stimulation with a low dose of CCK can be abolished by atropine or cold blockade of the vagal nerves, suggesting involvement of neural pathways. Magee & Naruse (Reference Magee and Naruse1983, Reference Magee and Naruse1988) explained this by an interplay between the nervous and hormonal regulation systems at the level of intrapancreatic nerves and ganglions. However, studies comparing the secretory responses to CCK8 administered into the general circulation or locally into a branch of the right gastroepiploic artery, which supplies the proximal duodenum (but not the pancreas), showed more pronounced responses following the intra-arterial infusions in both conscious and anaesthetised animals (Pierzynowski et al. Reference Pierzynowski, Mårtensson, Ahrén and Weström1991; Zabielski et al. Reference Zabielski, Kiela, Barej, Pierzynowski, Weström and Karlsson1991, Reference Zabielski, Onaga, Mineo, Pierzynowski and Kato1994; Kiela et al. Reference Kiela, Zabielski, Podgurniak, Midura, Barej, Gregory and Pierzynowski1996). This led to the conclusion that the information driven by CCK must be switched into a neural mechanism before leaving the gut. This indirect mechanism agrees with the facts that amylase release from human pancreatic acinar cells is not mediated by either the CCK1 or CCK2 receptor in vitro (Miyasaka et al. Reference Miyasaka, Shinozaki, Jimi and Funakoshi2002) and that the administration of antagonists of the CCK2 receptor does not totally inhibit the in vivo pancreatic response to a meal in the pig (Lhoste et al. Reference Lhoste, Fiszlewicz and Corring2002). Moreover, if we consider the classic hypothesis of hormonal action of CCK via the blood, we must keep in mind, first, that the blood plasma contains enzymes, endopeptidases and aminopeptidases, capable of deactivating CCK (Deschodt-Lanckman et al. Reference Deschodt-Lanckman, Bui, Koulisher, Paroutaud and Strosberg1983), and second, that the intestinal blood promptly transports these newly released gut peptides to the liver, an important site of gut peptide deactivation. It seems unlikely, therefore, that a message precisely generated in response to food or other local stimuli in the upper gut would be arbitrarily modified in the first pass by the liver and blood plasma enzymes well before reaching the exocrine pancreas.
In calves, intra-arterial infusion of CCK8 (10 and 100 pmol/kg body weight) induced secretion of pancreatic juice rich in enzymes, without affecting the concentration of CCK in the peripheral blood plasma (Zabielski et al. Reference Zabielski, Onaga, Mineo, Pierzynowski and Kato1994). The intra-arterial stimulation was greater and had a shorter lag time than the respective intravenous stimulation. Cold blockade of vagal nerve conductivity in conscious calves diminished the effect of intra-arterial CCK8, and delayed and decreased the pancreatic response to intravenous CCK8, suggesting that vagal reflexes are particularly important in the local duodenal mechanism (Zabielski et al. Reference Zabielski, Onaga, Mineo, Pierzynowski and Kato1994). In piglets, the intra-arterial infusion of a physiological-like dose of CCK8 (15 pmol/kg body weight) stimulated pancreatic secretion while intravenous infusion was ineffective (Kiela et al. Reference Kiela, Zabielski, Podgurniak, Midura, Barej, Gregory and Pierzynowski1996). Participation of mucosal CCK1 receptors has been indicated following studies with intraduodenal application of a poorly absorbable CCK1 receptor antagonist from the benzodiazepine family, tarazepide (Solvay Pharmaceuticals, Hannover, Germany), in conscious calves (Zabielski et al. Reference Zabielski, Leśniewska, Borlak, Gregory, Kiela, Pierzynowski and Barej1998b). In a rat model, Li & Owyang (Reference Li and Owyang1993, Reference Li and Owyang1994) showed that exogenous CCK8 infused intravenously at large doses may stimulate pancreas protein secretion directly, while low concentrations may stimulate it via vagal afferent (capsaicin-sensitive) pathways. CCK receptors, predominantly of the CCK1 type, located on the peripheral vagal afferent fibres, were suggested to be a target site for this mechanism. Gastroduodenal but not jejunal administration of capsaicin abolished the response to low doses of CCK, confirming that the mechanism might originate in the gastroduodenal area. Thus, currently there is strong evidence for neuronal rather than endocrine action of CCK on pancreatic secretion (Owyang, Reference Owyang1996; Deng & Whitcomb, Reference Deng and Whitcomb1998). The evidence for such neuronal action of CCK on the pancreas also derives from earlier studies in dogs in which atropine was found to inhibit the pancreatic secretion induced by endogenous stimulants of CCK such as leucine or tryptophan (Konturek et al. Reference Konturek, Tasler and Obtulowicz1972), but also by lower, more physiological doses of CCK. Zabielski et al. (Reference Zabielski, Onaga, Mineo, Kato and Pierzynowski1995) found in conscious suckling calves that luminal administration of CCK8 resulted in the stimulation of pancreatic juice flow, and bicarbonate and protein output in a dose-related manner. The protein-secretory increments for equimolar intravenous infusions were, however, greater than for intraduodenal infusions. The effect of luminal CCK8 was delayed by several minutes in comparison with intravenous CCK8, which may be related to the time needed for CCK8 to permeate to the mucosal receptors, but in contrast to the latter it was atropine sensitive, indicating involvement of a cholinergic mechanism. Application of tarazepide helped to clarify the mucosal CCK-related mechanism. It was shown that an intraduodenal bolus administration of tarazepide led to immediate reduction of pancreatic secretion well before any tarazepide was detected in the portal or peripheral blood. The reduction of pancreatic secretion was observed for several hours (Zabielski et al. Reference Zabielski, Leśniewska, Borlak, Gregory, Kiela, Pierzynowski and Barej1998b). Pharmacological blockage of mucosal CCK1 receptors with tarazepide alone, as well as in combination with atropine, totally abolished the pancreatic response to intraduodenal CCK8.
Cholecystokinin–gastrin family peptides and diseases: some examples
Some GI peptides, including peptides of the CCK–gastrin family and their receptors, appear to be involved in the growth of neoplasms of the GI tract, and more particularly in the tumorigenesis of the stomach, colon and pancreas as it was described about 15 years ago (Silen & Gardner, Reference Silen and Gardner1993) and then reviewed more recently (Rozengurt & Walsh, Reference Rozengurt and Walsh2001; Jensen, Reference Jensen2002; Morisset et al. Reference Morisset, Lainé, Biernat and Julien2004; Schally et al. Reference Schally, Szepeshazi, Nagy, Comaru-Schally and Halmos2004). In this section, the objectives are to describe some biological responses occurring upon binding of CCK and gastrin to their specific receptor subtypes in different GI organs under pathological conditions (Table 2).
Table 2 Summary of the recent knowledge on the involvement of cholecystokinin (CCK)–gastrin family peptides and their receptors in the control of digestive functions and more generally their role in the field of nutrition in mammals, in pathological conditions
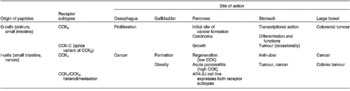
Gastrin and cholecystokinin effects through cholecystokinin 1 receptor occupation
Effects on the stomach
Kawano et al. (Reference Kawano, Hirashima, Mori, Saitoh and Kurosumi1992) reported that OLETF rats were spontaneous mutants with little or no expression of the CCK1 receptor gene (Takiguchi et al. Reference Takiguchi, Takata, Funakoshi, Miyasaka, Kataoka, Fujimura, Goto and Kono1997). In these CCK1 receptor-deficient rats, it was shown that thyroxine-releasing hormone which increases vagal efferent activity, indomethacin which decreases mucosal PG levels, a protective molecule for the stomach, hydrochloric acid and ethanol which increase the severity of gastric mucosal damage, increased the severity of gastric mucosal lesions when compared with control rats. Indeed, it has been demonstrated that CCK has an anti-ulcer action on the gastric mucosa through its action via the CCK1 receptor in rats (Ohumura et al. Reference Ohumura, Shoji, Onodera and Kohgo1996).
During chronic H. pylori infection, pro-inflammatory cytokines are released that can affect ECL cells, thus impairing the secretory function and viability which can predispose to hypochlorhydria and gastric carcinogenesis. Gastrin binds to specific CCK2 receptors on ECL cells and activation of these receptors causes a variety of transcriptional activities which can result in diseases such as enterochromaffin-like cells carcinoids (Prinz et al. Reference Prinz, Zanner and Gratzl2003; Havu, Reference Havu1986).
Effects on the exocrine and endocrine pancreas
In CCK1 receptor-deficient rats, the in vivo release of pancreatic protein in response to exogenous CCK8 and endogenous CCK-release by pancreatic juice diversion were significantly impaired (Funakoshi et al. Reference Funakoshi, Miyasaka, Jimi, Kawanai, Takata and Kono1994); a lack of response to CCK was also observed using freshly isolated acini from these OLETF rats (Funakoshi et al. Reference Funakoshi, Miyasaka, Jimi, Kawanai, Takata and Kono1994).
According to Lacourse et al. (Reference Lacourse, Swanberg, Gillespie, Rehfeld, Saunders and Samuelson1999), the concentration of CCK1 receptor mRNA remained normal in CCK-deficient mice, suggesting that agonist binding does not regulate receptor gene expression. Moreover, in these CCK-deficient mice, growth of their pancreas and their enzymes' adaptation to different diets remained also comparable with control values. It thus seems that other regulatory pathways took over to compensate for the CCK deficiency. These data obtained from CCK-deficient mice agree in some way with those obtained in rats without expression of the CCK1 receptor (Miyasaka et al. Reference Miyasaka, Suzuki, Kanai, Masuda and Funakoshi1999). Indeed, in the OLETF rats, the pancreatic wet weight increases were significantly lower than in normal Long-Evans Tokushima rats at all ages examined but total DNA contents in the whole pancreas and protein concentrations were comparable in both strains. These studies point to the fact that the CCK1 receptor might not be an absolute requirement for normal pancreas growth at least in rodents. Although the pancreatic gland develops normally in CCK1 receptor-deficient rats, its regeneration is significantly delayed after 30 % pancreatectomy, suggesting its importance for pancreatic regeneration (Miyasaka et al. Reference Miyasaka, Ohta, Masuda and Funakoshi1997b).
The absence of CCK1 receptors also impaired functions of the endocrine pancreas; although the pancreatic insulin contents were not affected in CCK1 receptor-deficient rats, its release in response to CCK8 remained at basal level; similarly, CCK8 had no effect on glucagon secretion while it increased the hormone release in normal pancreas. In response to a meal, plasma insulin was reduced and associated with transcient hyperglycaemia in CCK1 receptor-deficient rats. These data clearly demonstrate the importance of the CCK1 receptor in the control of insulin and glucagon secretion along with glycaemia (Funakoshi et al. Reference Funakoshi, Miyasaka, Kanai, Masuda, Yasunami, Nagai, Ikeda, Jinu, Kawanami and Kono1996) and they agree with the recent co-localisation of the CCK1 receptor with insulin and glucagon by immunofluorescence (Morisset et al. Reference Morisset, Julien and Lainé2003). In obese Zucker rats, their pancreatic protein secretion in response to increasing doses of CCK8 was significantly reduced at all doses tested; this impaired release was also associated with significant decreases in the CCK1 receptor high and low affinity sites with no modification in their respective affinity (Praissman & Izzo, Reference Praissman and Izzo1986).
Stimulation of the rat pancreatic gland by a supraphysiological dose of caerulein, a CCK analogue, leads to acute pancreatitis with destruction of the pancreas architecture and a loss of tissue. Regeneration of the pancreas was then observed following caerulein treatment at a physiological dose (Jurkowska et al. Reference Jurkowska, Grondin, Massé and Morisset1992a) during which CCK1 receptor mRNA were tremendously increased (Morisset & Calvo, Reference Morisset and Calvo1998). The regeneration process involved the CCK1 receptors because it was prevented by a concomitant treatment with the CCK1 receptor antagonist, L-364,718 (Jurkowska et al. Reference Jurkowska, Grondin and Morisset1992b).
Effects on the gallbladder
A deletion of a 262 bp coding region of the human gallbladder CCK1 receptor led to obesity and cholesterol gallstone disease in a patient with this mutation. After sequencing, it was found that the majority of the mRNA produced from this gene was abnormally processed, resulting in the deletion of the third exon; this mRNA encoded an inactive receptor unable to bind agonists. Although not yet proven in substantial number of patients, it is tempting to associate this peculiar mutation with gallstone formation and obesity (Miller et al. Reference Miller, Holicky, Ulrich and Wieben1995).
Gastrin and cholecystokinin effects through cholecystokinin 2 receptor occupation
Proliferation of the oesophagus
Over the last two decades, there has been an enormous increase in the incidence of Barrett's metaplasia and oesophageal adenocarcinoma. The reasons behind this phenomenon remain poorly understood and once metaplasia is ongoing, it is highly proliferative. Since gastrin plays an important role in the regulation of GI organ proliferation and differentiation, it became important to evaluate its involvement in the regulation of Barrett's metaplasia. In a recent study (Haigh et al. Reference Haigh, Attwood, Thompson, Jankowski, Kirton, Pritchard, Varro and Dimaline2003), CCK2 receptors were detected by RT-PCR in 30 % of normal patients, in 80 % of patients with oesophagitis, in 100 % of patients with Barrett's metaplasia and in 70 % of patients with oesophageal adenocarcinomas. In the Barrett's group, all patients expressed twice the amount of CCK2 receptors than the controls. In Barrett's mucosal biopsies, gastrin significantly increased DNA synthesis, an effect blocked by the CCK2 receptor antagonist L-740,093. The overexpression of the CCK2 receptor in Barrett's metaplasia may have implications for the management of patients in whom gastrin is elevated by acid-suppression therapy.
Alterations in the stomach
One way to investigate the effects of gastrin on the stomach components and functions is to remove the major site of gastrin production, the gastric antrum. However, contradictory data came out regarding this surgical procedure on the stomach physiology (Martin et al. Reference Martin, MacLoed and Sircus1970; Lehy et al. Reference Lehy, Bonnefond, Dubrasquet, Nasca, Lewin and Bonfils1973). With the event of molecular biology and gene manipulation, receptor-deficient mice were produced and so were mice without CCK2 receptors. In such animals, a marked increase in basal gastric pH was observed along with major increases in plasma gastrin. In the stomach of these deficient animals, parietal and ECL cells were decreased, explaining the reduction in acid output. In the antrum, the gastrin cell population was increased with a reduction in that of the somatostatin cells, consistent with increased plasma gastrin. These data stress the importance of the CCK2 receptors to maintain normal cellular composition, distribution and functions of the gastric gland (Langhans et al. Reference Langhans, Rindi, Chiu, Rehfeld, Ardman, Beinborn and Kopin1997). In similar CCK2 receptor-deficient mice, the following alterations were also observed: thinning of the oxyntic mucosa; reduction in parietal cell number; absence of normal ECL cells with undetectable histidine decarboxylase activity responsible for histamine synthesis. These major changes in the stomach structure and functions plead for a strategic role of the CCK2 receptors in differentiation and functions of the stomach (Chen et al. Reference Chen, Zhao, Al-Haider, Hakanson, Rehfeld and Kopin2002).
Alterations in the pancreas: transfection of the cholecystokinin 2 receptors in normal mice pancreas
With transfection of the human CCK2 receptor in mouse pancreatic acinar cells, a location where it does not belong normally (Morisset et al. Reference Morisset, Julien and Lainé2003), the pancreas of these mice grow significantly bigger at 50 d of life when compared with controls. However, when these mice were crossed with gastrin-mice expressing gastrin in their pancreatic β-cells to obtain continuous gastrin release and thus stimulation of the CCK2 receptors, some of these animals (three out of twenty homozygous) developed malignant transformations through an acinar-ductal carcinoma sequence (Clerc et al. Reference Clerc, Leung-Theung-Long, Wang, Dockray, Bouisson, Delisle, Vaysse, Pradayrol, Fourmy and Dufresne2002). When oedematous pancreatitis is induced in rats by supramaximal doses of caerulein, the pancreas of these animals begins to express the CCK2 receptor early during the destruction process of the gland. However, if a treatment to induce pancreas regeneration by low doses of caerulein is not begun, the CCK2 receptor mRNA expression vanished while it is sustained during 4 d with repeated injection of caerulein (Morisset & Calvo, Reference Morisset and Calvo1998). Expression of CCK2 in the murine pancreas was also shown to modulate acinar cell adhesion and cell differentiation (loss of cell polarity, defective secretion) in vivo. This result suggests an implication in initial sites of cancer formation in conjunction with chemical carcinogens (Bierkamp et al. Reference Bierkamp, Bonhoure, Mathieu, Clerc, Fourmy, Pradayrol, Seva and Dufresne2004).
Alterations in the pancreas: stable transfection of cholecystokinin receptors in human pancreatic cell lines
Transfection of equal amounts of CCK1 and CCK2 receptors in pancreatic Panc and Mia Paca cancerous cells led to a sustained inhibition of their anchorage-independent and also anchorage-dependent growth. In these cells, DNA synthesis was also inhibited in a CCK8-dependent concentration (Detjen et al. Reference Detjen, Fenrich and Logsdon1997). These inhibitions observed in the presence of CCK8 in these cancer cells differ from a stimulation of rat pancreatic acinar cell growth by CCK in vitro (Logsdon, Reference Logsdon1986). These opposite responses are not yet quite understood but may indicate that human cancerous cells of ductal origin behave differently from normal acinar cells isolated from rat pancreas.
Alterations in the pancreas: expression of cholecystokinin receptors in human cancer cells
In six different pancreatic cell lines, binding of [H3]L-365,260, a potent CCK2 receptor antagonist, was specific in all cells with variable concentrations of receptor per cell; CCK1 receptors could not be identified in any cell line (Palmer-Smith et al. Reference Palmer-Smith, Liu, Soundararajan, McLaughlin and Zagon1994). GI tumour cell lines from gastric and colorectal origin, all express the CCK2 receptor with some of them expressing a truncated receptor. These CCK2 truncated receptor cells were always coupled with co-expression of the gastrin gene, implying that a gastrin–CCK2 autocrine loop may operate in these cells (McWilliams et al. Reference McWilliams, Watson, Crosbee, Michaeli and Seth1998).
Alterations in the pancreas: expression of cholecystokinin receptors in human tumours
In rat pancreatic carcinoma obtained from implanted DSL-6 cells (azaserine-induced pancreatic carcinoma), CCK1 receptors already present on these cells were overexpressed while novel expression of the CCK2 receptors was observed (Zhou et al. Reference Zhou, Povoski, Longnecker and Bell1992). From CCK receptor evaluation by in vitro receptor autoradiography, CCK2 receptors were found occasionally in gastroenteropancreatic tumours while the CCK1 subtype was often present (Reubi et al. Reference Reubi, Schaer and Waser1997). The expression of both CCK receptor subtypes in human GI cancers remains poorly documented and is still of a controversial nature. For example, by RT-PCR, CCK1 receptor mRNA was detected in oesophageal cancers, in gastric cancers and in colon cancers; on the contrary, CCK2 receptor mRNA was absent from oesophageal cancers, detected in gastric cancer and in few colon adenocarcinomas (Clerc et al. Reference Clerc, Dufresne, Saillan, Chastre, André, Escrieut, Kennedy, Vaysse, Gespach and Fourmy1997). Their absence from oesophageal cancers disagrees with another study in which oesophageal adenocarcinomas expressed the CCK2 receptors in 70 % of the patients, using the same technique (Haigh et al. Reference Haigh, Attwood, Thompson, Jankowski, Kirton, Pritchard, Varro and Dimaline2003). From a study using autoradiography as a means of receptor detection, it was shown that ductal pancreatic carcinomas rarely expressed both subtypes of CCK receptor; tumours of neuroendocrine differentiation sometimes expressed the CCK2 receptor at the mRNA and protein level (Reubi et al. Reference Reubi, Waser, Gugger, Friess, Kleeff, Kayed, Buchler and Laissue2003). Contrary to normal human pancreas which expressed only traces of poorly processed progastrin, most pancreatic carcinomas and resection margin samples synthesised amidated gastrin. CCK2 receptor mRNA was present in all pancreatic carcinomas, resection margins, and normal pancreatic tissue. Most tumours possess the CCK1 receptor but the α-admidated and O-sulfated CCK peptides were absent from carcinoma and normal pancreatic tissue. These data support the hypothesis for a local gastrin regulatory mechanism in growth of pancreatic carcinoma (Goetze et al. Reference Goetze, Nielsen, Burcharth and Rehfeld2000). Moreover, angiogenesis is the production of new blood vessels from pre-existing ones. This process is necessary for the growth and metastasis of solid tumours. Gastrin induces marked pro-angiogenic effects both in vitro (in human endothelial cells) and in vivo (in human experimental glioma). CCK8 had marginal effects only. Moreover, a CCK2 receptor antagonist (L365,260) significantly antagonised the in vivo G17-mediated pro-angiogenic effects in gliomas, whereas a CCK1 receptor antagonist (L364,718) did not (Lefranc et al. Reference Lefranc, Mijatovic, Mathieu, Rorive, Decaestecker, Debeir, Brotchi, Van Ham, Salmon and Kiss2004).
Other actions in pathological conditions
Cholecystokinin cancer receptor occupation
It is likely that gastrin and CCK influence the growth of the malignant cells of the pancreas and phenotypic transformation (Silen & Gardner, Reference Silen and Gardner1993). Many data reveal the presence of a unique CCK receptor in human pancreatic cancer that functions in growth and is not present in the normal human pancreas. It was well characterised and the term CCK-C receptor or ‘cancer’ receptor, has been proposed to signify the relationship of this receptor to neoplasia (Smith et al. Reference Smith, Verderame, McLaughlin, Martenis, Ballard and Zagon2002). This CCK-C receptor is completely different from another type of CCKc receptor (see p. 264). It is functional and plays a crucial role in the growth of human cancer. It is a splicing variant of the CCK2 receptor which differs from the CCK2 receptor by the presence of intron 4 (Smith et al. Reference Smith, Stanley, Verderame and Zagon2004). It is also expressed in colonic tumours, hepatic metastases and an I-cell line (sk-Co15) (Biagini et al. Reference Biagini, Monges, Vuaroqueaux, Parriaux, Cantaloube and De Micco1997). Moreover, CCK2 receptors which are not present in normal rat pancreas constituted about 34 % of the total high-affinity CCK receptors in tumours. It was suggested that the expression of CCK2 receptors might be induced by gene mutation or amplification during carcinogenesis and may promote tumour growth (Zhou et al. Reference Zhou, Povoski, Longnecker and Bell1992). Tumours of the central and peripheral nervous system exhibited both CCK2 and/or CCK-C receptors (Lefranc et al. Reference Lefranc, Sadeghi, Metens, Brotchi, Salmon and Kiss2003).
Heterodimerisation of cholecystokinin 1 and cholecystokinin 2 receptors
Dimerisation of several GPCR have recently been described, but little is known about their clinical and functional relevance. CCK1 and CCK2 receptors have been found to co-localise in selected areas of the brain where opioids have effects, and both of these receptors have been described to be expressed on AR42J cells. CCK1 and CCK2 receptor heterodimers bind natural agonists normally, but they exhibit unusual functional and regulatory characteristics. Such complexes demonstrated enhanced agonist-stimulated cellular signalling and delayed agonist-induced receptor internalisation. As a likely consequence, agonist-stimulated cell growth was markedly enhanced in cells simultaneously expressing both of these receptors. These results provide the first evidence of interaction between subtypes of CCK1 and CCK2 receptors, along with unique and potentially quite important functional consequences. The physiological and pharmacological activities of CCK and gastrin that have been observed are complex and have been difficult to understand based on the existence of only CCK1 and CCK2 receptor subtypes. Examples of this include the observations that, neither CCK1 nor CCK2 receptor antagonists are able to antagonise the antinociceptive action of CCK in the mouse, and the spectrum of antagonist affinities for CCK receptors on the AR42J rat pancreatic tumour cell line is not consistent with either subtype CCK1 or subtype CCK2 receptors (Cheng et al. Reference Cheng, Harikumar, Holicky and Miller2003).
Applications – future challenges
Over the last 20 years, considerable progress has been made in understanding the physiological factors that regulate CCK and gastrin secretion. These advances have been made possible by the development of specific assays for measuring CCK and gastrin in blood and tissues and the appropriate use of animal models for examining pharmacological agents and nutrients that affect peptide release. These studies have laid out the groundwork for more extensive investigation in animal and human physiology of nutrition and diseases. Thus, the suggestion that gastrin and CCK might also promote the development of cancers of the GIT has been controversial, but an increasing body of evidence now supports the view that the amidated and non-amidated forms of gastrins act as growth factors via different receptors in different regions of the gut.
Gastrin, cholecystokinin and performances
The biological properties of gastrin and CCK as well as their intermediate forms or the molecules involved in their mechanism of action could be used to increase the development (growth and maturation) of the GIT and the digestive performances in animal and human nutrition by using directly these peptides or by the way of increasing their endogenous production and release. For example, in the pig, an enhanced pancreatic function might help to ameliorate the problems that may appear in modern pig production which are associated with weaning. Indeed a red kidney bean lectin treatment was shown to result in an increased capacity of pancreatic enzyme secretion in the suckling piglets due to an increase in CCK secretion (Evilevitch et al. Reference Evilevitch, Pierzynowski, Linderoth, Ahren, Erlanson-Albertsson, Podgurniak and Westrom2005). In calves fed milk replacer containing soya proteins, sodium butyrate, used as an additive in the diet, improved the GIT maturation and increased pancreatic enzyme secretion simultaneously with an elevation of blood levels of gastrin and mainly CCK (Guilloteau et al. Reference Guilloteau, Romé, Le Normand, Savary and Zabielski2004). Moreover, it was shown that the diet component digestibility depends on pancreatic enzyme quantity present in the proximal duodenum (Guilloteau et al. Reference Guilloteau, Le Huërou-Luron, Romé and Plodari1999; Guilloteau & Zabielski, Reference Guilloteau, Zabielski and Garnsworthy2005b).
In human nutrition, incorporation of fibres in the diet is often suggested. Recently, in hypercholesterolaemic men and women, it was shown that solubilised cellulose fibre (free of a multitude of components linked to the plant cell wall, for example, phytic acid, plant sterols, saponins) decreased peak postprandial glucose concentrations after a liquid mixed meal via a decrease in peak postprandial blood CCK concentrations (Geleva et al. Reference Geleva, Thomas, Gannon and Keenan2003). These findings may suggest that plasma CCK could act on the absorption rate of nutrients and consequently could be implicated in the maintenance of good health. In man, the concept of ‘fast’ and ‘slow’ proteins was introduced by Boirie et al. (Reference Boirie, Dangin, Gachon, Vasson, Maubois and Beaufrere1997) to describe the differences in digestion and absorption of whey and casein, and, as a remark, more than 20 years before, by Guilloteau et al. (Reference Guilloteau, Paruelle, Toullec and Mathieu1975) in calves fed milk replacer. Using this concept, Hall et al. (Reference Hall, Millward, Long and Morgan2003) have shown that a preload drink of whey protein is associated with a higher postprandial circulating level of amino acids and CCK compared with an isoenergetic casein preload. This can help in the treatment of obesity and weight management as well as less satiating foods containing ‘slow’ proteins that might be useful in clinical nutrition as sip feeds for elderly or sick patients where increased food intake is desired. In another way, total parenteral nutrition does not stimulate pancreatic secretion and blood gastrin and CCK levels contrary to oral and/or enteral nutrition, underlining the importance of the mucosal origin of the stimuli (O'Keefe et al. Reference O'Keefe, Lee, Anderson, Gennings, Abou-Assi, Clore, Heuman and Chey2003), even if CCK could also act via paracrine and/or neurocrine pathways.
Molecular forms: roles and therapy
Globally, the metabolic clearance rate of the CCK–gastrin family peptides is proportional to the length of the molecular forms, and the actions regarding the molecular forms depend on species as well as the origin (exogenous v. endogenous). Different molecular forms have specific localisations and roles (see pp. 225–256 and pp. 258–260). The regulation of sulfatation alters the pattern of physiological activity of CCK by changing an exclusive CCK1 agonist into an agonist for both CCK1 and CCK2 receptors. Therefore, the physiological relevance of non-sulfated CCK58 (CCK58NS) can be evaluated by determining (1) its existence in blood, brain and peripheral nerves, (2) if there are physiological states that alter the ratio of sulfated and non-sulfated forms of CCK in these tissues and (3) if the concentrations of CCK58NS are sufficient to activate CCK2 receptor in an endocrine, paracrine or neurocrine manner (Reeve et al. Reference Reeve, Liddle, McVey, Vigna, Solomon, Keire, Rosenquist, Shively, Lee, Chew, Green and Coskun2004a). Synthetic canine CCK58 stimulated rat bile pancreatic volume whereas CCK8 caused no increase in volume (Reeve et al. Reference Reeve, Wu, Keire, Faull, Chew, Solomon, Green and Coskun2004b). In addition, purified porcine CCK58 produced a pattern for contraction of the gallbladder different from that of CCK8 (Tatemoto et al. Reference Tatemoto, Jornvall, Siimesmaa, Hallden and Mutt1984). By contrast, porcine CCK33 and CCK8 had similar potencies for stimulation of amylase release from purified acinar cells (Liddle et al. Reference Liddle, Elashoff and Reeve1986). The similar activity of CCK8 and CCK33 and the different activity of CCK58 suggest that the region outside the COOH terminus of rat CCK58 influences expression of CCK biological activity and/or binding and activation of the CCK1 receptor (Reeve et al. Reference Reeve, Keire, Coskun, Green, Evans, Ho, Lee, Davis, Shively and Solomon2003b). In the case of blood perfusion of the regulatory substance, the administered molecular form could determine the effects evoked in the pancreas. Thus, during continuous infusion of sulfated CCK8 (CCK8S), the decreased apoptosis could explain the increased pancreatic weight. By contrast, upon intermittent injections of CCK8S, an increased apoptosis could explain the lack of pancreatic weight gain despite the stimulation of cell proliferation. Injections of CCK8S only transiently decreased the tissue levels of its receptor (Ohlsson et al. Reference Ohlsson, Borg, Rehfeld, Axelson and Sundler2001). These findings also suggest that the method of administration of the regulatory substance could be implicated.
Concerning gastrin, the full-length precursor progastrin (human progastrin1–80) molecule is more potent as a growth factor for large intestinal epithelial cells, for the normal colon and in vitro, than the incompletely processed Gly-extended gastrins and the completely processed peptides (G17), via high-affinity binding sites (Wang et al. Reference Wang, Koh, Varro, Cahill, Dangler, Fox and Dockray1996; Singh et al. Reference Singh, Lu, Cobb, Miller, Tarasova, Varro and Owlia2003). Moreover, this stimulation is similar with progastrin6–80, indicating that the first five residues are not required for biological activity (McQueen et al. Reference McQueen, Kovac, Ho, Rorison, Pannequin, Neumann, Shulkes and Baldwin2002). In addition, progastrin may act as a co-carcinogen in the development of colorectal carcinoma (Singh et al. Reference Singh, Velasco, Given, Varro and Wang2000). In a similar way, available data indicate that proCCK is expressed in certain neuroendocrine tumours and sarcomas whereas the secretion of CCK is impaired in coeliac disease and bulimia nervosa (Rehfeld, Reference Rehfeld2004).
Taking these results together, it seems clear that total immunoreactivity following a RIA measurement for gastrin or CCK cannot provide a reliable indicator of the identity and properties of all the active-derived peptides in different conditions. This is true for most of the prepeptides and biosynthetic intermediates which can have their own effects. Thus, the RIA generally used to determine plasma gastrin do not react with progastrin or biosynthetic intermediates such as the COOH-terminal Gly-extended gastrins (Dockray, Reference Dockray2004). These last products are now thought to have their own biological properties and sometimes are associated with cancers (pancreatic adenocarcinoma, colorectal carcinoma, lung cancer) and nutritional diseases (obesity, intestinal malabsorption).
Diagnosis
To have a better diagnosis as well as a better comprehension of the mechanisms involved, an evaluation of the molecular forms and of the intermediate peptides occurring during the biosynthesis is more and more relevant. Thus, non-classical RIA to determine the multiple classes of gastrin may therefore prove necessary for full analysis in the management of patients with gastrin-related disease (Varro & Ardill, 2004). Another situation in which it is necessary to have a representative diagnostic is to know the degree of pancreatic insufficiency in patients with pancreatitis or pancreatic duct obstruction. In this case, CCK is useful as a single agent for stimulating direct pancreatic enzyme secretions and measurements in the absence of commercially available secretin (Pfefferkorn et al. Reference Pfefferkorn, Fitzgerald, Croffie, Gupta and Caffrey2002). Simple quantitative measurement of duodenal fluid lipase may be a marker of pancreatic secretory function and this physiological observation can serve as basis for further investigation of CCK-stimulated lipase concentration as a new test in the assessment of pancreatic insufficiency (Conwell et al. Reference Conwell, Zuccaro, Morrow, Van Lente, O'Laughlin, Vargo and Dumot2002). Thus, stimulation with exogenous CCK has been proven useful in diagnostic tests of gallbladder and pancreatic diseases (Rehfeld, Reference Rehfeld2004). In another way, Konturek et al. (Reference Konturek, Konturek, Bielanski, Karczewska, Zuchowicz, Hartwich, Rehfeld, Goetze and Hahn2003a) concluded by suggesting that determination of high serum progastrin, amidated gastrins and IL-8 combined with low serum pepsinogen I may be useful biomarkers of gastric cancer (often associated with an H. pylori infection) with acute pangastritis followed by chronic active gastritis, gastric atrophy, intestinal metaplasia and displasia. In addition to standard markers such as pepsinogen, gastrin and IL-8, reactive oxygen species were recently confirmed as biomarkers in patients with gastric inflammation (Naito et al. Reference Naito, Ito, Watanabe and Suzuki2005).
Therapy
Agonist and antagonist tools could be used as therapy. For example, the generation of antibodies to gastrin that bind and thereby sequester the hormone is the basis of the antigen G17DT (Watson & Gilliam, Reference Watson and Gilliam2001). The immunogen raises antibodies that bind the NH2-terminus of G17 and G17-Gly; it is therefore uncertain whether they neutralise other active forms. G17 is a growth factor for pancreatic, stomach and colorectal cancers, and a potent stimulator of gastric acid secretion. The anti-gastrin immunogen, G17DT, consists of a large carrier protein, called diptheria toxoid (DT) and a synthetic peptide, similar to a portion of the G17 hormone, attached to the carrier protein. When administered to patients, G17DT induces an immune response producing antibodies which cross-react and neutralise the target hormone thus preventing its interaction with disease-causing or -participating cells. G17DT has recently been submitted to different phases of approval in the USA, Australia and European Union for the treatment of gastric and pancreatic cancers (Dockray, Reference Dockray2004). In another way, concerning the immune system, exogenous administration of neuropeptides to maintain normal immune defences represents a new field of pharmacotherapeutics against bacterial invasion (Genton & Kudsk, 2003).
Cholecystokinin–gastrin family receptors
The CCK receptor subtypes remain the key elements to all the unanswered questions and controversial responses to CCK and gastrin related to their physiological effects. Due to recent insights elucidating the structure of the two GPCR that mediate their cellular actions, characterisation of receptor location, peptide and receptor genes, development of receptor antagonists and receptor and peptide knockout animals, especially the role of gastrin and CCK and to a lesser extent, gastrin, in normal GI physiology as well as in clinically important GI pathological states, was recently clarified, but again, remains unclear and in many cases, controversial (Jensen, Reference Jensen2002). Again now, it is mandatory to establish the respective cellular location of the CCK receptor subtypes in different organs and in various species for potential therapies with selective and appropriate hormones and receptor inhibitors. Such studies will help to understand physiological responses to CCK and gastrin and thus eliminate many controversies. CCK1 and CCK2 receptor gene-deficient animal models could be useful. In the near future, we will have to deal with the phenomenon of CCK receptor heterodimerisation to explain some integrated physiological responses. It also continues to be necessary to understand the mechanism of the CCK1 receptor promoter polymorphism as it is related to disease processes such as chronic pancreatitis, gallstone formation as well as psychiatric disorders (Miyasaka & Funakoshi, Reference Miyasaka and Funakoshi2003). Polymorphism in the CCK2 receptor can alter ligand affinity and activity as well as basal (or ligand-independent) signalling (Kopin et al. Reference Kopin, McBride, Schaffer and Beinborn2000; Ji et al. Reference Ji, Kopin and Logsdon2000). Thus, species differences between rat and mouse CCK1 receptors determine the divergent acinar cell response to the CCK analogue JMV-180.
Biologically active amidated gastrins act as potent cellular growth factors that are implicated in a variety of normal and abnormal biological processes including maintenance of the gastric mucosa, proliferation of ECL cells, and neoplastic transformation. The expression of the CCK2 receptor in human cancers has also been documented. Studies in transgenic mice and in cultured tumours have suggested that incompletely processed gastrins may have trophic activity independent of amidated gastrins. An important task for the future will be to identify the specific receptor(s) that mediates the biological responses induced by these gastrins and to develop cell model systems and specific antagonists for studying the intracellular signalling pathways stimulated by these novel receptors (Rozengurt & Walsh, Reference Rozengurt and Walsh2001). Thus, as for other GPCR, the cloning of CCK–gastrin family receptor cDNA and genes has stimulated the generation of new biological models (transgenic animals, GM cells, etc) and opened new avenues for research in physiology, pathophysiology, molecular pharmacology and structure–function relationships of receptors.
A number of antagonist and agonist tools are available and could be used as therapeutic treatments (Black & Kalindjian, Reference Black and Kalindjian2002). Thus, on one hand, a CCK1 antagonist might have therapeutic potential for the treatment of pancreatic disorders as prokinetics for the treatment of gastro-oesophageal reflux disease, bowel disorders and gastroparesis. On the other hand, a CCK2 antagonist might have application for the treatment of gastric acid secretion and anxiety disorders (Herranz, Reference Herranz2003). As a first example, since CCK is involved in sensory and motor responses to distension in the GIT (by the way of the CCK1 receptor), it may contribute to the symptoms of constipation, bloating and abdominal pain that are often characteristic of functional GI disorders in general and in irritable bowel syndrome, in particular; CCK1 receptor antagonists are therefore currently under development for the treatment of constipation-predominant IBS (Varga et al. Reference Varga, Balint, Burghardt and D'Amato2004). As a second example, an impairment of pancreatic exocrine function in acute pancreatitis, together with a transient disturbance of bile flow into the duodenum by stones or oedema of the pancreas, may cause an increase in plasma CCK release. The increased CCK may further aggravate pancreatitis and worsen the prognosis of acute pancreatitis by stimulating the injured pancreas, resulting in the vicious cycle via endogenous CCK release. The CCK1 receptor antagonist may have exhibited its therapeutic usefulness in acute pancreatitis by breaking the vicious cycle (Otsuki, Reference Otsuki2000). In a similar way, a variety of potential therapeutic approaches based on the biology of gastrin and its receptors are currently under exploration, including receptor antagonists and the targeted delivery of imaging and cytotoxic agents (Dockray, Reference Dockray2004), but the efficacy of theses therapies needs to be determined.
New techniques to be utilised for detection or therapy of disease implicating cholecystokinin–gastrin family peptides
Several types of diseases are linked to the peptides from the CCK–gastrin family in relation to their receptor subtypes. The first group contains biliary dyskinesia which includes both chronic acalculous cholecystisis and sphincter of Oddi spasm which are well detected by techniques using CCK and/or gastrin assays. Measurement of gallbladder ejection (GBEF) with an intravenous infusion of exogenous CCK8 can be cited as an example of a test method (Krishnamurthy & Krishnamurthy, Reference Krishnamurthy and Krishnamurthy1997). Patients with diabetes have lower plasma levels of CCK which may explain their relatively hypotonic gallbladder and reduced gastric motility (Bucceri et al. Reference Bucceri, Calogero and Brogna2002). The abilility to potentially modify different populations of enteroendocrine cells may become an important therapeutic strategy for treating and/or preventing a variety of common human diseases such as diabetes and obesity (Schonhoff et al. Reference Schonhoff, Giel-Moloney and Leiter2004). New therapy in some nutritional diseases appears in using regulatory peptides. As an example, Brand et al. (Reference Brand, Tagerud, Lambert, Magil, Tatarkiewicz, Doiron and Yan2002) have demonstrated that systemic administration of gastrin or epidermal growth factor can stimulate islet neogenesis in adult diabetic animals resulting in an increased pancreatic secretion and improvement of blood glucose level. Thus, gastrin or epidermal growth factor treatement is potentially an attractive alternative to islet transplantation achieving β-islet cell replacement without invasive surgery or immunosuppression needed to prevent transplant rejection.
Another group, the pathogenesis of the cancers, causes more drastic consequences in the human population as recently reported by global statistics (Burch et al. Reference Burch, Block and Schroeder2000; Parkin et al. Reference Parkin, Bray, Ferlay and Pisani2005). Overall, each year, there were 10·9 millions new cases, 6·7 million deaths and 24·6 million individuals alive with cancer (within 3 years of diagnosis until 2002). Among the total cases, GIT cancers (i.e. strictly oesophageal, stomach, pancreas and colorectal cancers) represent almost 25 %. Colorectal cancer is the most abundant (9·4 %), but the relatively good prognosis means that mortality is about half that incidence (about 0·53 million deaths in 2002), while prevalence is second only to that of breast cancer wordwide (23 % of total cancers). Until recently, stomach cancer was the second most common cancer, but in 2002 it represented only 8·6 % of the new cancer cases and is often linked to H. pylori infection. Oesophageal cancer is the eighth most common cancer wordwide (4·2 % of the total) and sixth most common cause of death from cancer (cancer of the oesophagus has a very poor survival). Pancreatic cancer is responsible for 0·23 million deaths annually (2·2 % of total cancers) and have a relative higher rank for incidence (thirteenth) because of the very poor prognosis (the mortality:incidence ratio is 98 %). Early diagnosis and screening for non-endocrine pancreatic cancer is difficult although the technology for detecting these small tumours is available (Comaru-Schally & Schally, Reference Comaru-Schally, Schally, Vickery and Lunenfeld1990; Watson & Gilliam, Reference Watson and Gilliam2001).
The delay of detection is mostly due to the fact that early symptoms are usually vague, non-specific and very often neglected by the patients and missed by the physicians. Although surgical resection has been shown to improve survival, the majority of patients have disease that has spread beyond the pancreas by the time of diagnosis. Unfortunately, treatment with chemotherapeutic agents has not significantly impacted the natural history of this cancer, with fluorouracil (Schnall & Macdonald, Reference Schnall and Macdonald1991) and gemcitabine (Casper et al. Reference Casper, Green, Kelsen, Heelan, Brown, Flombaum, Trochanowski and Tarassoff1994) offering 4·4 and 5·6 months survival respectively. Thus, conventional chemotherapy has not produced dramatic improvements in response rates or patient survival. Possible new approaches to treat this malignancy could be based on inhibition of gastrin and CCK or their receptors by administration of hormonal peptide analogues as well as on monoclonal antibodies against oncogene receptors; this philosophy could be applied in the case of similar diseases caused by other gut regulatory peptides and/or their own receptors (Schally et al. Reference Schally, Szepeshazi, Nagy, Comaru-Schally and Halmos2004). Because of the poor response of pancreatic cancer to standard chemotherapy and radiation therapy, the investigators have studied this malignancy to determine the mechanisms that are responsible of its growth regulation. Since an additional sixty-nine amino acids in the third intracellular loop of the CCK-C receptor is associated with accelerated growth, it could be speculated that by blocking the translation or function of this portion of the receptor, one could establish normal growth. Additionally, selective gene therapy targeted at the unspliced segment of the CCK-C receptor could possibly restore cancerous cells to normal growth. Thus, Smith et al. (Reference Smith, Verderame, McLaughlin, Martenis, Ballard and Zagon2002) have shown that an antibody produced against this receptor inhibited pancreatic cancer cell growth in culture; this specific antibody could be used to detect pancreatic cancer in the early stages. Moreover, elimination of this CCK-C receptor through antisense technology arrests growth in culture and inhibits growth of established tumours in mice (Smith et al. Reference Smith, Stanley, Verderame and Zagon2004). This form of therapy may be useful clinically for patients with established pancreatic cancer.
Conclusion
In conclusion, after respiration (and oxygenation), nutrition can be considered as the second vital function in mammals since its aim is to transform the components of the diet into nutrients directly absorbable across the wall of the GIT and then to bring the nutrients towards the numerous body cells. This function is under the dependence of an immuno-hormono-nervous regulation by the way of a multitude of regulatory substances; among them, CCK–gastrin family peptides (and their receptors) play a key role in physiological conditions. These peptides are also involved in several pathological states. Intestinal epithelial cell proliferation is essential for the maintenance of the multilayered defence, digestion and absorption of the GIT. However, excess proliferation is also associated with increased risk of cancer. Thus, even if considerable progresses were recently obtained in this field, a better knowledge of the mechanisms involved could be useful to increase the efficiency of the nutritional function as well as to treat the abnormalities in pathological conditions.
Acknowledgements
Thanks are due to A. Barbeau and J. Chevalier (INRA-SENAH, St Gilles, France) for their help in bibliographical research and presentation of illustration, respectively, as well as to A. Sahar for English revision.





